Abstract
Depression is frequent in the general population and among people who attend primary health-care clinics. Therefore, primary health-care clinicians play an essential role in providing timely and quality depression care, including the detection, diagnosis, treatment, monitoring, and referral of depressed patients. However, depression is usually underdiagnosed and undertreated in primary health care, with structural, organizational, provider, and patient barriers. Several studies have demonstrated that psychosocial, psychological, and pharmacological interventions for depression are feasible and effective in primary health-care settings. Systematic reviews and meta-analyses have consistently found that combined interventions, provided in a stepped-care manner, under a team-driven approach, and accompanied by system-level improvements, are the most effective. Although most of the evidence comes from developed countries, packages of low-resource interventions for depression have been proposed for developing nations.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 The Global Burden of Adult Depression
Depression has been one of the most relevant public health problems in recent decades. According to the Global Burden of Disease (GBD) Study 2019, led by the Institute for Health Metrics and Evaluation (IHME), 279 million people worldwide suffer from depressive disorders – equivalent to 3.8% of the world’s population (GBD 2019 Mental Disorders Collaborators, 2022). A closer inspection of the data provided by the IHME notes that the prevalence of depression increases during adulthood, reaching a peak of 6.0% immediately before older adulthood (Global Burden of Disease Collaborative Network, 2020). Depression mainly affects people during the most productive years of their lives, producing more significant declines in health than chronic physical illnesses such as arthritis or diabetes (Moussavi et al., 2007). Importantly, the health loss attributed to depression occurs earlier than those ascribed to these chronic physical diseases (Global Burden of Disease Collaborative Network, 2020). The patterning of the decrements in health produced by depression makes it one of the leading causes of years lived with disability, particularly in the 20–59 age group (GBD 2019 Mental Disorders Collaborators, 2022).
Depression is also associated with one of the most significant causes of death globally – suicide. The World Health Organization’s (WHO) Global Health Estimates (2017) report that more than 800,000 people die by suicide worldwide every year. Notably, depression is responsible for nearly half (46.1%) of the suicide burden attributed to mental and substance use disorders (Ferrari et al., 2014). Moreover, according to a recent systematic review and meta-regression, people with major depression are nearly eight times more likely than those not having this disorder to die by suicide (Moitra et al., 2021). Complementarily, there is very suggestive evidence of a possible association between depression and excess mortality in cancer, heart failure, and acute myocardial infarction, which would be mediated by pathological and physiological mechanisms and alterations in the behavior of the disease (Machado et al., 2018).
Depression does not affect the adult population equally. The IHME data suggests that, as older adulthood approaches, the prevalence of depression is twice as high in adults living in low-income vs. high-income countries (Global Burden of Disease Collaborative Network, 2020). The same source of information shows that for every depressed man, there are 1.5 depressed women in adulthood, regardless of the income level of the nation (Global Burden of Disease Collaborative Network, 2020). Furthermore, the GBD Study 2019 and WHO estimates found higher health losses attributable to depression in countries with increased rates of childhood sexual abuse, intimate partner violence, and conflict and war (Charlson et al., 2019; GBD 2019 Risk Factors Collaborators, 2020), highlighting population-level vulnerabilities to depression and its health consequences due to differential exposure to psychosocial risk factors. Notably, a recent systematic analysis of the prevalence of major depressive disorders during the ongoing COVID-19 pandemic noticed that the locations hardest hit by the pandemic had the most significant increases in the burden of depressive disorders (Santomauro et al., 2021).
2 Adult Depression in Primary Health Care
In the 1990s, the WHO led a relevant international study on psychological problems in general health care (Üstün & Sartorius, 1995). Primary health-care facilities in 14 culturally and economically diverse countries participated in the study. The diagnostic criteria of the International Classification of Diseases, Tenth Edition (ICD-10), were used to determine diagnoses for depression, anxiety disorders, and alcoholism, among others (Üstün & Sartorius, 1995). The WHO primary health-care study established that depression was the most prevalent mental disorder among the consulting population (10.4%), being more frequent in women (female/male ratio of 1.9) and patients with lesser education (Üstün & Sartorius, 1995). In four primary health-care centers (Santiago de Chile, Rio de Janeiro, Paris, and Bangalore), the female rate of depression was significantly higher than the male rate (Üstün & Sartorius, 1995). In addition, the WHO primary health-care study showed that psychiatric comorbidity of depression was consistently associated with severe limitations in daily activities and poorer health perception (Üstün & Sartorius, 1995).
More recently, a meta-analysis of 41 studies totaling 50,371 patients in mainly urban primary health-care clinics from more than ten countries explored the accuracy of unassisted diagnoses of depression by general practitioners (Mitchell et al., 2009). The studies included in Mitchell et al.’s meta-analysis identified cases of depression through psychiatric expert diagnosis or validated structured or semi-structured interviews. When studies recruiting adult patients aged 18–65 years were considered, the prevalence of depression in primary health care was 18.4% (Mitchell et al., 2009). Mitchell et al. (2009) estimated a depression prevalence of 17.2% for ICD-based studies, differing from the WHO primary health-care study, which reported a depression prevalence of 10.4% through the same method (Üstün & Sartorius, 1995). Such discrepancies might be driven by variations in sampling procedures or differences across primary health-care centers – e.g., the meta-analysis by Mitchell et al. (2009) relied mainly on primary health-care clinics from Western developed countries.
Large primary health-care cohorts in Australia (n = 7620 patients) (Gunn et al., 2012), England (n = 403,985) (Cassell et al., 2018), and Scotland (n = 1,751,841) (Smith et al., 2014) have established that comorbid depression and chronic physical conditions are the rules and not the exception. Depressed individuals in primary health care were more likely than nondepressed individuals to have physical comorbidities (Smith et al., 2014). Moreover, nearly half of depressed patients suffer multimorbidity, which is the presence of multiple diseases or conditions (Gunn et al., 2012; Smith et al., 2014). The most typical comorbidities found in depressed patients were painful conditions, stroke, and irritable bowel syndrome (Cassell et al., 2018; Gunn et al., 2012; Smith et al., 2014). Notably, one of the studies reported a dose-response relationship between the number of chronic physical diseases and the severity of depressive symptoms (Gunn et al., 2012). Multimorbidity in depressed patients was associated with socioeconomic deprivation (Cassell et al., 2018; Smith et al., 2014), considerable health losses (Gunn et al., 2012; Smith et al., 2014), and health services utilization (Cassell et al., 2018).
