Abstract
Cognitive decline, both due to ageing or disease, presents one of Western societies’ most significant disease burdens. Personalized preventive actions and public health interventions and policies can contribute to the prevention of dementia and healthy ageing. Nutrition is an integral part of the exposome, acting either as a risk factor or preventive intervention. Precision nutrition approach for prevention of cognitive decline involves the ability to profile the population for the risk of dementia, knowledge of the impact of nutrients and dietary patterns on biological processes involved in the pathogenesis of cognitive decline and the ability to predict individual heterogeneity response to diet. Genetic factors, either as rare monogenic causes or polygenic risk scores and known risk factors for dementia, can be used to assess the individual risk for dementia. In addition, several nutrients and dietary patterns influencing common mechanisms involved in dementia pathogenesis like oxidative stress, neuroinflammation, and hypoxia have been investigated as potential preventive interventions—the evidence is still accumulating. Finally, genomic variation, epigenetics, and microbiome have been proposed to modulate individual response to diet, and different »omic« surrogate biomarkers could improve the monitoring of individual response to nutrition. Large population data sets covering comprehensive information on mentioned variables are needed for the system medicine approach to dementia prevention. In addition, there is an urgent need for standardization of the methodological inventory and study design on the international level for that purpose.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
8.1 Introduction
The cognitive decline that progresses to dementia is currently the fifth most significant contributor to the global burden of disease (Prince et al. 2015)) and substantially affects patients’ lives, their families, and society. It affects around 1% of the population aged 30–64 years (Hendriks et al. 2021). Due to the ageing population worldwide, it is projected that the prevalence will triple by 2050 (Collaborators et al. 2016); therefore, dementia is considered a global public health priority. It was estimated that a five-year delay in the onset of dementia would reduce the number of people with a disease by 33–50% by 2050 (Jennings et al. 2020).
Dementia is not a specific disease but rather an overarching term to describe a group of symptoms affecting memory, thinking, and social abilities which interfere with daily life. It is associated with several distinct diseases with different aetiology and pathophysiology. Alzheimer disease is the most common cause, followed by vascular dementia, dementia with Lewy bodies, frontotemporal degeneration, and dementias associated with brain injury, infections, alcohol abuse, and genetic causes. Different entities are associated with specific etiological factors and neuropathologic hallmarks, while etiological factors and neuropathologic signs are often shared among dementias (Raz et al. 2015). Alzheimer’s disease is characterized by the extracellular accumulation of senile plaques composed of a peptide and intraneuronal accumulation of neurofibrillary tangles composed of hyperphosphorylated microtubule-binding protein-tau. Vascular dementia is a heterogeneous disorder associated with endothelial dysfunction, atherosclerosis, small vessel disease, ischemia, and haemorrhage. Dementia with Lewy bodies is characterized by abnormal aggregation of the synaptic protein alpha-synuclein, while frontotemporal dementia may be associated with either cellular p-tau inclusions, ubiquitin-positive tau-negative neuronal inclusions, or neurodegeneration without ubiquitin or tau inclusions. There is significant heterogeneity in the comorbidity, and the cognitive impact of age-related neuropathology and mixed neuropathologies is the most common cause of dementia in the population (Boyle et al. 2021). Thus, the contribution of neuropathologies to cognitive decline is person-specific which has an essential impact on prevention strategies (Boyle et al. 2018).
Common mechanisms involved in dementias include neuroinflammation, neurodegeneration, autophagy, hypoxia with cerebrovascular dysfunction, blood–brain barrier dysfunction, and oxidative stress (Raz et al. 2015; Dominguez and Barbagallo 2018). Equally important for designing preventive interventions are functional pathways associated with cognitive resilience, including inflammation, amyloid degradation, memory function, and neurotransmission (Pérez-González et al. 2021).
Understanding pathology and mechanisms associated with cognitive decline provides a basis for prevention. In addition to public health interventions and policies, personalized preventive actions can contribute to dementia prevention. Preliminary evidence has not demonstrated that population screening for dementia had clear benefits or harm in quality of life, mood, or improved diagnostics (Fowler et al. 2020). Therefore, individualized strategies to identify risk factors and planning intervention strategies are expected to impact future prevention significantly.
