Abstract
Imaging for arachnoid cysts (ACs) after surgery focuses on assessing for changes in cyst volume. Changes in volume are traditionally considered a marker of surgical success. This chapter provides an overview of relevant literature demonstrating that cysto-peritoneal shunting may provide a greater degree of cyst volume reduction than fenestration. However, multiple studies have demonstrated poor correlation between volume change and symptom improvement. The chapter will also discuss the timing of volume change post-operatively in cases of symptomatic ACs.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
The majority of arachnoid cysts (ACs) are found incidentally and do not require surgical intervention. Surgical intervention is reserved for cysts which are causing symptoms due to mass effect or growing on surveillance imaging. It is expected that following surgical intervention the cyst will reduce in size and the brain expands to fill some, or all, of the space occupied by the AC. The change in the brain shape is referred to as brain plasticity. This chapter will explore how surgical intervention changes the cyst size, subsequent brain plasticity and what implications this has for patient outcomes.
2 Brain Compliance
Brain plasticity and the change in cyst volume are governed by the principles of compliance. Compliance is the tendency of a structure to change volume dependent on the change in pressure exerted against it. Elastance/stiffness is the inverse of compliance:
Although ACs are congenital, those that undergo surgery are likely symptomatic and thus growing. Growth occurs as intra-cystic pressure puts increased stress on the brain parenchyma, thus deforming it. When the intra-cystic pressure is reduced, following surgery, a new pressure gradient is generated across the cyst wall. The absolute value of pre-operative intra-cystic pressure does not relate to the degree of post-operative volume change [19]; thus variations in brain compliance likely determine the degree of post-operative brain expansion following the reduction of intra-cystic pressure.
Brain parenchyma is modelled as viscoelastic, and its stiffness is measured using the complex (dynamic) shear modulus. Complex shear modulus increases with age [34] and myelination [6] and varies within the brain. For example, the cerebellum is softer than the cerebrum [6]. Unlike elastic materials which do not lose energy when deformed (and thus demonstrate complete return to original size when stress is released), viscoelastic materials lose energy due to molecule reorganisation and thus display plastic deformation even if the stress is within the elastic limit (maximum degree of deformation before effect becomes permanent). These principles have been demonstrated based on short-term deformations, over seconds, and how they apply to the relaxation of the brain which has been deformed over weeks, months or even years is not known. The brain is far more complex than a simple polymer and exists in a dynamic environment; however, its viscoelastic nature may limit how much it will return to its original size.
3 How to Measure Cyst Volume
There are a number of techniques which can be used to measure AC volume depending on the imaging technology available. Techniques differ in their accuracy, skillset required to calculate and time requirement.
3.1 The MacDonald Method
The MacDonald method was initially described to measure tumour volumes using simple measures on cross-sectional imaging [10]. However, it is also translatable to measuring volumes of ACs [39, 40]. The modified MacDonald method uses linear measurements on cross-sectional imaging and takes the largest diameters of the cyst in cross section (named d1 and d2), the number of slices the cyst appears on (s) and the thickness of the slices (t). It is very similar to the better-known ABC/2 method with subtle differences generated by the incorporation of π. It does not require additional computational input beyond linear measurements on source images and is quick to calculate:
3.2 Volumetric Segmentation
Segmentation is the process of building a 3D model of a structure based on its boundaries as shown on radiological imaging such as CT or MRI. Many good descriptions on the science of volume segmentation have already been published [38], and further detail is beyond the scope of this chapter. There are a number of computer programmes available for clinicians which utilise DICOM data and simplify the process to produce a final volume. While previous work by the authors used the open-source 3D Slicer [16], there is no evidence that any one program is superior.
Choosing which imaging sequence to use for building a segmentation model will depend on the cyst anatomy. For example, large convexity cysts have boundaries that are easily visualised on any type of cross-sectional imaging and all MRI sequences. However small cysts in regions with multiple arachnoid layers (e.g. suprasellar cysts) require more sensitive MRI sequences such as a fine slice constructive interference in steady state (CISS) to best delineate the cyst margins. The slice thickness can influence model accuracy as the top and bottom boundaries of the cyst will lie between slices. The greater the slice thickness, the more cyst will be missed as the true boundary is further from the last slice on which the cyst is visible. This is illustrated in Fig. 1 with a theoretical spherical cyst with 50-mm diameter and assumes a slice thickness of 5 mm which demonstrates a potential 2% error for each end of the sphere. If the cyst is smaller and all other parameters are the same, then this error will be greater.