Well-designed prospective cohort studies have identified the main risk factors for depression in primary health-care adult patients. The WHO primary health-care study found that psychological problems (e.g., recurrent suicidal thoughts and previous depressive episodes), as well as poor health status, predicted new depressive episodes at 12-month follow-up (Barkow et al., 2002). The same study noticed that sociodemographic factors (i.e., low formal education and unemployment) appeared to be more salient for sustained non-remission of a depressive episode (Barkow et al., 2003). The PredictD international study developed a predictive algorithm for depression in primary health care based on data from 10,045 attendees in Europe and Chile. Psychosocial and clinical variables (e.g., difficulties in paid and unpaid work, lifetime depression, family history of psychological problems, poor physical and mental health status) were consistently selected in the PredictD algorithm (King et al., 2008).
Thus, depression appears to be particularly frequent in Western urban primary health-care facilities, and it is commonly associated with both physical and psychiatric comorbidities, generating significant degrees of disability. As in the general non-consultant population, depression mainly affects women, with psychosocial, psychological, and clinical variables leading to an increased propensity to depression in primary health-care attendees. Interestingly, secondary analyses of the PredictD data expand our understanding of the interplay between sex and risk factors for the onset of depression in primary health-care attendees (Stegenga et al., 2012). According to this study, women were not only more exposed than men to known risk factors, but they also faced enhanced susceptibility to depression resulting from exposure to these risk factors (Stegenga et al., 2012). Women were particularly affected by poor neighborhood conditions, whereas men were significantly impacted by living alone (Stegenga et al., 2012).
3 Integrating Mental Health into Primary Health Care
The WHO primary health-care study revealed that general practitioners acted as first contact care and gatekeepers for more than 75% of patients with mental health problems (Üstün & Sartorius, 1995). Complementarily, analyses of the WHO World Mental Health Surveys 2000–2005 described the use of mental health services for anxiety, mood, and substance disorders (Wang et al., 2007). The study found that among 84,850 participants in 17 low-, middle-, and high-income countries, the general practitioners were the largest source of mental health services (Wang et al., 2007). These findings confirm that primary health care plays a relevant role in the management of mental disorders, especially depression. Thus, it is necessary for general practitioners and allied health professionals in primary health care to timely and adequately detect, diagnose, and manage depression.
International organizations such as the WHO and its Regional Office for the Americas (PAHO), with support from the United Nations Children’s Fund (UNICEF), have been instrumental in advancing the political and technical case for mental health integration into primary health care, with a particular emphasis on the Region of the Americas. As a point of reference, the Third Special Meeting of the Americas’ Ministers of Health, held in Chile in 1972, summarized the health sector’s challenges and achievements (Organización Panamericana de la Salud, 1972). Regarding mental health care, the 1972 meeting recognized the critical state of mental health services in the Region, with virtually no coverage for a then vast rural population and the severe insufficiency to meet the needs of a comprehensive mental health program (Organización Panamericana de la Salud, 1972). The 1972 meeting envisioned the necessary changes to address the mental health services crisis, such as integrating psychiatric care into primary health care and primary mental health promotion and prevention activities into general health care (Organización Panamericana de la Salud, 1972).
The highly influential International Conference on Primary Health Care in Alma-Ata took place just 6 years after the 1972 meeting. The International Conference on Primary Health Care was jointly sponsored by the WHO and UNICEF, in which 134 countries and 67 international organizations participated (World Health Organization, 1978). The Conference recognized the urgent need to act on the grave inequalities in the global state of health and exhorted promotion and protection actions to realize the right to health (World Health Organization, 1978). According to the Conference, a primary health-care approach was deeply needed to achieve equity in health for all the people of the world (World Health Organization, 1978). Primary health care was considered essential health care that is universally accessible, acceptable, and affordable, “bringing health care close to where people live and work” (World Health Organization, 1978). The Conference emphasized that primary health care was the cornerstone of the health-care system and one of the foundations for social and economic development (World Health Organization, 1978).
The International Conference on Primary Health Care broadly recommended a set of priority contents for primary health care, such as the promotion of food supply and proper nutrition, the provision of maternal and child health care, and immunization against major infectious diseases (World Health Organization, 1978). The inclusion of mental health promotion was stressed among these subjects, an initial expression of the willingness and relevance of integrating mental health into primary health care (World Health Organization, 1978). This seminal disposition would find the definitive political and technical impetus with the Conference for the Restructuring of Psychiatric Care in Latin America, held in Caracas in 1990 (Levav et al., 1994). Although mainly regional in scope, with the participation of 11 Latin American countries (Levav et al., 1994), the Caracas Declaration has been recognized as a very influential milestone in global mental health (Patel et al., 2018).
The Caracas Declaration became a reference for mental health services reform processes, enshrining the commitment of Latin American governments to the development of community-based alternatives to psychiatric hospitals while respecting human rights (Levav et al., 1994). The Caracas Declaration explicitly states that restructuring psychiatric care should be based on primary health care, emphasizing decentralization, social participation and inclusion, and a preventive approach (Levav et al., 1994). Subsequent PAHO/WHO Executive Committee Resolutions have urged Latin American and Caribbean member states to adopt and deepen the principles set by the Caracas Declaration. Specifically, the Strategy and Plan of Action on Mental Health, among its recommendations, stresses the need to “review the organization of mental health services and carry out needed changes, emphasizing decentralization and strengthening the mental health component of primary health care” (Pan American Health Organization, 2009). This document also recognizes depression as a priority condition for which essential interventions should be available in primary health care (Pan American Health Organization, 2009).
Gathering much of the experience accumulated in Latin America, the WHO and the World Organization of Family Doctors (WONCA) provide a series of arguments for integrating mental health into primary health care (World Health Organization & World Organization of Family Doctors, 2008). Most reasons for primary mental health care are directly linked to the principles highlighted by the International Conference on Primary Health Care: an accessible, acceptable, affordable, and holistic approach to mental health care, taking advantage of the embeddedness of primary health care in local communities (World Health Organization & World Organization of Family Doctors, 2008). Furthermore, the WHO and WONCA recognized that primary mental health care minimizes stigma and discrimination and prevents human rights violations as they typically occur in psychiatric hospitals (World Health Organization & World Organization of Family Doctors, 2008).
The WHO/WONCA document also states that the integration of mental health into primary health care should be made explicit in all the areas of action of mental health policies and plans, safeguarding continued financial and human resources (World Health Organization & World Organization of Family Doctors, 2008). As for human resources, the WHO/WONCA document underlines that primary health-care workers need undergraduate and in-service training and supervision to perform specific and well-defined mental health tasks adequately (World Health Organization & World Organization of Family Doctors, 2008). Essential psychotropic medications should be directly available to patients in primary health-care facilities, and specialized mental health resources should be available to primary health-care patients and workers. Advocacy is required to sensitize political leaders, health authorities, and primary health-care workers on the relevance of primary mental health care. Thus, to ensure clear and continued commitments and investments to the integration processes from government health and non-health and nongovernment sectors. Finally, health and intersectoral coordination are fundamental in helping primary health-care patients integrate fully into their communities (World Health Organization & World Organization of Family Doctors, 2008).
