Abstract
Genetic determinants of arachnoid cysts (ACs) are poorly understood. Despite their common incidence, there is little understanding about how ACs form or how they expand. In this chapter, we reviewed published literature and discuss hypotheses on AC formation and expansion. This is followed by a description of the common syndromes and genes associated with ACs to gain insights into their pathogenesis. Finally, we will focus on hydrocephalus and its relationship to ACs due to the common pathophysiology of the two diseases. The most common syndrome that was associated with ACs was glutaric aciduria type 1 which should be considered by the clinician in patients with bilateral ACs. The genes associated with ACs and their usual function are summarized.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Arachnoid cyst
- Pathophysiology of arachnoid cysts
- Syndromes associated with arachnoid cysts
- Genetics of arachnoid cysts
- Hydrocephalus
1 Introduction
Arachnoid cysts (ACs) are cerebrospinal fluid-filled sacs that are enclosed by the arachnoid membrane [103, 142]. ACs have a prevalence [52] of 1.2% in the general population [138]. Men are more commonly affected than women [138, 141]. ACs are found in multiple locations of the brain and spinal cord; however, most are found in the middle cranial fossa and the retrocerebellar fossa [2]. Other frequent locations are the suprasellar and quadrigeminal cisterns, the posterior fossa, and the convexity [2, 8]. Spinal intradural ACs are rare [23]. When they do occur, anterior spinal ACs of idiopathic origins are found mostly in the cervical spine, and posterior spinal ACs are found mostly in the thoracic and thoracolumbar spine [23].
ACs are primarily asymptomatic but can present with clinical findings [141]. Intracranial abnormalities associated with ACs are more common than extracranial abnormalities [8]. Intracranial abnormalities commonly associated with ACs include ventriculomegaly, corpus callosum abnormality (agenesis or absence), microcephaly, hydrocephalus, and mass effect on adjacent structures [8, 143]. With many of these associated abnormalities such as ventriculomegaly, it is unclear whether the AC caused the abnormality or if ACs are a consequence of the abnormality [143]. Further, it is possible that the abnormality is totally unrelated to the AC and that the AC and the abnormality arose because of a third external factor. Less frequently found complications of ACs include chronic subdural hematomas (CSDH) [141]. These are common in younger patients and individuals who have had recent head trauma [141]. Neurological symptoms of ACs are more commonly found in spinal ACs and usually affect motor function [21]. These can include progressive paraparesis or quadriparesis [21]. In the pediatric population, spinal ACs usually present with motor deficits [22]. Other nonspecific clinical features of all ACs include headache, seizures, vomiting, paralysis, and spasms [52].
In addition to the clinical findings attributed to ACs, there are also syndromes associated with ACs. These include glutaric aciduria type I (GA-I) [75] and Proteus syndrome [4] among others. Whether ACs are truly an integral part of these syndromes or whether they are incidental findings will be discussed.
The development of ACs is poorly understood, but there have been genes that are proposed to have an impact on the formation of ACs. These include the KAL1 gene on chromosome Xp22.3 [77] and CHD7 on 8q21.1 [77]. Some of these genes such as the KAL1 gene are indirectly associated with ACs due to the role they play in a syndrome (Kallmann syndrome) that is thought to be linked to ACs [77]. This chapter will introduce and discuss some of these common genes.
2 Method
Prior to the compilation of this chapter, we conducted an extensive literature review using PubMed. We looked at papers discussing the pathogenesis of ACs, the genetics of ACs, and the syndromes associated with ACs. The results were then filtered to look at the systematic reviews and the review articles. We also specifically explored the link between ACs and hydrocephalus. The reason for this is that there is more written about the pathogenesis of hydrocephalus than that of ACs and the two seem to be related via the syndromes.
3 Pathophysiology of ACs
Multiple theories have been suggested in the past regarding the congenital formation of ACs. One theory is that the arachnoid membrane either duplicates, splits, or tears and CSF is forced through this defect by arterial pulsations [8]. The manner in which these defects arise has not been specified, and it is unclear if there are other factors, e.g., thinning of the membrane, that make ACs more likely in some individuals [8].
Another hypothesis is that defects are present in the arachnoid membrane and the cyst expands due to one of two reasons. Either choroid plexus-like tissue within the cyst produces CSF, or a ball and valve mechanism allows CSF to flow into and become trapped in the cyst [143]. Hamada et al. showed that there was choroid plexus tissue present in a 7-month-old patient whose cyst re-enlarged after resection [46]. Singleton et al. also found ectopic choroid plexus tissue in a 26-year-old patient who had an AC in her cerebellopontine angle [122]. Both of these case reports, however, concede that the presence of choroid plexus tissue within the AC is a rare finding. So, in these cases, the ACs may still be incidental findings [46, 122].
The causes of spinal intradural ACs can be idiopathic, traumatic, posthemorrhagic, or post-inflammatory [23]. However, the spinal intradural ACs may form in the same manner as other ACs (ball-valve mechanism, etc.) but remain asymptomatic. They only become symptomatic and detectable when there is trauma or inflammation and thus leads to the impression that the cyst arose because of trauma or inflammation [23].
Kouyialis et al.’s theory supports the posttraumatic and post-inflammatory causes of AC formation [65]. Leptomeningeal inflammation can cause adhesive arachnoiditis with impaired CSF dynamics and loculation that can cause the cysts to form [65]. Then a ball-valve mechanism can cause the AC to increase in size until it becomes symptomatic [65].
Dr. Evangelou, a Neurology Professor at the University of Nottingham [1], and his team’s findings support the Kuhlendahl theory for the formation of ACs [23]. Kuhlendahl proposed that a vent-like CSF flow obstruction caused by arachnoid trabeculae in the spinal canal can be asymptomatic for long periods of time. A pathological process, e.g., inflammation or trauma, can increase the flow of CSF into the previously existing cyst leading to a pressure gradient development [23]. The gradient would allow CSF to flow into the cyst freely but not out and hence result in enlargement of the cyst [23, 44]. Although obstruction is discussed, it is still unclear exactly how to understand the mechanisms that draw water into the cyst in light of Dr. Grzybowski’s findings [37].
Grzybowski did work on in vitro models and showed that the entire arachnoid membrane absorbs CSF. This would provide a much larger surface area for CSF absorption [37]. Further, Dr. Grzybowski found that the membrane absorbs more CSF than the granulations [61]. It was argued that the in vitro models would not be accurate as cell adhesion would not be present, but Dr. Grzybowski demonstrated that the tight junctions are preserved in the in vitro models [50].
There is insufficient evidence to prove or disprove these hypotheses. Furthermore, these theories explain how ACs expand, but do not explore how the defect in the arachnoid membrane formed. To explore this, we need to look at the syndromes and genes associated with ACs.
One hypothesis for the formation of ACs is given by Demir et al. [19]. They propose that the perimedullary mesh (endomeninx), which is a precursor to the pia and arachnoid mater, splits and duplicates anomalously during week 15 of gestation which is when CSF escapes into the layers of the mesh following rupture of the rhombic roof [19].
4 Syndromes Associated with ACs
4.1 Glutaric Aciduria Type 1 (GA-1)
This is an autosomal recessive inborn error of metabolism [75]. A deficiency in glutaryl-CoA dehydrogenase enzyme results in motor symptoms such as dystonia and psychomotor delay due to an inability to catabolize lysine, hydroxylysine, and tryptophan [75]. Macrocephaly, dystonia, and the presence of bilateral temporal ACs are considered diagnostic of GA-1 [72, 75, 115]. However, there is no clear indication of whether the ACs are directly linked to the syndrome as treating the cysts did not relieve the symptoms [75]. The severity of the symptoms has been found to be directly linked to the degree of enlargement of the fissures in the bilateral frontotemporal region around the Sylvian fissures [3, 57, 72]. There can be variation in the presentation of clinical symptoms both between and within families [26].
In a regional neurosurgical department, a total of 147 patients with ACs were found in a population of 890,000 [10, 15, 131, 134]. Of these, only two patients presented with GA-1. So, there was a 1.3% prevalence of ACs and GA-1 in the population.
There is a lot of cerebral damage associated with GA-1, and one explanation for this is that there is a direct effect of glutaric acid (or another related metabolite) on the neurons [75]. Another explanation is that the symptoms are caused by the deposition of l-carnitine in the cerebral tissue [75]. Either way, the loss of neurons, especially in the caudate and the putamen, results in reduced levels of GABA in the brain and CSF [57, 75].
Hald et al. posed an explanation as to how ACs might arise in patients with GA-1. The rapid frontotemporal atrophy would lead to changes in CSF dynamics and cause fluid accumulation [45]. If these changes took place during the folding of the neural tube, then it can result in anomalous splitting of the arachnoid layers resulting in true ACs [45]. Alabedeen et al. found that in GA-1 the location of the ACs aligns with the areas of the brain that are predisposed to atrophy (i.e., the frontotemporal region) [57]. This paper argued that the arachnoid membrane might split due to loss of brain tissue in the surrounding areas and not due to the enzyme imbalances brought about by GA-1 [57]. Other papers in the literature support this hypothesis [3, 72]. An alternative theory is that the atrophy and chronic subdural effusion might be caused by the 3-OHGA affecting endothelial structures in the brain during development and resulting in vascular dysfunction [26].
