Abstract
Purpose
To assess the link between multimorbidity, type of chronic physical health problems and depressive symptoms
Method
The study was a cross-sectional postal survey conducted in 30 General Practices in Victoria, Australia as part of the diamond longitudinal study. Participants included 7,620 primary care attendees; 66% were females; age range from 18 to 76 years (mean = 51years SD = 14); 81% were born in Australia; 64% were married and 67% lived in an urban area. The main outcome measures include the Centre for Epidemiologic Studies Depression Scale (CES-D) and a study-specific self-report check list of 12 common chronic physical health problems.
Results
The prevalence of probable depression increased with increasing number of chronic physical conditions (1 condition: 23%; 2 conditions: 27%; 3 conditions: 30%; 4 conditions: 31%; 5 or more conditions: 41%). Only 16% of those with no listed physical conditions recorded CES-D scores of 16 or above. Across the listed physical conditions the prevalence of ‘probable depression’ ranged from 24% for hypertension; 35% for emphysema; 35% for dermatitis to 36% for stroke. The dose–response relationship is reduced when functional limitations and self-rated health are taken into account, suggesting that these factors mediate the relationship.
Conclusions
A clear dose–response relationship exists between the number of chronic physical problems and depressive symptoms. The relationship between multimorbidity and depression appears to be mediated via self-perceived health related quality of life. Primary care practitioners will identify more cases of depression if they focus on those with more than one chronic health problem, no matter what the problems may be, being especially aware in the group who rate their health as poor/fair.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Depression and physical illness commonly co-occur and depression is commoner in those with a chronic condition, as found in the large, worldwide WHO study [1]. There is growing interest in understanding the links between depression and physical illness, which are thought to be bi-directional [2, 3]; depression can increase the risk of the development of other health conditions through mechanisms such as lifestyle factors, poor health behaviours, delayed help-seeking and treatment non-compliance [4], and depression can develop subsequent to the diagnosis of a chronic health condition through physiological, pharmacological or psychological mechanisms [5–8] .
Studies are emerging which investigate the links between, for example, diabetes and depression [9] and asthma and depression [10, 11]. However, questions remain around whether the observed link is due to a particular condition (hence some common underlying biological pathway), the number of conditions, a particular combination of conditions or a common pathway through functional limitations. An analysis of a subsample of the European Study of the Epidemiology of Mental Disorders (ESEMeD) reported by Stegmann and Ormel et al. (2010) [2] suggests that previous studies may have overestimated the association between individual physical conditions and depression. They postulate that the association between physical conditions (which included arthritis, allergy, heart disease, hypertension, asthma, diabetes and stomach/duodenal ulcer) and depression can be explained by functional disability (which they measure as ‘days out of role’). Their finding, however, is limited to major depressive disorder and they were not able to account for the possible effect of antidepressant use.
Nevertheless, their finding is important and calls into question the current health policy focus in many countries on co-morbidity (a single condition such as diabetes or heart disease with depression). Added to this is the growing recognition and interest in the number of individuals experiencing multimorbidity, defined as any co-occurrence of two or more chronic medical conditions [12–15]. A recent systematic review reported a prevalence rate of 60% for multimorbidity, compared with rates for individual conditions of 6.5% for asthma, 29.6% for hypertension and 8.7% for diabetes [16] and a Dutch study reported that rates of multimorbidity doubled between 1985 and 2005 [13].
Multimorbidity complicates appropriate diagnosis and treatment and has been linked to greater utilization of health care services, reduced life expectancy and poorer health outcomes [13], yet our health care systems fail to address the needs of these patients [17]. From the patients’ perspective multimorbidity can have profound, detrimental effects on their ability to function physically, socially and psychologically [18], resulting in a reduction in quality of life [16, 19] and an increased risk of depression [19]. Depression and psychological distress in patients with multiple physical conditions may further increase the negative impact of those conditions by increasing pain and disability, and reducing compliance with treatment recommendations concerning medication and lifestyle changes. Multimorbidity is especially relevant in primary care where people attend for comprehensive health care and often present with a mix of undifferentiated physical and mental health symptoms and disabilities. Understanding the interplay between multimorbidity, functional limitations and self-rated health and depressive disorders in the primary care setting is crucial to developing more effective interventions for the growing number of people experiencing multiple physical and mental health conditions.
