Abstract
Purpose of Review
The purposes of this review were to examine literature published over the last 5 years and to evaluate the role of nutrition in cognitive function and brain ageing, focussing on the Mediterranean diet (MeDi), Dietary Approaches to Stop Hypertension (DASH), and Mediterranean-DASH Intervention for Neurodegenerative Delay (MIND) diets.
Recent Findings
Results suggest that higher adherence to a healthy dietary pattern is associated with preservation of brain structure and function as well as slower cognitive decline, with the MIND diet substantially slowing cognitive decline, over and above the MeDi and DASH diets.
Summary
Whilst results to-date suggest adherence to a healthy diet, such as the MeDi, DASH, or MIND, is an important modifiable risk factor in the quest to develop strategies aimed at increasing likelihood of healthy brain ageing, further work is required to develop dietary guidelines with the greatest potential benefit for public health; a research topic of increasing importance as the world’s population ages.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction—Healthy vs. Pathological Brain Ageing
Whilst some cognitive functions remain stable or even improve with advancing age (e.g. crystallised intelligence and judgement abilities), most healthy adults experience age-related decline in a variety of cognitive functions including spatial orientation, episodic memory, speed of processing, language, decision-making abilities, judgement, and abstract thinking [1]. These detrimental cognitive changes are amplified and accelerated by common progressive age-related neurodegenerative pathologies such as Alzheimer’s disease (AD) and other forms of dementia.
Structural imaging studies utilising magnetic resonance imaging (MRI) reveal that brain shrinkage occurs with advancing age. Whole brain atrophy rates range from 0.3 to 0.7% per year in healthy older adults [2], with the hippocampus, entorhinal cortex, orbitofrontal cortex, and cerebellum regions particularly affected. Hippocampal volume decreases at a rate of 2–4% per annum in healthy aged individuals [3]: a significant finding when considering the important role of the hippocampus in aspects of memory. By contrast, MRI in AD, for example, reveals widespread cortical atrophy, particularly within medial temporal lobe structures including the amygdala, hippocampus, and parahippocampal gyrus [4], with whole brain atrophy rates ranging from 1 to 4% per year [2].
Imaging modalities such as positron emission tomography (PET) also reveal age-related functional changes in the brain. Fluorodeoxyglucose (FDG)-PET enables cerebral glucose metabolism to be quantified as an indicator of neuronal and synaptic activity. FDG-PET studies have shown that between 20 and 70 years of age, global cerebral metabolic rate decreases by 12–13% [5]. Further, healthy ageing is associated with mild cortical hypometabolism preferentially involving the frontal lobes, most notably within the anterior cingulate, dorsolateral and medial prefrontal, and orbitofrontal cortices. By contrast, other regions such as the precuneus, mesial temporal lobes (hippocampus, amygdala, parahippocampal gyrus), primary motor, and occipital cortices are least affected by healthy ageing [5]. Metabolic changes in the AD brain are, however, far more pronounced, with FDG-PET studies of AD patients demonstrating a typical pattern of hypometabolism in temporoparietal regions with sparing of the basal ganglia, thalamus, cerebellum, and primary sensorimotor cortex [6]. Pittsburgh Compound B (PiB)-PET is used to visualise and quantify deposition of the protein beta-amyloid (Aβ) within the living brain [7]. Aβ is derived from proteolytic cleavage of the much larger membrane-spanning amyloid precursor protein (APP). The normal physiological function of Aβ and APP is poorly understood; however, putative functions of the latter include regulation of neuritic outgrowth, cell adhesion, synaptogenesis, and cell survival [8]. Elevated levels of cerebral Aβ in apparently healthy persons are found in 12% of those in their 60s, 30% of those in their 70s, and at least 50% of those over 80 years of age [7]. Moreover, PiB-PET determined cerebral Aβ levels correlate with rate of memory decline in healthy older adults [7]: consistent with the notion that Aβ accumulation promotes neuronal death, which ultimately results in cognitive impairment. In AD however, the brain is characterised neuropathologically by significant cerebral Aβ burden, with levels highest in the frontal cortex, cingulate gyrus, precuneus, striatum, parietal cortex, and lateral temporal cortex [7].
Accumulating data suggests that nutrition likely influences trajectories of cognitive and neurobiological change in older adults, with healthy diets appearing to ‘tip the balance’ in favour of healthy ageing, and decrease risk of neurodegenerative pathologies such as AD and other forms of dementia. The purpose of this review is to examine research published within the past 5 years to evaluate the role of nutrition in cognitive function and brain ageing. We focussed on studies which reported on the relationship between cognitive and neuroimaging outcome measures and the following three dietary patterns: (1) the Mediterranean diet (MeDi), (2) the Dietary Approaches to Stop Hypertension (DASH) diet, and (3) the Mediterranean-DASH Intervention for Neurodegenerative Delay (MIND) diet. Dietary patterns take into account the fact that foods and nutrients are biologically interactive, acting in concert rather than as solitary physiological agents; all three patterns are created ‘a priori’, with the DASH and MIND diets recently developed based on current nutrition knowledge.
