Abstract
Rhabdoid tumors are rare malignancies that typically present in infants and children. The most common anatomic locations are the central nervous system, where they are referred to as atypical teratoid/rhabdoid tumor (AT/RT), the kidney, and other soft tissues (extra-renal rhabdoid tumor). The vast majority of rhabdoid tumors arise as the result of homozygous inactivation of the SMARCB1 gene on chromosome 22. Predisposing germline mutations or copy number alterations of SMARCB1 are present in approximately 25% of patients. Germline and acquired mutations of the SMARCA4 locus have also been described in probands and family members with rhabdoid tumors. This chapter will address the spectrum of alterations seen in rhabdoid tumors and related malignancies associated with SMARCB1, as well as summarize our current and evolving approaches to genetic counseling for this disease.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Rhabdoid tumor is a rare, clinically aggressive, and often fatal malignancy that typically arises in infants and young children. The most common anatomic locations are the central nervous system, referred to as atypical teratoid/rhabdoid tumor (AT/RT), kidney (malignant rhabdoid tumor, MRT or RTK), and soft tissues (extra-renal rhabdoid tumor), including the lung, liver, orbit, neck, skin, and extremities. Rhabdoid tumors account for approximately 1–2% of renal [1] and brain tumors [2] in the pediatric population. There is a slight male predominance [1, 2]. Rhabdoid tumors in all anatomic locations have a peak incidence in the first 3 years of life, and those infants diagnosed in the neonatal period through the first year of life have the worst prognosis [1]. Patients often present with metastatic disease at diagnosis, which impacts therapy and is a negative predictor of outcome. Successful treatment requires surgery and combination chemotherapy regimens, often accompanied by stem cell rescue, with or without radiation therapy [3,4,5,6,7,8,9,10,11]. Although 5-year survival rates were originally less than 11% [3, 4], limited institution [5] and European collaborative group studies (EU-RHAB) [10] and the first prospective Children’s Oncology Group Trial ACNS0333 [9] suggest that short-term survival may approach 40% with the introduction of more intensive regimens. However, the associated morbidity that results from high-dose chemotherapy and radiation, especially in infants with AT/RT, is significant. Novel strategies utilizing direct injection of oncolytic viruses or poly(beta-amino ester) nanoparticles containing herpes simplex virus type I thymidine kinase are in development, based on their effective inhibition of rhabdoid tumor cell proliferation both in vitro and in xenograft studies using RT cell lines [12,13,14], and may help avoid some of the toxicity associated with chemotherapy and cranial radiation.
Rhabdoid tumor of the kidney was initially described as a rhabdomyosarcomatous variant of Wilms tumor [15], although it is now known that the genetic etiologies for Wilms tumor, rhabdomyosarcoma, and MRT are quite distinct. During the next two decades, histologically similar tumors in the brain and soft tissues were described [16, 17]. The most interesting of these reports was a case series that included seven patients with synchronous embryonal tumors of the brain and MRT [18]. In the first extensive report from the National Wilms Tumor Study Group, 15 of 111 patients with MRT also had a malignant brain tumor, suggesting that they had a genetic cancer predisposition syndrome [19].
Rorke et al. [2] reported the first large series of patients with rhabdoid tumors of the brain, in which they described the complex histology of these tumors. Less than 15% of the tumors presented with pure rhabdoid histology. The rhabdoid cells had large eccentrically placed nuclei with prominent nucleoli and abundant and eosinophilic cytoplasm composed of whorls of intermediate filaments, visible by electron microscopy, which showed positive staining with antibodies to epithelial membrane antigen (EMA) and vimentin (Fig. 3.1). In addition to the rhabdoid component, the vast majority of tumors had areas composed of densely cellular tumor mimicking primitive neuroectodermal tumor (PNET). Epithelial differentiation was normally confined to a few small, gland-like spaces, and a fascicular architecture lent a sarcoma-like or mesenchymal appearance. This combination of malignant histologic components was reminiscent of what is seen in teratomas and led Rorke to coin the name “atypical teratoid tumor” (ATT). The term in use today, AT/RT, exemplifies the finding that tumors may contain a variety of distinct histologic areas, with or without a predominant rhabdoid component. Although the cell of origin has not been confirmed and may be age-dependent, in vitro and in vivo models of rhabdoid tumors have suggested that they arise from pluripotent or neural stem cells [20,21,22]. In mice, the phenotype is exquisitely sensitive to gestational age and promoter used for inactivating the key driver of rhabdoid tumors, SMARCB1.
Representative histopathology of AT/RT. (a) AT/RT cells demonstrate peripherally placed nuclei, prominent nucleoli, and eosinophilic cytoplasm (H&E, magnification—400×). (b) Immunohistochemistry analysis shows loss of SMARCB1 protein expression is seen in AT/RT cells along with positive SMARCB1 staining in the endothelial cells (SMARCB1, magnification—200×). (c) Scattered AT/RT cells show immunoreactivity for epithelial membrane antigen (EMA) (EMA, magnification—200×). (d) AT/RT cells are strongly immunoreactive for vimentin (vimentin, magnification—200×). (Figure provided by Dr. Mariarita Santi)
Renal and extra-renal soft tissue rhabdoid tumors also demonstrate complex histologic patterns with rhabdoid cells and primitive neuroepithelial, epithelial, spindle, and lymphoid cells [17, 19, 23, 24]. This is especially true for epithelioid sarcomas, which may be difficult to distinguish from extra-renal rhabdoid tumor.
3.1 Identification of SMARCB1 Alterations in Rhabdoid Tumors
Cytogenetic studies yielded the first clues as to the genetic etiology of rhabdoid tumors. Several case reports and small clinical cohorts of children with MRT, AT/RT, and extra-renal rhabdoid tumors described overlapping deletions in chromosome band 22q11.2, suggesting the presence of a tumor suppressor gene that mapped to this region of the genome. Versteege et al. [25] first reported somatic mutations of the hSNF5 (INI1 ) gene in MRT and extra-renal rhabdoid tumors, followed shortly thereafter by the report from Biegel et al. of germline and somatic mutations in INI1/hSNF5 in patients with rhabdoid tumors of the brain, kidney, and soft tissues [26]. SMARCB1, for SWI/SNF-related, matrix-associated, actin-dependent regulator of chromatin, subfamily B, member 1, is now the recommended nomenclature for this gene, replacing the former names human sucrose nonfermenting gene number 5 (hSNF5), integrase interactor 1 (INI1) , and 47-Kd Brg1/Brm-associated factor (BAF47).