The aims of this study were to assess, in primary care attendees, the link between the number and type of chronic physical health problems and depressive symptoms and how this link might interact with functional limitations and self-rated health, taking into account the important potential confounder of antidepressant use.
Methods
Participant selection and screening procedures
The data reported here are from the diamond study; a large longitudinal study approved by The University of Melbourne’s Human Research Ethics Committee, conducted in Victoria, Australia, which focuses on depression in general practice. Full details have been reported earlier [20, 21]. Eligible GPs were approached from a randomised list generated by the Health Insurance Commission [22] until 30 agreed to take part. Practice staff, supported by a research assistant, searched the GPs’ computerised records to randomly sample 600 eligible patients from each of the 30 practices. Each eligible patient was sent a screening postal survey with a covering letter from their GP. A total of 7,667 (43.1%) patients returned their survey and form the sample for this study. A de-identified record of age and sex was available to determine the representativeness of the survey responders.
Measures
The Centre for Epidemiologic Studies Depression Scale (CES-D) is a 20-item scale designed to measure depressive symptoms experienced in the past week using a four point response scale [23]. Scores range from 0 to 60 with high scores indicating higher depressive symptoms. A cut-point of 16, indicating ‘probable clinical depression’ was used [23].
The survey also included a list of 12 common chronic physical conditions seen in Australian general practice and the National health priority areas [24, 25]: asthma, emphysema or other chronic lung problem, diabetes (high blood sugar), arthritis or any kind of rheumatism, back problems, chronic back pain or sciatica, hypertension (high blood pressure), chronic sinusitis, lipid disorder (high cholesterol), heart disease (angina, heart failure, heart attack), cancer (includes melanoma but not other skin cancer), stroke, and dermatitis. Respondents were asked to tick any listed chronic physical condition that they had experienced in the past 12 months. They then responded ‘Yes’ or ‘No’ to the following question: “Do you have any long-term illness, health problem or disability, which limits your daily activities or the work you can do (including problems that are due to old age)?”; and rated their health by answering the question: “In general, would you say your health is; Excellent, Very good, Good, Fair or Poor?” as self-rated health and functional limitations give an indication of perceived health-related quality of life. Participants were also asked whether they had experienced depression/and or anxiety in the past 12 months.
Statistical analysis
All analyses were conducted using STATA version 11 [26]. Data were summarised using frequencies and percentages for categorical data, and means and standard deviations (SD) for continuous data. Co-morbidity was defined as the total number of physical conditions experienced in the past 12 months across the 12 listed chronic physical conditions. The numbers of comorbid physical conditions experienced for each of the 12 listed conditions were summarised using quantiles. Multimorbidity was created using the total number of the 12 listed specific physical conditions. Logistic regression using generalised estimating equations with robust standard errors was used to examine the association between chronic physical conditions and depressive symptoms, allowing for the clustering effect due to recruiting participants from the same general practice, and controlling for the effects of age, sex, general practice location and additionally whether they were taking antidepressant medication. Results are reported as unadjusted and adjusted odds ratios (ORs) with 95% confidence intervals (CI) and p values (p). The Likelihood-ratio test was used to compare the logistic model treating the number of chronic conditions as a continuous variable against the logistic model treating the number of conditions as a categorical variable using dummy variables to look for evidence against linearity.
Results
Sample characteristics
The sample consisted of 7,620 participants, with 47 excluded from the analysis due to missing data on the chronic physical conditions. The majority of the sample were female (66% compared with 61% sent a survey) and ages ranged from 18 to 76 years (mean age of responders was 51 years (SD, 14.2) compared with the mean age of participants sent a survey 46.2 (SD, 15.3)). The majority of survey responders were born in Australia (81%) with 95% indicating that English was their first language. The majority were married (64%), without post-secondary education (57%), with two-thirds (67%) living in an urban area (Table 1).
Prevalence of chronic health conditions
Table 2 shows the number and percentage of participants that reported experiencing any of the 12 listed chronic physical conditions in the past 12 months, the percentage with multimorbidity, the median number of comorbid chronic physical conditions, proportion of females and mean age for each condition. The most commonly reported chronic physical condition was back problems (28%) followed by arthritis (18%) and hypertension (17%). Almost one-quarter (24%) reported depression and/or anxiety in the past 12 months.
