Abstract
Introduction
Endoscopic fenestration remains a first-line treatment option for symptomatic arachnoid cysts. After fenestration, the cyst does not collapse but reaches an equilibrium state. The aim of this study was to evaluate the change in cyst volume following successful fenestration and symptomatic improvement.
Methods
Cyst volume was measured on serial MR scans of 4 children (1 female, 3 males) with symptomatic arachnoid cysts (middle fossa n = 2, choroidal fissure n = 1 and posterior fossa n = 1), who experienced symptom resolution after endoscopic fenestration. Average follow-up was 20.5 months (range 3–48).
Results
Significant cyst volume reduction was seen in all four patients. In patient 1, preoperative cyst volume was 336 cm3 and decreased to 194 cm3 at 7 months (42% reduction). In patient 2, preoperative volume was 12.64 cm3 and reduced to 1.51 cm3 at 3 months (88% reduction). In patient 3, preoperative volume was 105 cm3 and reduced to 72 cm3 in 2 months (30% reduction). In patient 4, preoperative volume was 125 cm3 and reduced to 54 cm3 at 7 months (56% reduction). All remained stable after 7 months and there has been no late increase in volume.
Conclusions
Significant reduction in arachnoid cyst volume at the order of 30–40% is seen after successful endoscopic fenestration. The cyst volume appears to decrease gradually in the first 3–7 months and reaches a plateau after that. Complete resolution of symptoms in the presence of residual volume may indicate that cyst volume below a threshold may not correlate directly with clinical status.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Arachnoid cysts were first described in 1831 as cystic malformations of the arachnoid layer [1]. Their prevalence has been reported to be approximately 1% of all intracranial lesions and has been detected in up to 2.6% of all the children undergoing brain MRI, with a male predominance [2]. The collection of fluid develops within the arachnoid membrane secondary to splitting or duplication of the structural layer. The exact pathophysiological mechanism though is still yet to be understood. The most common locations are the middle cranial fossa (temporal, sylvian fissure), the posterior or anterior fossa, the convexity or other less common locations (ventricular/suprasellar/interhemispheric region, quadrigeminal plate) [2, 3].
In the majority of cases, the arachnoid cysts have a benign natural history and remain stable in size. A small proportion of them does increase in size secondary to a possible slit-valve mechanism that allows CSF to enter the cyst but not to return back to the ventricles [4, 5] causing symptoms due to direct mass effect in nearby structures or hydrocephalus from obstruction of the CSF pathways. Three main treatment options are available: insertion of a cysto-peritoneal shunt, microsurgical fenestration or endoscopic fenestration. With proliferation of endoscopic techniques during the last decade, endoscopic fenestration has become the treatment of choice for most cranial arachnoid cysts.
Following successful endoscopic fenestration, it has been reported in various studies that arachnoid cysts usually reduce in size, sometimes remain stable and they very rarely disappear [3, 6,7,8,9,10,11,12,13,14,15]. However, the exact CSF hydrodynamics, the change of cyst size in time and the association with the success of the endoscopic fenestration remain poorly understood. The aim of this study was to assess the cyst volume change in the long term following successful endoscopic fenestration in children with symptomatic congenital cranial arachnoid cysts.
Materials and methods
The study was a retrospective review of prospectively collected data of MR scans of 4 children treated for symptomatic arachnoid cysts with endoscopic fenestration, performed by the senior author in the period between June 2009 and February 2014. One more child was treated during the same period but had to be excluded due to lack of adequate preoperative radiological data.
There was a male predominance (3:1), mean age at the time of operation was 2.45 years (range 0.57–6.84 years) and average follow-up was 24.75 months (range 3–48 months). The location of the cysts was in the following: middle cranial fossa n = 2, choroidal fissure n = 1 and posterior fossa n = 1 (Table 1).
All patients had a preoperative MRI scan followed by postoperative sequential MRI scans to follow up any changes of the cyst for up to 2 years. Volume calculation was performed on the DICOM data of T2-weighted images using semi-manual segmentation tools of the programme 3D Slicer, which has been used and validated previously for volumetric analysis of brain tumours and CSF spaces [15,16,17].