SMARCB1 is a member of the human SWI/SNF complex [27, 28]. The SWI/SNF complex acts in an adenosine triphosphate (ATP)-dependent manner to remodel chromatin and both activates and represses gene transcription. In the cancer setting, SMARCB1 functions as a tumor suppressor gene. Tumors arise as a consequence of inactivation of both copies of the gene, due to mutations, structural alterations, and mitotic recombination events leading to loss of heterozygosity. The homozygous inactivation of the genomic locus results in loss of nuclear expression of the SMARCB1 protein, which facilitated the development of a specific immunohistochemistry (IHC) assay for SMARCB1 (Fig. 3.1) [29]. The IHC assay has had unsurpassed clinical utility for distinguishing rhabdoid and related SMARCB1-associated tumors from other brain tumors, including medulloblastoma, primitive neuroectodermal tumor (PNET), and choroid plexus carcinoma (CPC) [29], as well as a variety of tumors in soft tissues [30]. Rhabdoid tumors may also arise in the setting of a previously benign tumor, in both the brain [31, 32] and peripheral nervous system [33, 34], following acquisition of a SMARCB1 mutation and/or deletion. The loss of expression of SMARCB1 by IHC clearly distinguishes the rhabdoid areas from the other (less malignant) components of the tumor. Although SMARCB1 is the predominant gene altered in rhabdoid tumors, approximately 2–3% of tumors with rhabdoid histology retain expression of the SMARCB1 protein by IHC and do not display inactivating mutations in the gene. Less than 1% of these tumors arise as a consequence of germline and/or somatic alterations of a second rhabdoid tumor predisposition locus, SMARCA4 [35, 36]. The majority of germline SMARCA4 mutations have been associated with small cell carcinoma of the ovary hypercalcemic type (SCCOHT) [37, 38], leading to the hypothesis that SCCOHT is a variant of extra-renal rhabdoid tumor with a different cell of origin. It is likely that the remaining rhabdoid tumors without SMARCB1 inactivation will also demonstrate alterations in other members of the SWI/SNF or another chromatin-remodeling complex.
A combination of approaches has been used to characterize the spectrum of alterations of SMARCB1 and chromosome 22 in patients with rhabdoid tumors, including standard cytogenetic analysis and preparation of karyotypes, fluorescence in situ hybridization (FISH), Sanger-based and next-generation sequencing of genomic DNA or cDNA, and single-nucleotide polymorphism (SNP)-based genomic arrays [25, 26, 39,40,41,42]. A representative SNP array profile for chromosome 22 is shown in Fig. 3.2, demonstrating a large deletion in the proximal part of 22q and a smaller deletion that includes exons 6–9 of SMARCB1. Confirmation of the exon 6 to 9 deletion was performed by multiplex ligation probe amplification (MLPA). MLPA is currently the most sensitive clinical assay used for detecting intragenic deletions or duplications in SMARCB1 and has revealed a spectrum of single or multi-exon deletions and duplications in SMARCB1 in both the germline and tumor tissue in patients with rhabdoid tumors from all anatomic locations [42,43,44].
Intragenic homozygous deletion in SMARCB1 revealed by Illumina (San Diego, CA) Human610-Quad single-nucleotide polymorphism (SNP) array. The upper plot shows the B-allele frequency and the lower plot the intensity (LogR) ratio for chromosome 22 in a single rhabdoid tumor. A deletion of the proximal portion of chromosome 22 from 22q11.1 to 22q12.1 is apparent from the loss of heterozygous alleles and the lower intensity ratio. An overlapping deletion in 22q11.23, demonstrated by the further decrease in the intensity plot, encompasses the genes shown in the blue boxes, resulting in a homozygous deletion of exons 6–9 of SMARCB1. Genes are not drawn to scale
Despite the fact that rhabdoid tumors are one of the most clinically aggressive tumors in the pediatric population, the tumors are typically diploid with few genetic alterations other than SMARCB1 and chromosome 22 loss [41, 42]. Genomic inactivation of SMARCB1 (and related SWI/SNF complex members) may be the only sequence-level event necessary for a tumor to develop. Whole exome and genome sequencing studies of rhabdoid tumors demonstrated mutations or deletions of SMARCB1 in virtually every tumor, and there were no other consistently mutated or altered genes [41]. Rhabdoid tumors, in fact, exhibit the lowest frequency of mutations overall compared to every other tumor type analyzed to date [45]. While cooperating genetic events in early murine models of rhabdoid tumors implicated a role for Tp53 and Smarcb1 [46], or Rb and Smarcb1 [47] in tumor development, the human tumors do not appear to have TP53 or RB1 mutations [41, 48].
The distribution of SMARCB1 and chromosome 22-inactivating mutations , deletions, and copy number neutral loss of heterozygosity (CN-LOH) in 193 sporadic AT/RTs, MRTs, and extra-renal rhabdoid tumors are shown in Table 3.1. In the majority of tumors (45.5%), there is a mutation in one allele, and the second copy of the gene is lost due to either a structural deletion in 22q11.2, monosomy 22, or as a result of an acquired CN-LOH event. Compound heterozygous mutations are infrequent in these patients (4%). Partial deletions and duplications, revealed by SNP array or MLPA, are detected in 15.5% of tumors. Homozygous deletions of exons 1–9 of SMARCB1 are present in 39% of rhabdoid tumors overall, although there is an unequal distribution with respect to anatomic location. Approximately 25% of AT/RTs, 40% of MRTs, and 70% of extra-renal rhabdoid tumors have homozygous deletions of the entire locus.
The mutations in sporadic rhabdoid tumors include single base-pair point mutations and insertion/deletion (indel) or frameshift mutations that are predicted to introduce a novel stop codon. The majority of mutations have been proposed to result in nonsense-mediated decay, although this has not formally been proven in most cases. The highest frequency of coding sequence mutations among the sporadic tumors is seen in exon 9. Single base deletions in codons 382 and 383 are somatic in origin and associated exclusively with AT/RT [26, 44]. Mutations in exons 2 and exons 4–7 are frequently observed in MRT and AT/RT. Four specific mutations, c.118C>T, c.157C>T, c.472C>T, and c.601C>T, in exons 2, 2, 4, and 5, respectively, are highly recurrent, although they do not appear to be specific for the brain or kidney [26, 43, 44]. Mutations in exons 1, 3, and 8 are rare. A low frequency of splice site mutations has been documented in sporadic rhabdoid tumors, resulting in loss of an exon in the processed message, similar to that predicted by MLPA. In contrast to the above mentioned nonsense mutations and indels, missense mutations do not appear to lead to inactivation of SMARCB1 in primary rhabdoid tumors. Interchromosomal balanced translocations result in loss of SMARCB1 in renal medullary carcinomas [49] and could mediate loss of protein expression of SMARCB1 in the small number of rhabdoid tumors with only one documented inactivating deletion or mutation of this locus. Mutations in non-coding regions of the SMARCB1 locus may also lead to altered splicing in rhabdoid tumors, which may be present in the germline and missed by routine clinical copy number and sequencing-based assays [50].