Defining volume boundaries is done either manually by tracing the outline on the imported imaging and repeating this for all the imaging slices for the object in question or automatically using the software’s algorithms based on the contrast against surrounding structures. Once a 3D model has been built, the segmented volumes require surface smoothing and hole filling to generate a final volume.
3.3 Method Comparison
With the easy access of the necessary computer programmes, segmentation models are now the gold standard method for measuring cyst volume. Segmentation allows more accurate measurement, particularly of irregular shapes, than the MacDonald method. A study by Tamimi et al. [39] using a mixed cohort of locations and ages found that volumetric segmentation models generated a larger cyst volume than the modified MacDonald method. However, the percentage volume change between pre- and post-operative scans was the same for both approaches. Neither method better correlated with symptom improvement. There is no consensus of whether automated or manual methods for defining the volume perimeter are more accurate, and it is likely that any differences are not clinically significant.
3.4 Classification of Post-Operative Radiological Outcomes
Once the cyst volume has been calculated pre- and post-operatively, it is possible to assign radiological outcomes based on the percentage of improvement. A volume reduction dichotomised to >50% or <50% is most commonly used in the literature to demonstrate surgical success. Helland et al. have expanded this to describe a simple 1–4 scoring system ranging from complete cyst disappearance (NOG1), >50% reduction (NOG2) and <50% reduction (NOG3) to no change (NOG4) [17]. How well these classifications actually relate to clinical outcome will be described below.
4 Influence of Surgical Modality on Brain Plasticity
As already well described, there are three broad categories for surgical intervention to treat an AC. These are endoscopic fenestration, microsurgical fenestration/marsupialisation and cysto-peritoneal shunting. Choosing between approaches is based on cyst location and surgeon preference and will not be discussed here nor will the clinical outcomes; however we will consider the effect of surgical approach on post-operative cyst volume change.
4.1 Endoscopic Series
4.1.1 Sylvian Fissure Cysts
The Sylvian fissure AC is the most common location, and its adjacence to the basal cisterns makes it ideal to be treated by fenestration. Over the last 30 years as endoscopic technology has improved, there has been a shift towards performing these fenestrations endoscopically.
Li et al. [25] used volumetric segmentation for their 28 patients and found average pre-operative volume of 135 cm3 which reduced to 93 cm3 at 4-month follow-up of which 21% of patients did not change their volume at all. The series from Couvreur et al. [8] reported that 91% of patients with a Sylvian cyst treated endoscopically saw at least a 10% cyst volume reduction afterwards. This was further itemised by Galassi classification with 100% of Galassi 1 and 88% of Galassi 3 cysts reaching the threshold of 10% reduction. Gui et al. [15] found that 16% of Sylvian cysts radiologically fully resolved, 60% showed partial reduction and 24% did not change in volume. Okano et al. [30] found similar results with 11% disappearing completely and the remainder showing partial resolution.
Notwithstanding the different reporting measures for radiological outcomes, all series of Sylvian cysts report up to 20% of patients showing no improvement with approximately 10–20% seeing full resolution.
4.1.2 Suprasellar Cysts
Suprasellar cysts are naturally much smaller than those in the Sylvian fissure, and thus the absolute volume reduction is not comparable. Given that they are less common, there are fewer series published on their radiological outcomes compared to the Sylvian location. A useful classification scheme from Paris combines an anatomical origin of these cysts with clinical and radiological features [5].
Gangemi et al. [13] published a series of five suprasellar cysts managed endoscopically using a mixture of ventriculo-cystostomy and ventriculo-cysto-cisternostomy (VCC). They found an average volume reduction of 34% including one patient whose cyst was unchanged. Ma et al. [26] presented a larger series of 23 patients treated predominantly with VCC and found a 68% average volume reduction, double that seen by Gangemi et al. The high pre-operative volume (mean 39 cm3) in Ma et al. may have resulted in large volume changes. Rizk et al. [33] only had six patients but started with an even higher mean of 153 cm3 and achieved a 75% volume reduction. Lastly, Maher and Goumnerova [27] treated 11 patients using VCC but did not use volumetrics for comparison although they did find that 73% of cysts fully resolved and only one did not change at all.
4.2 Open Series
Open microsurgical techniques depend on the cyst location and proximity to a CSF space, and the options include fenestration into a cistern or ventricle or marsupialisation (remove the parietal cyst membrane) or both.
The Helland and Wester group presented a series of 45 patients [21] treated with craniotomy, parietal cyst wall resection and cistern fenestration, all of which were Sylvian in location. Using their NOG outcome classification, 55% of their patients achieved a 50% reduction in cyst volume or better, and only 4% had no change in cyst volume.