Measuring multimorbidity
Figure 1 shows how we sampled participant data for this paper. Overall, 42.6% of respondents (3,247/7,620) did not experience any of the 12 listed chronic physical conditions in the past 12 months. Of these 3,247 participants, 679 reported having a long-term illness or disability limiting their activity, yet we were not able to discern the nature or number of long-term conditions they were experiencing. In addition, 77 participants who did not experience any of the 12 listed chronic physical conditions did not record a response to the question about long-term illness or disability limiting their activity. Hence, these participants were not included in the analysis of multimorbidity reported in Tables 3, 4 and 5 which is based only upon the responses from the remaining 6,864 participants (Fig. 1).
31% (2,154/6,864) reported two or more chronic physical conditions, with 2.4% reporting five or more of the listed conditions. Of the participants reporting at least one condition (n = 4,373), 49% (n = 2,154) were multimorbid. The multimorbidity rates were higher among the older age group (65+ years), with 47% (245/524) of males and 50% (341/676) of females reporting two or more chronic physical conditions (Table 3). 4% of this older age group reported five or more conditions, compared with less than 1% among the youngest age group (18–44 years). Among the older age group with at least one chronic condition, 61% (245/401) of males and 65% (341/527) of females were multimorbid.
Depressive symptoms across physical conditions and multimorbidity
The percentage of participants recording CES-D scores ≥16 (indicating probable depression) was identified for the 12 listed chronic physical conditions (Table 6). For respondents reporting a chronic physical condition, the prevalence of ‘probable depression’ ranged from a low of 24% (hypertension) to a high of 36% (stroke). Participants reporting dermatitis and emphysema (35%) also recorded high levels of depressive symptoms.
The results of the logistic regression model comparing the odds of probable depression for participants with and without each of the listed chronic physical conditions are shown in Table 6. Adjusted analyses show strong evidence for an association between depressive symptoms and each chronic physical condition (p value < 0.001), except for cancer (p value = 0.16) and hypertension (p = 0.08).
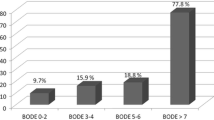
Multimorbidity was also associated with higher odds of probable depression. For participants classified within the group ‘no chronic physical condition’, only 16% recorded CES-D scores ≥16. While 23% of respondents reporting one chronic physical condition recorded CES-D scores ≥16, over 40% of respondents reporting five or more chronic physical conditions recorded CES-D scores indicating probable depression. There was a strong association between depressive symptoms and the number of chronic physical conditions reported (Table 4 and Fig. 2). As the likelihood-ratio test showed weak evidence against linearity (p = 0.02 for the unadjusted analysis and p = 0.01 for the adjusted analysis) odds ratios are reported for each of the multimorbidity levels compared with the reference group participants who did not list any chronic physical condition or functional limitation. With each increase in the number of reported chronic physical conditions, the odds of experiencing depressive symptoms became more likely, up to four times in cases where five or more physical conditions were reported compared with none. When we additionally adjusted multimorbidity for the functional limitations or self-rated health, substantial decreases in the associations (odds ratios) with depressive symptoms were observed. However, statistically significant associations of multimorbidity with depressive symptoms remained (Table 4), indicating that condition count is independently associated with depressive symptoms, yet suggesting that it is also mediated via functional limitations and self-rated health.
Depressive symptoms across chronic physical conditions limited to one organ system
We also investigated whether there was a link between conditions grouped by ‘organ system’ and depressive symptoms. We combined chronic physical conditions into the appropriate organ system groups. The cardiovascular system groups together stroke, heart disease, lipid disorder and hypertension. The musculoskeletal system groups together back problems and arthritis. Chronic physical conditions related to the respiratory system includes emphysema, chronic sinusitis and asthma. Skin as an organ system only comprised of dermatitis and diabetes the only condition related to the endocrine system. All of the organ system types were independently and significantly related to depressive symptoms. Statistically significant adjusted odds ratios for all organ systems linked conditions ranged from 1.28 (cardiovascular) to 1.84 (endocrine). (Tables available on request).
We additionally adjusted for the presence of each ‘organ system’ group condition. No substantial decreases in the association with depressive symptoms were observed, except for cardiovascular system (OR = 1.10, p = 0.94). When controlling for functional limitations and self-rated health there was a decrease in all odds ratios; most striking was the decrease in the odds of association for the cardiovascular conditions. The only organ systems that remained statistically significant were musculoskeletal (adjusted OR = 1.25, p < 0.001, 95% CI (1.10–1.42)) and skin (adjusted OR = 1.41, p < 0.001, 95% CI (1.17–1.69)).