3.2 Germline Alterations in SMARCB1 Predispose Individuals to the Development of Rhabdoid Tumor
The initial hypothesis that there was a genetic predisposition to rhabdoid tumor was based on reports of individuals who presented with a synchronous brain and kidney tumor or with bilateral renal tumors [18, 19]. The histology of the two tumors was distinct, and they did not appear to be metastases. Lynch et al. [51] reported one family in which two sisters developed paravertebral tumors, but the classic presentation of multi-generation families with rhabdoid tumors was not observed. This was likely due to the fatal nature of these malignancies, which was confirmed once SMARCB1 was identified as the primary rhabdoid tumor predisposition locus [26]. In fact, germline mutations, deletions, or intragenic duplications of SMARCB1 are most often de novo [43, 44]. Early reports of patients with inherited SMARCB1 mutations highlighted families with two or more affected first-degree relatives who inherited a mutation from an unaffected parent [40, 52,53,54]. There was reduced penetrance for the germline mutations of SMARCB1 and rhabdoid tumor in these families, and as of yet estimates of cancer risk in carriers have not been established. Sevenet et al. [53] described two families with multiple affected siblings and presumed gonadal mosaicism in one of the parents, which has subsequently been confirmed in additional families [44, 55]. Plon et al. [40] also reported one patient with an apparently de novo, germline mosaic, single-exon deletion in SMARCB1, indicating that sensitive detection methods are required to effectively rule out the presence of a predisposing germline alteration in affected individuals.
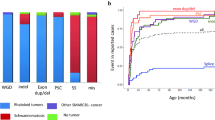
Twenty-five to 35% of newly diagnosed patients with rhabdoid tumor, and almost all children with two primary tumors, have a germline alteration of SMARCB1 that predisposed them to cancer [43, 44, 56, 57]. These children are much more likely to be diagnosed in the first year of life than patients with sporadic malignancies (Fig. 3.4). In our patient cohort, the median age at diagnosis for the patients with germline SMARCB1 alterations was 0.5 years (range, 1 day to 5 years) compared to a median age at diagnosis of 1.5 years (range, 1 day to 32 years) for patients with sporadic tumors (Fig. 3.3).
The spectrum of germline mutations, deletions, and duplications from patients with rhabdoid tumors generally reflects that seen in sporadic tumors (Table 3.2 and Fig. 3.4). Approximately 20% of the germline alterations are deletions in chromosome band 22q11.2 that include all of SMARCB1, whereas 25% of the patients have a partial deletion or duplication involving one to five exons of the gene. The remaining patients have a variety of truncating mutations due to single base point mutations or indels leading to a frameshift. Splice site mutations are the least common type of mutations observed in children who first present with a rhabdoid tumor [58].
Three specific mutations, c.118C>T in exon 2, c.157C>T in exon 2, and c.472C>T in exon 4, are the most frequently detected germline mutations [26, 43, 44]. With the exception of the two exon 9 frameshift mutations described below, the same mutations predispose carriers to AT/RT, MRT, and to a lesser extent extra-renal tumors, even in the same patient. In contrast, the two most common mutations in AT/RT, the single base deletions c.1144del and c.1148del (exon 9), have not been detected as a predisposing mutation in the blood from these patients [58]. These two frameshift mutations are not predicted to be subject to nonsense-mediated decay and theoretically would result in the addition of 100 amino acids to the protein. Similar to the other rhabdoid tumors with coding sequence alterations, there is no expression of the protein by immunohistochemistry in AT/RTs with these two exon 9 deletions [29]. It is possible that this mutation functions as a dominant negative mutation during early development, which is an area for future research.
The distribution of the second inactivating events in tumors from the patients with germline SMARCB1 alterations is shown in Table 3.2. The most frequent second hit is a large 22q deletion or monosomy 22 or a CN-LOH-generating event that unmasks the mutation or deletion on the remaining allele.
The most common chromosomal deletion syndrome in the general population is the 22q11.2 deletion associated with DiGeorge and Velocardiofacial syndrome (DGS/VCFS) [59]. Patients with this genomic disorder have a constellation of abnormalities, including cleft palate, immune deficiency, abnormal ears, heart defects, learning differences, and an increased risk for schizophrenia [59]. The majority of patients with classic DGS/VCFS have deletions mediated by low copy repeats A to D in chromosome band 22q11.2 [59,60,61]. More distal deletions, which typically include BCR (breakpoint cluster region), are associated with a less severe and more variable phenotype [62,63,64,65,66]. Those patients with deletions that extend to low copy repeat G are deleted for SMARCB1 and thus are at increased risk for rhabdoid tumor [39, 44, 67,68,69,70,71]. With the adoption of high-resolution genomic arrays as the first-tier test for patients with a suspected genomic disorder [72], the identification of infants and young children with distal 22q11.2 deletions that include SMARCB1 as an incidental finding is becoming more common. This will likely increase as whole-genome copy number analysis and sequencing are utilized in the prenatal setting. Genetics professionals will need to counsel these families about the risk for malignancies in these patients as well as a future risk for development of schwannoma.
Patients with other constitutional structural abnormalities of chromosome 22, including ring chromosomes [73] or deletions of distal 22q13 [74], also appear to be at increased risk for development of rhabdoid tumors. The unstable nature of these structurally altered chromosomes is likely related to the increased risk for monosomy 22, a frequent somatic event in rhabdoid tumors. In contrast, cancers in individuals with the supernumerary derivative chromosome 22 derived from the t(11;22)(q23;q11.2) have only rarely been reported [75, 76].
Rare patients have also been reported with a rhabdoid tumor and another genetic disorder, including Beckwith-Wiedemann syndrome [77], neurofibromatosis type 1 (NF1) [78], epidermolysis bullosa [79], and Goldenhar syndrome [67]. Modena et al. [80] also reported a patient with a germline SMARCB1 mutation and mosaic Klinefelter syndrome. At the present time, the occurrence of the two genetic disorders appears to be coincidental.