The following paragraphs are dedicated to detailing a successful example for developing and integrating a mental health component into primary health care, which particularly applies to the case of adult depression. The Chilean case aligns very well with the principles stated in the WHO/WONCA framework. Following the restoration of democracy in Chile, psychiatric reform found the political will to expand community mental health care (Minoletti et al., 2012). In 1993, the first national mental health plan was published, emphasizing the importance of developing a mental health component in primary health care as one of its priority areas. This plan was accompanied by attempts to provide ongoing mental health training to human resources and integrate psychosocial practitioners (e.g., psychologists) into traditionally biomedical health teams. The deinstitutionalization process was complemented and significantly aided by establishing community mental health facilities and day hospitals (Minoletti et al., 2012).
The National Mental Health and Psychiatry Plan was created in 2000 in response to the limitations identified following the first national mental health plan’s experiences and to lessen the prevalence of impairment linked with mental diseases (Gobierno de Chile, 2020). This new mental health strategy established a model for mental health services networks and specified the roles of health teams. It also incorporated sectoral and intersectoral efforts in mental health (e.g., in education, housing, and justice) and identified seven programmatic priorities: depression, alcohol and drug misuse and dependency, attention deficit hyperactivity disorder, victims of violence, schizophrenia, and dementia are among the topics covered in this section (Ministerio de Salud de Chile, 2000). The National Depression Program exemplifies how a mental health component can be integrated into primary health care among the programmatic aims.
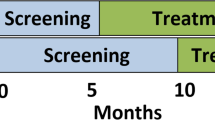
Araya et al. (2003) conducted one of the first randomized clinical trials in a middle-income country in the early 2000s. In Chile, the authors evaluated the effectiveness of a stepwise improvement program for treating depression in primary health-care attendees. Given the substantial proportion of women affected by depression in primary health care, this study enrolled 240 adult women diagnosed with major depression using the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV) criteria. Women were randomly assigned to receive usual care for depression or a stepped-care program, a highly structured, multicomponent intervention consisting of the following components: (1) a manualized, group-based psychoeducational intervention, (2) systematic monitoring of clinical evolution, and (3) a pre-established relapse prevention strategy (Araya et al., 2003).
The results of this clinical trial were highly positive: at 3 and 6 months, 49% and 70% of women who received the stepped-care program experienced recovery from depression, as measured by a Hamilton Depression Scale score of less than 8, respectively, compared to 15% and 32% of women who received usual treatment (Araya et al., 2003). This clinical trial was notable for the reorganization of primary health-care resources, with most actions carried out by nonmedical health professionals, and for the increased adherence of users in their treatment, which had a significant impact on the structure of the National Depression Program (Araya et al., 2003).
The National Depression Program began with a pilot phase in 2001, following the second National Mental Health and Psychiatry Plan adoption, and by 2003 had expanded to virtually every Chilean territory. The National Depression Program includes the following components (Alvarado et al., 2012):
-
1.
On-site diagnostic evaluation of patients with a suspected depressive episode by a general practitioner or psychologist, based on the diagnostic criteria for depression in the ICD.
-
2.
Indication of stepped-care treatment, according to severity level, incorporating (1) comprehensive evaluation by the primary health-care team, (2) treatment with antidepressant drugs, (3) individual psychotherapy and psychoeducational group intervention, and (4) visits to monitor the patient’s clinical progress.
-
3.
Patients with mild to moderate depression are managed in primary health-care clinics. The more severe cases are referred to specialized and outpatient mental health facilities for evaluation by a psychiatrist. If the clinical response to initial treatment is not favorable, the patient is reassessed by a psychiatrist at the primary health-care facility and, if necessary, referred to specialty care.
In September 2004, the Regime of Explicit Health Guarantees became law, mandating public and private health-care providers to guarantee access, quality, timeliness, and financial coverage for health care for prioritized health conditions (Araya et al., 2009). At the end of 2005, the second Regime of Explicit Health Guarantees came into force, which incorporated depression among the prioritized health conditions, and established that (1) all beneficiaries aged 15 years and over, with diagnostic confirmation, will have access to treatment; (2) for beneficiaries with mild or moderate depressions, treatment must be promptly initiated from the diagnostic confirmation, and, in more severe cases, consultation with a specialist must be made within 30 days from referral; (3) financial protection corresponds to a maximum co-payment of 20%; and (4) quality is defined by the provision of specific benefits for depression by an accredited or certified provider (Ministerio de Salud de Chile, 2006).
The Clinical Guidelines for Depression in People Aged 15 Years and Over currently direct the National Depression Program (Ministerio de Salud de Chile, 2013). The Clinical Guidelines stated objectives are to facilitate the active detection of depressive disorders, the reduction of their complications through comprehensive and continuous management, and to promote the rational use of available resources. Its successive editions and other regulatory documents, such as the Guidelines for Network Planning and Programming 2019 (Ministerio de Salud de Chile, 2019), have emphasized the management of major depression in primary health care, assisted referral to specialized mental health care in those cases with high suicidal risk, bipolar disorder, or treatment resistance (Ministerio de Salud de Chile, 2013), and the administration of individual psychotherapy in specialized mental health facilities (Ministerio de Salud de Chile, 2019).
4 Barriers to the Treatment of Depression in Primary Health Care
The Lancet Commission on Global Mental Health and Sustainable Development stresses that mental health is a public good necessary for sustainable development (Patel et al., 2018). However, the low priority given to mental health is one of the main macrostructural barriers that threaten access to this public good and sustainable development (Patel et al., 2018). An influential review on resources for mental health care found that scarcity, inequity, and inefficiency of such resources are the main obstacles to better mental health (Saxena et al., 2007). These severe limitations mean that the populations most vulnerable and in greatest need of mental health care have the least access to these services (Saxena et al., 2007). While mental health policies, plans, and laws exist in many countries, they are often outdated and poorly aligned with human rights standards to protect people with mental disorders (Saxena et al., 2007). As referred below, these structural barriers affect the quality of mental health services in primary health care.