The series of 20 patients by Tamimi et al. [39] contained an assortment of locations and patient ages treated with fenestration and cyst wall removal. Eighty-five percent of the series had a Sylvian/fronto-temporo-parietal cyst making it loosely comparable to Helland and Wester, and they achieved an overall reduction in cyst volume from 111 cm3 to 34 cm3 (70% reduction). Only two patients had a reduction of less than 10%. Unfortunately, because they report outcomes using different measures, it isn’t possible to make further comparisons between these two purely open series.
4.3 Cysto-peritoneal Shunt Series
The large series by Zhang et al. [43] of primary cysto-peritoneal shunting in children reports that only 5% of cysts did not reduce in volume. This is comparable to the two open series described above. Unfortunately, Zhang et al. did not include further details on cyst volumes or percent (%) volume reduction which are required to further compare this series to volume reduction in other treatment methods [43].
4.4 Series Comparing Surgical Modalities
Our series contained 56 patients treated with any of the three modalities [16]. The overall cyst volume change ranged from 30 to 40% for each technique which is more modest than some of the open series described above. Even when we focused on the subgroup with Sylvian cysts, both the endoscopic and microsurgical groups only achieved 25–30% volume reduction which is much lower than the 70% reported by Tamimi et al. [39]. Our clinical outcomes were still comparable despite the lower volume reduction as will be discussed further below.
Amelot et al. [4] published a large series of patients with Sylvian ACs with an average pre-operative volume of 107 cm3 which matches Tamimi et al. [39] above. However, they also found lower volume reduction than Tamimi et al. ranging from 45 to 60%. Amelot et al. confirmed our results that there is little difference in radiological outcome between endoscopic and microsurgical procedures. Amelot et al. were able to better compare CP shunts and demonstrated that cyst volume reduction was greater (60%) than the other techniques albeit not significantly so.
The trend of greater volume reduction following CP shunting has been repeated in several other studies comparing the three treatment modalities. Kandenwein et al. [22] compared open fenestration (+ cyst wall resection in one third) to cysto-peritoneal shunting and found a higher volume reduction in shunts than with open fenestration (74% vs. 58%). Shim et al. [36] measured how many patients achieved >50% cyst volume reduction and found this threshold was reached in 100% of CP shunt, 92% of open procedures and only 75% of endoscopic fenestrations. Lastly, a systematic review of AC treatment in patients over 60 years old [28] reported using the Helland and Wester classification found that 85–88% of patients treated with cysto-peritoneal shunting or cyst wall resection achieved at least >50% volume reduction, but this was only achieved by 68% of patients treated with fenestration (endoscopic or microsurgical). This last paper is slightly marred by the grouping of microsurgical and endoscopic fenestrations together but does raise the suggestion that cyst wall removal may provide superior radiological results compared to fenestration alone.
Chen et al. [7] published a meta-analysis of treatment methods for Sylvian ACs. They report on the rate of cyst reduction and found that 93% of cysts treated with CP shunts reduce in size compared to 87% managed with craniotomy and 76% managed with endoscopy.
Comparing the cyst volume reduction across surgical modalities is inherently limited due to the heterogeneity of the groups. The current evidence is limited to small-volume single-centre series and a single meta-analysis on Sylvian cysts. The mixture of ages and cyst locations as well as different measures for radiological success makes it difficult to make direct comparison between techniques. It also does not recognise that clinical success in different locations, e.g. suprasellar or posterior fossa, may be achieved with smaller cyst volume changes and the technique offering the highest change of cyst obliteration may not be necessary.
Similar measurements of the ventricular system after successful endoscopic third ventriculostomy [37] showed that the degree of volume reduction correlated with the initial size (larger ventricles showed smaller reduction) and the chronicity of the symptoms (longer duration had smaller reduction). In addition, the ventricular size even after some reduction and clinical improvement remained supernormal and stabilized between 3 and 6 months. In contrast, measurements in hydrocephalic patients treated with VP shunts showed more obvious volume reductions and a tendency to stabilise between 6 and 12 months [42].
5 Correlation of Symptomatology to Cyst Volume Reduction
The primary aim of surgical intervention for the large or growing AC is to improve the symptoms experienced by the patient. The symptoms vary by cyst location but can include headaches, focal neurology, seizures, papilledema and reduced level of consciousness. In order to manage surgical goals and patient expectations, it is important to understand how radiological outcomes relate to clinical outcomes and thus what degree of brain plasticity and cyst reduction constitute a surgical success.