Health rate and long-term illness or disability limiting activity and its effect on depressive symptoms
Table 5 shows the proportion of participants with each number of chronic physical conditions who reported long-term illness or disability limiting their daily activities. Almost 72% of participants with four chronic conditions and over 71% of respondents with five chronic conditions reported long-term illness or disability limiting their daily activities. These groups also recorded the highest proportion of participants with a ‘poor’ or ‘fair’ health rating (42 and 54% respectively).
Figure 3 details the proportion of cases with health rated as ‘poor’ and long-term illness or disability limiting activity across each of the number of chronic physical conditions. Among the participants with five or more chronic conditions, approximately 75% experienced long-term illness or disability limiting activity and 17% rated their health as ‘poor’.
Self-rated health was strongly associated with depressive symptoms (adjusted OR = 4.80; 95% CI 4.12–5.59; p < 0.001). Also, there was a strong association between functional limitations and depressive symptoms (adjusted OR = 2.74, 95% CI (2.38–3.15) p < 0.001). As presented in the previous section multimorbidity was strongly associated with depressive symptoms and this relationship was statistically significant. However, controlling for functional limitations or self-rated health reduced the observed odds ratios and the associations with depressive symptoms substantially decreased. As depressive symptoms were strongly and statistically significantly associated with self-rated health and functional limitations, it appears that self-rated health and functional limitations may play a mediating role in the relationship between multimorbidity and depressive symptoms (Fig. 4) suggesting that the number of co-occurring conditions also affects depressive symptoms indirectly through the impact on perceived health-related quality of life [27].
Discussion
In this paper we have shown a clear dose–response relationship between the number of chronic physical health problems (multimorbidity) and depressive symptoms, and we have shown how this link may also be mediated via perceived health-related quality of life. This is the largest scale study to our knowledge that reports such a dose–response relationship across a wide range of chronic physical conditions and our findings build upon those previously reported [1, 2]. The finding that probable depression is as much linked to problems such as dermatitis, as it is to diabetes and heart disease, calls into question the usefulness of the current strong focus on a particular disease association such as diabetes and depression in the primary care setting. The clear dose–response relationship suggests that primary care practitioners will identify more cases of depression if they focus on those with more than one chronic health problem, no matter what the problems may be.
We have also examined the way in which multimorbidity, specific organ system conditions, functional limitations and self-rated health are associated with depressive symptoms. Although our regression analysis shows that the dose–response relationship loses robustness when adjustment is made for either functional limitations or self-rated health, we have clearly demonstrated that multimorbidity and depressive symptoms are strongly linked to functional limitations and self-rated health. This suggests that multimorbidity and depressive symptoms are partially mediated by health-related quality of life: functional limitations and self-rated health. We put forward that this is a more clinically useful way of thinking about the link between multiple chronic health conditions and depression, rather than postulating that one of these factors is more important than the other. The next step will be to explore this possible partial mediation using more sophisticated statistical analysis techniques such as structural equation modelling or logistic regression with binary mediation using the product of coefficients approach allowing for computing the direct and indirect effects.
The strengths of this study are the large and representative sample size, the focus on 12 common and chronic physical conditions that form a large component of disease burden and our use of a well validated measure for depressive symptoms. The response rate of 43.1% to the initial mail-out survey may be seen as a study limitation; yet it is consistent with responses rates from other well conducted large-scale primary care studies investigating depression [28], including the international PREDICT study being conducted in six European countries [29].
Both the chronic physical conditions checklist and the depression scale (CES-D) used in this study are self-report measures, introducing the potential for inaccuracies due to either under- or over-reporting of conditions. Self-report measures are, however, used extensively in the health and medical literature and a number of studies have suggested reasonable concordance between patient self-report and physician diagnoses or laboratory reports [30, 31]. Whilst medical records are a source for patient data on encounters/diagnoses, information recorded often differs from patient self-reported conditions due to differences in illness behaviour and practice variation of the GP [32]. We have measured multimorbidity using a simple count of the number of chronic physical conditions reported by our participants from a specified list of 12 common physical conditions. The use of counts may be seen as a limitation by some [19] who advocate for the use of sophisticated scales to assess multimorbidity, taking into account the severity of the health condition (e.g. Cumulative Illness Rating Scale [33]). We argue that these more complex and time-consuming measures have a place in research settings but are limited in the way the findings can be applied in the routine clinical encounter.