In contrast to the known risk, albeit with reduced penetrance, for carriers of SMARCB1 alterations to develop rhabdoid tumors, there are no established risk factors for the development of sporadic tumors. Heck et al. [81] performed the first population-based epidemiologic analysis as part of an Air Pollution and Childhood Cancer Study in the state of California. Demographic data and pregnancy history were collected from a total of 105 children with rhabdoid tumors and 208,178 controls under 6 years of age. Fathers were more likely to be white and non-Hispanic, and mothers to have completed a higher level of education than controls. Cases were also more likely to have had private health insurance. The significant findings from the study were an association with low birthweight, preterm birth, and late-term delivery. Of interest, twin pregnancies were seen in association with rhabdoid tumor, which has also been noted by Bourdeaut et al. [43], and in a single-institution case series by Nicolaides et al. [82] that included one twin pregnancy born after in vitro fertilization (IVF). Cecen et al. [83] also reported a single case of a rhabdoid tumor in a patient born after IVF, and we have studied an additional three tumors from children conceived by IVF who had de novo germline SMARCB1 mutations [unpublished data]. Although some studies suggest a small increased risk for cancer with the use of assisted reproductive technologies [84], this remains controversial [85]. While at present there is only anecdotal evidence to suggest that children born after IVF may be at risk for development of rhabdoid tumors, this should be a subject for further research.
Long-term genotype-phenotype studies are necessary in the context of clinical trials to determine the association of germline and acquired mutations and copy number alterations in SMARCB1 and SMARCA4 with patient outcome. Although patients with germline alterations in SMARCB1 typically present at an earlier age than patients with sporadic tumors, it is not yet known whether this accounts for the apparent increased risk for death in the youngest patients [1, 5, 9, 10]. Patients with germline mutations and deletions of SMARCB1 have an increased risk for development of second primary tumors, and virtually all patients with second tumors die of their disease. Whether this is due to the underlying presence of the mutation in all cells of their body or resistance to current therapies is also unknown.
3.3 Familial Schwannomatosis and SMARCB1
Neurofibromatosis type 2 is associated with alterations of the NF2 locus in chromosome band 22q12, and patients typically present with bilateral acoustic neuromas or vestibular schwannomas (OMIM#101000). Schwannomatosis is a distinct disorder, characterized by the presence of multiple schwannomas, which although histologically benign may result in severe morbidity (OMIM#162091). Treatment of schwannomas is challenging, since the goal is to avoid exposure to mutagenic and carcinogenic agents in a patient with a cancer predisposition syndrome [86]. Tumors that undergo malignant transformation, typically to malignant peripheral nerve sheath tumors, require surgery and chemotherapy.
Genetic association studies of patients with familial schwannomatosis initially demonstrated linkage to chromosome 22; however there were no constitutional mutations of the most likely candidate gene, NF2 [87]. Boyd et al. [88] and Hadfield et al. [89] demonstrated that approximately one third of patients with familial schwannomatosis have germline mutations in the SMARCB1 gene. Early genotype-phenotype studies suggested that both splice site mutations and mutations in exon 1 were more common in the familial schwannoma cases than in rhabdoid tumors. A link to NF2 was nonetheless established with published reports of concomitant deletions in NF2 in the tumors from these patients. As monosomy 22, large 22q11.2–22q12 deletions, and CN-LOH can all result in loss of the wild-type copy of both SMARCB1 in 22q11.23 and NF2 in 22q12, the inactivation of either or both of these loci may influence the phenotype and malignant potential of schwannomas in these families [86].
Some of the most interesting families that have been reported to date are those in which the same germline-inactivating mutation of SMARCB1 results in schwannoma in older individuals and classic AT/RT in the second and/or third generation [44, 55, 90, 91]. We reported one family in which the proband presented with an AT/RT in infancy [44]. She was found to have a characteristic germline c.472C>T SMARCB1 mutation. Her father and paternal grandmother were subsequently shown to carry the same germline mutation, and each was also reported to have one or more schwannomas that presented in adulthood. Of note, the proband’s paternal great-uncle died in childhood from a malignant brain tumor, which in retrospect was likely an AT/RT. Similar families have been reported with single-exon deletions, duplications, and splice site mutations [55, 91].
It is noteworthy that the families that are ascertained due to the occurrence of a child with a rhabdoid tumor often have a history of a relative who died at a young age with one or more tumors [55], but adult members of the family who are mutation carriers are typically unaffected or develop schwannomas. This suggests that there is a window of time during the early years when the risk for a rhabdoid tumor is the greatest and that the risk decreases with age. This is more typical of families with embryonal tumors, such as retinoblastoma or Wilms tumor, as compared to carriers of mutations in more commonly altered tumor suppressor genes such as BRCA1 or PTEN. The majority of adults with rhabdoid tumors appear to have sporadic disease [92] with acquired inactivating SMARCB1 mutations and deletions not present in matched blood samples. This is consistent with the hypothesis that the cells that are most vulnerable to sustaining SMARCB1 mutations or deletions decrease with age, leading to a lower incidence of tumors in older individuals. It is also interesting to note that isolated, sporadic schwannomas do not appear to be due to genomic alterations of either NF2 or SMARCB1 (reviewed by [86]). Notably, Voisin et al. [93] recently reported a sellar AT/RT in a 51-year-old mother from a three-generation family with SMARCB1-related brain tumors due to a splice site loss of function mutation in exon 7, confirming that lifelong surveillance will be required for carriers of mutations or inactivating copy number alterations in rhabdoid tumor cancer predisposition genes.
3.4 Molecular Subgrouping of AT/RT
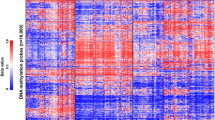
Although inactivation of SMARCB1 and to a lesser extent SMARCA4 is the hallmark of rhabdoid tumors, at least three molecular subgroups have been defined on the basis of gene expression and DNA methylation profiling of primary AT/RTs [94]. The ATRT-TYR subgroup is characterized by overexpression of the enzyme tyrosinase, and most tumors in this group can be distinguished by IHC to the protein [95]. ATRT-TYR tumors are also characterized by upregulation of the bone morphogenic protein (BMP) pathway, as well as PDGFRB, and OTX2. The tumors often demonstrate focal loss involving 22q11.2 in one copy of chromosome 22 and mutation of the remaining copy of SMARCB1; patients are less than 3 years of age at diagnosis; and tumors are most often located in infratentorial locations. Cribriform neuroectodermal tumors (CRINETs) demonstrate mutations in SMARCB1 [96,97,98] and have a similar expression profile to this group of AT/RTs. Patients with CRINET can achieve a response to combination therapeutic strategies and appear to have a somewhat improved prognosis compared to patients with AT/RT [96]. Clinical and molecular studies of additional patients with CRINET as well as the patients with ATRT-TYR will be required to substantiate these early predictions.