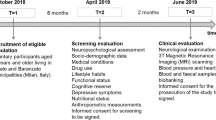
Precision nutrition interventions could impact several biological processes involved in the pathogenesis of cognitive decline one hand. Also, there is individual heterogeneity in response to diet. To explore the potential individualized nutritional interventions, we will discuss current evidence of dietary effects on cognition, individual differences in response to nutrition in the context of cognition, as well as our understanding of risk factors for dementia which could lead to an assessment of individualized risk for dementia or stratification individuals for precision nutrition interventions (Fig. 8.1).
8.2 Nutrients and Dietary Patterns
Many nutritions are associated with mechanisms and risk factors for cognitive decline and dementia. However, most of the evidence linked to potential interventions is still lacking or is contradictory. Moreover, in several cases, potential favourable effects are limited to specific subpopulations, which requires further scientific confirmation and stipulates the potential of individualized nutritional interventions.
8.2.1 Antioxidants
The contribution of oxidative stress to neurodegenerative disorders is not clearly understood, and several mechanisms have been proposed (Cobley et al. 2018). The primary antioxidant defences include vitamin C, vitamin E, carotenoids, flavonoids, and polyphenols.
The meta-analysis demonstrated low-certainty evidence for a positive effect of vitamin C and carotenoids on overall cognitive function (Rutjes et al. 2018). A recent meta-analysis of randomized intervention trials suggested that carotenoids are associated with better cognitive performance (Davinelli et al. 2021). Furthermore, there is partial evidence of synergism between carotenoids and vitamin E regarding basic cognitive performance (Beydoun et al. 2020). The results on vitamin E impact on cognition have been mixed (Lakhan et al. 2021).
Flavonoids were associated with a beneficial effect for maintaining cognitive function (Yeh et al. 2021; Gardener et al. 2021).
Similarly, polyphenols have been reported to improve cognitive function in both healthy middle-aged volunteers and students (Philip et al. 2019; Carrillo et al. 2021).
8.2.2 Vitamins
Both vitamin B12 and vitamin B6 are involved in the metabolism of homocysteine. Most systematic reviews showed no overall evidence that oral B vitamin supplementation prevented cognitive decline (Rutjes et al. 2018; Behrens et al. 2020; Markun et al. 2021). Pooled post hoc analysis of two randomized clinical trials showed that B vitamins had favourable effects on global cognitive functioning and whole-brain atrophy in older people with mild cognitive impairment (Wu et al. 2021). Furthermore, a combination of B6 and B12, folate, and n-3 fatty acids contributed to preserving semantic memory in a subgroup of women and men with previous coronary artery disease or ischaemic stroke aged 45–80 years in a randomized clinical trial (Andreeva et al. 2011).
Observational studies on folic acid supplementation provided mixed results (Scarmeas et al. 2018). A recent randomized clinical trial provided evidence that combining folic acid and docosahexaenoic acid therapy might improve cognitive function and reduce Aβ production in patients with mild cognitive impairment (Bai et al. 2021).
Few evidence on vitamin D supplementation demonstrated no significant effect on cognition; there is some evidence of modest effect in older black adults (Kang et al. 2021).
8.2.3 Omega-3 Fatty Acids
Randomized clinical trials reported mixed findings with supplementation of docosahexaenoic acid (DHA), however, in the LipiDiDiet trial Souvenaid (medicinal food with docosahexaenoic acid as one of the bioactive ingredients) improved clinical dementia rating score (Soininen et al. 2017). Recently, it was suggested that the supplementation of eicosapentaenoic acid but not DHA improved global cognitive function (Patan et al. 2021), while no treatment effect was found after omega-3 supplementation in young adults (Marriott et al. 1854). Combining DHA and folic acid therapy might be more beneficial in improving cognitive function and reducing Aβ-related biomarkers in older adults with mild cognitive impairment (Bai et al. 2021).
