Abstract
Imaging has a decisive role in every stage of a Bile Duct Injury (BDI), from prevention to ultimate management.
Preoperative Ultrasound (US) and Magnetic Resonance Imaging (MRI)/Magnetic Resonance Cholangiopancreatography (MRCP) can warn of the likelihood of difficult cholecystectomy, while the use of Intraoperative Cholangiogram (IOC) or Indocyanine Green (ICG) fluorescent cholangiography contributes to the early diagnosis of the lesion injury and avoids further damage if the intraoperative imaging is interpreted correctly.
If the BDI happened to occur, the abdominal US and Computed Tomography (CT) scan represents the first-line methods addressing the patient’s immediate needs (sepsis, fluid collections, peritonitis, perforation, etc.).
MRI/MRCP and the use of hepato-specific agents provide a correct evaluation of the biliary anatomy with the detection of possible bile leaks.
Finally, the use of CT angiography allows a precise characterization of the associated vascular injuries, decisive for planning the resolution of the BDI.
We thoroughly discuss the extension and application of these methods in the different stages of this disease throughout the chapter.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
Imaging methods have a protagonistic role in Bile Duct Injuries (BDI) along with different circumstances:
-
Preventively, the ultrasound (US) can alert the surgeon to anticipate a potential challenging case.
-
Intraoperatively, the Intraoperative Cholangiogram (IOC) or the laparoscopic US can enlighten the anatomical uncertainties that predispose to BDIs playing a fundamental role in their prevention [1].
-
If a BDI has been established, can be diagnosed at the time of surgery using IOC, or either in the early or late postoperative period using the US, Computed Tomography (CT) scan, Magnetic Resonance Imaging/Magnetic Resonance Cholangiopancreatography (MRI/MRCP) offer different diagnostic benefits depending on the time of presentation and the patient’s clinical condition [2, 3].
Prevention
US is widely accepted as the method of choice for the initial study of the gallbladder and biliary tract. Its role in the risk stratification of complex biliary pathology is unquestionable.
In this sense, acute cholecystitis (AC), exacerbated chronic cholecystitis (CC), and scleroatrophic gallbladders imply a higher risk of surgical treatment and can be easily detected by the routine US [4].
Those signs include a very thickened gallbladder wall (greater than 10 mm), cholelithiasis impacted in the infundibulum, and the presence of abscess or perivesicular plastron [5], Fig. 9.1.
A collapsed or fluidless gallbladder with or without parietal calcifications is usually related to scleroatrophic changes. The presence of dilatation of intrahepatic bile ducts, associated with dilatation of the proximal sector of the extrahepatic ducts should suggest Mirizzi syndrome. In addition, dilatation of the distal extrahepatic ducts may be associated with choledochal lithiasis, not always visible in US.
Abdominal CT scan and MRI are not first-line methods for the study of gallbladder pathology and are usually reserved for acute or chronic cholecystitis with extensive local involvement or to rule out gallbladder cancer [6].
MRCP is particularly useful for confirmation of Mirizzi’s syndrome and for choledochal lithiasis not visible by US, as well as allowing a correct evaluation of the biliary anatomy in order to detect variants with significant implications for surgery [7, 8] Fig. 9.2.
Whether or not IOC should be used systematically and selectively is still a matter of debate. What has been demonstrated is that IOC helps to detect an early injury, preventing the progression of damage and thus further related complications [9] (See Chap. 7).
A multicenter study including 1381 patients assessed the routine use of laparoscopic US in gallbladder surgery. This study demonstrated that routine use of laparoscopic US during LC has significantly improved its safety, compared to the previously reported BDI prevention rates (1 out of 200–400 LCs) [10]. The main issue is that laparoscopic US probes are often expensive and not widely available. Moreover, requires training and experience to achieve the best results.
Diagnosis of a BDI in the Early Postoperative Period
The most complex scenario is when the BDI occurred and was not recognized during the primary surgery.
In this situation, the patient is seen within the first week of the postoperative period with abdominal pain, peritonitis, sepsis, and overall poor general condition.
Any patient presenting like this after an elective cholecystectomy should be worked up, with a high suspicion of a BDI. The preferred initial studies are US and CT scan.
The presence of free peritoneal fluid, a perihepatic collection, or a fluid collection that lies adjacent to the CBD, with or without dilatation in the mentioned clinical context could represent indirect signs of a BDI, Fig. 9.3.