Results
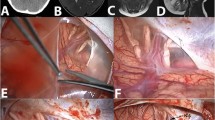
Following endoscopic fenestration, all four patients responded clinically and cyst volume decreased significantly (Fig. 1). In patient 1, preoperative cyst volume was 336 cm3 and decreased to 194.61 cm3 at 7 months (42% reduction). In patient 2, preoperative cyst volume was 12.64 cm3 and reduced to 1.51 cm3 at 3 months with almost complete resolution (88% reduction). In patient 3, preoperative volume was 104.68 cm3 and reduced to 72.37 cm3 in 2 months (30% reduction). In patient 4, preoperative volume was 124.81 cm3 and reduced to 54.33 cm3 at 7 months (56% reduction). All volumes remained stable after 7 months and there has been no late increase (Table 2, Fig. 2).
In every patient, the cyst rapidly reduced the first 3 to 6 months by 30–40% and reached a plateau after that (Fig. 3) with the exception of one patient (case 2) in which the cyst was small at presentation and almost disappeared during follow-up. All patients remained well clinically during follow-up.
Discussion
This study demonstrated that following successful endoscopic fenestration of arachnoid cysts in four symptomatic children, the cyst volume reduced rapidly in the first few months, reaching a plateau at approximately 6 months, with no significant further changes. Clinical response to the treatment was seen immediately and the children remain asymptomatic in the long term despite the fact that the cyst did not completely disappear and even in some cases remained large. This may indicate that the cyst size below a threshold might not directly correlate with the clinical status or that the fenestration produces a state of compensated coexistence with the surrounding brain, not causing a condition of raised pressure.
The radiological follow-up with assessment of cyst size following treatment of arachnoid cysts is not well reported. Li et al. [15], proposed the use of 3D modelling to assess the response of middle cranial fossa arachnoid cysts to treatment since it was felt that the use of the Galassi classification is not accurate. They reported a significant reduction in cyst volumes at 4 months postoperatively in all 26 cases that responded well clinically, while in two cases that were not successfully treated, an increase in the size was noted. Interestingly, the two cases that did not respond well even though the patency of the stomas was confirmed, they were both infants and they hypothesised that in these cases, the fenestration leads to a state of “post-endoscopic fenestration communicating hydrocephalus” with eventual break of the CSF circulation equilibrium.
Molina et al. [11] looked into the middle fossa cyst size changes following endoscopic treatment in children in comparison with adults. In a series of four adults, there was no change in cyst size and three of them responded well clinically to treatment. They also reported 7 cases in the children population that the cysts disappeared. However, there is no correlation with the initial size or the relative changes. They noted that cyst reduction is more remarkable in the paediatric population possibly secondary to increased elasticity of the younger brain, which has been compressed for a shorter period. A similar conclusion was made by Schroeder et al. [10] regarding the significant cyst reduction in children.
Ali et al. [7] studied a case series of 83 children with intracranial arachnoid cysts that were treated either with endoscopic fenestration, a cysto-peritoneal shunt or craniotomy and microsurgical fenestration. A similar proportion from each group (70–80%) at 6 months post-treatment had a reduction of more than 10 cm3, while in 20%, there was no change (as defined by any reduction in size < 10 cm3 or increase < 10 cm3) and an 11% that showed an increase in size. In the last group, 4 out of the 6 cases were infantile patients having a similar outcome with that reported by Li et al., as mentioned above. When those findings were correlated to the clinical outcome, they concluded that changes in cyst size is not associated with postoperative symptom resolution within the first 6 months of the treatment. Similarly, Galarza et al. [18] concluded that postoperative cyst reduction does not correlate with improvement of the symptoms when looking in a paediatric population that was treated either with cysto-peritoneal shunts of with craniotomy and cyst fenestration. In contrast to that, in the paediatric series from Karabatsou et al. [3] that all patients were treated with endoscopy, all the patients that showed progress of clinical symptoms had no radiological evidence of cyst size reduction and from the opposite point of view. Gangemi et al. [6] reported that all the cases that showed either complete remission or significant clinical improvement had a concomitant cyst size reduction.
The mechanism by which symptoms appear to be relieved following endoscopic fenestration despite the fact that the cyst does not completely disappear is still unknown. It is possible that following treatment, the communication between the cyst and the ventricular system creates a system of new CSF dynamics that might still include enlarged ventricles with a persistent cyst in a state of compensation. As described above, the cysts seem to decrease in size up to 6 months postoperatively and they remain stable further on. A similar finding has been described previously when looking at the ventricular size following endoscopic third ventriculostomy for hydrocephalus [19]. It was also noted that in patients with moderate initial volumes, there was a less steep reduction of the ventricular size in these first 3–6 months and that the final volumes remained higher than normal despite symptom resolution. These findings are similar to this study when looking at the differences in the rate of the cyst volume change depending on how big the cyst is prior to treatment.