8.2.4 Dietary Patterns
Due to the complex interactions among different nutrients on one side and complex evolution of cognitive decline on the other, dietary patterns rather than single nutrients could better address the therapeutic potential of nutrients. Three dietary patterns were most extensively studied with cognitive decline: Mediterranean diet, dietary approaches to stop hypertension (DASH) and Mediterranean—DASH intervention for neurodegenerative delay (MIND).
While several observational studies reported beneficial effects of mostly Mediterranean and MIND diets on cognition, few randomized controlled trials with mixed results do not provide conclusive evidence (Duplantier and Gardner 2021). Furthermore, standardized approaches are needed both for nutrition and cognitive assessment (Scarmeas et al. 2018; Duplantier and Gardner 2021).
8.3 Individualized Response to Diet
There is considerable individual variation in how nutrients and food-derived bioactive molecules are absorbed and metabolized in humans. Understanding and assessing this variation may lead to better dietary recommendations and personalized dietary interventions. Sources for metabolic heterogeneity may include the human genome, epigenome, and microbiome (Zeisel 2020).
8.3.1 Human Genome
Genetic variation in the human genome may be associated with differential responses to nutrients (nutrigenetics). Few studies were addressing nutrigenetic implications in cognitive disfunction. In four studies, a healthy lifestyle including diet, fatty fish consumption, fruits and vegetables, and moderate intake of polyunsaturated fats were associated with reduced dementia risk (Samieri et al. 2021). Additionally, genetic variation in the MTHFR gene was associated with the total plasma homocysteine concentrations following B vitamin supplementation in the SU.FOL.OM3 trial (Fezeu et al. 2018). Polymorphisms in genes involved in vitamin uptake, transport, and metabolism were associated with vitamin status (Niforou et al. 2020). Similarly, data on the genetic variation of antioxidant enzymes relevant to nutritional components accumulate (Birk 2021).
8.3.2 Epigenome
The field of epigenetics is concerned with changes in gene expression that are not related to changes in DNA sequence. Epigenetic control of gene expression involves several mechanisms, including DNA methylation and hydroxymethylation, histone modifications, non-protein-coding RNA molecules, RNA editing, chromatin remodelling, and telomere control. Epigenetic marks are reversible and influenced by several environmental factors, including nutrition, infections, chemicals, stress and age, to name only a few.
Some dietary factors, such as folate, vitamins B6 and B12, choline and methionine, are involved in metabolic pathways directly related to DNA methylation. However, diet effects also other epigenetic mechanisms, such as histone modifications and non-coding RNAs (Dauncey 2014). Consequently, dietary factors such as deficiency in folate, vitamins B6 and B12 effect cognition via alterations in DNA methylation or in the case of vitamins A, E and C via histone acetylation (Polverino et al. 2021).
8.3.3 Microbiome
The microbiome is involved in nutrient metabolism and releases specific diet-microbial metabolites in the gut and the bloodstream. These include neurotransmitters, pro-inflammatory factors, and short-chain fatty acids. There are marked person-specific diet-microbiome interactions in the population, and thus, the gut microbiome contributes to the variation of subject-specific responses to diet (Leshem et al. 2020). In addition, several gut-derived metabolites linked to the brain metabolism, which are associated with specific diet—bacterial strains interactions, were identified (Samieri et al. 2021).
8.4 Risk Factors for Dementia
Risk factors for dementia include both nonmodifiable such as age, sex, and genetic predisposition as well as modifiable risk factors including less education, hypertension, hearing impairment, smoking, obesity, depression, physical inactivity, diabetes, low social contact, excessive alcohol consumption, traumatic brain injury, and air pollution (Livingston et al. 2020).
While diabetes and obesity may present direct targets for nutritional prevention or intervention and will be discussed in the next chapter, genetic predisposition may be used to estimate the risk of developing the disease. Moderately raised concentrations of homocysteine were reported to be associated with an increased risk of dementia in men and women over 65 years (Smith et al. 2018). It has been estimated that 25% of individuals aged 55 years and older have a family history of dementia (Loy et al. 2014) which might be associated with a monogenic or polygenic predisposition and complex interactions with environmental factors.