Should the BDI be confirmed, efforts at this stage should be directed to stabilize the patient and control the sepsis. The imaging is important to conduct therapies to address the acute disturbances the patient is facing, such as draining localized fluid collections or indicating abdominal washout in case of a choleperitoneum. More detailed studies should be deferred once the first objective (compensating and getting the patient out of the “danger zone”) is achieved.
CT scan has some advantages over the US in delineating abdominal fluid collections as well as in their therapeutic planning their percutaneous drainage is necessary, Fig. 9.4.
Diagnosis of a BDI in the Late Postoperative Period
BDIs that have gone unnoticed during the primary surgery and have not shown early symptoms, usually manifest later with fewer press symptoms.
These subacute manifestations of BDIs occur as a result of either partial or complete stenosis of secondary to metallic clips, thermal injuries causing progressive fibrosis or scarring or ischemia of the biliary tree. Symptoms are usually manifestations of cholestasis and include jaundice, pruritus, and cholangitis.
MRCP represents the method of choice for the evaluation of biliary anatomy at this stage. The presence of a sector of the biliary duct with a reduction in caliber or interruption of the signal allows the diagnosis of partial or complete stenosis, respectively. The localization of the extension of the stenosis can be determined with precision using this method, and the extent of the injury can be measured as well allowing precise surgical planning [7], Fig. 9.5.
Planning Surgical Reconstruction
Restoring the bilioenteric continuity and preventing cholestasis is the main priority once BDI’s had been compensated in the acute phase.
At this point, the main role of imaging is to define as accurately as possible the type of BDI the patient has and whether or not it is accompanied by vascular injury.
Is key to knowing if there’s biliary dilatation, any repercussion in the liver parenchyma, or if any other finding throughout the abdomen needs to be addressed as well.
All this information will play a fundamental role in the preparation for reconstructive surgery and will determine which is the best surgical approach.
Navigating the Uncertainties
In patients with a BDI, the diagnostic accuracy of conventional MRI/MRCP to detect a bile leak is about 70%. For the rest of the cases, or when there are some uncertainties about the location of the BDI (marked inflammation, collections, surgical clips, or drains either in the biliary tree or in the right upper quadrant), we can utilize other methods to better identify this [11].
Hepatobiliary Scintigraphy (HBS) is a widely available and economic method to detect the presence of bile leak, however, it lacks anatomical detail to aid in treatment planning [12].
Until a few years ago, this information was provided by Endoscopic Retrograde Cholangiopancreatography (ERCP) was the gold standard as it allows to identify directly and dynamically the presence of contrast extravasation outside the biliary tree at the site of the BDI and provides the window for therapeutic stent placements if necessary.
However, does not provide information about the status of the biliary duct proximal to the site of the BDI when the section is complete. In addition, as an invasive procedure is not exempt from complications (acute pancreatitis, infection, etc.) See Chap. 13.
Hepato-specific contrast Gadoxetic Disodium Acid (Gd-EOB-DTPA, Primovist), is a type of Gadolinium that has the characteristic of a rapid distribution in the bloodstream and a dual elimination pathway (50% renal and 50% biliar), combining the characteristic of conventional extracellular contrast agent with those hepato-specific.
Due to its chemical composition, it is taken up by the hepatocyte and then eliminated via the biliary system. It is worth mentioning that the uptake of hepatocyte-specific contrast is mediated by the same membrane transporter as bilirubin. Therefore, the lack of opacification of the biliary tree 20–30 mins after contrast administration may suggest biliary obstruction or poor liver function [13].
Its main indication classically lay in the detection and distinction of focal hepatic injuries (focal nodular hyperplasia vs. adenomas; determination of the number of hepatic metastases or characterization of nodules in cirrhotic patients) [14].
Recently, MRI with hepato-specific agents has been shown to provide dynamic and functional information on the biliary excretion and indirectly on liver function as well, similar to HBS.
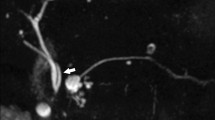
Their role in the management of BDI lies in the fact that has the capacity of performing accurate cholangiograms since demonstrate the biliary anatomy in a similar way to an MRCP, although with direct excreted contrast [13], Fig. 9.6.