The WHO Mental Health Atlas 2020 reported that the median global public expenditure on mental health was a meager 2.1% of total government health expenditure (World Health Organization, 2021). Moreover, most countries (81%) allocated less than a fifth of this expenditure to primary health care (World Health Organization, 2021). The WHO Mental Health Atlas 2020 assessed the functional integration of mental health into primary health care, considering the adoption of guidelines, the availability of pharmacological and psychosocial interventions, and training and supervision of primary health-care professionals (World Health Organization, 2021). Only 15% of countries met all criteria for functional integration of mental health into primary health care, whereas 31% met most criteria (World Health Organization, 2021). Notably, a low proportion of countries informed the provision of pharmacological (39%) and psychosocial (21%) interventions in primary health-care centers (World Health Organization, 2021).
Although 80% of countries noted that training was available for primary health-care professionals, the WHO Mental Health Atlas does not report details such as type, duration, or coverage (World Health Organization, 2021). An assessment of the mental health systems of 42 low- and middle-income countries made by the WHO offers a complementary view (World Health Organization, 2009). The evaluation showed that the proportion of total undergraduate training hours devoted to mental health is negligible for primary health-care professionals; the same occurs with refresher courses and in-service training (World Health Organization, 2009). In general, the higher the income level, the greater the training opportunities reported for primary health-care professionals (World Health Organization, 2009). The scarce training opportunities may affect primary health-care professionals’ ability to manage depression. For instance, despite Chile’s successful integration of mental health into primary health care, a recent study found that nurses, midwives, and general practitioners had difficulties in depression screening and diagnosis (Martínez et al., 2019).
International studies led by the WHO have shown that general practitioners in primary health care are the first and foremost source of mental health care (Üstün & Sartorius, 1995; Wang et al., 2007). However, the WHO primary health-care study and Mitchell et al.’s meta-analysis observed that nearly half of depressed patients (47.3–54.2%) were correctly recognized by general practitioners, signaling the need for improved diagnosis (Mitchell et al., 2009; Üstün & Sartorius, 1995). The detection of depression by primary health-care clinicians in low- and middle-income countries is considerably lower, with rates typically in the ranges of 0–12% (Fekadu et al., 2020). Low detection rates might be influenced by illness behavior, as patients usually present somatic symptoms instead of psychological complaints (Üstün & Sartorius, 1995). Organizational factors might also shape detection accuracies, such as increased performance monitoring, periodic review of clinical outcomes, presence of an appointment system, and general practitioners assuming responsibility for coordination of patient care (Mitchell et al., 2011; Üstün & Sartorius, 1995).
A return on investment analysis for depression and anxiety disorders in 36 countries estimated that between 80% and 95% of depressed people do not receive basic psychosocial treatments or antidepressants, the usual primary health-care treatments for depression, when available (Chisholm et al., 2016). Complementarily, Pence et al. conducted a literature review to study the depression treatment continuum in primary health care (Pence et al., 2012). The authors determined that of all primary health-care patients with a major depressive episode, 24% received any treatment, 9% were adequately treated, and 6% achieved remission (Pence et al., 2012). They also projected that improving the adequacy of treatment would have the largest single impact on remission rates. It is relevant to address the barriers to managing depression in primary health care because early detection and treatment of depressive disorders facilitates the treatment response and remission of mood symptoms and reduces the risk of a chronic course of illness (Ghio et al., 2014).
Several syntheses of qualitative and quantitative studies have explored the barriers to managing depression in primary health care (Barley et al., 2011; Carlsen et al., 2007; Holm & Severinsson, 2012; McPherson & Armstrong, 2012; Schumann et al., 2012). These syntheses underscore that one of the main issues primary health-care clinicians face is understanding depression either as social distress or as a chemical imbalance (Barley et al., 2011; McPherson & Armstrong, 2012; Schumann et al., 2012). Acknowledging the social origins of depression leads primary health-care clinicians to confront the limits of their capabilities, feeling powerless in managing the disease (e.g., should social problems be medicalized?), whereas a “true” depression conforms to a biomedical disease model (Barley et al., 2011; McPherson & Armstrong, 2012; Schumann et al., 2012). Another primary concern is detecting and diagnosing depression. General practitioners refer to depression as puzzling, usually masked in physical symptoms (Barley et al., 2011; McPherson & Armstrong, 2012; Schumann et al., 2012). Making the diagnosis of depression requires a personalized assessment of patients, demanding time (a rare commodity), watchful waiting, and active listening (Barley et al., 2011; McPherson & Armstrong, 2012; Schumann et al., 2012). Addressing patients’ stigma and fears toward mental illness and having a good doctor-patient relationship are essential to overcoming the difficulties found in these processes (Barley et al., 2011; McPherson & Armstrong, 2012; Schumann et al., 2012).
Regarding therapeutic options available, general practitioners admit that active listening, emotional support, and empathy are their best assets when treating depression (Barley et al., 2011; McPherson & Armstrong, 2012; Schumann et al., 2012). These resources also help them negotiate antidepressant use with patients (Barley et al., 2011). However, the management of depression in primary health care is further complicated by organizational factors. For instance, primary health-care clinicians complain about the lack of clear role definitions, difficulties in the coordination of teamwork, and the poor availability of specialized mental health care, perceived as burdened with patients having severe mental disorders (Barley et al., 2011; Carlsen et al., 2007; Holm & Severinsson, 2012; McPherson & Armstrong, 2012). These barriers are complemented by the perception of clinical guidelines for depression as not readily applicable to real clinical contexts and as a threat to the judicialization of the doctor-patient relationship (Carlsen et al., 2007; Holm & Severinsson, 2012). Finally, even when clinicians recognize the need for training in depression management, negative experiences with previous depression training programs and prioritization of training in addressing physical health problems are limitations to furthering their skills (Barley et al., 2011; McPherson & Armstrong, 2012).
5 Evidence-Based Interventions for Adult Depression in Primary Health Care
In this section, the main findings of recent systematic reviews and meta-analyses on the effectiveness of psychological and pharmacological interventions that have been tested in primary health care are reviewed. Furthermore, acknowledging the relevance of combined psychological and pharmacological interventions, we introduce the principles of the collaborative care model. The collaborative care model is a complex, highly effective, and influential approach to treating depression in primary health care. We finalize with a brief mention of the integration of information technologies into the primary health-care treatment of depression.
Antidepressants are acceptable and more effective than placebo in adults with major depression (Cipriani et al., 2018). However, most of the evidence cannot be directly applied to primary health care: studies have been conducted in different settings and recruited individuals with moderate to severe depressive symptoms (Cipriani et al., 2018). Few clinical trials have evaluated the efficacy of antidepressants in primary health care, despite the availability of psychotropics being a principle in primary mental health care (World Health Organization & World Organization of Family Doctors, 2008). Arroll et al.’s (2016) meta-analysis found 17 studies comparing antidepressants to placebo in primary health care. In general, these studies enrolled patients with mild to moderate depressive symptoms and explored short-term outcomes. The authors concluded that tricyclic antidepressants (e.g., amitriptyline) and selective serotonin reuptake inhibitors (e.g., sertraline and escitalopram) provided significant benefits in terms of response (i.e., >50% reduction in depressive symptoms from baseline) (Arroll et al., 2016). However, they caution that their data does not shed light as to when, who, and for how long antidepressants should be used in primary health-care attendees (Arroll et al., 2016).
