Abstract
Hepatocellular carcinoma (HCC) has many options for management; some of them are complicated by development of portal hypertension (PHT). Doppler ultrasound is an effective method to diagnose and monitor PHT changes after HCC ablation procedures. The aim of this study is to investigate changes in portal pressure hemodynamics of HCC patients following treatment with different interventional strategies: radiofrequency ablation (RFA), microwave ablation (MWA), and transarterial chemoembolization (TACE). A total of 60 patients with HCC were divided into three main groups, and each group received a different type of therapy (RFA, MWA, and TACE). Full medical record and basic investigations were performed including Doppler ultrasound and upper GIT endoscopy for evaluation of PHT parameters, and then repeated after three months of ablation. RFA is associated with the increased splenic artery resistive index, while MWA has no significant impact on PHT indices. TACE has led to a marked increase in liver vascular index with significant decrease in hepatic artery resistive index and PHI after treatment. No significant changes in esophageal varices were observed by upper GIT endoscopy following all ablation methods. RFA is quite safe but associated with degree of PHT. On the contrary, TACE is associated with improved PHT parameters. MWA has no significant association to development of PHT following the technique. Doppler ultrasound could be used as a reliable and effective method of evaluation of PHT post ablation for HCC.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Hepatocellular carcinoma (HCC) is the sixth among the cancer types occurring worldwide, and the second largest causal factor to cancer mortality [1]. The incidence of HCC is rising all over the world, especially due to a rising incidence of nonalcoholic fatty liver disease (NAFLD) and a rapid rise in the number of patients with hepatitis C-induced cirrhosis. About 80% of HCC patients are cirrhotic patients [2].
Although advances in screening, diagnosis, and therapy have greatly improved the prognosis of HCC patients, HCC remains a catastrophic tumor because of high rates of metastases and recurrence [3, 4]. Although curative measures, such as surgical resection and liver transplantation, continue to be the gold standard, approximately from 70% to 80% of patients are poor candidates for such invasive procedures. Locoregional therapy has become increasingly important for patients with HCC because of advances in techniques, survival benefit, and a favorable safety profile [5, 6].
The development of portal hypertension (PHT) is a crucial event in the evolution of cirrhosis and is defined by an increase in the portal pressure above the normal range of 1–5 mmHg, as measured by the hepatic vein pressure gradient (HVPG). When the HVPG increases further to ≥10 mmHg, PH is defined as clinically significant [7].
Portal hypertension (PHT) may occur after ablation procedures of HCC, which is considered one of the major complications following these methods of intervention [8–10].
In PHT imaging, the liver vascular index (LVI) is a highly sensitive and specific Doppler ultrasound parameter in the diagnosis of cirrhosis and PHT [11]. Also, the assessment of the hepatic vein waveform with Doppler US could be considered a useful adjunctive method in the noninvasive assessment of the severity of PHT [12]. The hepatic artery pulsatility index (HAPI), Liver vascular index, and Congestion index (CI) are indicative indices in patients with PHT, suggesting that color Doppler ultrasonography can be used as a noninvasive evaluation method for evaluating the PHT degree [13].
The aim of this study is to investigate changes in portal pressure hemodynamics of HCC patients following treatment with different interventional strategies such as radiofrequency ablation (RFA), microwave ablation, and transarterial chemoembolization.
Materials and methods
This study was a prospective interventional (Randomized Control Trial) study. It was conducted in the Tropical Medicine Department of Mansoura University Hospital, Egypt.
HCC diagnosis was confirmed by triphasic abdominal computerized tomography scan or dynamic contrast-enhanced MRI. Diagnosis was based on the identification of the typical hallmark of HCC (hyper vascular in the arterial phase with washout in the portal venous or delayed phases).
The inclusion criteria were as follows: (i) Patients exhibiting good compliance and providing informed consent. (ii) Patients with primary HCC and naïve to treatment. (iii) Patients with liver cirrhosis of Child-Pugh class A or B.
Thirteen patients who met the exclusion criteria included those with metastatic tumor and liver cirrhosis of Child-Pugh class C, and also those who had refused to participate in the study were excluded from the study.
This study included three main groups: Group A (RFA group): Patients in this group were treated with RFA; Group B (MWA group): Patients in this group were treated with microwave ablation, MWA; and Group C (TACE group): Patients in this group were treated with transarterial chemoembolization therapy, TACE. An informed consent was obtained before patients were enrolled in the study.