Monogenic forms of dementia may be due to pathogenic genetic variations in the APP, PSEN1 and PSEN2 genes related to Alzheimer disease, MAPT, GRN, C9orf72, CHMP2B, FUS, VCP, SQSTM1, OPTN, UBQLN2 and TBK1 genes related to frontotemporal dementia, NOTCH3, GLA, TREX1, COL4A1 and HTRA1 genes associated with the vascular type of dementia, and more than 168 genes related to rare syndromic forms of dementia (Huq et al. 2021). In addition to rare monogenic forms of dementia, polygenic risk scores can be used to predict the risk of developing dementia, as has been shown for Alzheimer disease (Rojas et al. 2021; Escott-Price et al. 2017; Leonenko et al. 2021).
Prognostic models may assess different risk factors and provide the likelihood that an individual will develop dementia; however, there is no golden standard to evaluate the dementia risk yet (Geethadevi et al. 2021; Goerdten et al. 2019).
8.5 Challenges and Future Directions
Presented data show evidence that, on the one hand, evidence is accumulating about the effects of nutrition on pathological processes involved in cognitive decline and for the assessment of individual responses to diet as well as risks for developing dementia. On the other hand, current evidence is mainly based on a single or small number of observed interactions. We are just at the beginning of understanding single elements that are part of much more complex and heterogeneous networks, necessary to understand and model in order to design comprehensive dietary interventions for an individualized approach to cognitive decline prevention (Ommen et al. 2017; Ebaid and Crewther 2020).
To advance the field, comprehensive data on multiple combinations of nutrition exposures for different, specific domains of cognitive function are needed (Samieri et al. 2021). High throughput technologies will provide several levels of nutrigenomic biomarkers, including transcriptomic, proteomic, metabolomic, lipidomic, and immunomic, which will provide data for a systems approach to understanding nutritional effects on molecular pathways. At the same time, data on potential sources influencing metabolic heterogeneity in response to nutrition, including individual genetic and microbiome data, should be available to personalize intervention strategies. Furthermore, tools for dementia risk assessment based on a combination of risk factors will provide information on individualized risk for cognitive decline to inform precision nutrition interventions. Finally, due to the heterogeneous and complex aetiology and pathogenesis of cognitive decline, precision nutrition is one of the multidomain interventions, which should simultaneously target several risk factors and mechanisms to achieve optimal preventive effects (Solomon et al. 2021).
Large cohorts from different world populations, standardized study designs, and analytical methods are needed to provide adequate power for evidence-based recommendations.
References
Andreeva VA, Kesse-Guyot E, Barberger-Gateau P, Fezeu L, Hercberg S, Galan P (2011) Cognitive function after supplementation with B vitamins and long-chain omega-3 fatty acids: ancillary findings from the SU.FOL.OM3 randomized trial. Am J Clin Nutr 94:278–86
Bai D, Fan J, Li M, Dong C, Gao Y, Fu M, Huang G, Liu H (2021) Effects of folic acid combined with DHA supplementation on cognitive function and amyloid-β-related biomarkers in older adults with mild cognitive impairment by a randomized, double blind. Placebo-controlled trial. J Alzheimer’s Dis 81:155–167