Cognitive behavioral therapy and problem-solving therapy are the most studied psychological treatments for adult depression in primary health care (Cuijpers et al., 2019; Zhang et al., 2019). While cognitive behavioral therapy aims to change dysfunctional thoughts and cognitive distortions (Hofmann et al., 2013), problem-solving therapy trains patients in adaptive problem-solving attitudes and skills (Bell & D’Zurilla, 2009). Cuijpers et al. (2019) found that psychotherapies for depression in primary health care are effective and that face-to-face comparisons revealed no significant differences between them. Moreover, the same evidence synthesis showed that psychotherapies for depression could be delivered by general practitioners and allied health-care workers (Cuijpers et al., 2019). The authors argue that such finding is relevant to scale-up primary health-care depression treatment in low- and middle-income countries (Cuijpers et al., 2019). Interestingly, research has shown that psychotherapies’ effectiveness for depression in primary health care is moderated by treatment modality: individual interventions and outside primary health-care facilities (i.e., closer to patients’ homes) are more effective (Zhang et al., 2019).
More recently, a network meta-analysis by Cuijpers et al. (2021) provided the first comparison between pharmacological, psychological, and combined interventions for depression in primary health care. Cuijpers et al.’s network meta-analysis (2021) included 58 studies, totaling 9301 mostly adult primary health-care attendees. The authors found that the three types of treatments explored were more effective than treatment as usual and waitlist controls (Cuijpers et al., 2021). However, a clear preference for combined pharmacological and psychological interventions was evidenced, achieving better response, remission, and improvement in depressive symptoms (Cuijpers et al., 2021). Notably, the network meta-analysis found no significant differences in the acceptability of these interventions, underlining the relevance of adapting treatment offer to patients’ preferences (Cuijpers et al., 2021).
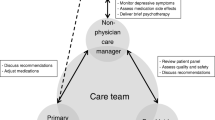
The collaborative care model might be thought of as a model for the integration of combined interventions for managing depression in primary health care. A group of researchers in the United States, led by Wayne Katon et al. (1995, 1996, 1997, 1999), developed the collaborative care model based on chronic and recurrent illness care. This model provided a multicomponent intervention, with increased patient engagement and education, more regular treatment in the acute phase of the illness, and more intensive treatment for more severe patients (i.e., stepped treatment). This was complemented by strict monitoring of treatment adherence, training for primary care physicians in the management of depression, and closer collaboration between treating physicians and psychiatrists (i.e., mental health consultancies). Collaborative care proved feasible to implement in primary health care, acceptable to patients and general practitioners, effective in reducing depressive symptoms, and cost-effective (Katon et al., 1995, 1996, 1997, 1999).
Currently, the collaborative care model has robust evidence for its benefits: decreased depressive symptoms, increased adherence and response to treatment, improvements in quality of life and satisfaction with care, and economic efficiency, in a wide range of depressed patients (Miller et al., 2013; Vanderlip et al., 2016). According to Vanderlip et al. (2016), the collaborative care model involves:
-
(i)
A general practitioner who leads a multidisciplinary health-care team in coordination with a case manager (e.g., a nurse). The primary health-care team receives consultation from a mental health specialist.
-
(ii)
Improving the quality of care and health outcomes of a population, through a systematic review of cases periodically to redirect health resources, and analysis of aggregated patient data to identify and act on gaps in care in the population.
-
(iii)
Health care is based on timely measurements for assessing progress in patients’ health status through reliable, change-sensitive, and simple-to-apply instruments (e.g., the Patient Health Questionnaire-9, PHQ-9, in the case of depression).
-
(iv)
The provision of evidence-based interventions, structured in a stepped manner (e.g., greater intensity of interventions as the case’s complexity increases), and with instruments to support clinical decision making (e.g., mental health consultancies, clinical guidelines with standardized management algorithms, among others).
A panel of experts studied the effectiveness of the collaborative care model in clinical trials published between 2004 and 2009, reporting the finding of robust evidence for significant improvements in depressive symptoms, adherence, and response to treatment, quality of life, and satisfaction with care in a wide range of depressed patients (Thota et al., 2012). Complementarily, a systematic review of the economic efficiency of the collaborative care model (Jacob et al., 2012), conducted by the same expert panel, found positive economic benefits, lower programmatic costs, willingness-to-pay exceeding expenses, and greater cost-effectiveness in sites receiving the intervention.
Finally, scientific innovations in the management of depression in primary health care from developed countries have been presented, raising questions about the feasibility of implementing such models in under-resourced settings in developing countries. In this regard, Patel et al. (2009) reviewed the evidence on the efficacy of treatments and the provision of interventions for the management of depression in low- and middle-income countries. They proposed a “package” of care for depression in these settings (Patel et al., 2009). The authors concluded that a basic package for depression management should include routine use of culturally adapted instruments to improve depression screening; patient education about their health problem and treatment alternatives; context-specific antidepressant treatments and psychotherapy, such as generic antidepressants and problem-solving therapy; and that task shifting to nonspecialist health workers, who provide first-line care and are supervised by specialists, is essential to integrate this package into routine care in community services (Patel et al., 2009).
6 Conclusion
Depression is a very important public health problem worldwide. It is frequent in people who attend primary care clinics, and it is frequently associated with chronic diseases and psychiatric comorbidities.
The primary care team can play a crucial role in depression management. Therefore, it is necessary for the development of a mental health component in primary care based on the principles of the collaborative care model that has demonstrated a highly effective and influential approach to treating depression in primary health care.