Dietary Pattern Background
MeDi
The MeDi is characterised by high intake of vegetables, legumes, fruits, cereals, fish, and unsaturated fatty acids (mostly olive oil); low intake of saturated fatty acids, meat, and poultry; low-to-moderate intake of dairy products (mostly cheese and yoghurt); and a regular but moderate amount of alcohol (mostly wine, generally with meals). An individual is assigned a value of 1 for each; beneficial component (fruits, vegetables, legumes, cereals, fish), if caloric-adjusted consumption is at or above the gender-specific median; for each detrimental component (meat and dairy products), where caloric-adjusted consumption is below the gender-specific median; and for a ratio of monounsaturated fats to saturated fats at or above the median. Individuals are also assigned a value of 1 for mild-to-moderate alcohol consumption (> 5 to < 25 g/day for females, > 10 to < 50 g/day for males). The MeDi score is generated by adding the scores for each category, and ranges from 0 to 9, with a higher score indicating greater adherence. This diet includes many dietary components reported to be beneficial for reducing neurodegenerative disease risk [9,10,11,12,13,14,15,16], and therefore has received much attention.
DASH Diet
The DASH diet was developed from an initiative to examine dietary factors that affect blood pressure. The DASH diet is high in fruits, vegetables, nuts, whole-cereal products, low-fat dairy products, fish, chicken, and lean meats, and therefore is designed to be low in saturated fat, total fat, and cholesterol; moderately high in protein; and high in minerals and fibre [17]. The DASH diet score focuses on eight components: high intake of fruits, vegetables, nuts and legumes, low-fat dairy products, and whole grains, and low intake of sodium, sweetened beverages, and red and processed meats. For each of the components, participants are classified into quintiles according to intake. For components where a high intake is desirable, quintile 1 (lowest intake) is assigned 1 point and quintile 5 (highest intake) is assigned 5 points. For sodium, red and processed meats, and sweetened beverages where low intake is desirable, the lowest intake quintile is assigned 5 points and the highest intake quintile is assigned 1 point. Component scores are then summed to obtain an overall DASH diet score ranging from 8 to 40.
MIND Diet
Combining the MeDi and DASH diets but with modifications reflecting the best evidence for neuroprotection, the MIND diet emphasises natural, plant-based foods, specifically promoting increased consumption of berries and leafy green vegetables, with limited intakes of animal-based and high saturated fat foods. However, the current literature is underdeveloped, and therefore, modifications to the MIND diet score are expected as new scientific advances are made. The MIND diet is composed of ten brain-healthy and five unhealthy components: green leafy vegetables, other vegetables, nuts, berries, beans, whole grains, fish, poultry, olive oil, and wine constitute the brain-healthy components, whilst red meats, butter and stick margarine, pastries and sweets, and fried or fast foods comprise the unhealthy components. Additional general guidelines include eating at least three servings of whole grains, a salad and one other vegetable, and a glass of wine each day. Further, nuts are used as a snack on most days, and beans every other day. Poultry and berries are recommended at least twice a week, and fish at least once a week. The unhealthy components are limited in intake, especially, butter (< 1 tablespoon/day), cheese, and fried or fast food (each, < 1 serving/week) [18•]. Dietary components are scored 0, 0.5, or 1 depending on level of consumption, with healthy components assigned a higher score with increasing consumption, and the reverse occurring for unhealthy components. Olive oil use is scored 1 if intake is 1 tablespoon or more per day, and 0 otherwise. Dietary component scores are then summed to obtain an overall score ranging from 0 to 15, with higher scores indicating greater MIND diet adherence [18•].
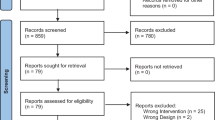
Dietary Patterns and Cognition
A summary of studies, published in the last 5 years, which report on the relationship between MeDi, DASH, or MIND dietary pattern adherence and cognitive outcomes is provided in Table 1. Of the three dietary patterns, to-date, the most evidence exists for an effect of the MeDi on cognition, with the majority of studies reporting beneficial outcomes. Among cohorts drawn from Greece, France, and the USA, higher MeDi adherence has been associated cross-sectionally with better global cognitive function [22, 29]; better performance in measures of attention, processing speed, and working memory [19]; as well as reduced likelihood of major cognitive impairment at age 70 [20].
Longitudinal studies conducted in Australia and the USA further support these data, with high MeDi adherence associated with less decline in executive function in carriers of the Apolipoprotein E ɛ4 allele (APOE ɛ4; a major genetic risk factor for AD); [27] slower decline in episodic memory, semantic memory, working memory, and global cognition; [26] and less likelihood of incident cognitive impairment [25]. Further, higher long-term MeDi adherence, assessed over a decade, has been associated with better performance, over the next 6 years, in a telephone adaptation of the MMSE, and composite scores of verbal memory and global cognition, with the authors estimating that higher MeDi adherence delayed cognitive ageing by 1 year [21].