While the paper by Martinez-Lage et al. [45] discusses how ACs are a part of the GA-1 syndrome, Serarslan et al. and other papers explore how bitemporal ACs and macrocephaly can occur in the absence of GA-1 [57, 118]. GA-1 is diagnosed by the detection of a high concentration of glutaric acid in the urine and a low plasma creatinine level [118]. There were patients present with bilateral ACs and no diagnosis of GA-1 [72, 118]. Thus, ACs can occur for many reasons, but they are commonly associated with GA-1. If they are found either on scans, especially alongside macrocephaly and dystonia, doctors should consider GA-1 as a differential diagnosis [45, 72, 118]. This is extremely important because even simple surgical procedures can be dangerous in children with GA-1 [72]. Surgery would induce a catabolic state in the patient and result in worsening of the metabolic disease.
4.2 Aicardi Syndrome
The syndrome is an X-linked dominant condition characterized by infantile spasms, chorioretinal lacunae, and agenesis of the corpus callosum (either complete or partial) [16, 42, 144, 149]. Here, it is worth noting that ACs are also strongly associated with agenesis of the corpus callosum [8, 143], so it is possible that AC formation is linked to Aicardi syndrome. However, due to the rarity of the syndrome itself, it is hard to conclude this.
Aicardi syndrome has an estimated incidence of 1:105,000 live births in the United States as of 2009 [149], and the prevalence is thought to be higher than reported with an estimated survival rate of 62% at 27 years of age [149].
Yuksel et al. present the case of a female infant with Aicardi syndrome and an AC [144]. They state that these are rare additional findings of the syndrome [144] and there has been a total of nine other examples of Aicardi syndrome with ACs in the literature. Barkovich et al.’s case series describes five patients who all presented with Aicardi syndrome, but not a single one had an AC [6]. Lee et al.’s findings were also similar to those of Barkovich [68]. Thus, ACs are not always associated with Aicardi syndrome and may be a coincidental finding.
Interestingly, Mohammad et al. found a midline AC in a male patient with the 47,XXY karyotype and state that cysts in the interhemispheric fissure are a common (but less emphasized) feature of Aicardi syndrome [149]. Another paper had similar findings [16]. So, while cysts of any nature are common, it is uncommon to find ACs specifically in patients with Aicardi syndrome. This conclusion is, however, unverified as there is limited histological information about the cysts [149].
Aicardi himself re-evaluated the syndrome and stated that corpus callosum agenesis is not the sole hallmark of the disease and is not needed to diagnose the condition if other abnormalities such as cysts were present [55]. Further, the presence of intracranial cysts may indicate some other abnormalities and warrant further investigation (e.g., a fetal MRI) [16]. The findings are important to neurosurgeons consulting parents whose fetus has been diagnosed with a cyst due to the impact it would have on prognosis [16].
4.3 Sturge-Weber Syndrome
Sturge-Weber syndrome is a neurocutaneous syndrome characterized by a facial port-wine stain and hemiparesis among other symptoms [24]. Epilepsy is an essential feature for the diagnosis of this syndrome which encompasses vascular malformations of the brain, skin, and eyes [24]. Of note, GA-1, Proteus, and PHACE syndrome, which are well associated with ACs, are also accompanied by vascular dysfunction. Hence, it may be vascular dysfunction that is causing the formation of ACs.
We identified one paper that described Sturge-Weber syndrome with an AC in a 2-year-old boy [24]. Therefore, it could be that ACs are associated with the syndrome, but it is hard to tell because the syndrome itself is so rare.
4.4 Trigeminal Neuralgia
Trigeminal neuralgia usually presents with paroxysmal lancinating pain in the distributions of the trigeminal nerve and its branches [136]. It can be idiopathic, or it can be caused by compression of the nerve [136]. In the idiopathic cases, demyelination of the trigeminal nerve root has been shown, and the ignition hypothesis proposes that light touch can be interpreted as pain by the nerve due to demyelination between nerve fibers that carry pain and those that carry light touch [136]. Vascular compression is recognized as the most common cause of trigeminal neuralgia, but there have been multiple cases of ACs in various parts of the brain also causing the syndrome [5, 27].
Several papers have reported trigeminal neuralgia being caused by an AC compressing the nerve [97, 136]. Kouyialis et al. report a 55-year-old female patient who experienced pain recurrence after vascular decompression for trigeminal neuralgia [65]. They proposed that direct compression of the nerve or arterial pulsation through a cyst may have caused the pain [65]. Excision of the AC relieved the patient’s symptoms, and so it was felt that the cyst was the cause of the recurrence [65]. Other papers have also reported cases in which the pain has been relieved either following the surgical excision of ACs [39, 47, 107, 126, 135, 145] or following medical therapy [38, 40]. Medical relief was most commonly employed when the AC was in Meckel’s cave and eroding the greater wing of the sphenoid bone [38, 40].
One paper presented a case where the patient had trigeminal neuralgia and an AC in Meckel’s cave. However, her symptoms improved despite the cyst remaining unchanged in size and location [9]. Thus, it is not only the location of the AC, but its size that impacts its ability to compress the nerve and cause trigeminal neuralgia.
There is a very strong association between ACs and trigeminal neuralgia. However, the AC was not a symptom of the syndrome but a cause.
5 Other Syndromes Associated with ACs
There are syndromes linked to ACs by one or two cases. These are listed in Table 1.
We did not explore these further as we feel that they were incidental findings.
6 Genetics of ACs
There have been multiple genes that have been thought to be associated with ACs. Many papers in the literature discuss autosomal dominant polycystic kidney disease (ADPKD) and ACs. In ADPKD, cysts are found in the kidneys, pancreas, seminal vesicles, and arachnoid membrane [48]. Arachnoid membrane cysts are present in 8% of affected individuals and are mostly asymptomatic [48]. This is a large proportion given the incidence of ACs in the general population is 1.2% [138]. Table 2 lists some of the main genes involved in ADPKD.
It is unclear how the proteins are involved in the genesis or sustenance of the AC or how these defects in protein synthesis relate to CSF flow. In the case of PKD1 and PKD2, it is thought that the disruption to the protein’s signaling function within the cell and in primary cilia leads to cells growing and dividing abnormally, causing cysts to develop [91, 92].
Kallmann syndrome is also linked to ACs. It is hypothesized that the syndrome is caused by a defect in the migration of GnRH-1 neurons due to abnormal development of olfactory nerves and bulbs and absence of adhesion proteins [77]. This defect in the neurodevelopmental pathway might contribute to the development of ACs. Table 3 lists some of the genes commonly found in this syndrome and hence may be linked to AC formation.
Long-term epilepsy-associated tumors (LEAT) have also been associated with the formation of ACs [124]. LEAT includes gangliogliomas (GG), dysembryoplastic neuroepithelial tumors (DNT), papillary glioneuronal tumors (PGNT), and adenoid cystic carcinomas [124]. Table 4 lists some of the genes commonly associated with LEAT entities.
While mutations in any of these genes could affect the proliferation of cells, it is uncertain how these mutations ultimately lead to the development of ACs.
Oculopharyngeal dystrophy is another condition to which ACs are linked [73]. This syndrome is caused by repeat expansions in the PABP2 gene (Chr.14q11 in humans) [73] which produces a protein needed for polyadenylation [90]. It is hypothesized that the extra alanine produced by the mutation clump up within muscles leading to loss of muscle function [90]. How this relates to AC formation is still unclear, and it is likely that this gene may not be related to AC formation [90].
One paper conducted a particularly interesting study that looked at the differences in gene expression between the normal arachnoid membrane and the cyst membrane [87]. This paper found 9 (out of 33,096) genes that were different. These are listed in Table 5.
Of these genes ASGR1, SHROOM3, A2BP1, ATP10D, and TRIML1 may be the genes involved in AC formation. Other mutations could be coincidental findings.
Another paper reported on intracranial ACs that showed an X-linked dominant inheritance pattern [24]. There were four family members who all presented with large, bilateral, symmetric middle fossa ACs [24]. They were all found to have a maternally inherited 720-kb duplication of the Xp22.2 chromosome that was not present in any of the unaffected family members [24]. This chromosome region includes the genes listed in Table 6.
Loss of function of MID1 and ARHGAP6 were found due to breakpoints in the duplication [24]. Here, it seems that genes needed for appropriate disposal (or recycling) of proteins were important in the formation of ACs. The other two genes in the region may not be related to the formation of ACs.
Tuberous sclerosis complex (TCS) is a condition caused by mutations in the TSC1 (on Chr.9q34 in humans) and TSC2 (on Chr.16p13.3 in humans) genes that lead to over-activation of the mTOR pathway [11]. Patients with these mutations have also been found to have ACs along with other clinical manifestations, and it seems that TSC2 mutations are more commonly associated with ACs than TSC1 in these individuals [11]. Both these genes are involved in cell growth and cell size control [95].