The ATRT-SHH subgroup demonstrates overexpression of sonic hedgehog (SHH) and notch pathway members, including GL12 and ASCL1, respectively. Most tumors have compound heterozygous mutations in SMARCB1 and fewer deletions in 22q11.2. Patients fall into an intermediate age group, with a median age of 20 months. Two subgroups of ATRT-SHH (ATRT-SHH-1 and ATRT-SHH-2) are distinguished by their supratentorial and infratentorial locations, respectively.
The ATRT-MYC subgroup was named based on the increased expression of the MYC oncogene, but without amplification of this locus, and overexpression of several HOXC gene clusters. The tumors often demonstrate homozygous deletions of SMARCB1 and fewer point mutations. The median age of patients in this subgroup is the highest of the three subgroups (median 27 months), but there is a broad range. Spinal cord AT/RTs, as well as other extra-cranial rhabdoid tumors, fall into the ATRT-MYC subgroup, although at least half of the AT/RTs are supratentorial in location.
Fruhwald et al. [10] reported that age less than 1 year and a non-TYR subgroup, as determined by DNA methylation profiling, are independent negative prognostic markers of overall survival for patients with AT/RT. Reddy et al. [9] demonstrated a trend for a worse outcome for patients with germline SMARCB1 mutations and age, but molecular subgroup was not a prognostic factor in the recently reported COG ACNS0333 randomized clinical trial. Establishing the prognostic significance of molecular subgroup in AT/RT will therefore require large cooperative group clinical trials in which classification according to molecular subgrouping is performed.
3.5 Loss of SMARCB1 Expression in Other Tumors
Although initial studies of childhood tumors suggested that SMARCB1 inactivation was specific for rhabdoid tumors [29, 30], we now know that a variety of other tumors also demonstrate loss of SMARCB1, either at the genomic or protein level [24]. These include peripheral tumors such as epithelioid sarcoma, malignant peripheral nerve sheath tumor, extraskeletal chondrosarcoma, myoepithelial carcinoma, and de-differentiated chordomas. The spectrum of tumors associated with germline mutations and deletions in SMARCB1 in the same individual or family is also expanding, which has made it challenging for pathologists to rely on SMARCB1 or SMARCA4 (Brg1) IHC analysis for the differential diagnosis of soft tissue tumors and CNS malignancies. Epithelioid sarcomas are typically associated with homozygous deletions of SMARCB1, and yet the frequency of mutations of the gene is extremely low [99, 100]. Neither of these findings can be used to distinguish epithelioid sarcoma from extra-renal rhabdoid tumor. Renal medullary carcinoma, often seen in patients with sickle cell disease, is characterized by loss of SMARCB1 expression by IHC [101], due to balanced chromosomal translocations that interrupt the SMARCB1 locus [49]. A small percentage of rare collecting duct carcinomas of the kidney may also demonstrate reduced or absent expression of SMARCB1 by IHC, although genomic studies have not yet been performed [102].
3.6 The SWI/SNF Complex and Cancer
SMARCB1 codes for a protein that is a component of the SWI/SNF chromatin-remodeling complex [27, 28]. This complex contains approximately 15 subunits, which requires either SMARCA4 (Brg1) or SMARCA2 (Brm) as the core ATPase for its function [28]. SMARCB1 is considered to be a necessary component of the SWI-SNF complex in all cell types; however the composition of the other subunits appears to depend on developmental state and organ system [27, 103,104,105,106]. It is likely that this variability contributes to the predilection for tumors to develop in the brain, kidney, and soft tissues and only extremely rarely in the hematopoietic system [107]. A variety of malignancies in both children and adults have now been described in association with mutations or deletions in almost all of the SWI/SNF members, including the loss of ARID1A in ovarian, breast, and endometrial cancers and SMARCA4 in lung tumors and medulloblastoma [108].
The mechanism by which loss of SMARCB1 drives cancer formation is an active area of research, yet early studies have already led to the development of several therapeutic approaches to reverse the epigenetic phenotype of rhabdoid tumors, including HDAC and EZH2 inhibitors [109]. Wang et al. [110] demonstrated that loss of SMARCB1 results in altered enhancer targeting by the SWI/NF complex, particularly at genes required for differentiation, while binding of the complex is retained at super-enhancers. Erkek et al. [111] demonstrated genome wide loss of both H3K27ac and H3K27me3 in SMARCB1-deficient AT/RT cell lines. The residual SWI/SNF complex (containing SMARCA4) and Polycomb complex (containing EZH2) were co-localized at active genes in AT/RTs, whereas the REST complex was postulated to impede SWI/SNF residual binding at repressed genes, notably neuronal differentiation genes. The interplay of both activating and repressive mechanisms of gene expression appears to restore tumor cells to a state that is similar to embryonic stem cells.
3.7 Genetic Counseling and Screening
Despite the fact that the genetic etiology for rhabdoid tumors has been known for more than 30 years, genetic counseling for individuals who are at risk for malignancy due to an associated SMARCB1 or SMARCA4 mutation is not a common practice outside of tertiary care centers, and surveillance guidelines are not firmly established. This is due in part to the fact that there have been few long-term survivors, and it is only recently that late second malignancies in patients treated in infancy have been reported in patients with predisposing germline mutations. Prenatal genetic counseling is further complicated by the recent reports of SWI/SNF mutations, notably ARID1A, ARID1B, SMARCA2, SMARCE1, and SMARCB1, in patients with genomic disorders such as Coffin-Siris syndrome (CSS) [112,113,114,115] or Nicolaides-Barrister syndrome (NBS) [116,117,118] who do not appear to be at an increased risk for cancer. Most patients with CSS and SMARCB1 alterations have heterozygous missense mutations, which are distinct from the typical nonsense mutations seen in patients with rhabdoid tumors or the splice site mutations often seen in familial schwannomatosis. Moertel et al. [119] reported one patient with CSS and a missense mutation in exon 9 who developed multiple schwannomas but not rhabdoid tumor. As whole-genome and whole-exome sequencing move into the arena of prenatal testing, the prediction of whether such mutations will result in a genomic disorder or increased risk for malignancy will become extremely challenging.