Of particular importance, the recently completed PREDIMED (PREvención con DIeta Mediterránea) study is the first randomised clinical trial to evaluate the effect of a long-term MeDi intervention on cognitive function. Participants were assigned to either a MeDi supplemented with extra virgin olive oil (MeDi+EVOO; 1 litre a week), a MeDi supplemented with raw, unprocessed mixed nuts (MeDi+Nuts; 30 g per day), or a control diet (advice to reduce dietary fat). The trial, conducted in Spain, included 11 sites with results to-date published using individual site data. The Navarra site administered the intervention to 522 participants for 6.5 years, with cognitive assessment only undertaken at study completion. Multivariate regression analyses revealed that participants in the MeDi+EVOO and MeDi+Nuts groups had higher mean MMSE (0.62; 95% CI 0.18–1.05, p = 0.005 and 0.57; 95% CI 0.11–1.03, p = 0.015, respectively) and Clock Drawing Test scores (0.51; 95% CI 0.20–0.82, p = 0.001 and 0.33; 95% CI 0.003–0.67, p = 0.048, respectively) than the control group [23]. The authors subsequently investigated a range of cognitive domains including, episodic memory, verbal memory, visual memory, visuospatial abilities, language, fluency, executive function, attention, working memory, and abstract reasoning, in a subset of 285 participants. The MeDi+EVOO group demonstrated significantly better performance across fluency and memory tasks compared to the control group; however, the MeDi+Nuts group did not differ in cognitive performance compared to the control group [24]. The Barcelona site administered the intervention for a mean of 4.1 years and performed cognitive assessments at both baseline and post-intervention. For 334 participants, memory, frontal (attention and executive function), and global cognitive composites were constructed. The study authors reported that compared with the control group, the memory composite improved significantly in the MeDi+Nuts group (0.09; 95% CI −0.05–0.23, p = 0.04), whereas the frontal (0.23; 95% CI 0.03–0.43, p = 0.003) and global cognition (0.05; 95% CI −0.11–0.21, p = 0.005) composites improved in the MeDi+EVOO group [28••].
Far fewer published studies have to-date investigated the relationship between the DASH and MIND dietary patterns and cognition. Besides exploring the link between MeDi adherence and cognition described above, the American Memory and Ageing Project also characterised the relationship of DASH diet scores to cognitive outcomes. Higher DASH diet score was associated with slower rates of decline in episodic memory, semantic memory, and global cognition over an average follow-up of 4 years (N = 826) [26]. In a cohort of 960 participants drawn from the same study, adherence to the MIND diet was associated with slower decline in global cognition (β = 0.0095, p < 0.0001) as well as in each of the following five cognitive domains: episodic memory, semantic memory, perceptual organisation, perceptual speed, and working memory, over an average 4.7 years of follow-up. The authors reported that those participants with MIND diet scores in the highest tertile demonstrated rates of decline that were equivalent to being 7.5 years younger in age than those individuals in the lowest adherence tertile, and concluded that MIND diet score was more predictive of cognitive decline than either the MeDi or DASH diet scores [18•]. Furthermore, a recently published second study of MIND diet adherence and cognition in an American cohort of community-dwelling older adults (N = 5907), describes a cross-sectional association between higher MIND diet score and better composite test scores of global cognitive function (p < 0.001) [29].
Precisely how the dietary patterns described above contribute to cognitive health remains to be determined, although accumulating literature suggests that it is likely via direct modulation of neurobiological changes in the brain.
Dietary Patterns and Neurobiological Changes
Diet and Structural Brain Changes
Indeed, mounting evidence, derived from MRI studies, suggests an association between higher MeDi adherence and preservation of brain structure. One such cross-sectional study of cognitively healthy American individuals (N = 52) reported greater thickness of AD-vulnerable brain regions in those with high MeDi adherence compared to the low adherence group, with the differences most pronounced in the orbitofrontal cortex, entorhinal cortex, and posterior cingulate cortex of the left hemisphere [30]. In a similar study of 674 dementia-free elderly adults (mean age 80.1 years) residing in Manhattan, higher MeDi adherence (scores of 5–9) was associated with larger total brain volume (β = 13.11, p = 0.007), total grey, and total white matter volumes (β = 5.00, p = 0.05 and β = 6.41, p = 0.05, respectively), compared to those with lower MeDi adherence (scores 0–4) [31]. The authors concluded that higher intake of fish and lower meat intake were the two MeDi components which appeared to confer the greatest benefit in their cohort [31]. Higher MeDi adherence has also been reported to be associated with larger frontal, parietal, occipital, and average lobar cortical thickness (CT: β = 0.011, p = 0.008; β = 0.009, p = 0.040; β = 0.007, p = 0.030; and β = 0.009, p = 0.010, respectively) in a cross-sectional study of 672 cognitively normal older adults (mean age 79.8 years) [32]. MeDi score was also positively correlated with CT of a number of individual brain regions including superior temporal, dorsolateral prefrontal, middle temporal, fusiform, precuneus, and lingual (β range 0.010–0.014; p range 0.010–0.009). When examining the individual MeDi components, the authors found higher legume and fish intakes to be associated with larger CT [32].
Whilst the majority of previous studies calculated MeDi scores using food frequency questionnaires which capture dietary habits over the preceding year, Titova et al. [33] determined MeDi adherence via food intake diaries completed, for a total of 7 days, by 194 cognitively healthy Swedish individuals aged 70 years. The authors found no association between total MeDi score and brain volumes, determined via MRI 5 years after food diary completion, instead reporting a link between the MeDi score component of meat and meat products and brain volume, with lower intake associated with larger total brain volume (β = −0.16, p = 0.04) [33]. Limitations of this study, however, include the brief period of dietary data collection, and the 5-year interval between this data collection and assessment of brain volumes, with no determination of dietary habits in-between. In a French cohort study, Pelletier et al. [34] reported associations between MeDi adherence and structural brain imaging outcomes with an even longer interval between dietary data collection and MRI assessment. Specifically, MeDi adherence was determined by dietary questionnaire completed by 146 non-demented older adults (mean age 73 years), with 3T MRI undertaken on average 9 years later. Whilst the authors found no relationship between MeDi adherence and grey matter parameters, higher MeDi score was associated with a general pattern of preserved white matter microstructure, suggestive of a beneficial effect on preservation of brain structure connectivity.