Papers have found a correlation between skull base meningiomas and middle cranial fossa ACs [128]. The specificity of the location of the condition indicates that local factors such as alterations in intracranial pressure, vascular occlusion, and localized release of bone growth factors might explain the pathology. IGF-1 (Chr.12q23.2), IGF-2 (Chr.11p15.5), and PDGF (Chr.22q13.1) are all involved in bone formation and growth (cell proliferation) [128].
ACs have been associated with syndromes such as spastic paraplegia which is caused by a mutation in the SPG4 gene [73]. The SPG4 gene (now called the SPAST gene) found on Chr.2p21-22 in humans has a role in the functioning of microtubules that allow transport of substances in and out of cells and in cell division [94]. This gene is particularly abundant in neurons [94].
Sporadic SEDAC is thought to be caused by haplo-insufficiency of the HOXD4 gene [106]. HOXD4 is found on Chr.2q31-37 [106] and is important in determining the position of developing limb buds during embryological growth [32].
Patients with Edward’s syndrome have also been found to have ACs [8]. Karyotypes include 47,XY,+18 and 47,X?,+18 [8]. The first karyotype also had severe developmental delay, and the second died neonatally [8].
Both a KAT6A de novo mutation (variant p.P528S, coding DNA c.1582 C > T—likely pathogenic variant) and an inherited USP9X X-linked mutation (variant p.E903G, coding DNA c.2708 A > G—variant of uncertain significance) presented with posterior fossa ACs (PFAC) [41]. KAT6A (Chr.8p11.21) is needed to encode proteins and is important in various parts of the body [104], and USP9X (Chr.Xp11.4) is important in chromosome alignment and segregation during centromere alignment in cell division [108].
The RERE gene (Chr.1p36.23) was found to have heterozygous missense mutations (c.2576C > T) in a 7-year-old and 6-year-old female human cousins. These patients also had intracranial ACs [137]. The RERE gene codes for a regulatory protein and is essential for the development of the brain, eyes, inner ear, heart, and kidneys [93]. The WNT1 gene on Chr.12q13.12 was also found in a patient with ACs [60]. This gene plays a role in the development of the embryonic brain and CNS [33]. Mutations in these genes may cause agenesis of brain structures, but there is not enough evidence to link this to the formation of ACs.
It has been found that lateral meningocele syndrome (LMS) is due to specific pathogenic variants in the last exon of the NOTCH3 gene (Chr.19p13.12) [12]. A paper discussed a patient who presented with this mutation and intradural and extradural ACs alongside other clinical presentations [12]. The NOTCH3 gene is important for the function and survival of vascular smooth muscle [89]. It is also thought to be necessary to maintain the blood vessels in the brain [89].
As discussed in the introduction, GA-1 is a metabolic disorder caused by a mutation in the GCDH gene at Chr.19p13 [127]. GA-1 has been commonly associated with ACs in the literature [127]. The GCDH gene is needed for the breakdown of amino acids lysine, hydroxylysine, and tryptophan [88].
The PAPB2 gene on Chr.14 was linked to genetic myopathy, oculopharyngeal muscular dystrophy (OPMD), and ACs in a family [56]. This gene might play a role in the formation of ACs, but we cannot be sure how this association occurs.
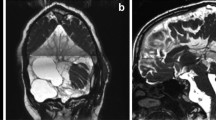
Autosomal recessive missense Rotatin (RTTN) mutations at Chr.18q22.2 have been associated with ACs [13]. In one case study, a brain MRI showed extensive dysgyria associated with nodular heterotopia, large interhemispheric ACs, and corpus callosum hypoplasia [13]. The RTTN gene is needed for left-right specification and plays a role in the maintenance of normal ciliary structure [34]. We are unsure how this relates to AC formation, and further study is needed to understand the association between mutations in this gene and ACs.
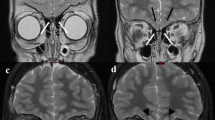
Primary ciliary dyskinesia-related MCIDAS gene mutation is associated with AC formation [116]. The reduced generation of multiple motile cilia (RGMC) and mutation in the multicilin (MCIDAS) gene on Chr.5q11.2 have been linked to a high incidence of hydrocephalus, ACs, and CPH in MCIDAS-associated RGMC [116]. The gene is also required for centriole biogenesis [35]. Thus, like a few other genes mentioned, this gene is required for cilia formation and function. However, we are unsure how this relates to AC formation or expansion.
A rare heterozygous variant in the NID1 gene on Chr.1q42.3 was associated with autosomal dominant Dandy-Walker malformation and occipital cephalocele (ADDWOC) [81]. The paper describes a three-generation family in which individuals presented with ACs in the proband and the proband’s maternal grandfather, an occipital cephalocele in the proband and his brother, and a small bony defect in the proband’s mother [81]. This gene is related to pathways such as MET that promote cell motility and degradation of the extracellular matrix [36]. However, there is no clear indication as to how this is associated with ACs.
A patient with a Col4A1 gene mutation (Chr.13q34) was also found to have an AC [18]. Col4A1 is needed to make one component of type IV collagen [85]. Type IV collagen is one of the main components of the basement membranes in almost all the tissue in the body including the blood vessels [85]. The basement membrane also plays a role in cell migration, proliferation, differentiation, and survival [85]. Mutations in this gene can lead to defects in the basement membrane of blood vessels and lead to impaired movement of electrolytes that may cause CSF flow to change. Igarashi et al. hypothesize that since ACs and vascular smooth muscles originate from mesenchymal cells that surround the neural tube, which also produce collagen for the extracellular matrix in cerebral vessels, both the vascular and mesenchymal structures may be forming at the same time [52]. Thus, the histogenesis of arachnoid and arterial layers may be involved at the same time [52], and defects in either or both may lead to the formation of ACs.
Microdeletions on chromosomes, specifically Chr.22q13.31q13.33 in one case report and Chr.22q13 and Chr.22q11 in another case report, were found along with ACs [43]. Both patients were human females and had other clinical features commonly associated with Phelan-McDermid syndrome (PMS) [43].
There are many other genes that are linked to ACs either through syndromes or via one or two cases in the literature. Table 7 summarizes these genes and their association with ACs.
In summary, genes associated with ACs can be grouped into four categories as shown in Fig. 1.
Given the lack of specific gene mutations associated with ACs, it is difficult to pinpoint which mutations are more impactful than others, and further research is needed to conclude if these genes are in fact related to the formation of ACs.
Some of these genes have been associated with hydrocephalus formation. For example, the primary ciliary dyskinesia-related MCIDAS gene mutation has been known to be found in patients with both ACs and hydrocephalus [35, 116].
7 Hydrocephalus
“Hydrocephalus (HC) is classically defined as dynamic imbalance between the production and absorption of cerebrospinal fluid (CSF), leading to enlarged ventricles” [70]. Hydrocephalus is often found in midline and posterior fossa ACs [76]. It is also possible to observe ventriculomegaly in interhemispheric lesions, but it is rare to see hydrocephalus in middle fossa lesions [76]. Since ACs can be found in all areas of the brain with arachnoid mater and hydrocephalus is not found in all of these areas, it indicates that ACs may not be the sole cause of hydrocephalus.
There has been speculation that some ACs are due to disturbed CSF dynamics and that ACs may be a localized form of hydrocephalus [76]. It may be that ACs are the cause of hydrocephalus or it could be that hydrocephalus causes ACs. However, Martinez-Lage et al. state that “CSF dynamics seem to play a major role in the development of both [arachnoid] cysts and hydrocephalus” [76].
A paper by Topsakal et al. describes a 67-year-old female patient who presented with symptoms of normal pressure hydrocephalus, lower cranial nerve pareses, and pyramidal and cerebellar signs associated with respiratory disturbances [130]. She was found to have a quadrigeminal AC that was compressing the aqueduct and other brain structures [130]. Removing the cyst surgically resolved some of her symptoms including the hydrocephalus [130]. Thus, in this case, it seems that the AC was the cause of the patient’s symptoms including the hydrocephalus.
Basaran et al. discuss a patient with persistent subarachnoid bleeds, hydrocephalus, and ACs [7]. Treating the hydrocephalus did not treat the patient’s symptoms of headaches and diplopia, but treating the ACs did resolve the symptoms [7]. Here it is difficult to distinguish if the hydrocephalus was caused by the AC, but it does show that the AC was not caused by the hydrocephalus since treating the hydrocephalus did not treat the AC. In addition, this article illustrates once again that hydrocephalus, and ACs do occur together very frequently.
There are other papers that support the notion that ACs cause hydrocephalus in patients, most frequently by obstructing and putting pressure on the key ventricular structures of the brain [78, 109, 112, 139].
However, a paper by Pradilla et al. found that only 9% of their 20 patients that presented with ACs had hydrocephalus [111]. So, it seems that hydrocephalus is not always found with ACs and discredits the idea that ACs cause hydrocephalus. Another paper also found that out of ten patients with ACs, only three had hydrocephalus [25]. But here it can be argued that the location, size, and extent of compression caused by the AC might play a role in the development of hydrocephalus [78, 109, 112, 139].