At the present time, any individual with a germline SMARCB1 deletion or mutation should be offered baseline ultrasound or magnetic resonance imaging (MRI) studies to rule out a brain or kidney tumor. The Children’s Oncology Group Rhabdoid Tumor Working group initially recommended monthly serial abdominal and trans-cranial ultrasonography and MRI performed every 3 months during the first year of life, with continued surveillance into the second and third year of life [120]. Rapid whole-body MRI in adult carriers of SMARCB1 mutations has successfully been utilized to identify schwannomas [121]. Current guidelines for screening patients with SMARCB1 and SMARCA4 alterations are based upon the high penetrance of SMARCB1 mutations and the high likelihood that a germline SMARCA4 mutation is inherited but with reduced penetrance [56, 122]. These include monthly physical examinations for the first year, baseline brain and spine MRI, and abdominal ultrasound, followed by brain, spine, and abdominal ultrasounds every 3 months for the first year. Nemes et al. [56] recommend brain and spine or whole-body MRI every 3 months until age 4 or 5 years for patients with AT/RT and abdominal or pelvic ultrasounds or whole-body MRI for patients with extra-cranial rhabdoid tumors. Patients should then be followed in a cancer surveillance clinic with twice yearly physical exams and targeting imaging. For patients with SMARCA4-related ovarian tumors, patients should have abdominal and pelvic ultrasounds every 6 months.
Unfortunately , given the rapid development and growth of malignant rhabdoid and related tumors, this may not be a sufficiently effective protocol for early detection and treatment. We are aware of at least two infants diagnosed prenatally with familial SMARCB1 mutations who developed AT/RT during the first year of life, despite clinical surveillance [43]. Furthermore, patients with germline alterations in SMARCB1 have developed second primary tumors as late as 15 years after successful treatment for a AT/RT [[123, 124], unpublished data].
Parents of probands should be counseled regarding the risk of recurrence in other children as well as potential family members who may be at risk. This should include counseling regarding gonadal mosaicism if the parents of a child with a germline mutation have negative test results from peripheral blood. Although the risk for gonadal mosaicism has not yet been determined, the theoretical risk for inheriting a mutation from a carrier of a SMARCB1 or SMARCA4 is 50%. Siblings and unaffected carriers should be offered the same type of surveillance described above, depending on their age.
SMARCB1 was the first tumor suppressor gene in the SWI/SNF chromatin-remodeling complex linked to the development of cancer. Although they are rare in the population, rhabdoid tumors are one of the most clinically aggressive malignancies in the brain, kidney, and soft tissues in children. Identification of SMARCB1 alterations as the initiating events in tumorigenesis have formed the basis for an entirely new field of cancer biology which has far-reaching implications for both constitutional genetic disorders and tumors associated with alterations in SWI/SNF function.
References
Tomlinson, G. E., Breslow, N. E., Dome, J., et al. (2005). Rhabdoid tumor of the kidney in the National Wilms' tumor study: Age at diagnosis as a prognostic factor. Journal of Clinical Oncology, 23, 7641–7645.
Rorke, L. B., Packer, R. J., & Biegel, J. A. (1996). Central nervous system atypical Teratoid/Rhabdoid tumors of infancy and childhood: Definition of an entity. Journal of Neurosurgery, 85, 56–65.
Hilden, J. M., Meerbaum, S., Burger, P., et al. (2004). Central nervous system atypical Teratoid/Rhabdoid tumor: Results of therapy in children enrolled in a registry. Journal of Clinical Oncology, 22, 2877–2884.
Tekautz, T. M., Fuller, C. E., Blaney, S., et al. (2005). Atypical Teratoid/Rhabdoid tumors (ATRT): Improved survival in children 3 years of age and older with radiation therapy and high-dose Alkylator-based chemotherapy. Journal of Clinical Oncology, 23, 1491–1499.
Geller, J. I., Roth, J. J., & Biegel, J. A. (2015). Biology and treatment of rhabdoid tumor. Critical Reviews in Oncogenesis, 20(3-4), 199–216. https://doi.org/10.1615/critrevoncog.2015013566
Walz, A. L., Fernandez, C. V., & Geller, J. I. (2019). Novel therapy for pediatric and adolescent kidney cancer. Cancer Metastasis Reviews, 38(4), 643–655. https://doi.org/10.1007/s10555-019-09822-4
Chi, S. N., Zimmerman, M. A., Yao, X., et al. (2009). Intensive multimodality treatment for children with newly diagnosed CNS atypical teratoid rhabdoid tumor. Journal of Clinical Oncology, 27, 385–389.
Frühwald, M. C., Biegel, J. A., Bourdeaut, F., et al. (2016). Atypical teratoid/rhabdoid tumors-current concepts, advances in biology, and potential future therapies. Neuro-Oncology, 18(6), 764–778. https://doi.org/10.1093/neuonc/nov264. [published correction appears in Neuro Oncol. 2016 Sep;18(9):1329].
Reddy, A. T., Strother, D. R., Judkins, A. R., et al. (2020). Efficacy of high-dose chemotherapy and three-dimensional conformal radiation for atypical teratoid/rhabdoid tumor: A report from the Children's Oncology Group Trial ACNS0333. Journal of Clinical Oncology, 38(11), 1175–1185. https://doi.org/10.1200/JCO.19.01776
Frühwald, M. C., Hasselblatt, M., Nemes, K., et al. (2020). Age and DNA methylation subgroup as potential independent risk factors for treatment stratification in children with atypical teratoid/rhabdoid tumors. Neuro-Oncology, 22(7), 1006–1017. https://doi.org/10.1093/neuonc/noz244
Hoffman, L. M., Richardson, E. A., Ho, B., et al. (2020). Advancing biology-based therapeutic approaches for atypical teratoid rhabdoid tumors. Neuro-Oncology, 22(7), 944–954. https://doi.org/10.1093/neuonc/noaa046
Wu, Y., Lun, X., Zhou, H., et al. (2008). Oncolytic efficacy of recombinant vesicular stomatitis virus and Myxoma virus in experimental models of rhabdoid tumors. Clinical Cancer Research, 14, 1218–1227.
Studebaker, A. W., Hutzen, B. J., Pierson, C. R., et al. (2017). Oncolytic herpes virus rRp450 shows efficacy in Orthotopic xenograft group 3/4 Medulloblastomas and atypical teratoid/rhabdoid tumors. Molecular Therapy Oncolytics, 6, 22–30. Published 2017 May 25. https://doi.org/10.1016/j.omto.2017.05.005
Choi, J., Rui, Y., Kim, J., et al. (2020). Nonviral polymeric nanoparticles for gene therapy in pediatric CNS malignancies. Nanomedicine, 23, 102115. https://doi.org/10.1016/j.nano.2019.102115
Beckwith, J. B., & Palmer, N. F. (1978). Histopathology and prognosis of Wilms tumors: Results from the first National Wilms' Tumor Study. Cancer, 41, 1937–1948.