In our own series of 56 patients [16] with symptomatic ACs treated by either endoscopic, microsurgical or shunting techniques, we dichotomised patients based on volume reduction of greater or less than 50%. We found that the percentage of patients with symptom improvement or resolution was approximately 90% in both groups. Galarza et al. [12] found similar results with 100% of patients symptom-free after surgery despite two thirds of patients having <50% reduction in cyst volume. This was true for both fenestration and shunting procedures. Other case series [3, 8, 14, 24] report no correlation between radiological and clinical outcomes without providing specific data.
Contrary to the above series, Kandenwein et al. found that the amount of cyst resolution weakly correlated with the degree of clinical improvement (r = 0.34, p = 0.035). Although when dichotomising cyst volume reduction >50% and <50% as the series above, despite a clear trend favouring more good outcomes in the >50% reduction group, there was no significant difference. Unlike the series above which group all degrees of partial improvement together, Kandenwein’s assessment of clinical improvement divided partial improvement into slight and significant. Thus, patients with only slight improvement may be diluting the treatment effect of larger volume reductions in other series.
Tamimi et al. [39] analysed a cohort of mixed cyst location in adults and paediatric patients treated by microsurgical fenestration. They grouped patients in the opposite manner by either complete or partial resolution of symptoms and found no difference in the percentage reduction in cyst volume in either group (49 vs. 60%).
The work by Helland and Wester further confirms the lack of correlation between size reduction and clinical outcomes in adults [18]. They found that 85% of patients had symptom reduction/resolution in both the groups with >50% and <50% cyst volume reduction. However, in their series on paediatric ACs, they did find a significant association between clinical and radiological outcomes [17]. Whether or not a paediatric subgroup of patients demonstrate better correlation between brain re-expansion and cyst volume reduction than adults is difficult to confirm as other paediatric cohorts have found no correlation [32].
The above studies measured clinical outcome using change in symptoms; however Mørkve et al. [29] prospectively included quality-of-life metrics (SF-36 and Glasgow Benefit Inventory) in addition to clinical symptoms. While they confirmed that improvement of symptoms including headache and dizziness improved quality of life, the degree of reduction in cyst volume was not associated with improved quality of life. Using a maze learning test around the hospital corridors, the Wester group demonstrated that in a cohort of mixed ages and cyst locations, the post-operative group performed better in maze learning, compared to pre-operatively, which correlated with symptom improvement but not with the degree of cyst volume reduction [21].
Karabagli and Etus [23] found that despite a clinical success rate of 90% only 55% of patients showed a reduction in cyst volume. However more than three quarters of patients had radiological evidence of a patent fenestration which suggests that cyst communication and thus intra-cystic pressure reduction are more important than cyst volume.
In conclusion, the evidence on whether clinical symptom improvement correlates with the percentage of cyst size reduction is limited to single-centre case series. The majority of these series report improvement following surgery but do not show a relationship between symptom improvement and cyst volume change. However, these series are often a mixture of ages and locations and contain low numbers; thus it remains possible that in certain subgroups a correlation does exist.
6 Temporal Pattern of Cyst Volume Reduction
It is expected that cyst volumes will reduce following surgery, but over what time period does this occur? Understanding this will help with patient counselling and planning routine post-operative imaging. Most surgical series describe a single point of follow-up, usually at the latest time point available, which misses how the cyst changes over time.
The series by Rabiei et al. [32] on paediatric cysts provides good long-term follow-up. They imaged patients at 3 and 12 months and found a significant different between pre-operative and 3 months, but no significant difference in cyst volumes between 3 and 12 months.
Schulz et al. [35] followed a paediatric series with mixed locations and treatment types for a median of 26 months. The short-term post-operative radiological follow-up (2–4 months) showed significantly smaller cyst volumes compared to pre-operatively, but no further significant reduction was seen at long-term follow-up (16–34 months). Lastly, Pitsika and Sgouros [31] published a small cohort of four patients which further confirms this picture whereby most of the improvement occurs in the first 3–6 months and then no/minimal change up to 48 months.
The similar results of these series show that all significant post-operative changes occur within the first few months (up to 6 months). Unfortunately, both of these series include a mixture of open and endoscopic techniques, and thus any differences due to surgical approach are not seen. Furthermore, neither series included CP shunting which instinctively is likely to cause even more rapid drainage of the cyst contents.
7 Brain Plasticity in Adults Compared to Children
Children and adults have different brain compliance depending on their age. Older people are known to have decreased brain compliance [9] and thus a decreased change in volume per unit of pressure. This affects brain plasticity when the intra-cystic pressure is released and thus the final volume of the cyst following surgery.
Making comparisons of volume reduction based on age is challenging because the recent literature is heavily weighted towards reporting paediatric rather than adult series. Furthermore, different methods of reporting, i.e. absolute volumes versus classifications, make it difficult to directly compare outcomes across the series. In order to make some comparisons based on age, we will focus on discussing the Sylvian cyst, as the archetypical location, in order to remove cyst location as a confounder.