There are also articles that focus on the presence of hydrocephalus and ACs and the role they play in the development of syringomyelia and Chiari malformation type 1 (CM-1) [20, 74, 129]. These papers do not help answer the question as to whether ACs cause hydrocephalus or vice versa, but they do indicate that the two occur together very frequently and may play a role in the formation of other secondary symptoms (such as CM-1).
Perna et al. describe 12 patients with ACs, CM-1, syringomyelia, and hydrocephalus [20]. Given the rarity of CM-1 [20], the fact that 12 cases were found with this combination of clinical symptoms provides some backing to the theory that there might be a third external factor causing the development of both hydrocephalus and ACs. Martinez-Lage et al. found a patient with this same presentation but concluded that the CM-1 and syringomyelia were caused by the hydrocephalus and AC because ventricular decompression and removal of the AC resolved the CM-1 and syringomyelia [74]. They also concur that, usually, the syringomyelia is caused by the obstruction of CSF flow by the AC [74].
ACs and hydrocephalus are closely associated with each other. Table 8 depicts some genes that are thought to be associated with both hydrocephalus and ACs. However, it is still unclear if one causes the other or if they are both the consequence of a third external factor such as a common gene mutation or syndrome.
8 Conclusion
From the above, we can see that there are some syndromes that have a significantly higher association with ACs than others. There are also genes that appear to be linked to AC formation. One common feature of these genes is that most of them seem to be involved in protein production, function, and (like in hydrocephalus) protein transport. Moreover, there is much coinciding between genes and syndromes of hydrocephalus and ACs, so there may be common features between hydrocephalus and ACs such as their mechanism of formation and expansion. Most ACs seem to be sporadic (non-syndromic), but there are instances in which they occur commonly along with other clinical presentations. The presence of agenesis of the corpus callosum (which is very strongly associated with the presence of ACs) should alert clinicians to look for structural malformations that can be present. Conclusively, the mechanism of formation of ACs and pathophysiologic mechanisms involved in their expansion are poorly understood. Further research is required to understand the mechanisms presented and discussed within this chapter.
References
Neurology Academy 2021. Available at: https://neurologyacademy.org/profiles/dr-nikos-evangelou. Accessed 20 November 2021.
Al-Holou W, Terman S, Kilburg C, Garton H, Muraszko K, Maher C. Prevalence and natural history of arachnoid cysts in adults. J Neurosurg. 2013;118(2):222–31.
Alkan A, Baysal T, Yakinci C, Sigirci A, Kutlu R. Glutaric aciduria type I diagnosed after poliovirus immunization: magnetic resonance findings. Pediatr Neurol. 2002;26(5):405–7. https://doi.org/10.1016/s0887-8994(01)00411-8.
Anik Y, Anik I, Gonullu E, Inan N, Demirci A. Proteus syndrome with syringohydromyelia and arachnoid cyst. Childs Nerv Syst. 2007;23(10):1199–202.; ; discussion 1203. https://doi.org/10.1007/s00381-007-0364-z.
Babu R, Murali R. Arachnoid cyst of the cerebellopontine angle manifesting as contralateral trigeminal neuralgia: case report. Neurosurgery. 1991;28(6):886–7. https://doi.org/10.1097/00006123-199106000-00018.
Barkovich AJ, Simon EM, Walsh CA. Callosal agenesis with cyst: a better understanding and new classification. Neurology. 2001;56(2):220–7. https://doi.org/10.1212/wnl.56.2.220.
Basaran R, Kaksi M, Efendioglu M, Onoz M, Balkuv E, Kaner T. Spinal arachnoid cyst associated with arachnoiditis following subarachnoid haemorrhage in adult patients: A case report and literature review. Br J Neurosurg. 2015;29(2):285–9. https://doi.org/10.3109/02688697.2014.976175. Epub 2014 Nov 3
Beresford C, Hall S, Smedley A, Mathad N, Waters R, Chakraborty A, Sparrow OC, Tsitouras V. Prenatal diagnosis of arachnoid cysts: a case series and systematic review. Childs Nerv Syst. 2020;36(4):729–41. https://doi.org/10.1007/s00381-019-04477-6. Epub 2020 Jan 2
Bigder MG, Helmi A, Kaufmann AM. Trigeminal neuropathy associated with an enlarging arachnoid cyst in Meckel’s cave: case report, management strategy and review of the literature. Acta Neurochir. 2017;159(12):2309–12. https://doi.org/10.1007/s00701-017-3262-5. Epub 2017 Jul 31
Bijarnia S, Wiley V, Carpenter K, Christodoulou J, Ellaway CJ, Wilcken B. Glutaric aciduria type I: outcome following detection by newborn screening. J Inherit Metab Dis. 2008;31(4):503–7. https://doi.org/10.1007/s10545-008-0912-z. Epub 2008 Aug 9
Boronat S, Barber I. Less common manifestations in TSC. Am J Med Genet C Semin Med Genet. 2018;178(3):348–54. https://doi.org/10.1002/ajmg.c.31648. Epub 2018 Aug 29
Cappuccio G, Apuzzo D, Alagia M, Torella A, Pinelli M, Franco B, Corrado B, Del Giudice E, D'Amico A, Nigro V, TUDP, Brunetti-Pierri N. Expansion of the phenotype of lateral meningocele syndrome. Am J Med Genet A. 2020;182(5):1259–62. https://doi.org/10.1002/ajmg.a.61536. Epub 2020 Mar 6
Cavallin M, Bery A, Maillard C, Salomon LJ, Bole C, Reilly ML, Nitschké P, Boddaert N, Bahi-Buisson N. Recurrent RTTN mutation leading to severe microcephaly, polymicrogyria and growth restriction. Eur J Med Genet. 2018;61(12):755–8. https://doi.org/10.1016/j.ejmg.2018.08.001. Epub 2018 Aug 16
Chapman T, Mahalingam S, Ishak GE, Nixon JN, Siebert J, Dighe MK. Diagnostic imaging of posterior fossa anomalies in the fetus and neonate: part 2, posterior fossa disorders. Clin Imaging. 2015;39(2):167–75. https://doi.org/10.1016/j.clinimag.2014.10.012. Epub 2014 Oct 22
Christensen E, Ribes A, Merinero B, Zschocke J. Correlation of genotype and phenotype in glutaryl-CoA dehydrogenase deficiency. J Inherit Metab Dis. 2004;27(6):861–8. https://doi.org/10.1023/B:BOLI.0000045770.93429.3c.
Columbano L, Luedemann W, Kusaka Y, Oi S, Samii M. Prenatal diagnosed cyst of the quadrigeminal cistern in Aicardi syndrome. Childs Nerv Syst. 2009;25(5):521–2. https://doi.org/10.1007/s00381-008-0772-8. Epub 2008 Dec 24
Correa GG, Amaral LF, Vedolin LM. Neuroimaging of Dandy-Walker malformation: new concepts. Top Magn Reson Imaging. 2011;22(6):303–12. https://doi.org/10.1097/RMR.0b013e3182a2ca77.
Değerliyurt A, Ceylaner G, Koçak H, Bilginer Gürbüz B, Cihan BS, Rizzu P, Ceylaner S. A new family with autosomal dominant porencephaly with a novel Col4A1 mutation. Are arachnoid cysts related to Col4A1 mutations? Genet Couns. 2012;23(2):185–93.
Demir HD, Deniz FE, Yardim H. A rare brain developmental anomaly in a patient with Usher’s syndrome. Int Ophthalmol. 2010;30(1):85–8. https://doi.org/10.1007/s10792-008-9277-4. Epub 2008 Nov 13
Di Perna G, Piatelli G, Rossi A, Consales A, Fiaschi P, Castaldo M, Pavanello M. Coexisting Retrocerebellar arachnoid cyst and Chiari type 1 malformation: 3 pediatric cases of surgical management tailored to the pathogenic mechanism and systematic review of the literature. World Neurosurg. 2021;148:44–53. https://doi.org/10.1016/j.wneu.2020.12.094. Epub 2020 Dec 29
Engelhardt J, Vignes J. Anterior cervical intradural arachnoid cyst, a rare cause of spinal cord compression: a case report with video systematic literature review. Eur Spine J. 2015;25(S1):19–26.
Evangelou P, Meixensberger J, Bernhard M, Hirsch W, Kiess W, Merkenschlager A, Nestler U, Preuss M. Operative management of idiopathic spinal intradural arachnoid cysts in children: a systematic review. Childs Nerv Syst. 2013;29(4):657–64. https://doi.org/10.1007/s00381-012-1990-7. Epub 2012 Dec 9
Evangelou P, Meixensberger J, Bernhard M, Hirsch W, Kiess W, Merkenschlager A, Nestler U, Preuss M. Operative management of idiopathic spinal intradural arachnoid cysts in children: a systematic review. Childs Nerv Syst. 2012;29(4):657–64.
Furey CG, Timberlake AT, Nelson-Williams C, Duran D, Li P, Jackson EM, Kahle KT. Xp22.2 chromosomal duplication in familial intracranial arachnoid cyst. JAMA Neurol. 2017;74(12):1503–4. https://doi.org/10.1001/jamaneurol.2017.3399.