Biggs, P. J., Garen, P. D., Powers, J. M., et al. (1987). Malignant rhabdoid tumor of the central nervous system. Human Pathology, 18, 332–337.
Sotelo-Avila, C., Gonzalez-Crussi, F., deMello, D., et al. (1986). Renal and extrarenal rhabdoid tumors in children: A clinicopathologic study of 14 patients. Seminars in Diagnostic Pathology, 3, 151–163.
Bonnin, J. M., Rubinstein, L. J., Palmer, N. F., et al. (1984). The association of embryonal tumors originating in the kidney and in the brain. A Report of Seven Cases. Cancer, 54, 2137–2146.
Weeks, D. A., Beckwith, J. B., Mierau, G. W., et al. (1989). Rhabdoid tumor of kidney. A report of 111 cases from the National Wilms' Tumor Study Pathology Center. The American Journal of Surgical Pathology, 13, 439–458.
Terada, Y., Jo, N., Arakawa, Y., et al. (2019). Human pluripotent stem cell-derived tumor model uncovers the embryonic stem cell signature as a key driver in atypical teratoid/rhabdoid tumor. Cell Reports, 26(10), 2608–2621.e6. https://doi.org/10.1016/j.celrep.2019.02.009
Han, Z. Y., Richer, W., Fréneaux, P., et al. (2016). The occurrence of intracranial rhabdoid tumours in mice depends on temporal control of Smarcb1 inactivation. Nature Communications, 7, 10421. Published 2016 Jan 28. https://doi.org/10.1038/ncomms10421
Vitte, J., Gao, F., Coppola, G., Judkins, A. R., & Giovannini, M. (2017). Timing of Smarcb1 and Nf2 inactivation determines schwannoma versus rhabdoid tumor development. Nature Communications, 8(1), 300. Published 2017 Aug 21. https://doi.org/10.1038/s41467-017-00346-5
Parham, D. M., Weeks, D. A., & Beckwith, J. B. (1994). The clinicopathologic spectrum of putative extrarenal rhabdoid tumors. An analysis of 42 cases studied with immunohistochemistry or electron microscopy. The American Journal of Surgical Pathology, 18, 1010–1029.
Pawel, B. R. (2018). SMARCB1-deficient tumors of childhood: A practical guide. Pediatric and Developmental Pathology, 21(1), 6–28. https://doi.org/10.1177/1093526617749671
Versteege, I., Sevenet, N., Lange, J., et al. (1998). Truncating mutations of hSNF5/INI1 in aggressive paediatric cancer. Nature, 394, 203–206.
Biegel, J. A., Zhou, J. Y., Rorke, L. B., et al. (1999). Germ-line and acquired mutations of INI1 in atypical teratoid and rhabdoid tumors. Cancer Research, 59, 74–79.
Phelan, M. L., Sif, S., Narlikar, G. J., et al. (1999). Reconstitution of a core chromatin remodeling complex from SWI/SNF subunits. Molecular Cell, 3, 247–253.
Wang, W., Xue, Y., Zhou, S., et al. (1996). Diversity and specialization of mammalian SWI/SNF complexes. Genes & Development, 10, 2117–2130.
Judkins, A. R., Mauger, J., Ht, A., et al. (2004). Immunohistochemical analysis of hSNF5/INI1 in Pediatric CNS neoplasms. The American Journal of Surgical Pathology, 28, 644–650.
Hoot, A. C., Russo, P., Judkins, A. R., et al. (2004). Immunohistochemical analysis of hSNF5/INI1 distinguishes renal and extra-renal malignant rhabdoid tumors from other pediatric soft tissue tumors. The American Journal of Surgical Pathology, 28, 1485–1491.
Allen, J. C., Judkins, A. R., Rosenblum, M. K., et al. (2006). Atypical teratoid/rhabdoid tumor evolving from an optic pathway ganglioglioma: Case study. Neuro-Oncology, 8, 79–82.
Chacko, G., Chacko, A. G., Dunham, C. P., et al. (2007). Atypical teratoid/rhabdoid tumor arising in the setting of a pleomorphic xanthoastrocytoma. Journal of Neuro-Oncology, 84, 217–222.
Carter, J. M., O'Hara, C., Dundas, G., et al. (2012). Epithelioid malignant peripheral nerve sheath tumor arising in a schwannoma, in a patient with "neuroblastoma-like" Schwannomatosis and a novel germline SMARCB1 mutation. The American Journal of Surgical Pathology, 36, 154–160.
Rizzo, D., Freneaux, P., Brisse, H., et al. (2012). SMARCB1 deficiency in tumors from the peripheral nervous system: A link between schwannomas and rhabdoid tumors? The American Journal of Surgical Pathology, 36, 964–972.
Hasselblatt, M., Gesk, S., Oyen, F., et al. (2011). Nonsense mutation and inactivation of SMARCA4 (BRG1) in an atypical teratoid/rhabdoid tumor showing retained SMARCB1 (INI1) expression. The American Journal of Surgical Pathology, 35, 933–935.
Schneppenheim, R., Fruhwald, M. C., Gesk, S., et al. (2010). Germline nonsense mutation and somatic inactivation of SMARCA4/BRG1 in a family with rhabdoid tumor predisposition syndrome. American Journal of Human Genetics, 86, 279–284.
Ramos, P., Karnezis, A. N., Craig, D. W., et al. (2014). Small cell carcinoma of the ovary, hypercalcemic type, displays frequent inactivating germline and somatic mutations in SMARCA4. Nature Genetics, 46(5), 427–429. https://doi.org/10.1038/ng.2928
Witkowski, L., Carrot-Zhang, J., Albrecht, S., et al. (2014). Germline and somatic SMARCA4 mutations characterize small cell carcinoma of the ovary, hypercalcemic type. Nature Genetics, 46(5), 438–443. https://doi.org/10.1038/ng.2931
Jackson, E. M., Shaikh, T. H., Gururangan, S., et al. (2007). High-density single nucleotide polymorphism array analysis in patients with germline deletions of 22q11.2 and malignant rhabdoid tumor. Human Genetics, 122, 117–127.
Plon, S. E., Wheeler, D. A., Strong, L. C., et al. (2011). Identification of genetic susceptibility to childhood cancer through analysis of genes in parallel. Cancer Genetics, 204, 19–25.