References
Alvarado, R., Rojas, G., Minoletti, A., Alvarado, F., & Domínguez, C. (2012). Depression program in primary health care. International Journal of Mental Health, 41(1), 38–47. https://doi.org/10.2753/IMH0020-7411410103
Araya, R., Alvarado, R., & Minoletti, A. (2009). Chile: An ongoing mental health revolution. Lancet (London, England), 374(9690), 597–598. https://doi.org/10.1016/S0140-6736(09)61490-2
Araya, R., Rojas, G., Fritsch, R., Gaete, J., Rojas, M., Simon, G., & Peters, T. J. (2003). Treating depression in primary care in low-income women in Santiago, Chile: A randomised controlled trial. Lancet (London, England), 361(9362), 995–1000. https://doi.org/10.1016/S0140-6736(03)12825-5
Arroll, B., Chin, W.-Y., Martis, W., Goodyear-Smith, F., Mount, V., Kingsford, D., Humm, S., Blashki, G., & MacGillivray, S. (2016). Antidepressants for treatment of depression in primary care: A systematic review and meta-analysis. Journal of Primary Health Care, 8(4), 325–334. https://doi.org/10.1071/HC16008
Barkow, K., Maier, W., Ustün, T. B., Gänsicke, M., Wittchen, H. U., & Heun, R. (2002). Risk factors for new depressive episodes in primary health care: An international prospective 12-month follow-up study. Psychological Medicine, 32(4), 595–607. https://doi.org/10.1017/s0033291702005263
Barkow, K., Maier, W., Ustün, T. B., Gänsicke, M., Wittchen, H.-U., & Heun, R. (2003). Risk factors for depression at 12-month follow-up in adult primary health care patients with major depression: An international prospective study. Journal of Affective Disorders, 76(1–3), 157–169. https://doi.org/10.1016/s0165-0327(02)00081-2
Barley, E. A., Murray, J., Walters, P., & Tylee, A. (2011). Managing depression in primary care: A meta-synthesis of qualitative and quantitative research from the UK to identify barriers and facilitators. BMC Family Practice, 12, 47. https://doi.org/10.1186/1471-2296-12-47
Bell, A. C., & D’Zurilla, T. J. (2009). Problem-solving therapy for depression: A meta-analysis. Clinical Psychology Review, 29(4), 348–353. https://doi.org/10.1016/j.cpr.2009.02.003
Carlsen, B., Glenton, C., & Pope, C. (2007). Thou shalt versus thou shalt not: A meta-synthesis of GPs’ attitudes to clinical practice guidelines. The British Journal of General Practice, 57(545), 971–978.
Cassell, A., Edwards, D., Harshfield, A., Rhodes, K., Brimicombe, J., Payne, R., & Griffin, S. (2018). The epidemiology of multimorbidity in primary care: A retrospective cohort study. British Journal of General Practice, 68(669), e245–e251. https://doi.org/10.3399/bjgp18X695465
Charlson, F., van Ommeren, M., Flaxman, A., Cornett, J., Whiteford, H., & Saxena, S. (2019). New WHO prevalence estimates of mental disorders in conflict settings: A systematic review and meta-analysis. Lancet (London, England), 394(10194), 240–248. https://doi.org/10.1016/S0140-6736(19)30934-1
Chisholm, D., Sweeny, K., Sheehan, P., Rasmussen, B., Smit, F., Cuijpers, P., & Saxena, S. (2016). Scaling-up treatment of depression and anxiety: A global return on investment analysis. The Lancet Psychiatry, 3(5), 415–424. https://doi.org/10.1016/S2215-0366(16)30024-4
Cipriani, A., Furukawa, T. A., Salanti, G., Chaimani, A., Atkinson, L. Z., Ogawa, Y., Leucht, S., Ruhe, H. G., Turner, E. H., Higgins, J. P. T., Egger, M., Takeshima, N., Hayasaka, Y., Imai, H., Shinohara, K., Tajika, A., Ioannidis, J. P. A., & Geddes, J. R. (2018). Comparative efficacy and acceptability of 21 antidepressant drugs for the acute treatment of adults with major depressive disorder: A systematic review and network meta-analysis. Lancet (London, England), 391(10128), 1357–1366. https://doi.org/10.1016/S0140-6736(17)32802-7
Cuijpers, P., Oud, M., Karyotaki, E., Noma, H., Quero, S., Cipriani, A., Arroll, B., & Furukawa, T. A. (2021). Psychologic treatment of depression compared with pharmacotherapy and combined treatment in primary care: A network meta-analysis. The Annals of Family Medicine, 19(3), 262–270. https://doi.org/10.1370/afm.2676
Cuijpers, P., Quero, S., Dowrick, C., & Arroll, B. (2019). Psychological treatment of depression in primary care: Recent developments. Current Psychiatry Reports, 21(12), 129. https://doi.org/10.1007/s11920-019-1117-x
Fekadu, A., Demissie, M., Berhane, R., Medhin, G., Bitew, T., Hailemariam, M., Minaye, A., Habtamu, K., Milkias, B., Petersen, I., Patel, V., Cleare, A. J., Mayston, R., Thornicroft, G., Alem, A., Hanlon, C., & Prince, M. (2020). Under detection of depression in primary care settings in low and middle-income countries: A systematic review and meta-analysis (p. 2020.03.20.20039628). https://doi.org/10.1101/2020.03.20.20039628
Ferrari, A. J., Norman, R. E., Freedman, G., Baxter, A. J., Pirkis, J. E., Harris, M. G., Page, A., Carnahan, E., Degenhardt, L., Vos, T., & Whiteford, H. A. (2014). The burden attributable to mental and substance use disorders as risk factors for suicide: Findings from the global burden of disease study 2010. PLoS One, 9(4), e91936. https://doi.org/10.1371/journal.pone.0091936
GBD 2019 Mental Disorders Collaborators. (2022). Global, regional, and national burden of 12 mental disorders in 204 countries and territories, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. The Lancet Psychiatry, 9(2), 137–150. https://doi.org/10.1016/S2215-0366(21)00395-3
GBD 2019 Risk Factors Collaborators. (2020). Global burden of 87 risk factors in 204 countries and territories, 1990-2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet (London, England), 396(10258), 1223–1249. https://doi.org/10.1016/S0140-6736(20)30752-2
Ghio, L., Gotelli, S., Marcenaro, M., Amore, M., & Natta, W. (2014). Duration of untreated illness and outcomes in unipolar depression: A systematic review and meta-analysis. Journal of Affective Disorders, 152–154, 45–51. https://doi.org/10.1016/j.jad.2013.10.002
Global Burden of Disease Collaborative Network. (2020). Global Burden of Disease Study 2019 (GBD 2019) results. Institute for Health Metrics and Evaluation (IHME). http://ghdx.healthdata.org/gbd-results-tool/result
Gobierno de Chile. (2020). Política Nacional para la Reducción del Riesgo de Desastres: Plan Estratégico Nacional 2020-2030 (p. 176). ONEMI – Ministerio del Interior y Seguridad Pública.