Galarza M, López-Guerrero AL, Martínez-Lage JF. Posterior fossa arachnoid cysts and cerebellar tonsillar descent: short review. Neurosurg Rev. 2010;33(3):305–14.; ; discussion 314. https://doi.org/10.1007/s10143-010-0262-9.
Garcia P, Martins E, Diogo L, Rocha H, Marcão A, Gaspar E, Almeida M, Vaz C, Soares I, Barbot C, Vilarinho L. Outcome of three cases of untreated maternal glutaric aciduria type I. Eur J Pediatr. 2008;167(5):569–73. https://doi.org/10.1007/s00431-007-0556-2. Epub 2007 Jul 28
Genc E, Dogan EA, Kocaogullar Y, Emlik D. A case with prepontine (clival) arachnoid cyst manifested as trigeminal neuralgia. Headache. 2008;48(10):1525–7. https://doi.org/10.1111/j.1526-4610.2008.01147.x. Epub 2008 Jun 11
Genecards.org. 2021. Available at: https://www.genecards.org/cgi-bin/carddisp.pl?gene=DPEP2. Accessed 20 November 2021.
Genecards.org. 2021. Available at: https://www.genecards.org/cgi-bin/carddisp.pl?gene=ATP10D#:~:text=UniProtKB%2FSwiss%2DProt%20Summary%20for,leaflet%20of%20the%20plasma%20membrane. Accessed 20 November 2021.
Genecards.org. 2021. Available at: https://www.genecards.org/cgi-bin/carddisp.pl?gene=NMU#:~:text=Stimulates%20muscle%20contractions%20of%20specific,the%20ileum%20and%20urinary%20bladder. Accessed 20 November 2021.
Genecards.org. 2021. Available at: https://www.genecards.org/cgi-bin/carddisp.pl?gene=BEND5. Accessed 20 November 2021.
Genecards.org. 2021. Available at: https://www.genecards.org/cgi-bin/carddisp.pl?gene=HOXD4. Accessed 20 November 2021.
Genecards.org. 2021. Available at: https://www.genecards.org/cgi-bin/carddisp.pl?gene=WNT1#:~:text=UniProtKB%2FSwiss%2DProt%20Summary%20for%20WNT1%20Gene&text=Plays%20an%20essential%20role%20in,23499309%2C%20PubMed%3A23656646). Accessed 20 November 2021.
Genecards.org. 2021. Available at: https://www.genecards.org/cgi-bin/carddisp.pl?gene=RTTN#:~:text=UniProtKB%2FSwiss%2DProt%20Summary%20for,of%20NODAL%2C%20LEFTY%20and%20PITX2. Accessed 20 November 2021.
Genecards.org. 2021. Available at: https://www.genecards.org/cgi-bin/carddisp.pl?gene=MCIDAS. Accessed 20 November 2021.
Genecards.org. 2021. Available at: https://www.genecards.org/cgi-bin/carddisp.pl?gene=NID1#:~:text=NID1%20(Nidogen%201)%20is%20a,Degradation%20of%20the%20extracellular%20matrix. Accessed 20 November 2021.
Glimcher SA, Holman DW, Lubow M, Grzybowski DM. Ex vivo model of cerebrospinal fluid outflow across human arachnoid granulations. Invest Ophthalmol Vis Sci. 2008;49(11):4721–8. https://doi.org/10.1167/iovs.08-2238. Epub 2008 Jul 9
Granata F, Alafaci C, Passalacqua M, Cacciola F, Caffo M, Salpietro FM, Vinci SL, Longo M. Non-traumatic sphenoidal intradiploic arachnoid cyst as a cause of trigeminal neuralgia. A case report. Neuroradiol J. 2011;24(6):867–71. https://doi.org/10.1177/197140091102400606. Epub 2011 Dec 23
Grande-Martín A, Díaz-Conejo R, Verdú-Pérez A, Hernández-Moneo JL. Trigeminal neuralgia in a child with a cerebellopontine angle arachnoid cyst. Pediatr Neurol. 2015;53(2):178–9. https://doi.org/10.1016/j.pediatrneurol.2015.03.010. Epub 2015 Mar 13
Grasso G, Passalacqua M, Giambartino F, Cacciola F, Caruso G, Tomasello F. Typical trigeminal neuralgia by an atypical compression: case report and review of the literature. Turk Neurosurg. 2014;24(1):82–5. https://doi.org/10.5137/1019-5149.JTN.7048-12.0.
Guell X, Anteraper SA, Ghosh SS, Gabrieli JDE, Schmahmann JD. Neurodevelopmental and psychiatric symptoms in patients with a cyst compressing the cerebellum: an ongoing enigma. Cerebellum. 2020;19(1):16–29. https://doi.org/10.1007/s12311-019-01050-4.
Guerriero S, Sciruicchio V, De Blasi R, Furino C, Smaldone G, Ciracì L, Galeone D. Chorioretinal lacunae: pathognomonic findings for Aicardi syndrome. J Pediatr Ophthalmol Strabismus. 2010;47:e1–3. https://doi.org/10.3928/01913913-20100324-03.
Ha JF, Ahmad A, Lesperance MM. Clinical characterization of novel chromosome 22q13 microdeletions. Int J Pediatr Otorhinolaryngol. 2017;95:121–6. https://doi.org/10.1016/j.ijporl.2016.12.008. Epub 2016 Dec 23
Halani SH, Safain MG, Heilman CB. Arachnoid cyst slit valves: the mechanism for arachnoid cyst enlargement. J Neurosurg Pediatr. 2013;12(1):62–6. https://doi.org/10.3171/2013.4.PEDS12609. Epub 2013 May 10
Hald JK, Nakstad PH, Skjeldal OH, Strømme P. Bilateral arachnoid cysts of the temporal fossa in four children with glutaric aciduria type I. AJNR Am J Neuroradiol. 1991;12(3):407–9.
Hamada H, Nonaka Y, Kusaka Y, Nakazaki H, Abdullah SH, Oi S. Huge arachnoid cyst incorporating choroid plexus. Childs Nerv Syst. 2006;22(4):420–3. https://doi.org/10.1007/s00381-005-1174-9. Epub 2005 Jun 3
Hanakita S, Oya S, Matsui T. Trigeminal neuralgia caused by an arachnoid cyst in Meckel’s cave: A case report and literature review. Surg Neurol Int. 2021;10(12):45. https://doi.org/10.25259/SNI_734_2020.
Harris PC, Torres VE. Polycystic kidney disease, autosomal dominant. 2002 Jan 10 [updated 2018 Jul 19]. In: Adam MP, Ardinger HH, Pagon RA, Wallace SE, bean LJH, Mirzaa G, Amemiya A, editors. GeneReviews®. Seattle (WA): University of Washington, Seattle; 1993–2021.
Helland CA, Aarhus M, Knappskog P, Olsson LK, Lund-Johansen M, Amiry-Moghaddam M, Wester K. Increased NKCC1 expression in arachnoid cysts supports secretory basis for cyst formation. Exp Neurol. 2010;224(2):424–8. https://doi.org/10.1016/j.expneurol.2010.05.002. Epub 2010 May 21
Holman DW, Grzybowski DM, Mehta BC, Katz SE, Lubow M. Characterization of cytoskeletal and junctional proteins expressed by cells cultured from human arachnoid granulation tissue. Cerebrospinal Fluid Res. 2005;13(2):9. https://doi.org/10.1186/1743-8454-2-9.
Holmes LB, Redline RW, Brown DL, Williams AJ, Collins T. Absence/hypoplasia of tibia, polydactyly, retrocerebellar arachnoid cyst, and other anomalies: an autosomal recessive disorder. J Med Genet. 1995;32(11):896–900. https://doi.org/10.1136/jmg.32.11.896.
Igarashi Y, Murai Y, Yamada O, Shirokane K, Hironaka K, Sato S, Sugiyama M, Tachizawa T, Morita A. Cerebral aneurysm associated with an arachnoid cyst: 3 case reports and a systematic review of the literature. World Neurosurg. 2018;109:e203–9. https://doi.org/10.1016/j.wneu.2017.09.139. Epub 2017 Sep 28
Ishizaka S, Hayashi K, Otsuka M, Fukuda S, Tsunoda K, Ushijima R, Kitagawa N, Suyama K, Nagata I. Syringomyelia and arachnoid cysts associated with spinal arachnoiditis following subarachnoid hemorrhage. Neurol Med Chir (Tokyo). 2012;52(9):686–90. https://doi.org/10.2176/nmc.52.686.
Islam MP. Neurocutaneous melanosis. Handb Clin Neurol. 2015;132:111–7. https://doi.org/10.1016/B978-0-444-62702-5.00007-X.
Iturralde D, Meyerle CB, Yannuzzi LA. Aicardi syndrome: chorioretinal lacunae without corpus callosum agenesis. Retina. 2006;26(8):977–8. https://doi.org/10.1097/01.iae.0000224937.78389.15.