One of the few imaging studies, which is longitudinal in nature, described slower rates of hippocampal atrophy among individuals in the middle or high MeDi adherence tertiles compared to those in the lowest tertile (β = 330, p = 0.02 and β = 331, p = 0.04, respectively), such that mid-high MeDi adherence slowed age-related atrophy by approximately 2.5 years [35•]. This study utilised an American cohort of 215 cognitively normal elderly participants (mean age 79.1 years), who underwent two MRI scans on average 4.5 years apart. A second, and very recent, longitudinal study investigating rates of brain atrophy in a cohort of older Scottish adults (N = 401) found lower MeDi adherence to be associated with greater total brain atrophy (β = 1.160, p = 0.018) [36]. Dietary data was collected at age 70 via food frequency questionnaire, whilst MRI scans were undertaken at ages 73 and 76.
Collectively, these results suggest that MeDi adherence contributes to preservation of brain structure and volume. Despite the promising cognitive findings, to-date, there are no published studies investigating the relationship of the DASH and MIND dietary patterns to structural neuroimaging outcome measures.
Diet and Functional Neuroimaging Outcomes: Cerebral Glucose Metabolism and Beta-Amyloid Burden
Some evidence exists which is suggestive of an association between dietary patterns and functional neuroimaging outcome measures, although overall, there is a relative paucity of such studies. One cross-sectional study published in the last 5 years measured cerebral glucose metabolism, via FDG-PET scans, in 45 cognitively healthy individuals from New York (mean age 54 years), with participants dichotomised into either ‘high’ or ‘low’ MeDi adherence groups (determined via self-report). Significantly reduced global cerebral glucose metabolism was observed among the ‘low’ MeDi adherence group compared to the ‘high’ MeDi adherence group. Further investigation of glucose metabolism within brain regions established that the spatial pattern providing the best separation between MeDi groups included the lateral and medial temporal cortex, fusiform gyrus, and inferior frontal cortex, primarily restricted to the left hemisphere (R2 = 0.23, p < 0.001) [37]. As part of the same study, these authors also assessed the associated between MeDi adherence and cerebral amyloid burden determined via PiB-PET. Significantly higher PiB retention (indicating higher cerebral Aβ burden) was observed in the ‘low’ MeDi adherence group compared to the ‘high’ adherence group. The best separation between MeDi groups was seen via a spatial pattern comprising of the frontal and temporal cortex, insula, and putamen of both hemispheres (R2 = 0.39, p < 0.001) [37].
A second cross-sectional study recently examined the association of frequency of following a Mediterranean-type diet with brain Aβ and tau among 44 individuals with mild cognitive impairment (MCI; often but not always precedes AD) or subjective memory impairment [38]. Participants were assigned to either an ‘often’ or ‘rarely’ diet frequency group based on their response to a single question. The authors reported a relationship between greater frequency of following a Mediterranean-type diet and less brain Aβ/tau burden. However, a pan-amyloid PET ligand which binds to both Aβ and tau deposits was used, thereby precluding determination of whether diet was associated with Aβ, tau, or a combination of both [38].
One study to-date has investigated the association between MeDi adherence and rate of Aβ accumulation in older adults. This study examined cerebral Aβ burden, determined via PiB-PET, over 36 months, in a subset of 77 cognitively healthy participants (mean age 71.1 years) from the AIBL Study of Ageing. These participants were all considered to be on the AD pathway by either demonstrating a high Aβ burden at baseline (standardised uptake value ratio (SUVR) ≥ 1.4) or presenting with rates of Aβ deposition higher than 0 over 36 months. Increasing MeDi score, determined via self-report, was associated with decreasing SUVR (β = −0.01, p = 0.007), with each one point MeDi score increase associated with an annual decrease in Aβ accumulation of 20%. Further evaluation revealed fruit intake to be the individual MeDi score component which contributed most strongly to this relationship, with a high intake of fruit associated with less accumulation of Aβ (p = 0.00036) [39••].
At the time of writing, no published studies have explored potential associations between the DASH and MIND dietary patterns and functional neuroimaging outcomes.
Important Beneficial Constituents of the Dietary Patterns
Fruit and vegetables are an important component of the three dietary patterns featured in this review and are likely contributors to the beneficial effects associated with pattern adherence. Indeed, oxidative stress and inflammation are considered to be underlying pathogenic mechanisms of cognitive decline [40, 41], whilst fruit and vegetables are an abundant source of both antioxidants and anti-inflammatory agents. Polyphenols, which are plentiful in both fruit and vegetables, are micronutrients with antioxidant properties. Flavonoids are the largest subclass of polyphenols, and berries, which feature prominently during MIND diet score calculation, contain a range of these compounds in high concentration. Higher intake of strawberries and blueberries has been associated with slower rates of cognitive decline in older adults, with the study authors hypothesising that this is due to the flavonoids they contain, as total flavonoid and anthocyanidin intakes (a flavonoid particularly high in these berries) were also associated with slower rates of cognitive decline in this cohort [42]. Berry-derived anthocyanidins are uniquely capable of crossing the blood brain barrier and localising in areas involved in learning and memory, such as the hippocampus [43]. Rat studies have shown supplementation with blueberries or strawberries results in significantly reduced age-related declines in neuronal signalling, and supplementation at older ages reversed neuronal and cognitive decline [44]. Flavonoids in general have been shown to lead to reductions in neuroinflammation and enhanced neuronal viability by inhibiting the c-jun N-terminal kinases, apoptosis signal-regulating kinase-1, and p38 pathways [45].