Gunn, J. M., Ayton, D. R., Densley, K., Pallant, J. F., Chondros, P., Herrman, H. E., & Dowrick, C. F. (2012). The association between chronic illness, multimorbidity and depressive symptoms in an Australian primary care cohort. Social Psychiatry and Psychiatric Epidemiology, 47(2), 175–184. https://doi.org/10.1007/s00127-010-0330-z
Hofmann, S. G., Asmundson, G. J. G., & Beck, A. T. (2013). The science of cognitive therapy. Behavior Therapy, 44(2), 199–212. https://doi.org/10.1016/j.beth.2009.01.007
Holm, A. L., & Severinsson, E. (2012). Chronic care model for the management of depression: Synthesis of barriers to, and facilitators of, success. International Journal of Mental Health Nursing, 21(6), 513–523. https://doi.org/10.1111/j.1447-0349.2012.00827.x
Jacob, V., Chattopadhyay, S. K., Sipe, T. A., Thota, A. B., Byard, G. J., Chapman, D. P., & Community Preventive Services Task Force. (2012). Economics of collaborative care for management of depressive disorders: A community guide systematic review. American Journal of Preventive Medicine, 42(5), 539–549. https://doi.org/10.1016/j.amepre.2012.01.011
Katon, W., Robinson, P., Von Korff, M., Lin, E., Bush, T., Ludman, E., Simon, G., & Walker, E. (1996). A multifaceted intervention to improve treatment of depression in primary care. Archives of General Psychiatry, 53(10), 924–932. https://doi.org/10.1001/archpsyc.1996.01830100072009
Katon, W., Von Korff, M., Lin, E., Simon, G., Walker, E., Bush, T., & Ludman, E. (1997). Collaborative management to achieve depression treatment guidelines. The Journal of Clinical Psychiatry, 58(Suppl 1), 20–23.
Katon, W., Von Korff, M., Lin, E., Simon, G., Walker, E., Unützer, J., Bush, T., Russo, J., & Ludman, E. (1999). Stepped collaborative care for primary care patients with persistent symptoms of depression: A randomized trial. Archives of General Psychiatry, 56(12), 1109–1115. https://doi.org/10.1001/archpsyc.56.12.1109
Katon, W., Von Korff, M., Lin, E., Walker, E., Simon, G. E., Bush, T., Robinson, P., & Russo, J. (1995). Collaborative management to achieve treatment guidelines. Impact on depression in primary care. JAMA, 273(13), 1026–1031.
King, M., Walker, C., Levy, G., Bottomley, C., Royston, P., Weich, S., Bellón-Saameño, J. A., Moreno, B., Svab, I., Rotar, D., Rifel, J., Maaroos, H.-I., Aluoja, A., Kalda, R., Neeleman, J., Geerlings, M. I., Xavier, M., Carraça, I., Gonçalves-Pereira, M., et al. (2008). Development and validation of an international risk prediction algorithm for episodes of major depression in general practice attendees: The PredictD study. Archives of General Psychiatry, 65(12), 1368–1376. https://doi.org/10.1001/archpsyc.65.12.1368
Levav, I., Restrepo, H., & de Macedo, C. G. (1994). The restructuring of psychiatric care in Latin America: A new policy for mental health services. Journal of Public Health Policy, 15(1), 71–85. https://doi.org/10.2307/3342608
Machado, M. O., Veronese, N., Sanches, M., Stubbs, B., Koyanagi, A., Thompson, T., Tzoulaki, I., Solmi, M., Vancampfort, D., Schuch, F. B., Maes, M., Fava, G. A., Ioannidis, J. P. A., & Carvalho, A. F. (2018). The association of depression and all-cause and cause-specific mortality: An umbrella review of systematic reviews and meta-analyses. BMC Medicine, 16(1), 112. https://doi.org/10.1186/s12916-018-1101-z
Martínez, P., Rojas, G., Martínez, V., Marín, R., Cornejo, J. P., & Gómez, V. (2019). Measuring primary health care clinicians’ skills for depression management. Frontiers in Psychiatry, 10, 570. https://doi.org/10.3389/fpsyt.2019.00570
McPherson, S., & Armstrong, D. (2012). General practitioner management of depression: A systematic review. Qualitative Health Research, 22(8), 1150–1159. https://doi.org/10.1177/1049732312448540
Miller, C. J., Grogan-Kaylor, A., Perron, B. E., Kilbourne, A. M., Woltmann, E., & Bauer, M. S. (2013). Collaborative chronic care models for mental health conditions: Cumulative meta-analysis and metaregression to guide future research and implementation. Medical Care, 51(10), 922–930. https://doi.org/10.1097/MLR.0b013e3182a3e4c4
Ministerio de Salud de Chile. (2000). Plan Nacional de Salud Mental y Psiquiatría. Gobierno de Chile.
Ministerio de Salud de Chile. (2006). Segundo Régimen de Garantías Explícitas en Salud. Gobierno de Chile.
Ministerio de Salud de Chile. (2013). Guía Clínica Depresión en personas de 15 años y más. Gobierno de Chile.
Ministerio de Salud de Chile. (2019). Orientaciones para la planificación y programación en red. Gobierno de Chile.
Minoletti, A., Rojas, G., & Horvitz-Lennon, M. (2012). Mental health in primary care in Chile: Lessons for Latin America. Cadernos Saúde Coletiva, 20, 440–447.