Jadeja KJ, Grewal RP. Familial arachnoid cysts associated with oculopharyngeal muscular dystrophy. J Clin Neurosci. 2003;10(1):125–7. https://doi.org/10.1016/s0967-5868(02)00105-4.
Jamjoom ZA, Okamoto E, Jamjoom AH, Al-Hajery O, Abu-Melha A. Bilateral arachnoid cysts of the sylvian region in female siblings with glutaric aciduria type I. report of two cases. J Neurosurg. 1995;82(6):1078–81. https://doi.org/10.3171/jns.1995.82.6.1078.
Jonklaas J. Atypical presentation of a patient with both Kallmann syndrome and a craniopharyngioma: case report and literature review. Endocr Pract. 2005;11(1):30–6. https://doi.org/10.4158/EP.11.1.30.
Kaisho Y, Miyazaki S, Shimo-oku M, Hayashi T, Tani E. A case of suprasellar arachnoid cyst followed up for a long time. Nippon Ganka Gakkai Zasshi. 1995;99(1):109–14. Japanese
Kantaputra PN, Sirirungruangsarn Y, Visrutaratna P, Petcharunpaisan S, Carlson BM, Intachai W, Sudasna J, Kampuansai J, Dejkhamron P. WNT1-associated osteogenesis imperfecta with atrophic frontal lobes and arachnoid cysts. J Hum Genet. 2019;64(4):291–6. https://doi.org/10.1038/s10038-019-0565-9. Epub 2019 Jan 28
Kapoor KG, Katz SE, Grzybowski DM, Lubow M. Cerebrospinal fluid outflow: an evolving perspective. Brain Res Bull. 2008;77(6):327–34. https://doi.org/10.1016/j.brainresbull.2008.08.009. Epub 2008 Sep 13
Kara B, Kayserili H, Imer M, Calişkan M, Ozmen M. Quadrigeminal cistern arachnoid cyst in a patient with kabuki syndrome. Pediatr Neurol. 2006;34(6):478–80. https://doi.org/10.1016/j.pediatrneurol.2005.11.006.
Kau T, Veraguth D, Schiegl H, Scheer I, Boltshauser E. Chudley-McCullough syndrome: case report and review of the neuroimaging spectrum. Neuropediatrics. 2012;43(1):44–7. https://doi.org/10.1055/s-0032-1307451. Epub 2012 Mar 19
Kollias SS, Ball WS Jr, Prenger EC. Cystic malformations of the posterior fossa: differential diagnosis clarified through embryologic analysis. Radiographics. 1993;13(6):1211–31. https://doi.org/10.1148/radiographics.13.6.8031352.
Kouyialis AT, Stranjalis G, Boviatsis EJ, Ziaka DS, Bouras TI, Sakas DE. Recurrence of trigeminal neuralgia due to an acquired arachnoid cyst. J Clin Neurosci. 2008;15(12):1409–11. https://doi.org/10.1016/j.jocn.2006.10.027. Epub 2008 Oct 7
Kurt S, Cevik B, Aksoy D, Sahbaz EI, Gundogdu Eken A, Basak AN. Atypical features in a large turkish family affected with friedreich ataxia. Case Rep Neurol Med. 2016;2016:4515938. https://doi.org/10.1155/2016/4515938. Epub 2016 Sep 7
Lee HJ, Cho DY. Symptomatic spinal intradural arachnoid cysts in the pediatric age group: description of three new cases and review of the literature. Pediatr Neurosurg. 2001;35(4):181–7. https://doi.org/10.1159/000050419.
Lee SW, Kim KS, Cho SM, Lee SJ. An atypical case of Aicardi syndrome with favorable outcome. Korean J Ophthalmol. 2004;18(1):79–83. https://doi.org/10.3341/kjo.2004.18.1.79.
Leibovitz Z, Guibaud L, Garel C, Massoud M, Karl K, Malinger G, Haratz KK, Gindes L, Tamarkin M, Ben-Sira L, Lev D, Shalev J, Brasseur-Daudruy M, Gutierrez C, de Piñeres CA, Lerman-Sagie T. The cerebellar “tilted telephone receiver sign” enables prenatal diagnosis of PHACES syndrome. Eur J Paediatr Neurol. 2018;22(6):900–9. https://doi.org/10.1016/j.ejpn.2018.08.006. Epub 2018 Sep 1
Leinonen V, Vanninen R, Rauramaa T. Cerebrospinal fluid circulation and hydrocephalus. Handb Clin Neurol. 2018;145:39–50.
Lerman-Sagie T, Prayer D, Stöcklein S, Malinger G. Fetal cerebellar disorders. Handb Clin Neurol. 2018;155:3–23. https://doi.org/10.1016/B978-0-444-64189-2.00001-9.
Lütcherath V, Waaler PE, Jellum E, Wester K. Children with bilateral temporal arachnoid cysts may have glutaric aciduria type 1 (GAT1); operation without knowing that may be harmful. Acta Neurochir. 2000;142(9):1025–30. https://doi.org/10.1007/s007010070058.
Martin MM, Lockspieler T, Slavotinek AM. Oculo-ectodermal syndrome: is arachnoid cyst a common finding? Clin Dysmorphol. 2007;16(1):35–8. https://doi.org/10.1097/MCD.0b013e328010b7f9.
Martínez-Lage JF, Almagro MJ, de San R, Pedro J, Ruiz-Espejo A, Felipe-Murcia M. Regression of syringomyelia and tonsillar herniation after posterior fossa arachnoid cyst excision. Case report and literature review. Neurocirugia (Astur). 2007;18(3):227–31.
Martínez-Lage JF, Casas C, Fernández MA, Puche A, Rodriguez Costa T, Poza M. Macrocephaly, dystonia, and bilateral temporal arachnoid cysts: glutaric aciduria type 1. Childs Nerv Syst. 1994;10(3):198–203. https://doi.org/10.1007/BF00301092.
Martínez-Lage JF, Pérez-Espejo MA, Almagro MJ, López-Guerrero AL. Hydrocephalus and arachnoid cysts. Childs Nerv Syst. 2011;27(10):1643–52. https://doi.org/10.1007/s00381-011-1481-2. Epub 2011 Sep 17
Massimi L, Izzo A, Paternoster G, Frassanito P, Di Rocco C. Arachnoid cyst: a further anomaly associated with Kallmann syndrome? Childs Nerv Syst. 2016;32(9):1607–14. https://doi.org/10.1007/s00381-016-3154-7. Epub 2016 Jul 5
Mattox A, Choi JD, Leith-Gray L, Grant GA, Adamson DC. Guidelines for the management of obstructive hydrocephalus from suprasellar-prepontine arachnoid cysts using endoscopic third ventriculocystocisternostomy. Surg Innov. 2010;17(3):206–16. https://doi.org/10.1177/1553350610377212. Epub 2010 Aug 5
Mayo Clinic. 2021. Hydrocephalus—symptoms and causes. Available at: https://www.mayoclinic.org/diseases-conditions/hydrocephalus/symptoms-causes/syc-20373604. Accessed 20 November 2021.
McKnight I, Hart C, Park IH, Shim JW. Genes causing congenital hydrocephalus: their chromosomal characteristics of telomere proximity and DNA compositions. Exp Neurol. 2021;335:113523. https://doi.org/10.1016/j.expneurol.2020.113523. Epub 2020 Nov 4
McNiven V, Ito YA, Hartley T, Kernohan K, Miller E, Care4Rare Canada, Armour CM. NID1 variant associated with occipital cephaloceles in a family expressing a spectrum of phenotypes. Am J Med Genet A. 2019;179(5):837–41. https://doi.org/10.1002/ajmg.a.61095. Epub 2019 Feb 17
Medlineplus.gov. 2021. AMELX gene: MedlinePlus Genetics. Available at: https://medlineplus.gov/genetics/gene/amelx/. Accessed 20 November 2021.
Medlineplus.gov. 2021. ATP1A3 gene: MedlinePlus Genetics. Available at: https://medlineplus.gov/genetics/gene/atp1a3/. Accessed 20 November 2021.
Medlineplus.gov. 2021. BRAF gene: MedlinePlus Genetics. Available at: https://medlineplus.gov/genetics/gene/braf/#conditions. Accessed 20 November 2021.
Medlineplus.gov. 2021. COL4A1 gene: MedlinePlus Genetics. Available at: https://medlineplus.gov/genetics/gene/col4a1/. Accessed 20 November 2021.
Medlineplus.gov. 2021. FGFR1 gene: MedlinePlus Genetics. Available at: https://medlineplus.gov/genetics/gene/fgfr1/. Accessed 20 November 2021.
Medlineplus.gov. 2021. FOXC2 gene: MedlinePlus Genetics. Available at: https://medlineplus.gov/genetics/gene/foxc2/#conditions. Accessed 20 November 2021.
Medlineplus.gov. 2021. GCDH gene: MedlinePlus Genetics. Available at: https://medlineplus.gov/genetics/gene/gcdh/#:~:text=The%20GCDH%20gene%20provides%20instructions,are%20building%20blocks%20of%20proteins. Accessed 20 November 2021.