More research is clearly needed into the prevalence and impact of multimorbidity, recognizing the complexity of the issue and identifying factors that may serve to either increase or decrease its detrimental effects.
Conclusion
A substantial proportion of patients attending primary care health settings have at least one chronic physical condition, with many being multimorbid. Primary care practitioners should have a raised awareness for depression in any patient that reports a common chronic physical condition and be especially aware in those who report two or more, and particularly so for those whom also report functional limitations or poor/fair self-rated health.
Ethical approval: Ethical approval for the study was obtained from The University of Melbourne Human Research Ethics Committee (Ethics ID: 030613).
References
Moussavi S, Chatterji S, Verdes E, Tandon A, Patel V, Ustun B (2007) Depression, chronic diseases, and decrements in health: results from the World Health Surveys. Lancet 370:851–858
Stegmann ME, Ormel J, de Graaf R, Haro JM, de Girolamo G, Demyttenaere K, Kovess V, Matschinger H, Vilagut G, Alonso J (2010) Functional disability as an explanation of the associations between chronic physical conditions and 12-month major depressive episode. J Affect Disord 124:38–44
Ormel J, FhV Rijsdijk, Sullivan M, van Sonderen E, Kempen GIJM (2002) Temporal and reciprocal relationship between IADL/ADL disability and depressive symptoms in late life. J Gerontol B Psychol Sci Soc Sci 57:P338–P347
Prince M, Patel V, Saxena S, Maj M, Maselko J, Phillips MR, Rahman A (2007) No health without mental health. Lancet 370:859–877
Koopmans G, Lamers L (2005) Assessing the construct validity of three indicators of psychological distress in relation to perceived health and physical illness. Soc Psychiatry Psychiatr Epidemiol 40:1012–1018
Patten SB, Williams JVA (2007) Assessment of physical etiologies for mood and anxiety disorders in structured diagnostic interviews. Soc Psychiatry Psychiatr Epidemiol 42:462–466
Dowrick C (2006) Chickens and eggs: examining the links between mental health and chronic disease. Intern J Psychiatry Med 36:263–267
Dowrick C, Katona C, Peveler R, Lloyd H (2005) Somatic symptoms and depression: diagnostic confusion and clinical neglect. Br J Gen Pract 55:829–830
Musselman DL, Betan E, Larsen H, Phillips LS (2003) Relationship of depression to diabetes types 1 and 2: epidemiology, biology, and treatment. Biol Psychiatry 54:317–329
Oga T, Nishimura K, Tsukino M, Sato S, Hajiro T, Mishima M (2007) Analysis of longitudinal changes in the psychological status of patients with asthma. Respir Med 101:2133–2138
Opolski M, Wilson I (2005) Asthma and depression: a pragmatic review of the literature and recommendations for future research. Clin Prac Epidemiol Ment Health 1:18
Fortin M, Soubhi H, Hudon C, Bayliss EA, van den Akker M (2007) Multimorbidity’s many challenges. BMJ Clinical research ed 334:1016–1017
Uijen AA, van de Lisdonk EH (2008) Multimorbidity in primary care: prevalence and trend over the last 20 years. Eur J Gen Pract 14(Suppl 1):28–32
van den Akker M, Buntinx F, Knottnerus A (1996) Comorbidity or multimorbidity: what’s in a name? A review of literature. Eur J Gen Pract 2:65–70
Britt HC, Harrison CM, Miller GC, Knox SA (2008) Prevalence and patterns of multimorbidity in Australia. Med J Aus 189:72–77
Fortin M, Lapointe L, Hudon C, Vanasse A, Ntetu AL, Maltais D (2004) Multimorbidity and quality of life in primary care: a systematic review. Health Qual Life Outcomes 2:51
Wright N, Smeeth L, Heath I (2003) Moving beyond single and dual diagnosis in general practice: many patients have multiple morbidities, and their needs have to be addressed. BMJ (Clinical research ed) 326:512–514
van den Akker M, Buntinx F, Metsemakers JF, Roos S, Knottnerus JA (1998) Multimorbidity in general practice: prevalence, incidence, and determinants of co-occurring chronic and recurrent diseases. J Clin Epidemiol 51:367–375
Fortin M, Bravo G, Hudon C, Lapointe L, Dubois MF, Almirall J (2006) Psychological distress and multimorbidity in primary care. Ann Fam Med 4:417–422