The series by Helland et al. [17] reported just over half of their paediatric temporal cysts were no longer visible on follow-up imaging and a further 21% were reduced to between 0 and 50% giving an overall rate of 75% experiencing at least 50% size reduction. By comparison their adult series [20] demonstrated lower extents of volume whereby only 28% were completely obliterated and a further 32% showed at least 50% reduction meaning only 60% of their patients achieved at least 50% reduction.
The results from the adult series by Wang et al. [41] do not split partial resolution into > or <50% and so are difficult to compare to Helland et al. [20]. However, their rate of complete cyst resolution (12%) is less than half that reported by Helland. Notably both of these adult series treated >80% of their Sylvian cysts via craniotomy and the remainder with shunts (cysto-subdural in Helland et al. or cysto-peritoneal in Wang et al.) so how comparable these findings are to modern practice which favours endoscopic fenestration and how much the differences in radiological outcome are due to the different shunt procedure are unknown.
Karabagli and Etus [23] reported only 50% of paediatric patients had any cyst volume reduction which is much lower than Helland et al. Among other paediatric series, the pre-operative volume of a Sylvian AC ranges from 65 to 230 cm3 which reduced to 15–119 cm3 following surgery with an average volume reduction of 45–61% [4, 31, 32, 35]. These figures include treatment through either endoscopic or microsurgical techniques.
Given that Karabagli and Etus [23] found 50% of paediatric cysts did not improve and Schulz et al. [35] found that 22% of patients had <10% improvement (akin to no improvement), the results from El-Ghandour [11] suggest that infant patients may be a distinct subgroup with regard to radiological outcomes. El-Ghandour found that only 6% of infants with middle fossa cysts did not show radiological improvement following endoscopic fenestration. Why infants show favourable radiological outcomes compared to other children has not been discussed, but potential mechanisms may include differing compliance of the unmyelinated brain or different CSF hydrodynamics that change with age.
The work by Tamimi et al. [39] comparing the modified MacDonald method to 3D segmentation for measuring volumes includes volume changes in adults and children for direct comparison. The series had a mixture of locations with 55% being Sylvian; however the spread of locations was comparable between age groups. Children exhibited approximately 20% greater reduction in cyst volume post-operatively compared to adults when measured with 3D volumetric models. Of note, the opposite results were found using the modified MacDonald method; however 3D segmentation is regarded as more accurate. This result is consistent with the work by Helland et al. above.
Li et al. [25] provide a further direct comparison between adults and children using 3D segmentation models in their series of Sylvian cysts. They found a statistically significant difference in the ages of patients whose cyst volumes reduced compared to those that remained unchanged (4.5 vs. 19 years).
8 Illustrative Cases
The following cases demonstrate some of the findings discussed above. All segmentation models have been generated by the authors using Brainlab (Munich, Germany).
8.1 Case 1: Sylvian Fissure
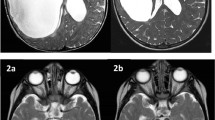
A 4-year-old female presented through the emergency department with a 10-day history of progressive headaches and vomiting following a minor head injury. She had not previously suffered with headaches nor any other neurological symptoms. She had no past medical history. On examination she was GCS 15/15 with no focal neurological deficit. She underwent CT scan in her local hospital which demonstrated a left Sylvian AC with hygroma and 5 mm of midline shift which was later confirmed with MRI. The pre-operative T2 MRI (Fig. 2a) demonstrates the membranous boundary between the AC and the subdural space which can be further identified by the vessels which run in the outer, parietal cyst membrane but do not transverse the subdural space (Fig. 2b). Segmentation models show that the cyst volume is 74 cm3, and the ipsilateral hygroma is 202 cm3 (Fig. 3).
The patient underwent endoscopic fenestration with a left temporal burr hole followed by fenestrations through the cyst wall into the optico-carotid and carotid oculo-motor triangle. Post-operatively the patient made a full recovery. Their post-operative MRI scan at 3 months (Fig. 2c) shows the cyst now measures 15 cm3 (80% reduction) and the midline shift has resolved, but the subdural hygroma has not changed at 202 cm3 (Fig. 3).
The patient likely started with a very large Galassi type 3 cyst which ruptured into the subdural space following trauma. The cyst itself is well decompressed as a result of a patent fenestration with some visible brain plasticity, notably the frontal operculum, and an objectively reduced cyst volume. Interestingly the hygroma remains unchanged as the severely deformed brain is unable to expand enough to fill the void likely due to the long-standing nature of the compression. The presence of a hygroma is clinically insignificant though the patient is asymptomatic, and over the following years, the brain may expand further.