It also allows Imaging methods: detection of active bile leak at the site of the BDI by direct visualization of the passage of contrast into the perihepatic or peribiliary fluid collections. This finding is represented by the presence of hyperintense signals in T1 sequences within these collections in images obtained in the hepatobiliary phase (20–60 mins). This then allows a correct noninvasive differential diagnoses between a BDI biloma and other possible etiologies of liquid collections near the surgical site (abscess, hematoma, cysts) [15].
Kantarci et al. demonstrated that the combination of conventional MRI + MRI cholangiography with hepato-specific contrast significantly increases the detection of BDI with associated bile leak [16].
In their series, they demonstrated that the identification of the BDI site using conventional MRCP was Imaging methods: obtained in 50% of patients but increased to a sensitivity of 81.2% and a specificity of 100% when combined with MRI with hepatocyte-specific agents.
In patients with a late manifestation of biliary stenosis, MRCP with hepato-specific agents can provide additional information about the degree of stenosis (partial or complete) based on the demonstration of contrast in the distal common bile duct below the site of stenosis as well [17].
Vascular Evaluation
The presence of a concomitant vascular injury has a variable incidence that depends on the type of BDI (See Chap. 6). However, the most frequent is an associated injury to the right hepatic artery (RHA) given its close relationship with the CBD (it runs posterior to the CBD in 71.6% and anterior in 8.3%) [18].
The development of an anastomotic network from the left hepatic artery (LHA) in general through the hilar plexus can supply sufficiently the irrigation of the right biliary tree. However, when the damage includes the portal vein (PV) as well, the risk of hepatic and biliary necrosis increases significantly [19].
A routine examination of the hepatic vasculature is recommended in every BDI, although it is fundamental to have it worked up when planning a reconstructive surgery.
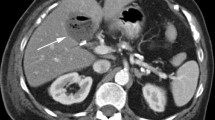
The advent of CT scan with multiplanar and three-dimensional reconstructions has made significant progress in the assessment of vascular anatomy of the liver. CT Angiography is now an adequate tool for the assessment of associated vascular lesions, detecting direct signs of associated vascular injury such as the presence of thinning, irregularity, or amputation of an artery, as well as the formation of pseudoaneurysms [20, 21] (See Chap. 11).
Indirect signs of vascular injury include areas of hepatic parenchymal infarction and necrosis, abscesses, lobar atrophy, and failure of attempted repair of a bilio-enteric anastomosis, Fig. 9.7.
Conclusions
Imaging has a decisive role in every stage of a BDI, from prevention to ultimate management.
Preoperative US and MRI can warn of the likelihood of difficult cholecystectomy, while the use of IOC contributes to the early diagnosis of the lesion injury and avoids further damage if the intraoperative imaging is interpreted correctly.
If the BDI happened to occur, the abdominal US and CT scan represent the first-line methods addressing the patient’s immediate needs (sepsis, fluid collections, peritonitis, perforation, etc.).
MRI/MRCP and the use of hepato-specific agents provide a correct evaluation of the biliary anatomy with the detection of possible bile leaks.
Finally, the use of CT angiography allows a precise characterization of the associated vascular injuries, decisive for planning the resolution of the BDI.
References
Alvarez FA, de Santibañes M, Palavecino M, Sánchez Clariá R, Mazza O, Arbues G, de Santibañes E, Pekolj J. Impact of routine intraoperative cholangiography during laparoscopic cholecystectomy on bile duct injury. Br J Surg. 2014;101:677–84.
Melamud K, LeBedis CA, Anderson SW, Soto JA. Biliary imaging: multimodality approach to imaging of biliary injuries and their complications. Radiographics. 2014;34:613–23.
Yeh BM, Liu PS, Soto JA, Corvera CA, Hussain HK. MR imaging and CT of the biliary tract. Radiographics. 2009;29:1669–88.
Elshaer M, Gravante G, Thomas K, Sorge R, Al-Hamali S, Ebdewi H. Subtotal cholecystectomy for “difficult gallbladders”: systematic review and meta-analysis. JAMA Surg. 2015;150:159–68.
de’ Angelis N, Catena F, Memeo R, et al. 2020 WSES guidelines for the detection and management of bile duct injury during cholecystectomy. World J Emerg Surg. 2021;16:30.
Hyodo T, Kumano S, Kushihata F, Okada M, Hirata M, Tsuda T, Takada Y, Mochizuki T, Murakami T. CT and MR cholangiography: advantages and pitfalls in the perioperative evaluation of the biliary tree. Br J Radiol. 2012;85:887–96.