Olive oil and nuts, which are features of all three dietary patterns discussed in this review, are also particularly rich in phenolic compounds [46], suggesting an additional dietary component that contributes to the beneficial effects associated with pattern adherence. The MeDi, and in particular extra virgin olive oil, contains a large amount of oleic acid which has been associated with lower inflammatory markers such as C-reactive protein (CRP) [47], and tumour necrosis factor alpha (TNR-α) [48], and in general, both the MeDi and DASH diets have been shown to lower levels of several inflammatory markers [49,50,51]. Furthermore, olecanthal, a phenolic component of extra virgin olive oil, has been shown to enhance brain Aβ clearance [52]. Polyphenols can also ameliorate neurologic health by additional mechanisms, including improved cerebrovascular blood flow, enhanced synthesis of neurotrophic factors, and stimulation of neurogenesis [53].
Fish intake is another important component of all three dietary patterns. Fish contains several beneficial nutrients including the omega-3 polyunsaturated fatty acids (PUFAs) eicosapentaenoic acid (EPA), and docosahexaenoic acid (DHA). The beneficial effects of omega-3 PUFAs on the brain include increasing neurite outgrowth and synaptogenesis, neurogenesis, as well as promoting anti-inflammatory actions [54]. EPA and DHA are able to affect a number of aspects of inflammation, and mechanisms underlying their actions include altered cell membrane phospholipid fatty acid composition, disruption of lipid rafts, and inhibition of activation of the pro-inflammatory transcription factor nuclear factor kappa B (thereby reducing expression of inflammatory genes) [55]. It is important to note, however, that the amount of omega-3 PUFAs in fish varies greatly depending on the type of fish (i.e. oily > > white), and this information should be considered when interpreting study findings.
Whilst we have discussed a few of the components common to the MeDi, DASH, and MIND dietary patterns, which are likely contributors to the beneficial effects associated with pattern adherence, it is important to remember that foods and nutrients are biologically interactive, acting in concert rather than as solitary physiological agents, and as such the true benefit of dietary pattern adherence is likely due to a complex milieu of beneficial effects rather than the contribution of individual components.
Conclusion
Of the three dietary patterns examined, the literature reviewed suggests that the MIND diet substantially slows cognitive decline, over and above the effect seen with the MeDi or DASH diets, and collectively, the evidence base discussed above suggests that diet affects brain structure and function which likely ultimately manifests as modulation of cognitive outcomes. Precisely how these diets might exert such effects on the brain remains to be determined although potential candidate mechanisms include increasing neurite outgrowth and synaptogenesis [54], antioxidant and anti-inflammatory effects [49,50,51, 56,57,58,59], as well as a favourable impact on brain vasculature, possibly indirectly via modulation of adiposity, lipid profiles, blood pressure, etc. [47, 58, 60,61,62,63,64,65]. Further, Aβ accumulation, which contributes to atrophy, and thus cognitive outcomes, is proposed to be lessened by adherence to a healthy diet [39••].
Whilst results to-date certainly suggest that adherence to a healthy diet such as the MeDi, DASH, or MIND is important for increasing likelihood of healthy brain ageing, and thereby decreasing risk of age-related neurodegenerative pathologies such as AD and other forms of dementia, further work is required to develop dietary guidelines with the greatest potential benefit for public health. The majority of published studies have been both cross-sectional and observational in nature, with limited evidence available from longitudinal or intervention trials. Cross-sectional studies cannot exclude the possibility of reverse causality (i.e., differences in brain structure, for example, result in behavioural changes including alterations in dietary habits), and causal relationships cannot be determined from observational studies. Moreover, methodological variations hinder comparison of results between studies, for example, use of different dietary questionnaires to capture nutrient intake, residual confounders, and differences in covariates included across studies. Despite these limitations, it is evident that nutrition is an important modifiable risk factor in the quest to develop strategies aimed at increasing likelihood of healthy brain ageing; a research topic of increasing importance as the world’s population ages.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Tucker-Drob EM, Reynolds CA, Finkel D, Pedersen NL. Shared and unique genetic and environmental influences on aging-related changes in multiple cognitive abilities. Dev Psychol. 2014;50(1):152–66.
Cover KS, van Schijndel RA, van Dijk BW, Redolfi A, Knol DL, Frisoni GB, et al. Assessing the reproducibility of the SienaX and Siena brain atrophy measures using the ADNI back-to-back MP-RAGE MRI scans. Psychiatry Res. 2011;193(3):182–90.
Raz N, Lindenberger U, Rodrigue KM, Kennedy KM, Head D, Williamson A, et al. Regional brain changes in aging healthy adults: general trends, individual differences and modifiers. Cereb Cortex. 2005;15(11):1676–89.
Jobst KA, Smith AD, Szatmari M, Molyneux A, Esiri ME, King E, et al. Detection in life of confirmed Alzheimer's disease using a simple measurement of medial temporal lobe atrophy by computed tomography. Lancet. 1992;340(8829):1179–83.