In conclusion, this study provides evidence that following endoscopic fenestration of arachnoid cysts and successful symptom control, the cyst does not disappear but reduces in volume significantly in a period of up 3 to 6 months after treatment and it reaches a plateau with no significant changes further on. The small patient sample in this series did not allow any statistical analysis, making this an observation study. Further studies with bigger sample size may elucidate the issue further.
References
Bright R (1831) Serous cysts in the arachnoid. Diseases of the brain and nervous system, part I: Reports of medical cases selected with a view of illustrating the symptoms and cure of diseases by a reference to morbid anatomy, vol 2. Longman, Rees, Orme, Brown, Green, Paternoster-Row, Highley, London, pp 437–439
Al-Holou WN, Terman S, Kilburg C, Garton HJL, Muraszko KM, Maher CO (2013) Prevalence and natural history of arachnoid cysts in adults. J Neurosurg 118:222–231
Karabatsou K, Hayhurst C, Buxton N, O’Brien DF, Mallucci CL (2007) Endoscopic management of arachnoid cysts: an advancing technique. J Neurosurg Pediatr 106:455–462
Halani SH, Safain MG, Heilman CB (2013) Arachnoid cyst slit valves: the mechanism for arachnoid cyst enlargement. J Neurosurg Pediatr 12:62–66
Schroeder HW, Gaab MR (1997) Endoscopic observation of a slit-valve mechanism in a suprasellar prepontine arachnoid cyst: case report. Neurosurgery 40:198–200
Gangemi M, Seneca V, Colella G, Cioffi V, Imperato A, Maiuri F (2011) Endoscopy versus microsurgical cyst excision and shunting for treating intracranial arachnoid cysts. J Neurosurg Pediatr 8:158–164
Ali M, Bennardo M, Almenawer SA, Zagzoog N, Smith AA, Dao D, BHSc OA, Farrokhyar F, Singh SK (2015) Exploring predictors of surgery and comparing operative treatment approaches for pediatric intracranial arachnoid cysts: a case series of 83 patients. J Neurosurg Pediatr 16:275–282
Ciricillo SF, Cogen PH, Harsh GR, Edwards MSB (1991) Intracranial arachnoid cysts in children. A comparison of the effects of fenestration and shunting. J Neurosurg 74:230–235
Pradilla G, Jallo G (2007) Arachnoid cysts: case series and review of the literature. Neurosurg Focus 22:E7
Schroeder HW, Gaab MR, Niendorf WR (1996) Neuroendoscopic approach to arachnoid cysts. J Neurosurg 85:293–298
Fernández Molina G (2013) Neuroendoscopic management of middle fossa arachnoid cysts. World Neurosurg 79:S19.e19–S19.e23
Kim MH (1999) The role of endoscopic fenestration procedures for cerebral arachnoid cysts. J Korean Med Sci 14:443–447. https://doi.org/10.3346/jkms.1999.14.4.443
Greenfield J, Souweidane MM (2005) Endoscopic management of intracranial cysts. Neurosurg Focus 19:1–9
El-Ghandour NMF (2014) Endoscopic treatment of intraparenchymal arachnoid cysts in children. J Neurosurg Pediatr 14:501–507
Li Y, Chen X, Xu B (2014) The efficacy of neuroendoscopic treatment for middle cranial fossa arachnoid cysts assessed by MRI 3D segmentation and modeling. Childs Nerv Syst 30:1037–1044
Domínguez G, Miguel CH, Ruisoto P, Juanes JA, Prats A, Hernández T (2016) Morphological and volumetric assessment of cerebral ventricular system with 3D slicer software. J Med Syst 40 Springer US:154
Egger J, Kapur T, Fedorov A, Pieper S, Miller JV, Veeraraghavan H, Freisleben B, Golby AJ, Nimsky C, Kikinis R (2013) GBM volumetry using the 3D slicer medical image computing platform. Sci Rep 3:1364
Galarza M, Pomata HB, Pueyrredón F, Bartuluchi M, Zuccaro GN, Monges JA (2002) Symptomatic supratentorial arachnoid cysts in children. Pediatr Neurol 27:180–185
St George E, Natarajan K, Sgouros S (2004) Changes in ventricular volume in hydrocephalic children following successful endoscopic third ventriculostomy. Childs Nerv Syst 20:834–838
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
No conflict of interest to report.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Pitsika, M., Sgouros, S. Volume change of cranial arachnoid cysts after successful endoscopic fenestration in symptomatic children. Childs Nerv Syst 35, 2313–2318 (2019). https://doi.org/10.1007/s00381-019-04315-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-019-04315-9