Behrens A, Graessel E, Pendergrass A, Donath C (2020) Vitamin B—can it prevent cognitive decline? A systematic review and meta-analysis. Syst Rev 9:111
Beydoun MA, Canas JA, Fanelli-Kuczmarski MT, Maldonado AI, Shaked D, Kivimaki M, Evans MK, Zonderman AB (2020) Association of antioxidant vitamins A, C, E and carotenoids with cognitive performance over time: a cohort study of middle-aged adults. Nutrients 12:3558
Birk R (2021) Nutrigenetics of antioxidant enzymes and micronutrient needs in the context of viral infections. Nutr Res Rev 34:174–184
Boyle PA, Yu L, Wilson RS, Leurgans SE, Schneider JA, Bennett DA (2018) Person-specific contribution of neuropathologies to cognitive loss in old age. Ann Neurol 83:74–83
Boyle PA, Wang T, Yu L, Wilson RS, Dawe R, Arfanakis K, Schneider JA, Bennett DA (2021) To what degree is late life cognitive decline driven by age-related neuropathologies? Brain 144:awab092
Carrillo JÁ, Arcusa R, Zafrilla MP, Marhuenda J (2021) Effects of fruit and vegetable-based nutraceutical on cognitive function in a healthy population: placebo-controlled, double-blind, and randomized clinical trial. Antioxidants 10:116
Cobley JN, Fiorello ML, Bailey DM (2018) 13 reasons why the brain is susceptible to oxidative stress. Redox Biol 15:490–503
Collaborators GD, Nichols E, Szoeke CEI, Vollset SE, Abbasi N, Abd-Allah F, Abdela J, Aichour MTE, Akinyemi RO, Alahdab F et al (2016) Global, regional, and national burden of Alzheimer’s disease and other dementias, 1990–2016: a systematic analysis for the Global Burden of disease study 2016. Lancet Neurol 18:88–106
Dauncey MJ (2014) Nutrition, the brain and cognitive decline: insights from epigenetics. Eur J Clin Nutr 68:1179–1185
Davinelli S, Ali S, Solfrizzi V, Scapagnini G, Corbi G (2021) Carotenoids and cognitive outcomes: a meta-analysis of randomized intervention trials. Antioxidants 10:223
de Rojas I, Moreno-Grau S, Tesi N, Grenier-Boley B, Andrade V, Jansen IE, Pedersen NL, Stringa N, Zettergren A, Hernández I et al (2021) Common variants in Alzheimer’s disease and risk stratification by polygenic risk scores. Nat Commun 12:3417
Dominguez LJ, Barbagallo M (2018) Nutritional prevention of cognitive decline and dementia. Acta Bio-Medica Atenei Parmensis 89:276–290
Duplantier SC, Gardner CD (2021) A critical review of the study of neuroprotective diets to reduce cognitive decline. Nutrients 13:2264
Durga J, van Boxtel MP, Schouten EG, Kok FJ, Jolles J, Katan MB, Verhoef P (2007) Effect of 3-year folic acid supplementation on cognitive function in older adults in the FACIT trial: a randomized, double blind, controlled trial. Lancet 369:208–216
Ebaid D, Crewther SG (2020) Time for a systems biological approach to cognitive aging?—a critical review. Front Aging Neurosci 12:114
Escott-Price V, Myers AJ, Huentelman M, Hardy J (2017) Polygenic risk score analysis of pathologically confirmed Alzheimer disease. Ann Neurol 82:311–314
Fezeu LK, Ducros V, Guéant J-L, Guilland J-C, Andreeva VA, Hercberg S, Galan P (2018) MTHFR 677C → T genotype modulates the effect of a 5-year supplementation with B-vitamins on homocysteine concentration: The SU.FOL.OM3 randomized controlled trial. Plos One 13:e0193352
Fowler NR, Perkins AJ, Gao S, Sachs GA, Boustani MA (2020) Risks and benefits of screening for dementia in primary care: The Indiana University Cognitive Health Outcomes Investigation of the Comparative Effectiveness of Dementia Screening (IU CHOICE)Trial. J Am Geriatr Soc 68:535–543
Gardener SL, Rainey-Smith SR, Weinborn M, Bondonno CP, Martins RN (2021) Intake of products containing anthocyanins, flavanols, and flavanones, and cognitive function: a narrative review. Front Aging Neurosci 13:640381