Berti V, Mosconi L, Pupi A. Brain: normal variations and benign findings in fluorodeoxyglucose-PET/computed tomography imaging. PET Clin. 2014;9(2):129–40.
Salmon E, Sadzot B, Maquet P, Degueldre C, Lemaire C, Rigo P, et al. Differential diagnosis of Alzheimer’s disease with PET. J Nucl Med. 1994;35(3):391–8.
Rowe CC, Villemagne VL. Brain amyloid imaging. J Nucl Med. 2011;52(11):1733–40.
Zheng H, Koo EH. Biology and pathophysiology of the amyloid precursor protein. Mol Neurodegener. 2011;6(1):27.
Gao X, Chen H, Fung TT, Logroscino G, Schwarzschild MA, Hu FB, et al. Prospective study of dietary pattern and risk of Parkinson disease. Am J Clin Nutr. 2007;86(5):1486–94.
Scarmeas N, Luchsinger JA, Mayeux R, Stern Y. Mediterranean diet and Alzheimer disease mortality. Neurology. 2007;69(11):1084–93.
Scarmeas N, Stern Y, Mayeux R, Luchsinger JA. Mediterranean diet, Alzheimer disease, and vascular mediation. Arch Neurol. 2006;63(12):1709–17.
Scarmeas N, Stern Y, Mayeux R, Manly JJ, Schupf N, Luchsinger JA. Mediterranean diet and mild cognitive impairment. Arch Neurol. 2009;66(2):216–25.
Scarmeas N, Stern Y, Tang MX, Mayeux R, Luchsinger JA. Mediterranean diet and risk for Alzheimer’s disease. Ann Neurol. 2006;59(6):912–21.
Trichopoulou A, Costacou T, Bamia C, Trichopoulos D. Adherence to a Mediterranean diet and survival in a Greek population. N Engl J Med. 2003;348(26):2599–608.
Sofi F, Abbate R, Gensini GF, Casini A. Accruing evidence on benefits of adherence to the Mediterranean diet on health: an updated systematic review and meta-analysis. Am J Clin Nutr. 2010;92(5):1189–96.
Sofi F, Cesari F, Abbate R, Gensini GF, Casini A. Adherence to Mediterranean diet and health status: meta-analysis. BMJ. 2008;337:a1344.
Appel LJ, Moore TJ, Obarzanek E, Vollmer WM, Svetkey LP, Sacks FM, et al. A clinical trial of the effects of dietary patterns on blood pressure. DASH Collaborative Research Group. N Engl J Med. 1997;336(16):1117–24.
• Morris MC, Tangney CC, Wang Y, Sacks FM, Barnes LL, Bennett DA, et al. MIND diet slows cognitive decline with aging. Alzheimers Dement. 2015;11(9):1015–22. This study examined all three dietary patterns investigated in this review, and concluded that low MIND diet adherence is more predictive of cognitive decline than either low MeDi or DASH diet scores.
Kesse-Guyot E, Andreeva VA, Lassale C, Ferry M, Jeandel C, Hercberg S, et al. Mediterranean diet and cognitive function: a French study. Am J Clin Nutr. 2013;97(2):369–76.
Samieri C, Sun Q, Townsend MK, Chiuve SE, Okereke OI, Willett WC, et al. The association between dietary patterns at midlife and health in aging: an observational study. Ann Intern Med. 2013;159(9):584–91.
Samieri C, Okereke OI, E ED, Grodstein F. Long-term adherence to the Mediterranean diet is associated with overall cognitive status, but not cognitive decline, in women. J Nutr. 2013;143(4):493–9.
Katsiardanis K, Diamantaras AA, Dessypris N, Michelakos T, Anastasiou A, Katsiardani KP, et al. Cognitive impairment and dietary habits among elders: the Velestino study. J Med Food. 2013;16(4):343–50.
Martinez-Lapiscina EH, Clavero P, Toledo E, Estruch R, Salas-Salvado J, San Julian B, et al. Mediterranean diet improves cognition: the PREDIMED-NAVARRA randomised trial. J Neurol Neurosurg Psychiatry. 2013;84(12):1318–25.
Martinez-Lapiscina EH, Clavero P, Toledo E, San Julian B, Sanchez-Tainta A, Corella D, et al. Virgin olive oil supplementation and long-term cognition: the PREDIMED-NAVARRA randomized, trial. J Nutr Health Aging. 2013;17(6):544–52.
Tsivgoulis G, Judd S, Letter AJ, Alexandrov AV, Howard G, Nahab F, et al. Adherence to a Mediterranean diet and risk of incident cognitive impairment. Neurology. 2013;80(18):1684–92.
Tangney CC, Li H, Wang Y, Barnes L, Schneider JA, Bennett DA, et al. Relation of DASH- and Mediterranean-like dietary patterns to cognitive decline in older persons. Neurology. 2014;83(16):1410–6.
Gardener SL, Rainey-Smith SR, Barnes MB, Sohrabi HR, Weinborn M, Lim YY, et al. Dietary patterns and cognitive decline in an Australian study of ageing. Mol Psychiatry. 2014;
•• Valls-Pedret C, Sala-Vila A, Serra-Mir M, Corella D, de la Torre R, Martinez-Gonzalez MA, et al. Mediterranean diet and age-related cognitive decline: a randomized clinical trial. JAMA Int Med. 2015;175(7):1094–103. This is the first MeDi intervention trial, with analysis of cognitive performance both pre- and post- intervention, demonstrating a positive effect of MeDi consumption, supplemented with both nuts and extra virgin olive oil, on cognition. Intervention trials are required to establish a causal relationship between diet and cognitive performance.