Reddy S, Lopes Vendrami C, Mittal P, Borhani AA, Moreno CC, Miller FH. MRI evaluation of bile duct injuries and other post-cholecystectomy complications. Abdom Radiol (NY). 2021;46:3086–104.
Md LM. The Mirizzi syndrome –major cause for biliary duct injury during laparoscopic cholecystectomy. Biomed J Sci Tech Res. 2017;1 https://doi.org/10.26717/bjstr.2017.01.000308.
Rystedt JML, Wiss J, Adolfsson J, Enochsson L, Hallerbäck B, Johansson P, Jönsson C, Leander P, Österberg J, Montgomery A. Routine versus selective intraoperative cholangiography during cholecystectomy: systematic review, meta-analysis and health economic model analysis of iatrogenic bile duct injury. BJS Open. 2021;5 https://doi.org/10.1093/bjsopen/zraa032.
Machi J, Johnson JO, Deziel DJ, Soper NJ, Berber E, Siperstein A, Hata M, Patel A, Singh K, Arregui ME. The routine use of laparoscopic ultrasound decreases bile duct injury: a multicenter study. Surg Endosc. 2009;23:384–8.
Aduna M, Larena JA, Martín D, Martínez-Guereñu B, Aguirre I, Astigarraga E. Bile duct leaks after laparoscopic cholecystectomy: value of contrast-enhanced MRCP. Abdom Imaging. 2005;30:480–7.
Sharma P, Kumar R, Das KJ, Singh H, Pal S, Parshad R, Bal C, Bandopadhyaya GP, Malhotra A. Detection and localization of post-operative and post-traumatic bile leak: hybrid SPECT-CT with 99mTc-Mebrofenin. Abdom Imaging. 2012;37:803–11.
Gupta RT, Brady CM, Lotz J, Boll DT, Merkle EM. Dynamic MR imaging of the biliary system using hepatocyte-specific contrast agents. AJR Am J Roentgenol. 2010;195:405–13.
Grazioli L, Olivetti L, Mazza G, Bondioni MP. MR imaging of hepatocellular adenomas and differential diagnosis dilemma. Int J Hepatol. 2013;2013:374170.
Médart L, Coibion C, Deflandre J. Hepatobiliary-specific contrast agent in biliary leak. JBR-BTR. 2018;102:58.
Kantarcı M, Pirimoglu B, Karabulut N, Bayraktutan U, Ogul H, Ozturk G, Aydinli B, Kizrak Y, Eren S, Yilmaz S. Non-invasive detection of biliary leaks using Gd-EOB-DTPA-enhanced MR cholangiography: comparison with T2-weighted MR cholangiography. Eur Radiol. 2013;23:2713–22.
Lee NK, Kim S, Lee JW, Lee SH, Kang DH, Kim GH, Seo HI. Biliary MR imaging with Gd-EOB-DTPA and its clinical applications. Radiographics. 2009;29:1707–24.
Dandekar U, Dandekar K, Chavan S. Right hepatic artery: a cadaver investigation and its clinical significance. Anat Res Int. 2015;2015:412595.
Buell JF, Cronin DC, Funaki B, Koffron A, Yoshida A, Lo A, Leef J, Millis JM. Devastating and fatal complications associated with combined vascular and bile duct injuries during cholecystectomy. Arch Surg. 2002;137:703–8. discussion 708–10
Madanur MA, Battula N, Sethi H, Deshpande R, Heaton N, Rela M. Pseudoaneurysm following laparoscopic cholecystectomy. Hepatobiliary Pancreat Dis Int. 2007;6:294–8.
Machado NO, Al-Zadjali A, Kakaria AK, Younus S, Rahim MA, Al-Sukaiti R. Hepatic or cystic artery Pseudoaneurysms following a laparoscopic cholecystectomy: literature review of aetiopathogenesis, presentation, diagnosis and management. Sultan Qaboos Univ Med J. 2017;17:e135–46.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Spina, J.C., Orta, R. (2022). Role of Imaging. In: Pekolj, J., Ardiles, V., Glinka, J. (eds) Fundamentals of Bile Duct Injuries. Springer, Cham. https://doi.org/10.1007/978-3-031-13383-1_9
Download citation
DOI: https://doi.org/10.1007/978-3-031-13383-1_9
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-13382-4
Online ISBN: 978-3-031-13383-1
eBook Packages: MedicineMedicine (R0)