Medlineplus.gov. 2021. NOTCH3 gene: MedlinePlus Genetics. Available at: https://medlineplus.gov/genetics/gene/notch3/#:~:text=The%20NOTCH3%20protein%20plays%20a,supply%20blood%20to%20the%20brain. Accessed 20 November 2021.
Medlineplus.gov. 2021. PABPN1 gene: MedlinePlus Genetics. Available at: https://medlineplus.gov/genetics/gene/pabpn1/#conditions. Accessed 20 November 2021.
Medlineplus.gov. 2021. PKD1 gene: MedlinePlus Genetics. Available at: https://medlineplus.gov/genetics/gene/pkd1/#:~:text=Normal%20Function&text=The%20PKD1%20gene%20provides%20instructions,made%20in%20normal%20adult%20kidneys. Accessed 20 November 2021.
Medlineplus.gov. 2021. PKD2 gene: MedlinePlus Genetics. Available at: https://medlineplus.gov/genetics/gene/pkd2/#:~:text=Normal%20Function&text=The%20PKD2%20gene%20provides%20instructions,and%20in%20many%20adult%20tissues. Accessed 20 November 2021.
Medlineplus.gov. 2021. RERE gene: MedlinePlus Genetics. Available at: https://medlineplus.gov/genetics/gene/rere/. Accessed 20 November 2021.
Medlineplus.gov. 2021. SPAST gene: MedlinePlus Genetics. Available at: https://medlineplus.gov/genetics/gene/spast/. Accessed 20 November 2021.
Medlineplus.gov. 2021. TSC1 gene: MedlinePlus Genetics. Available at: https://medlineplus.gov/genetics/gene/tsc1/. Accessed 20 November 2021.
Medlineplus.gov. 2021. ZIC2 gene: MedlinePlus Genetics. [online] Available at: https://medlineplus.gov/genetics/gene/zic2/#:~:text=The%20ZIC2%20gene%20provides%20instructions,the%20activity%20of%20certain%20genes. Accessed 20 November 2021.
Mitsos AP, Samelis AI, Panteleakou-Sameli HM, Kottas GD. Arachnoid cyst of quadrigeminal cistern presenting as trigeminal neuralgia. Acta Neurochir. 2006;148(1):93–4.; ; discussion 94. https://doi.org/10.1007/s00701-005-0640-1.
Miyake S, Tamaki N, Nagashima T, Kurata H, Eguchi T, Kimura H. Idiopathic spinal cord herniation. Report of two cases and review of the literature. J Neurosurg. 1998;88(2):331–5. https://doi.org/10.3171/jns.1998.88.2.0331.
Miyamoto T, Ebisudani D, Kitamura K, Ohshima T, Horiguchi H, Nagahiro S. Surgical management of symptomatic intrasellar arachnoid cysts--two case reports. Neurol Med Chir (Tokyo). 1999;39(13):941–5. https://doi.org/10.2176/nmc.39.941.
Mussell HG, Dure LS, Percy AK, Grabb PS. Bobble-head doll syndrome: report of a case and review of the literature. Mov Disord. 1997;12(5):810–4. https://doi.org/10.1002/mds.870120534.
Nadkarni TD, Menon RK, Shah AH, Goel A. Chudley McCullough syndrome. Childs Nerv Syst. 2008;24(5):541–4. https://doi.org/10.1007/s00381-007-0518-z. Epub 2007 Oct 26
Najjar MW, Baeesa SS, Lingawi SS. Idiopathic spinal cord herniation: a new theory of pathogenesis. Surg Neurol. 2004;62(2):161–70; discussion 170–1. https://doi.org/10.1016/j.surneu.2003.10.030.
Ninds.nih.gov. 2021. Arachnoid Cysts Information Page|National Institute of Neurological Disorders and Stroke. Available at: https://www.ninds.nih.gov/Disorders/All-Disorders/Arachnoid-Cysts-Information-Page. Accessed 20 November 2021.
NORD (National Organization for Rare Disorders). 2021. KAT6A Syndrome—NORD (National Organization for Rare Disorders). Available at: https://rarediseases.org/rare-diseases/kat6a-syndrome/#:~:text=The%20KAT6A%20gene%20contains%20instructions,a%20type%20of%20histone%20acetyltransferase. Accessed 20 November 2021.
Odent S, Le Marec B, Toutain A, David A, Vigneron J, Tréguier C, Jouan H, Milon J, Fryns JP, Verloes A. Central nervous system malformations and early end-stage renal disease in oro-facio-digital syndrome type I: a review. Am J Med Genet. 1998;75(4):389–94.
Ogura Y, Miyake N, Kou I, Iida A, Nakajima M, Takeda K, Fujibayashi S, Shiina M, Okada E, Toyama Y, Iwanami A, Ishii K, Ogata K, Asahara H, Matsumoto N, Nakamura M, Matsumoto M, Ikegawa S. Identification of HOXD4 mutations in spinal extradural arachnoid cyst. PLoS One. 2015;10(11):e0142126. https://doi.org/10.1371/journal.pone.0142126.
Ohnishi YI, Fujimoto Y, Taniguchi M, Tsuzuki T, Taki T. Neuroendoscopically assisted cyst-cisternal shunting for a quadrigeminal arachnoid cyst causing typical trigeminal neuralgia. Minim Invasive Neurosurg. 2007;50(2):124–7. https://doi.org/10.1055/s-2007-982507.
Omim.org. 2021. OMIM Entry—* 300072—UBIQUITIN-SPECIFIC PROTEASE 9, X-LINKED; USP9X. Available at: https://www.omim.org/entry/300072. Accessed 20 November 2021.
Park SW, Cho KH, Shin YS, Kim SH, Ahn YH, Cho KG, Huh JS, Yoon SH. Helmetlike skull deformity with a large arachnoid cyst. Surg Neurol. 2006;65(1):95–8; discussion 98. https://doi.org/10.1016/j.surneu.2005.03.039.
Peter JC, Fieggen G. Congenital malformations of the brain--a neurosurgical perspective at the close of the twentieth century. Childs Nerv Syst. 1999;15(11–12):635–45. https://doi.org/10.1007/s003810050452.
Pradilla G, Jallo G. Arachnoid cysts: case series and review of the literature. Neurosurg Focus. 2007;22(2):E7. https://doi.org/10.3171/foc.2007.22.2.7.
Price SJ, David KM, O'Donovan DG, Aspoas AR. Arachnoid cyst of the craniocervical junction: case report. Neurosurgery. 2001;49(1):212–5. https://doi.org/10.1097/00006123-200107000-00034.
Qin X, Wang Y, Xu S, Hong X. Familial arachnoid cysts: a review of 35 families. Childs Nerv Syst. 2019;35(4):607–12. https://doi.org/10.1007/s00381-019-04060-z. Epub 2019 Jan 23
Quillo-Olvera J, Quillo-Reséndiz J, Gutiérrez-Partida CF, Rodríguez-García M. Quiste aracnoideo extradural espinal: reporte de un caso y revisión de la literatura [Spinal extradural arachnoid cyst: A case report and review of literature]. Cir Cir. 2017;85(6):544–8. https://doi.org/10.1016/j.circir.2016.09.003. Epub 2016 Oct 14
Renner C, Razeghi S, Uberall MA, Hartmann P, Lehnert W. Clinically asymptomatic glutaric aciduria type I in a 4 5/12-year-old girl with bilateral temporal arachnoid cysts. J Inherit Metab Dis. 1997;20(6):840–1. https://doi.org/10.1023/a:1005348624375.
Robson EA, Dixon L, Causon L, Dawes W, Benenati M, Fassad M, Hirst RA, Kenia P, Moya EF, Patel M, Peckham D, Rutman A, Mitchison HM, Mankad K, O'Callaghan C. Hydrocephalus and diffuse choroid plexus hyperplasia in primary ciliary dyskinesia-related MCIDAS mutation. Neurol Genet. 2020;6(4):e482. https://doi.org/10.1212/NXG.0000000000000482.
Sakellaridis N, Panagopoulos D, Mahera H. Sacral epidural noncommunicating arachnoid cyst. Case report and review of the literature. J Neurosurg Spine. 2007;6(5):473–8. https://doi.org/10.3171/spi.2007.6.5.473.
Serarslan Y, Melek IM, Sangün O, Akçora B, Akdemir G. Macrocephaly and bitemporal arachnoid cysts not associated with glutaric aciduria type I in a child. Turk Neurosurg. 2008;18(2):172–6.
Shekdar K. Posterior fossa malformations. Semin Ultrasound CT MR. 2011;32(3):228–41. https://doi.org/10.1053/j.sult.2011.02.003.
Shields JA, Shields CL, Eagle RC Jr, Arevalo F, De Potter P. Ophthalmic features of the organoid nevus syndrome. Trans Am Ophthalmol Soc. 1996;94:65–86; discussion 86–7. https://doi.org/10.1016/s0002-9394(14)70161-8.