Geethadevi GM, Quinn TJ, George J, Anstey K, Bell JS, Cross AJ (2021) Multidomain prognostic models used in middle aged adults without known cognitive impairment for predicting subsequent dementia. Cochrane Db Syst Rev. https://doi.org/10.1002/14651858.cd014885
Goerdten J, Čukić I, Danso SO, Carrière I, Muniz-Terrera G (2019) Statistical methods for dementia risk prediction and recommendations for future work: a systematic review. Alzheimer’s Dementia Transl Res Clin Interventions 5:563–569
Hendriks S, Peetoom K, Bakker C, Flier WM van der, Papma JM, Koopmans R, Verhey FRJ, Vugt M de, Köhler S, Group Y-ODES et al (2021) Global prevalence of young-onset dementia. Jama Neurol 78:1080–1090
Huq AJ, Sexton A, Lacaze P, Masters CL, Storey E, Velakoulis D, James PA, Winship IM (2021) Genetic testing in dementia-a medical genetics perspective. Int J Geriatr Psych 36:1158–1170
Jennings A, Cunnane SC, Minihane AM (2020) Can nutrition support healthy cognitive ageing and reduce dementia risk? BMJ 369:m2269
Kang JH, Vyas CM, Okereke OI, Ogata S, Albert M, Lee I-M, D’Agostino D, Buring JE, Cook NR, Grodstein F et al (2021) Effect of vitamin D on cognitive decline: results from two ancillary studies of the VITAL randomized trial. Sci Rep-Uk 11:23253
Lakhan R, Sharma M, Batra K, Beatty FB (2021) The role of vitamin E in slowing down mild cognitive impairment: a narrative review. Healthc 9:1573
Leonenko G, Baker E, Stevenson-Hoare J, Sierksma A, Fiers M, Williams J, de Strooper B, Escott-Price V (2021) Identifying individuals with high risk of Alzheimer’s disease using polygenic risk scores. Nat Commun 12:4506
Leshem A, Segal E, Elinav E (2020) The gut microbiome and individual-specific responses to diet. Msystems 5:e00665-e720
Livingston G, Huntley J, Sommerlad A, Ames D, Ballard C, Banerjee S, Brayne C, Burns A, Cohen-Mansfield J, Cooper C et al (2020) Dementia prevention, intervention, and care: 2020 report of the lancet commission. Lancet 396:413–446
Loy CT, Schofield PR, Turner AM, Kwok JB (2014) Genetics of dementia. Lancet 383:828–840
Markun S, Gravestock I, Jäger L, Rosemann T, Pichierri G, Burgstaller JM (2021) Effects of vitamin B12 supplementation on cognitive function, depressive symptoms, and fatigue: a systematic review, meta-analysis, and meta-regression. Nutrients 13:923
Marriott BP, Turner TH, Hibbeln JR, Newman JC, Pregulman M, Malek AM, Malcolm RJ, Burbelo GA, Wismann JW (1854) Impact of fatty acid supplementation on cognitive performance among United States (US) military officers: the ranger resilience and improved performance on phospholipid-bound omega-3’s (RRIPP-3) study. Nutrients 2021:13
Niforou A, Konstantinidou V, Naska A (2020) Genetic variants shaping inter-individual differences in response to dietary intakes—a narrative review of the case of vitamins. Front Nutr 7:558598
Patan MJ, Kennedy DO, Husberg C, Hustvedt SO, Calder PC, Khan J, Forster J, Jackson PA (2021) Supplementation with oil rich in eicosapentaenoic acid, but not in docosahexaenoic acid, improves global cognitive function in healthy, young adults: results from randomized controlled trials. Am J Clin Nutrition 114:914–924
Pérez-González M, Badesso S, Lorenzo E, Guruceaga E, Pérez-Mediavilla A, García-Osta A, Cuadrado-Tejedor M (2021) Identifying the main functional pathways associated with cognitive resilience to Alzheimer’s disease. Int J Mol Sci 22:9120