8.2 Case 2: Convexity AC
A male patient was born at term with an ante-natal diagnosis of a convexity AC. On examination he had macrocrania with a head circumference on the 99.6th centile but no other neurological deficit. He underwent MRI scan on day 2 of life (Fig. 4) which demonstrated a large convexity AC. Segmentation confirms the volume at 235 cm3. Of note an ante-natal MRI scan 1 week prior to birth had a cyst volume of 201 cm3.
The cyst wall extended to the quadrigeminal cistern which presents a potential site of fenestration. However, given the patient’s young age and the high-risk anatomy in the quadrigeminal cistern, it was decided he should undergo a cysto-peritoneal shunt which was completed without incident on day 4. A post-operative MRI scan (Fig. 5) 1 month following surgery demonstrated complete obliteration of the cyst with a thin hygroma. He required no further surgical intervention and at 2 years of follow-up was developing normally, and his head circumference stabilised at the 91st centile.
This case demonstrates both the validity of minimally invasive approaches and the plasticity of the paediatric brain. While it is appealing to fenestrate the cyst because it is a definitive treatment option and avoids the risk of shunt dependency, very good results are achievable with CP shunts. In this case the cyst rapidly emptied allowing full re-expansion of the brain. In the young, unmyelinated brain, there is little pressure differential across the stoma because the brain lacks stiffness to push against the cyst, whereas a shunt generates a much greater pressure differential between the intra-cystic and intra-abdominal compartments.
8.3 Case 3: Suprasellar AC
This 8-year-old girl is known to the neurosurgical department for undergoing a ventriculo-peritoneal shunt at 1 year of age to treat post-traumatic hydrocephalus. A routine MRI at 2 years of age demonstrated a suprasellar arachnoid cyst measuring 2.7 cm3. This was managed conservatively with a repeat MRI at 8 years showing the cyst had grown to 3.7 cm3 (Fig. 6a) and was now distorting the pituitary stalk and optic chiasm. Due to the concern of future endocrine and/or visual disturbance, she underwent an endoscopic ventriculo-cystostomy. Fenestration into the cistern was not possible due to thickened opaque arachnoid membranes which were not easily divided nor could vasculature be visualised. A post-operative MRI at 2 months (Fig. 6b) demonstrated the cyst volume had now reduced to 2.8 cm3 (21% reduction) and the bowing of the pituitary stalk and optic tracts had reduced. Their post-operative course was uneventful, and they remain asymptomatic.
This case demonstrates the importance of the correct MRI sequences when dealing with small cysts in the suprasellar region. Being able to define the membranes is crucial in order to accurately measure the cyst volume especially when volumes are small and thus more susceptible to errors. It also demonstrates that cysts in some locations do not need a large volume change in order to achieve a clinically successful surgery.
9 Proposed Algorithm for the Follow-Up of Untreated Arachnoid Cysts
10 Conclusion
There is a significant literature reporting radiological outcomes after AC surgery. However, it is difficult to draw any conclusions on the cyst volume reduction following surgery due to the heterogeneity in outcome reporting. Ideally future series will present volumetric data in order to allow comparison between studies. A number of trends are noted in the studies discussed above. Firstly, cyst volume reduction following surgery does not correlate with clinical improvement. Secondly, the greatest change in cyst volume following surgery is seen in the first 6 months, with minimal reduction in volume seen beyond this time point. Finally, brain plasticity/cyst volume changes reduce as the patient ages. The primary role of post-operative imaging may therefore be to obtain a new baseline cyst volume to monitor for re-growth rather than as a marker of treatment success.
References
Al-Holou WN, Yew AY, Boomsaad ZE, Garton HJ, Muraszko KM, Maher CO. Prevalence and natural history of arachnoid cysts in children. J Neurosurg Pediatr. 2010;5(6):578–85.
Al-Holou WN, Terman S, Kilburg C, Garton HJ, Muraszko KM, Maher CO. Prevalence and natural history of arachnoid cysts in adults. J Neurosurg. 2013;118(2):222–31.
Ali M, Bennardo M, Almenawer SA, Zagzoog N, Smith AA, Dao D, et al. Exploring predictors of surgery and comparing operative treatment approaches for pediatric intracranial arachnoid cysts: a case series of 83 patients. J Neurosurg Pediatr. 2015;16(3):275–82.
Amelot A, Beccaria K, Blauwblomme T, Bourgeois M, Paternoster G, Cuny ML, et al. Microsurgical, endoscopic, and shunt management of pediatric temporosylvian arachnoid cysts: a comparative study. J Neurosurg Pediatr. 2019;23(6):749–57.