Siddiqui S, Naaz S, Ahmad M, Khan ZA, Wahab S, Rashid BA. Encephalocraniocutaneous lipomatosis: A case report with review of literature. Neuroradiol J. 2017;30(6):578–82. https://doi.org/10.1177/1971400917693638. Epub 2017 Jul 14
Singleton WG, Lawrence T, Green AL, Jeans A, Kerr RS. Cerebellopontine angle arachnoid cyst containing ectopic choroid plexus--case report. Acta Neurochir. 2010;152(5):881–3. https://doi.org/10.1007/s00701-009-0516-x. Epub 2009 Oct 6
Sioutos P, Arbit E, Tsairis P, Gargan R. Spontaneous thoracic spinal cord herniation. A case report. Spine. 1996;21(14):1710–3. https://doi.org/10.1097/00007632-199607150-00019.
Slegers RJ, Blumcke I. Low-grade developmental and epilepsy associated brain tumors: a critical update 2020. Acta Neuropathol Commun. 2020;8(1):27. https://doi.org/10.1186/s40478-020-00904-x.
Society for Maternal-Fetal Medicine (SMFM), Yeaton-Massey A, Monteagudo A. Intracranial cysts. Am J Obstet Gynecol. 2020;223(6):B42–6. https://doi.org/10.1016/j.ajog.2020.08.185. Epub 2020 Nov 7
Sugita K, Niizuma H, Suzuki J, Tsuburaya K. A case of arachnoid cyst in the middle cranial fossa presenting with trigeminal neuralgia. No Shinkei Geka. 1986;14(12):1481–5.
Suzuki H, Takanashi J, Sugita K, Barkovich AJ, Kohno Y. Retrocerebellar arachnoid cysts in siblings with mental retardation and undescended testis. Brain and Development. 2002;24(5):310–3. https://doi.org/10.1016/s0387-7604(02)00061-x.
Sweatman J, Beltechi R. Pneumosinus Dilatans: an exploration into the association between arachnoid cyst, meningioma and the pathogenesis of Pneumosinus Dilatans. Clin Neurol Neurosurg. 2019;185:105462. https://doi.org/10.1016/j.clineuro.2019.105462. Epub 2019 Aug 14
Thotakura AK, Marabathina NR. Acquired Chiari I malformation with syringomyelia secondary to colloid cyst with hydrocephalus-case report and review of literature. World Neurosurg. 2017;108:995.e1–4. https://doi.org/10.1016/j.wneu.2017.09.012. Epub 2017 Sep 9
Topsakal C, Kaplan M, Erol F, Cetin H, Ozercan I. Unusual arachnoid cyst of the quadrigeminal cistern in an adult presenting with apneic spells and normal pressure hydrocephalus--case report. Neurol Med Chir (Tokyo). 2002;42(1):44–50. https://doi.org/10.2176/nmc.42.44.
Tsai FC, Lee HJ, Wang AG, Hsieh SC, Lu YH, Lee MC, Pai JS, Chu TH, Yang CF, Hsu TR, Lai CJ, Tsai MT, Ho PH, Lin MC, Cheng LY, Chuang YC, Niu DM. Experiences during newborn screening for glutaric aciduria type 1: diagnosis, treatment, genotype, phenotype, and outcomes. J Chin Med Assoc. 2017;80(4):253–61. https://doi.org/10.1016/j.jcma.2016.07.006. Epub 2017 Mar 13
Utsunomiya H, Yamashita S, Takano K, Ueda Y, Fujii A. Midline cystic malformations of the brain: imaging diagnosis and classification based on embryologic analysis. Radiat Med. 2006;24(6):471–81. https://doi.org/10.1007/s11604-006-0049-7.
Vallée B, Mercier P, Menei P, Bouhour F, Fischer C, Fournier D, Bougeard R, Diabira S, Mahla K. Ventral transdural herniation of the thoracic spinal cord: surgical treatment in four cases and review of literature. Acta Neurochir. 1999;141(9):907–13. https://doi.org/10.1007/s007010050396.
van der Watt G, Owen EP, Berman P, Meldau S, Watermeyer N, Olpin SE, Manning NJ, Baumgarten I, Leisegang F, Henderson H. Glutaric aciduria type 1 in South Africa-high incidence of glutaryl-CoA dehydrogenase deficiency in black south Africans. Mol Genet Metab. 2010;101(2-3):178–82. https://doi.org/10.1016/j.ymgme.2010.07.018. Epub 2010 Aug 3
Verghese J, Mahore A, Goel A. Arachnoid cyst associated with painful tic convulsif. J Clin Neurosci. 2012;19(5):763–4. https://doi.org/10.1016/j.jocn.2011.07.039. Epub 2012 Feb 8
Visagan R, Wright D, Jayamohan J. Trigeminal neuralgia in a paediatric patient caused by arachnoid cyst. Br J Neurosurg. 2015;29(1):103–4. https://doi.org/10.3109/02688697.2014.957161. Epub 2014 Sep 15
Wang Y, Cui J, Qin X, Hong X. Familial intracranial arachnoid cysts with a missense mutation (c.2576C > T) in RERE: A case report. Medicine (Baltimore). 2018;97(50):e13665. https://doi.org/10.1097/MD.0000000000013665.
Database G. 2022. RTTN Gene - GeneCards | RTTN Protein|RTTN Antibody. Genecards.org. Available at: https://www.genecards.org/cgi-bin/carddisp.pl?gene=RTTN#:~:text=UniProtKB%2FSwiss%2DProt%20Summary%20for,of%20NODAL%2C%20LEFTY%20and%20PITX2. Accessed 1 September 2022.
Westermaier T, Vince GH, Meinhardt M, Monoranu C, Roosen K, Matthies C. Arachnoid cysts of the fourth ventricle - short illustrated review. Acta Neurochir. 2010;152(1):119–24. https://doi.org/10.1007/s00701-009-0309-2. Epub 2009 Apr 23
Wiese JA, Gentry LR, Menezes AH. Bobble-head doll syndrome: review of the pathophysiology and CSF dynamics. Pediatr Neurol. 1985;1(6):361–6. https://doi.org/10.1016/0887-8994(85)90073-6.
Wu X, Li G, Zhao J, Zhu X, Zhang Y, Hou K. Arachnoid cyst–associated chronic subdural hematoma: report of 14 cases and a systematic literature review. World Neurosurg. 2018;109:e118–30.
Yeaton-Massey A, Monteagudo A. Intracranial cysts. Am J Obstet Gynecol. 2020;223(6):B42–6.
Youssef A, D'Antonio F, Khalil A, Papageorghiou A, Ciardulli A, Lanzone A, Rizzo G, Thilaganathan B, Pilu G. Outcome of fetuses with supratentorial extra-axial intracranial cysts: A systematic review. Fetal Diagn Ther. 2016;40(1):1–12.
Yüksel D, Yilmaz D, Usak E, Senbil N, Gürer Y. Arachnoid cyst and costovertebral defects in Aicardi syndrome. J Paediatr Child Health. 2009;45(6):391–2. https://doi.org/10.1111/j.1440-1754.2009.01520.x.
Zakaria J, Wemhoff M, Anderson D. Microvascular decompression and arachnoid cyst fenestration for treatment of medulla oblongata compression caused by arachnoid cyst-vascular loop complex. World Neurosurg. 2018;113:293–5. https://doi.org/10.1016/j.wneu.2018.02.104. Epub 2018 Feb 25
Zarate YA, Boccuto L, Srikanth S, Pauly R, Ocal E, Balmakund T, Hinkle K, Stefans V, Schaefer GB, Collins RT 2nd. Constitutive activation of the PI3K-AKT pathway and cardiovascular abnormalities in an individual with Kosaki overgrowth syndrome. Am J Med Genet A. 2019;179(6):1047–52. https://doi.org/10.1002/ajmg.a.61145. Epub 2019 Apr 2
Zhang N, Qi Z, Zhang X, Zhong F, Yao H, Xu X, Liu J, Huang Y. Dandy-Walker syndrome associated with syringomyelia in an adult: a case report and literature review. J Int Med Res. 2019;47(4):1771–7. https://doi.org/10.1177/0300060518808961. Epub 2019 Feb 24
Zieliński G, Podgórski JK, Koziarski A, Potakiewicz Z. Sródsiodłowa torbiel pajeczynówki. Opis przypadku i przeglad piśmiennictwa [Intrasellar arachnoid cyst. A case report and review of the literature]. Neurol Neurochir Pol. 2006;40(4):347–52; discussion 353
Zubairi MS, Carter RF, Ronen GM. A male phenotype with Aicardi syndrome. J Child Neurol. 2009;24(2):204–7. https://doi.org/10.1177/0883073808322337.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2023 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Randeni, A., Colvin, S., Krishnamurthy, S. (2023). Genetics of Arachnoid Cysts. In: Turgut, M., Akhaddar, A., Turgut, A.T., Hall, W.A. (eds) Arachnoid Cysts. Springer, Cham. https://doi.org/10.1007/978-3-031-22701-1_8
Download citation
DOI: https://doi.org/10.1007/978-3-031-22701-1_8
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-22700-4
Online ISBN: 978-3-031-22701-1
eBook Packages: MedicineMedicine (R0)