All participants in all groups were subjected to full history taking, clinical examination (general and abdominal examination), liver function tests (serum albumin level, serum bilirubin level, and international normalized ratio), anti-HCV antibodies, and HBs antigen by the third-generation ELISA, serum alpha fetoprotein level (AFP), abdominal ultrasonography, triphasic abdominal computerized tomography, and color Doppler ultrasonography for measurement of portal blood pressure before treatment and three months after treatment.
Upper gastrointestinal endoscopy was performed for all patients before treatment for diagnosis of esophageal varices and three months after treatment in a single endoscopy unit using an Olympus GIF-Q240 gastrointestinal videoscope (Olympus Corporation, Tokyo, Japan).
Esophageal varices were classified at endoscopy according to Sandy and Feinman scoring system as F I (Small, straight varices), F II (Enlarged, tortuous varices that occupy less than one-third of the lumen), or F III (Large, coil-shaped varices that occupy more than one-third of the lumen).The interobserver variation coefficients for portal blood pressure measurements and the presence of varices were evaluated in all the patients (less than 2%).
After eight hours of fasting and bowel preparation, all patients were subjected to Doppler ultrasound for measurement of portal blood pressure before treatment and three months after treatment using a Toshiba Xario™ ultrasound (Toshiba Medical Systems Corporation, Toshio Takiguchi, Japan).
Color Doppler was used to assess specific and sensitive Doppler ultrasound parameters that are shown in Table 1; see also (Fig. 1).
Doppler indices were obtained from portal trunk, proper hepatic artery, and splenic artery and flow velocity measured during quiet respiration.
Data were analyzed using SPSS version 21. The normality of data was first tested by Shapiro–Wilk test.
Qualitative data were described using number and percent. Association between categorical variables was tested using Chi-square test. Continuous variables were presented as mean ± standard deviation (SD). Paired t test (parametric data) and Wilcoxon Signed Ranks (nonparametric data) were used to compare paired two groups. Analysis of variance (ANOVA test) used for comparison of means of more than two groups, while Kruskal Wallis Test was used for comparison of medians of more than two groups (nonparametric data)
For all the above-mentioned statistical tests done, the threshold of significance is fixed at 5% level (p value).
The results were considered nonsignificant when the probability of error is more than 5% (p > 0.05), significant when the probability of error is less than 5% (p < 0.05), and highly significant when the probability of error is less than 0.1% (p < 0.001).The smaller the p-value obtained, the more significant are the results.
Results
This study was conducted on 60 patients selected from 73 patients diagnosed with HCC. Of the patients with HCC, there were 36 males and 24 females, and their ages ranged from 37 to 63 years with the mean age of (57.6 ± 5.93). According to Child–Turcotte–Pugh classification, 50 patients were classified as class A and 10 as class B. (Table 2).
All the patients of the study had HCV infection as a cause of liver cirrhosis and HCC subsequently.
Our patients performed a variety of clinical interventional procedures including RFA (20), MWA (20), and finally TACE (20). All the patients survived to the date of follow-up with no major complications or morbidity.
The changes in liver function tests after treatment were statistically not significant (Table 3).
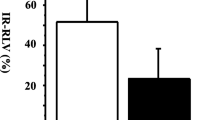
Changes in Doppler ultrasound parameters after treatment in the groups of HCC patients are shown in Tables 4 and 5, which demonstrate the tendency of partial variables changes. In the RFA group, the PVVel and LVI nonsignificantly decreased after treatment (p = 0.48 and 0.601, respectively) with no significant increase in the HAPI, hepatic artery resistive index (HARI), CI and PHI (p = 0.672, 0.736, and 0.167 respectively), but the splenic artery resistive index (SARI) significantly increased (p = 0.003).In the MWA group; there were no significant differences in all the studied Doppler ultrasound parameters. In the TACE group, the LVI remarkably increased after treatment (p = 0.027), with HARI and PHI, however, dramatically decreasing after treatment (p = 0.13), but there were no significant changes in the other studied Doppler parameters (Figs. 2, 3).
Doppler ultrasonography of a 54-year-old man with HCC in the right lobe of the liver treated with TACE. A Measurement of PVVel before the ablation. There was a significant increase in PVVel after treatment (B). C HAPI and HARI before the ablation. D Significant decreases of both HAPI and HARI after treatment
In all the three groups, there were no significant differences in the levels of esophageal varices after treatment (Table 6).