André A, Zérah M, Roujeau T, Brunelle F, Blauwblomme T, Puget S, et al. Suprasellar arachnoid cysts: toward a new simple classification based on prognosis and treatment modality. Neurosurgery. 2016;78(3):370–9; discussion 9-80.
Budday S, Ovaert TC, Holzapfel GA, Steinmann P, Kuhl E. Fifty shades of brain: a review on the mechanical testing and modeling of brain tissue. Arch Comput Methods Eng. 2020;27(4):1187–230.
Chen Y, Fang HJ, Li ZF, Yu SY, Li CZ, Wu ZB, et al. Treatment of middle cranial fossa arachnoid cysts: a systematic review and meta-analysis. World Neurosurg. 2016;92:480–90.e2.
Couvreur T, Hallaert G, Van Der Heggen T, Baert E, Dewaele F, Kalala Okito JP, et al. Endoscopic treatment of temporal arachnoid cysts in 34 patients. World Neurosurg. 2015;84(3):734–40.
Czosnyka M, Czosnyka ZH, Whitfield PC, Donovan T, Pickard JD. Age dependence of cerebrospinal pressure-volume compensation in patients with hydrocephalus. J Neurosurg. 2001;94(3):482–6.
Dang M, Modi J, Roberts M, Chan C, Mitchell JR. Validation study of a fast, accurate, and precise brain tumor volume measurement. Comput Methods Prog Biomed. 2013;111(2):480–7.
El-Ghandour NMF. Endoscopic treatment of intracranial cysts in infants: personal experience and review of literature. Childs Nerv Syst. 2021;37(11):3447–53.
Galarza M, Pomata HB, Pueyrredón F, Bartuluchi M, Zuccaro GN, Monges JA. Symptomatic supratentorial arachnoid cysts in children. Pediatr Neurol. 2002;27(3):180–5.
Gangemi M, Colella G, Magro F, Maiuri F. Suprasellar arachnoid cysts: endoscopy versus microsurgical cyst excision and shunting. Br J Neurosurg. 2007;21(3):276–80.
Gangemi M, Seneca V, Colella G, Cioffi V, Imperato A, Maiuri F. Endoscopy versus microsurgical cyst excision and shunting for treating intracranial arachnoid cysts. J Neurosurg Pediatr. 2011;8(2):158–64.
Gui S, Bai J, Wang X, Zong X, Li C, Cao L, et al. Assessment of endoscopic treatment for quadrigeminal cistern arachnoid cysts: a 7-year experience with 28 cases. Childs Nerv Syst. 2016;32(4):647–54.
Hall S, Smedley A, Rae S, Mathad N, Waters R, Chakraborty A, et al. Clinical and radiological outcomes following surgical treatment for intra-cranial arachnoid cysts. Clin Neurol Neurosurg. 2019;177:42–6.
Helland CA, Wester K. A population-based study of intracranial arachnoid cysts: clinical and neuroimaging outcomes following surgical cyst decompression in children. J Neurosurg. 2006;105(5 Suppl):385–90.
Helland CA, Wester K. Arachnoid cysts in adults: long-term follow-up of patients treated with internal shunts to the subdural compartment. Surg Neurol. 2006;66(1):56–61; discussion.
Helland CA, Wester K. Intracystic pressure in patients with temporal arachnoid cysts: a prospective study of preoperative complaints and postoperative outcome. J Neurol Neurosurg Psychiatry. 2007;78(6):620–3.
Helland CA, Wester K. A population based study of intracranial arachnoid cysts: clinical and neuroimaging outcomes following surgical cyst decompression in adults. J Neurol Neurosurg Psychiatry. 2007;78(10):1129–35.
Isaksen E, Leet TH, Helland CA, Wester K. Maze learning in patients with intracranial arachnoid cysts. Acta Neurochir. 2013;155(5):841–8. discussion 8.
Kandenwein JA, Richter HP, Börm W. Surgical therapy of symptomatic arachnoid cysts - an outcome analysis. Acta Neurochir. 2004;146(12):1317–22; discussion 22.
Karabagli H, Etus V. Success of pure neuroendoscopic technique in the treatment of Sylvian arachnoid cysts in children. Childs Nerv Syst. 2012;28(3):445–52.
Khan IS, Sonig A, Thakur JD, Nanda A. Surgical management of intracranial arachnoid cysts: clinical and radiological outcome. Turk Neurosurg. 2013;23(2):138–43.