Mitchell, A. J., Rao, S., & Vaze, A. (2011). International comparison of clinicians’ ability to identify depression in primary care: Meta-analysis and meta-regression of predictors. British Journal of General Practice, 61(583), e72–e80. https://doi.org/10.3399/bjgp11X556227
Mitchell, A. J., Vaze, A., & Rao, S. (2009). Clinical diagnosis of depression in primary care: A meta-analysis. Lancet (London, England), 374(9690), 609–619. https://doi.org/10.1016/S0140-6736(09)60879-5
Moitra, M., Santomauro, D., Degenhardt, L., Collins, P. Y., Whiteford, H., Vos, T., & Ferrari, A. (2021). Estimating the risk of suicide associated with mental disorders: A systematic review and meta-regression analysis. Journal of Psychiatric Research, 137, 242–249. https://doi.org/10.1016/j.jpsychires.2021.02.053
Moussavi, S., Chatterji, S., Verdes, E., Tandon, A., Patel, V., & Ustun, B. (2007). Depression, chronic diseases, and decrements in health: Results from the World Health Surveys. Lancet (London, England), 370(9590), 851–858. https://doi.org/10.1016/S0140-6736(07)61415-9
Organización Panamericana de la Salud. (1972). Informe sobre la III reunión especial de Ministros de Salud y medidas necesarias para dar cumplimiento a las decisiones adoptadas. Organización Panamericana de la Salud – Organización Mundial de la Salud. https://iris.paho.org/handle/10665.2/5926
Pan American Health Organization. (2009). Strategy and plan of action on mental health. PAHO/WHO. https://iris.paho.org/handle/10665.2/33930
Patel, V., Saxena, S., Lund, C., Thornicroft, G., Baingana, F., Bolton, P., Chisholm, D., Collins, P. Y., Cooper, J. L., Eaton, J., Herrman, H., Herzallah, M. M., Huang, Y., Jordans, M. J. D., Kleinman, A., Medina-Mora, M. E., Morgan, E., Niaz, U., Omigbodun, O., et al. (2018). The Lancet Commission on global mental health and sustainable development. Lancet (London, England), 392(10157), 1553–1598. https://doi.org/10.1016/S0140-6736(18)31612-X
Patel, V., Simon, G., Chowdhary, N., Kaaya, S., & Araya, R. (2009). Packages of care for depression in low- and middle-income countries. PLoS Medicine, 6(10), e1000159. https://doi.org/10.1371/journal.pmed.1000159
Pence, B. W., O’Donnell, J. K., & Gaynes, B. N. (2012). The depression treatment cascade in primary care: A public health perspective. Current Psychiatry Reports, 14(4), 328–335. https://doi.org/10.1007/s11920-012-0274-y
Santomauro, D. F., Herrera, A. M. M., Shadid, J., Zheng, P., Ashbaugh, C., Pigott, D. M., Abbafati, C., Adolph, C., Amlag, J. O., Aravkin, A. Y., Bang-Jensen, B. L., Bertolacci, G. J., Bloom, S. S., Castellano, R., Castro, E., Chakrabarti, S., Chattopadhyay, J., Cogen, R. M., Collins, J. K., et al. (2021). Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic. The Lancet, 398(10312), 1700–1712. https://doi.org/10.1016/S0140-6736(21)02143-7
Saxena, S., Thornicroft, G., Knapp, M., & Whiteford, H. (2007). Resources for mental health: Scarcity, inequity, and inefficiency. Lancet (London, England), 370(9590), 878–889. https://doi.org/10.1016/S0140-6736(07)61239-2
Schumann, I., Schneider, A., Kantert, C., Löwe, B., & Linde, K. (2012). Physicians’ attitudes, diagnostic process and barriers regarding depression diagnosis in primary care: A systematic review of qualitative studies. Family Practice, 29(3), 255–263. https://doi.org/10.1093/fampra/cmr092
Smith, D. J., Court, H., McLean, G., Martin, D., Martin, J. L., Guthrie, B., Gunn, J., & Mercer, S. W. (2014). Depression and multimorbidity: A cross-sectional study of 1,751,841 patients in primary care. The Journal of Clinical Psychiatry, 75(11), 4205. https://doi.org/10.4088/JCP.14m09147
Stegenga, B. T., King, M., Grobbee, D. E., Torres-González, F., Švab, I., Maaroos, H.-I., Xavier, M., Saldivia, S., Bottomley, C., Nazareth, I., & Geerlings, M. I. (2012). Differential impact of risk factors for women and men on the risk of major depressive disorder. Annals of Epidemiology, 22(6), 388–396. https://doi.org/10.1016/j.annepidem.2012.04.011
Thota, A. B., Sipe, T. A., Byard, G. J., Zometa, C. S., Hahn, R. A., McKnight-Eily, L. R., Chapman, D. P., Abraido-Lanza, A. F., Pearson, J. L., Anderson, C. W., Gelenberg, A. J., Hennessy, K. D., Duffy, F. F., Vernon-Smiley, M. E., Nease, D. E., Williams, S. P., & Community Preventive Services Task Force. (2012). Collaborative care to improve the management of depressive disorders: A community guide systematic review and meta-analysis. American Journal of Preventive Medicine, 42(5), 525–538. https://doi.org/10.1016/j.amepre.2012.01.019
Üstün, T. B., & Sartorius, N. (1995). Mental illness in general health care: An international study. John Wiley & Sons.
Vanderlip, E. R., Rundell, J., Avery, M., Alter, C., Engel, C., Fortney, J., & Williams, M. (2016). Dissemination of integrated care within adult primary care settings: The collaborative care model. American Psychiatric Association and Academy of Psychosomatic Medicine.
Wang, P. S., Aguilar-Gaxiola, S., Alonso, J., Angermeyer, M. C., Borges, G., Bromet, E. J., Bruffaerts, R., de Girolamo, G., de Graaf, R., Gureje, O., Haro, J. M., Karam, E. G., Kessler, R. C., Kovess, V., Lane, M. C., Lee, S., Levinson, D., Ono, Y., Petukhova, M., et al. (2007). Use of mental health services for anxiety, mood, and substance disorders in 17 countries in the WHO world mental health surveys. Lancet (London, England), 370(9590), 841–850. https://doi.org/10.1016/S0140-6736(07)61414-7
World Health Organization. (1978). Primary health care: Report of the international conference on Primary Health Care, Alma-Ata, USSR, 6–12 September 1978: Jointly sponsored by the World Health Organization and the United Nations Children’s Fund. WHO.
World Health Organization. (2009). Mental health systems in selected low- and middle-income countries: A WHO-AIMS cross-national analysis (p. 103). World Health Organization. https://apps.who.int/iris/handle/10665/44151
World Health Organization. (2017). Depression and other common mental disorders: Global health estimates. World Health Organization.
World Health Organization. (2021). Mental health atlas 2020. World Health Organization. https://apps.who.int/iris/handle/10665/345946
World Health Organization, & World Organization of Family Doctors. (2008). Integrating mental health into primary care: A global perspective. WHO/WONCA.
Zhang, A., Franklin, C., Jing, S., Bornheimer, L. A., Hai, A. H., Himle, J. A., Kong, D., & Ji, Q. (2019). The effectiveness of four empirically supported psychotherapies for primary care depression and anxiety: A systematic review and meta-analysis. Journal of Affective Disorders, 245, 1168–1186. https://doi.org/10.1016/j.jad.2018.12.008
Acknowledgments
This work was supported by ANID – Millennium Science Initiative Program – ICS13_005, ANID – FONDECYT – 1180224, and U Redes Consolidación (Grant URC 007/18).
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2023 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Martínez, P., Rojas, G. (2023). Interventions for Adult Depression in Primary Health-Care Clinics. In: Martínez, V., Miranda-Castillo , C. (eds) Prevention and Early Treatment of Depression Through the Life Course. Depression and Personality. Springer, Cham. https://doi.org/10.1007/978-3-031-13029-8_7
Download citation
DOI: https://doi.org/10.1007/978-3-031-13029-8_7
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-13028-1
Online ISBN: 978-3-031-13029-8
eBook Packages: Behavioral Science and PsychologyBehavioral Science and Psychology (R0)