Gunn JM, Gilchrist GP, Chondros P, Ramp M, Hegarty KL, Blashki GA, Pond DC, Kyrios M, Herrman HE (2008) Who is identified when screening for depression is undertaken in general practice? Baseline findings from the diagnosis, management and outcomes of depression in primary care (diamond) longitudinal study. Med J Aus 188:S119–S125
Potiriadis M, Chondros P, Gilchrist G, Hegarty K, Blashki G, Gunn JM (2008) How do Australian patients rate their general practitioner? A descriptive study using the general practice assessment questionnaire. Med J Aus 189:215–219
Calcino G (1993) Sampling from the HIC data set. In: Calcino G (ed) Proceedings from the General Practice Evaluation Program 1993 work-in-progress conference. Department of Health, Housing, Local Government and Community Services, Canberra
Radloff L (1977) The CES-D scale: a self-report depression scale for research in the general population. Appl Psychol Meas 1:385–401
Britt H, Miller G, Charles J, Bayram C, Pan Y, Henderson J, Valenti L, O’Halloran J, Harrison C, Fahridin S (2008) General practice activity in Australia 2006–07. General practice series no 21 Cat no GEP 21. AIHW, Canberra
Australian Institute of Health and Welfare (2008) Australia’s Health 2008. AIHW, Canberra
StataCorp. (2009) Stata Statistical Software: Release 11. StataCorp LP, College Station, Texas
MacKinnon DP, Lockwood CM, Hoffman JM, West SG, Sheets V (2002) A comparison of methods to test mediation and other intervening variable effects. Psychol Methods 7:83–104
Gilchrist G, Gunn J (2007) Observational studies of depression in primary care: What do we know? BMC Fam Pract 8:28
Zuithoff NPA, Vergouwe Y, King M, Nazareth I, Hak E, Moons KGM, Geerlings MI (2009) A clinical prediction rule for detecting major depressive disorder in primary care: the PREDICT-NL study. Fam Pr 26:241–250
Simpson CF, Boyd CM, Carlson MC, Griswold ME, Guralnik JM, Fried LP (2004) Agreement between self-report of disease diagnoses and medical record validation in disabled older women: factors that modify agreement. J Am Geriatr Soc 52:123–127
Kriegsman DM, Penninx BW, van Eijk JT, Boeke AJ, Deeg DJ (1996) Self-reports and general practitioner information on the presence of chronic diseases in community dwelling elderly. A study on the accuracy of patients’ self-reports and on determinants of inaccuracy. J Clin Epidemiol 49:1407–1417
Kolk AMM, Hanewald G, Schagen S, Gijsbers van Wijk CMT (2002) Predicting medically unexplained physical symptoms and health care utilization: a symptom-perception approach. J Psychosom Res 52:35–44
Linn BS, Linn MW, Gurel L (1968) Cumulative illness rating scale. J Am Geriatr Soc 16:622–626
Acknowledgments
The diamond study was funded by the National Health and Medical Research Council (ID 299869, 454463 & 566511) and the Victorian Centre for Excellence in Depression and Related Disorders, an initiative between beyondblue and the Victorian Government. Neither funding body had a role in study design; the collection, analysis, and interpretation of data; the writing of the manuscript; or the decision to submit this manuscript for publication. The listed authors submit this paper on behalf of the diamond project team, including the investigators and researchers involved in the study: A/Professor Kelsey Hegarty, Dr Grant Blashki, Dr Gail Gilchrist, Professor Michael Kyrios, Professor Dimity Pond, Ms Vanessa Madden, Dr David Pierce, Ms Maria Potiriadis, Ms Melina Ramp, Dr Lena Sanci, Dr Jane Sims, Ms Donna Southern, and the casual research staff. We are grateful to the thirty dedicated GPs, their patients and practice staff for making this research possible.
Conflict of interest
All authors declare that the answer to the questions on competing interest form are all ‘No’ and therefore have nothing to declare.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Gunn, J.M., Ayton, D.R., Densley, K. et al. The association between chronic illness, multimorbidity and depressive symptoms in an Australian primary care cohort. Soc Psychiatry Psychiatr Epidemiol 47, 175–184 (2012). https://doi.org/10.1007/s00127-010-0330-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00127-010-0330-z