McEvoy CT, Guyer H, Langa KM, Yaffe K. Neuroprotective diets are associated with better cognitive function: the health and retirement study. J Am Geriatr Soc. 2017;65(8):1857–62.
Mosconi L, Murray J, Tsui WH, Li Y, Davies M, Williams S, et al. Mediterranean diet and magnetic resonance imaging-assessed brain atrophy in cognitively normal individuals at risk for Alzheimer’s disease. J Prev Alzheimers Dis. 2014;1(1):23–32.
Gu Y, Brickman AM, Stern Y, Habeck CG, Razlighi QR, Luchsinger JA, et al. Mediterranean diet and brain structure in a multiethnic elderly cohort. Neurology. 2015;85(20):1744–51.
Staubo SC, Aakre JA, Vemuri P, Syrjanen JA, Mielke MM, Geda YE, et al. Mediterranean diet, micronutrients and macronutrients, and MRI measures of cortical thickness. Alzheimer's & dementia : the journal of the Alzheimer's Association. 2017;13(2):168–77.
Titova OE, Ax E, Brooks SJ, Sjogren P, Cederholm T, Kilander L, et al. Mediterranean diet habits in older individuals: associations with cognitive functioning and brain volumes. Exp Gerontol. 2013;48(12):1443–8.
Pelletier A, Barul C, Feart C, Helmer C, Bernard C, Periot O, et al. Mediterranean diet and preserved brain structural connectivity in older subjects. Alzheimer's & dementia : the journal of the Alzheimer's Association. 2015;11(9):1023–31.
• Gu Y, Scarmeas N, Stern Y, Manly J, Schupf N, Mayeux R, et al. Mediterranean diet is associated with slower rates of hippocampal atrophy: a longitudinal study in cognitively normal older adults. Alzheimers Dement. 2016;12(7):193–4. One of the few longitudinal studies investigating MeDi adherence and brain atrophy in a relatively large cohort of cognitively normal participants. Higher MeDi adherence was associated with slower rate of hippocampal atrophy.
Luciano M, Corley J, Cox SR, Valdes Hernandez MC, Craig LC, Dickie DA, et al. Mediterranean-type diet and brain structural change from 73 to 76 years in a Scottish cohort. Neurology. 2017;88(5):449–55.
Matthews DC, Davies M, Murray J, Williams S, Tsui WH, Li Y, et al. Physical activity, Mediterranean diet and biomarkers-assessed risk of Alzheimer’s: a multi-modality brain imaging study. Adv J Mol Imaging. 2014;4(4):43–57.
Merrill DA, Siddarth P, Raji CA, Emerson ND, Rueda F, Ercoli LM, et al. Modifiable risk factors and brain positron emission tomography measures of amyloid and tau in nondemented adults with memory complaints. Am J Geriatr Psychiatry. 2016;24(9):729–37.
•• Rainey-Smith SR, Gu Y, Gardener SL, Doecke JD, Villemagne VL, Brown BM, et al. Mediterranean diet adherence and rate of cerebral Aβ-amyloid accumulation: data from the Australian Imaging, Biomarkers and Lifestyle Study of Ageing. Transl Psychiatry. 2018; This is the only study to-date investigating MeDi adherence and accumulation of cerebral Aβ longitudinally, conducted in individuals on the pathway to Alzheimer's disease. Higher MeDi adherence was associated with significantly less Aβ accumulation over three years.
Mecocci P. Oxidative stress in mild cognitive impairment and Alzheimer disease: a continuum. J Alzheimers Dis. 2004;6(2):159–63.
Galimberti D, Scarpini E. Inflammation and oxidative damage in Alzheimer’s disease: friend or foe. Front Biosci. 2011;3:252–66.
Devore EE, Kang JH, Breteler MM, Grodstein F. Dietary intakes of berries and flavonoids in relation to cognitive decline. Ann Neurol. 2012;72(1):135–43.
Andres-Lacueva C, Shukitt-Hale B, Galli RL, Jauregui O, Lamuela-Raventos RM, Joseph JA. Anthocyanins in aged blueberry-fed rats are found centrally and may enhance memory. Nutr Neurosci. 2005;8(2):111–20.
Joseph JA, Shukitt-Hale B, Willis LM. Grape juice, berries, and walnuts affect brain aging and behavior. J Nutr. 2009;139(9):1813S–7S.
Bakhtiari M, Panahi Y, Ameli J, Darvishi B. Protective effects of flavonoids against Alzheimer's disease-related neural dysfunctions. Biomed Pharmacother. 2017;93:218–29.
Urpi-Sarda M, Casas R, Chiva-Blanch G, Romero-Mamani ES, Valderas-Martinez P, Arranz S, et al. Virgin olive oil and nuts as key foods of the Mediterranean diet effects on inflammatory biomakers related to atherosclerosis. Pharmacol Res. 2012;65(6):577–83.
Estruch R, Martinez-Gonzalez MA, Corella D, Salas-Salvado J, Ruiz-Gutierrez V, Covas MI, et al. Effects of a Mediterranean-style diet on cardiovascular risk factors: a randomized trial. Ann Intern Med. 2006;145(1):1–11.