Philip P, Sagaspe P, Taillard J, Mandon C, Constans J, Pourtau L, Pouchieu C, Angelino D, Mena P, Martini D et al (2019) Acute intake of a grape and blueberry polyphenol-rich extract ameliorates cognitive performance in healthy young adults during a sustained cognitive effort. Antioxidants 8:650
Polverino A, Sorrentino P, Pesoli M, Mandolesi L (2021) Italy I of D and THC Naples, Italy D of M and WS University of Naples “Parthenope”, Naples, France I de N des S Aix-Marseille University, Marseille, Italy I of AS and IS National Research Council, Pozzuoli, Italy D of HS University of Naples Federico II, Naples,: Nutrition and cognition across the lifetime: an overview on epigenetic mechanisms. Aims Neurosci 8:448–476
Prince M, Wimo A, Guerchet M et al. World Alzheimer Report 2015. Alzheimers Disease International, London
Raz L, Knoefel J, Bhaskar K (2015) The neuropathology and cerebrovascular mechanisms of dementia. J Cereb Blood Flow Metabolism 36:172–186
Rutjes AW, Denton DA, Nisio MD, Chong L, Abraham RP, Al‐Assaf AS, Anderson JL, Malik MA, Vernooij RW, Martínez G et al (2018) Vitamin and mineral supplementation for maintaining cognitive function in cognitively healthy people in mid and late life. Cochrane Db Syst Rev 2019:CD011906
Samieri C, Yassine HN, van Lent DM, Lefèvre-Arbogast S, van de Rest O, Bowman GL, Scarmeas N (2021) Personalized nutrition for dementia prevention. Alzheimer’s Dementia J Alzheimer’s Assoc. https://doi.org/10.1002/alz.12486
Scarmeas N, Anastasiou CA, Yannakoulia M (2018) Nutrition and prevention of cognitive impairment. Lancet Neurol 17:1006–1015
Smith AD, Refsum H, Bottiglieri T, Fenech M, Hooshmand B, McCaddon A, Miller JW, Rosenberg IH, Obeid R (2018) Homocysteine and dementia: an international consensus statement1. J Alzheimer’s Dis 62:561–570
Soininen H, Solomon A, Visser PJ, Hendrix SB, Blennow K, Kivipelto M, Hartmann T, group L clinical study, Hallikainen I, Hallikainen M et al (2017) 24-month intervention with a specific multinutrient in people with prodromal Alzheimer’s disease (LipiDiDiet): a randomized, double-blind, controlled trial. Lancet Neurol 16:965–975.
Solomon A, Handels R, Wimo A, Antikainen R, Laatikainen T, Levälahti E, Peltonen M, Soininen H, Strandberg T, Tuomilehto J et al (2021) Effect of a multidomain lifestyle intervention on estimated dementia risk. J Alzheimer’s Dis 82:1461–1466
van Ommen B, van den Broek T, de Hoogh I, van Erk M, van Someren E, Rouhani-Rankouhi T, Anthony JC, Hogenelst K, Pasman W, Boorsma A et al (2017) Systems biology of personalized nutrition. Nutr Rev 75:579–599
Wu Y, Smith AD, Refsum H, Kwok T (2021) Effectiveness of B vitamins and their interactions with aspirin in improving cognitive functioning in older people with mild cognitive impairment: pooled post-hoc analyses of two randomized trials. J Nutrition Heal Aging 25:1154–1160
Yeh T-S, Yuan C, Ascherio A, Rosner BA, Willett WC, Blacker D (2021) Long-term dietary flavonoid intake and subjective cognitive decline in US men and women. Neurology 97:e1041–e1056
Zeisel SH (2020) Precision (personalized) nutrition: understanding metabolic heterogeneity. Annu Rev Food Sci T 11:1–22
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Borut, P., Bojan, Z., Ana, P. (2022). Precision Nutrition and Cognitive Decline. In: Haslberger, A.G. (eds) Advances in Precision Nutrition, Personalization and Healthy Aging. Springer, Cham. https://doi.org/10.1007/978-3-031-10153-3_8
Download citation
DOI: https://doi.org/10.1007/978-3-031-10153-3_8
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-10152-6
Online ISBN: 978-3-031-10153-3
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)