Discussion
Hepatocellular carcinoma (HCC) is becoming increasingly as one of the leading causes of mortality and morbidity worldwide; this is due to many factors mainly including the increased incidence of liver cirrhosis and prevalence of viral hepatitis mostly of HCV and HBV types. Liver cirrhosis always leads to PHT and all its consequent complications such as bleeding esophageal varices, ascites, hepatic encephalopathy, as well as HCC.
Different treatment modalities have been discovered and applied successfully, ranging from hepatic resection to percutaneous ablation methods up to TACE technique, with satisfactory results of healing. However, these methods of intervention have their respective specific side effects and hazards, which may limit its use under certain circumstances. One of these risks is the development or the increased degree of PHT following the ablative method. Increased PHT may lead to the decreased effectiveness of the ablation process or the development of some other morbid conditions.
Using ultrasound for detection and monitoring of PHT is one of the most popular and the preferred methods due to its noninvasiveness, accuracy, and low cost. In our study, color Doppler was used to assess specific and sensitive Doppler ultrasound parameters concerning PHT such as, PVD, PVVel, HAPI, HARI, SARI, LVI, CI, and PHI. Patients were assessed before and three months after ablation. Sixty patients were divided into three groups (RFA, MWA, and TACE).
Few papers in the literature have described post-ablative side effects especially with regard to PHT. RFA complications were widely studied; however, only very few were carried out on TACE.
Concerning PHT parameters by Doppler ultrasound, no significant changes in portal indices were noted in RFA group apart from SARI (p = 0.003), indicating a marked increase in the portal resistance after ablation. The RFA electrodes cause alteration of currents, agitation of ions, and generation of fractional heat leading to destruction of tumor tissue including small blood vessels and generation of PHT. In a multicenter study by Livraghi et al. [8], PHT developed in one case due to generation of arterioportal shunt following RFA which was not the case in our study, since we had no shunt.
Also there were no changes in the levels of esophageal varices after RFA as evidenced by the upper endoscopy, and this result is a clinical parameter of RFA’s safety and long-term efficacy in hepatic patients who suffered from HCC. Although SARI has increased, it was not reflected upon the esophageal pressure and variceal development. This is in contrast to Sonomura et al. [9] who reported a case of a patient with rapid deterioration of esophageal varices caused by PHT accompanied by a large arterioportal shunt that developed after RFA of HCC. However, the incidence was low, and only large arterioportal shunt can cause significant PHT and variceal bleeding.
In the MWA group, there were no statistically significant results concerning PHT parameters by Doppler ultrasound; this reflects the idea that MWA is quite safe and very unlikely to cause PHT or affect tissue resistance or blood velocity, and also that it was not associated with any disturbance in esophageal varices after the ablation sessions.
MWA is another form of thermal ablation for HCC, which involves the use of microwave energy that causes molecular vibration of dipoles, especially water molecules in tissue, and produces dielectric heat and thermal coagulation around the electrode [14]. In our results, MWA was not associated with PHT contrary to RFA even though the agent of ablation in both RFA and microwave ablation is heat; this is because the mechanism of delivery differs. The amount of heat in MWA does not depend on the passage of electricity through tissues. There is no heat–sink effect in MWA, and it can be used to ablate tumors adjacent to major vessels. These factors lead to a large ablation volume, and result in good local control and fewer complications [15]; moreover, this fact matches with our results concerning MWA and PHT.
Regarding TACE group, marked decreases in tissue resistances and PHT parameters have been noted as evidenced by the significant results in HARI (p = 0.04) (decreased), LVI (p = 0.027) (increased), and PHI (p = 0.013). These results are in contrast with many studies in the literature [10–17], which reported increase in the clinical features of PHT following ablation procedures. However, Tasneem et al. [10] reported post-TACE syndrome and cirrhosis decompensation and concluded that severe complications of TACE correlated to increased PHT before the procedure, but not as a consequence of the ablation itself.
The increased PHT could be explained on the basis of severe necro-inflammation of blood vessels and adjacent tissues due to the nature of the therapeutic chemical substance used in ablation leading to vascular obliteration, increased tissue resistance, and finally PHT. However, HCC ablation may lead to improved portal circulation, remove malignant debris from vascular tissue, prevent seeding of micrometastatic foci, and improve portal HTN consequently as detailed in the results of our study.
Again, the decreased portal pressure following TACE had no clinical impact on esophageal varices, and did not result in any significant change in upper endoscopic observations, raising the suspicion regarding the effectiveness of using endoscopic technique as an indirect method for the evaluation and follow-up of PHT.