Vassiliou EK, Gonzalez A, Garcia C, Tadros JH, Chakraborty G, Toney JH. Oleic acid and peanut oil high in oleic acid reverse the inhibitory effect of insulin production of the inflammatory cytokine TNF-alpha both in vitro and in vivo systems. Lipids Health Dis. 2009;8:25.
Fung TT, Chiuve SE, McCullough ML, Rexrode KM, Logroscino G, Hu FB. Adherence to a DASH-style diet and risk of coronary heart disease and stroke in women. Arch Intern Med. 2008;168(7):713–20.
Mena MP, Sacanella E, Vazquez-Agell M, Morales M, Fito M, Escoda R, et al. Inhibition of circulating immune cell activation: a molecular antiinflammatory effect of the Mediterranean diet. Am J Clin Nutr. 2009;89(1):248–56.
Chrysohoou C, Panagiotakos DB, Pitsavos C, Das UN, Stefanadis C. Adherence to the Mediterranean diet attenuates inflammation and coagulation process in healthy adults: The ATTICA Study. J Am Coll Cardiol. 2004;44(1):152–8.
Abuznait AH, Qosa H, Busnena BA, El Sayed KA, Kaddoumi A. Olive-oil-derived oleocanthal enhances beta-amyloid clearance as a potential neuroprotective mechanism against Alzheimer’s disease: in vitro and in vivo studies. ACS Chem Neurosci. 2013;4(6):973–82.
Del Rio D, Rodriguez-Mateos A, Spencer JP, Tognolini M, Borges G, Crozier A. Dietary (poly)phenolics in human health: structures, bioavailability, and evidence of protective effects against chronic diseases. Antioxid Redox Signal. 2013;18(14):1818–92.
Dyall SC. Long-chain omega-3 fatty acids and the brain: a review of the independent and shared effects of EPA, DPA and DHA. Front Aging Neurosci. 2015;7:52.
Calder P. Omega-3 polyunsaturated fatty acids and inflammatory processes: nutrition of pharmacology. Br J Clin Pharmacol. 2012;75(3):645–62.
Erlinger TP, Miller ER 3rd, Charleston J, Appel LJ. Inflammation modifies the effects of a reduced-fat low-cholesterol diet on lipids: results from the DASH-sodium trial. Circulation. 2003;108(2):150–4.
Miller ER 3rd, Erlinger TP, Sacks FM, Svetkey LP, Charleston J, Lin PH, et al. A dietary pattern that lowers oxidative stress increases antibodies to oxidized LDL: results from a randomized controlled feeding study. Atherosclerosis. 2005;183(1):175–82.
Blumenthal JA, Babyak MA, Hinderliter A, Watkins LL, Craighead L, Lin PH, et al. Effects of the DASH diet alone and in combination with exercise and weight loss on blood pressure and cardiovascular biomarkers in men and women with high blood pressure: the ENCORE study. Arch Intern Med. 2010;170(2):126–35.
Azadbakht L, Surkan PJ, Esmaillzadeh A, Willett WC. The Dietary Approaches to Stop Hypertension eating plan affects C-reactive protein, coagulation abnormalities, and hepatic function tests among type 2 diabetic patients. J Nutr. 2011;141(6):1083–8.
Casas R, Sacanella E, Urpi-Sarda M, Chiva-Blanch G, Ros E, Martinez-Gonzalez MA, et al. The effects of the mediterranean diet on biomarkers of vascular wall inflammation and plaque vulnerability in subjects with high risk for cardiovascular disease. A randomized trial. PLoS One. 2014;9(6):e100084.
Romaguera D, Norat T, Mouw T, May AM, Bamia C, Slimani N, et al. Adherence to the Mediterranean diet is associated with lower abdominal adiposity in European men and women. J Nutr. 2009;139(9):1728–37.
Estruch R, Ros E, Salas-Salvado J, Covas MI, Corella D, Aros F, et al. Primary prevention of cardiovascular disease with a Mediterranean diet. N Engl J Med. 2013;368(14):1279–90.
Domenech M, Roman P, Lapetra J, Garcia de la Corte FJ, Sala-Vila A, de la Torre R, et al. Mediterranean diet reduces 24-hour ambulatory blood pressure, blood glucose, and lipids: one-year randomized, clinical trial. Hypertension. 2014;64(1):69–76.
Asemi Z, Tabassi Z, Samimi M, Fahiminejad T, Esmaillzadeh A. Favourable effects of the Dietary Approaches to Stop Hypertension diet on glucose tolerance and lipid profiles in gestational diabetes: a randomised clinical trial. Br J Nutr. 2013;109(11):2024–30.
Moore TJ, Alsabeeh N, Apovian CM, Murphy MC, Coffman GA, Cullum-Dugan D, et al. Weight, blood pressure, and dietary benefits after 12 months of a web-based nutrition education program (DASH for health): longitudinal observational study. J Med Internet Res. 2008;10(4):e52.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Samantha L. Gardener and Stephanie R. Rainey-Smith declare they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Neurological Disease and Cognitive Function
Rights and permissions
About this article
Cite this article
Gardener, S.L., Rainey-Smith, S.R. The Role of Nutrition in Cognitive Function and Brain Ageing in the Elderly. Curr Nutr Rep 7, 139–149 (2018). https://doi.org/10.1007/s13668-018-0229-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13668-018-0229-y