Li Y, Chen X, Xu B. The efficacy of neuroendoscopic treatment for middle cranial fossa arachnoid cysts assessed by MRI 3D segmentation and modeling. Childs Nerv Syst. 2014;30(6):1037–44.
Ma G, Li X, Qiao N, Zhang B, Li C, Zhang Y, et al. Suprasellar arachnoid cysts in adults: clinical presentations, radiological features, and treatment outcomes. Neurosurg Rev. 2021;44(3):1645–53.
Maher CO, Goumnerova L. The effectiveness of ventriculocystocisternostomy for suprasellar arachnoid cysts. J Neurosurg Pediatr. 2011;7(1):64–72.
Merola J, Manivannan S, Ooi S, Chia WL, Makwana M, Lang J, et al. The efficacy of cystoperitoneal shunting for the surgical management of intracranial arachnoid cysts in the elderly: a systematic review of the literature. Surg Neurol Int. 2021;12:624.
Mørkve SH, Helland CA, Amus J, Lund-Johansen M, Wester KG. Surgical decompression of arachnoid cysts leads to improved quality of life: a prospective study. Neurosurgery. 2016;78(5):613–25.
Okano A, Ogiwara H. The effectiveness of microsurgical fenestration for middle fossa arachnoid cysts in children. Childs Nerv Syst. 2016;32(1):153–8.
Pitsika M, Sgouros S. Volume change of cranial arachnoid cysts after successful endoscopic fenestration in symptomatic children. Childs Nerv Syst. 2019;35(12):2313–8.
Rabiei K, Högfeldt MJ, Doria-Medina R, Tisell M. Surgery for intracranial arachnoid cysts in children-a prospective long-term study. Childs Nerv Syst. 2016;32(7):1257–63.
Rizk E, Chern JJ, Tagayun C, Tubbs RS, Hankinson T, Rozzelle C, et al. Institutional experience of endoscopic suprasellar arachnoid cyst fenestration. Childs Nerv Syst. 2013;29(8):1345–7.
Sack I, Streitberger KJ, Krefting D, Paul F, Braun J. The influence of physiological aging and atrophy on brain viscoelastic properties in humans. PLoS One. 2011;6(9):e23451.
Schulz M, Oezkan Y, Schaumann A, Sieg M, Tietze A, Thomale UW. Surgical management of intracranial arachnoid cysts in pediatric patients: radiological and clinical outcome. J Neurosurg Pediatr. 2021;2021:1–11.
Shim KW, Lee YH, Park EK, Park YS, Choi JU, Kim DS. Treatment option for arachnoid cysts. Childs Nerv Syst. 2009;25(11):1459–66.
St George E, Natarajan K, Sgouros S. Changes in ventricular volume in hydrocephalic children following successful endoscopic third ventriculostomy. Childs Nerv Syst. 2004;20(11-12):834–8.
Taha AA, Hanbury A. Metrics for evaluating 3D medical image segmentation: analysis, selection, and tool. BMC Med Imaging. 2015;15:29.
Tamimi AF, Al Ryalat NT, Al Qaisi AK, Juweid ME, Obeidat FN, Al Hyasat TG, et al. Microsurgical fenestration of intracranial arachnoid cysts: volumetric analysis and clinical outcome. Pediatr Neurosurg. 2021;56(1):35–44.
Tan Z, Li Y, Zhu F, Zang D, Zhao C, Li C, et al. Children with intracranial arachnoid cysts: classification and treatment. Medicine. 2015;94(44):e1749.
Wang Y, Wang F, Yu M, Wang W. Clinical and radiological outcomes of surgical treatment for symptomatic arachnoid cysts in adults. J Clin Neurosci. 2015;22(9):1456–61.
Xenos C, Sgouros S, Natarajan K, Walsh AR, Hockley A. Influence of shunt type on ventricular volume changes in children with hydrocephalus. J Neurosurg. 2003;98(2):277–83.
Zhang B, Zhang Y, Ma Z. Long-term results of cystoperitoneal shunt placement for the treatment of arachnoid cysts in children. J Neurosurg Pediatr. 2012;10(4):302–5.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2023 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Hall, S., Gaastra, B., Tsitouras, V. (2023). Follow-Up of Arachnoid Cysts: Brain Plasticity Following Surgery for Arachnoid Cysts. In: Turgut, M., Akhaddar, A., Turgut, A.T., Hall, W.A. (eds) Arachnoid Cysts. Springer, Cham. https://doi.org/10.1007/978-3-031-22701-1_32
Download citation
DOI: https://doi.org/10.1007/978-3-031-22701-1_32
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-22700-4
Online ISBN: 978-3-031-22701-1
eBook Packages: MedicineMedicine (R0)