Conclusion
Different methods of treatment of HCC are now available, with varying degrees of side effects and complications. RFA is quite safe and effective method of intervention; however it is associated with degree of PHT. On the contrary, TACE is associated with the improved PHT parameters. MWA has no significant association to development of PHT following the technique. Doppler ultrasound could be used as a reliable and effective method of evaluation of PHT post ablation for HCC.
The monitoring of esophageal varices by upper endoscopy revealed no significant changes in variceal grades post HCC ablation by different methods.
There were some limitations in our study. First, the sample size is still limited as this study focused on the effect of interventional techniques that need certain criteria to be fulfilled. Second, the follow up of the patients was for short period which limited the detection of recurrence of HCC if present. So, more studies with large sample size and for longer period are recommended.
References
Ferlay J, Shin HR, Bray F, et al. (2010) Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008. Int J Cancer 127(12):2893–2917
Simpson HN, McGuire BM (2015) Screening and detection of hepatocellular carcinoma. Clin Liver Dis 19(2):295–307
Bruix J, Gores GJ, Mazzaferro V (2014) Hepatocellular carcinoma: clinical frontiers and perspectives. Gut 63(5):844–855
Fausto N (2004) Liver regeneration and repair: hepatocytes, progenitor cells, and stem cells. Hepatology 39(6):1477–1487
Govaere O, Roskams T (2015) Pathogenesis and prognosis of hepatocellular carcinoma at the cellular and molecular levels. Clin Liver Dis 19(2):261–276
Llovet JM, Burroughs A, Bruix J (2003) Hepatocellular carcinoma. Lancet 362:1907–1917
Casado M, Bosch J, García-Pagán JC, et al. (1998) Clinical events after transjugular intrahepatic portosystemic shunt: correlation with hemodynamic findings. Gastroenterology 114(6):1296–1303
Livraghi T, Solbiati L, Meloni MF, et al. (2003) Treatment of focal liver tumors with percutaneous radio-frequency ablation: complications encountered in a multicenter study. Radiology 226(2):441–451
Sonomura T, Kawai N, Kishi K, et al. (2014) N-butyl cyanoacrylate embolization with blood flow control of an arterioportal shunt that developed after radiofrequency ablation of hepatocellular carcinoma. Korean J Radiol 15(2):250–253
Tasneem AA, Abbas Z, Luck NH, Hassan SM, Faiq SM (2013) Adverse events following transarterial chemoembolization for hepatocellular carcinoma and factors predicting such events. J Pak Med Assoc 63(2):239–244
Iwao T, Toyonaga A, Oho K, et al. (1997) Value of Doppler ultrasound parameters of portal vein and hepatic artery in the diagnosis of cirrhosis and portal hypertension. Am J Gastroenterol 92(6):1012–1017
Baik SK, Kim JW, Kim HS, et al. (2006) Recent variceal bleeding: Doppler US hepatic vein waveform in assessment of severity of portal hypertension and vasoactive drug response. RSN 240(2):574–580
Zhang L, Duan YY, Li JM, Yin JK (2007) Hemodynamic features of Doppler ultrasonography in patients with portal hypertension. J Ultrasound Med 26:1689–1696
Tabuse K, Katsumi M, Kobayashi Y, et al. (1985) Microwave surgery: hepatectomy using a microwave tissue coagulator. World J Surg 9(1):136–143
Thandassery RB, Goenka U, Goenka MK (2014) Role of local ablative therapy for hepatocellular carcinoma. J Clin Exp Hepatol 4(Suppl 3):S104–S111
Liang SN, Liu LL, Su HY, et al. (2008) Analysis of severe complications after transcatheter arterial chemoembolization for primary hepatocellular carcinoma. Zhonghua Zhong Liu ZaZhi 30(10):790–792
Chan AO, Yuen MF, Hui CK, Tso WK, Lai CL (2002) A prospective study regarding the complications of transcatheter intraarterial lipiodol chemoembolization in patients with hepatocellular carcinoma. Cancer 94(6):1747–1752
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was taken from each patient. The research protocol was duly approved by the Ethical Committee of Faculty of Medicine, Mansoura University.
Rights and permissions
About this article
Cite this article
El Sherbiny, W., AbdelRahman, A., Diasty, M. et al. Changes in Doppler parameters of portal pressure after interventional management of hepatocellular carcinoma. Abdom Radiol 41, 1532–1538 (2016). https://doi.org/10.1007/s00261-016-0704-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-016-0704-0