Lee, R. S., Stewart, C., Carter, S. L., et al. (2012). A remarkably simple genome underlies highly malignant pediatric rhabdoid cancers. The Journal of Clinical Investigation, 122, 2983–2988.
Jackson, E. M., Sievert, A. J., Gai, X., et al. (2009). Genomic analysis using high-density single nucleotide polymorphism-based oligonucleotide arrays and multiplex ligation-dependent probe amplification provides a comprehensive analysis of INI1/SMARCB1 in malignant rhabdoid tumors. Clinical Cancer Research, 15, 1923–1930.
Bourdeaut, F., Lequin, D., Brugieres, L., et al. (2011). Frequent hSNF5/INI1 germline mutations in patients with Rhabdoid tumor. Clinical Cancer Research, 17, 31–38.
Eaton, K. W., Tooke, L. S., Wainwright, L. M., et al. (2011). Spectrum of SMARCB1/INI1 mutations in familial and sporadic rhabdoid tumors. Pediatric Blood & Cancer, 56, 7–15.
Lawrence, M. S., Stojanov, P., Polak, P., et al. (2013). Mutational heterogeneity in cancer and the search for new cancer-associated genes. Nature, 499, 214–218.
Isakoff, M. S., Sansam, C. G., Tamayo, P., et al. (2005). Inactivation of the Snf5 tumor suppressor stimulates cell cycle progression and cooperates with p53 loss in oncogenic transformation. Proceedings of the National Academy of Sciences of the United States of America, 102, 17745–17750.
Chai, J., Lu, X., Godfrey, V., et al. (2007). Tumor-specific cooperation of retinoblastoma protein family and Snf5 inactivation. Cancer Research, 67, 3002–3009.
Kieran, M. W., Roberts, C. W., Chi, S. N., et al. (2012). Absence of oncogenic canonical pathway mutations in aggressive pediatric rhabdoid tumors. Pediatric Blood & Cancer, 59, 1155–1157.
Calderaro, J., Masliah-Planchon, J., Richer, W., et al. (2016). Balanced translocations disrupting SMARCB1 are hallmark recurrent genetic alterations in renal medullary carcinomas. European Urology, 69(6), 1055–1061. https://doi.org/10.1016/j.eururo.2015.09.027
Tauziède-Espariat, A., Masliah-Planchon, J., Brugières, L., et al. (2017). Deep intronic hotspot variant explaining rhabdoid tumor predisposition syndrome in two patients with atypical teratoid and rhabdoid tumor. European Journal of Human Genetics, 25(10), 1170–1172. https://doi.org/10.1038/ejhg.2017.115
Lynch, H. T., Shurin, S. B., Dahms, B. B., et al. (1983). Paravertebral malignant rhabdoid tumor in infancy. In vitro studies of a familial tumor. Cancer, 52, 290–296.
Taylor, M. D., Gokgoz, N., Andrulis, I. L., et al. (2000). Familial posterior fossa brain Tumors of infancy secondary to germline mutation of the hSNF5 gene. American Journal of Human Genetics, 66, 1403–1406.
Sevenet, N., Sheridan, E., Amram, D., et al. (1999). Constitutional mutations of the hSNF5/INI1 gene predispose to a variety of cancers. American Journal of Human Genetics, 65, 1342–1348.
Janson, K., Nedzi, L. A., David, O., et al. (2006). Predisposition to atypical teratoid/rhabdoid tumor due to an inherited INI1 mutation. Pediatric Blood & Cancer, 47, 279–284.
Bruggers, C. S., Bleyl, S. B., Pysher, T., et al. (2011). Clinicopathologic comparison of familial versus sporadic atypical teratoid/rhabdoid tumors (AT/RT) of the central nervous system. Pediatric Blood & Cancer, 56, 1026–1031.
Nemes, K., Bens, S., Bourdeaut, F., et al. (2017). Rhabdoid tumor predisposition syndrome. In M. P. Adam, H. H. Ardinger, R. A. Pagon, et al. (Eds.), GeneReviews®. University of Washington, Seattle.
Pinto, E. M., Hamideh, D., Bahrami, A., et al. (2018). Malignant rhabdoid tumors originating within and outside the central nervous system are clinically and molecularly heterogeneous. Acta Neuropathologica, 136(2), 315–326. https://doi.org/10.1007/s00401-018-1814-2
Holsten, T., Bens, S., Oyen, F., et al. (2018). Germline variants in SMARCB1 and other members of the BAF chromatin-remodeling complex across human disease entities: A meta-analysis. European Journal of Human Genetics, 26(8), 1083–1093. https://doi.org/10.1038/s41431-018-0143-1
Emanuel, B. S., McDonald-McGinn, D., Saitta, S. C., et al. (2001). The 22q11.2 deletion syndrome. Adv Pediatr, 48, 39–73.
Shaikh, T. H., Kurahashi, H., & Emanuel, B. S. (2001). Evolutionarily conserved low copy repeats (LCRs) in 22q11 mediate deletions, duplications, translocations, and genomic instability: An update and literature review. Genetics in Medicine, 3, 6–13.
Shaikh, T. H., Kurahashi, H., Saitta, S. C., et al. (2000). Chromosome 22-specific low copy repeats and the 22q11.2 deletion syndrome: Genomic organization and deletion endpoint analysis. Human Molecular Genetics, 9, 489–501.
Mikhail, F. M., Burnside, R. D., Rush, B., et al. (2013). The recurrent distal 22q11.2 microdeletions are often De novo and do not represent a single clinical entity: A proposed categorization system. Genetics in Medicine, 16, 92.
Rauch, A., Pfeiffer, R. A., Leipold, G., et al. (1999). A novel 22q11.2 microdeletion in DiGeorge syndrome. American Journal of Human Genetics, 64, 659–666.
Saitta, S. C., McGrath, J. M., Mensch, H., et al. (1999). A 22q11.2 deletion that excludes UFD1L and CDC45L in a patient with conotruncal and craniofacial defects. American Journal of Human Genetics, 65, 562–566.
Mikhail, F. M., Descartes, M., Piotrowski, A., et al. (2007). A previously unrecognized microdeletion syndrome on chromosome 22 band q11.2 encompassing the BCR gene. American Journal of Medical Genetics. Part A, 143A, 2178–2184.
Ben-Shachar, S., Ou, Z., Shaw, C. A., et al. (2008). 22q11.2 distal deletion: A recurrent genomic disorder distinct from DiGeorge syndrome and Velocardiofacial syndrome. American Journal of Human Genetics, 82, 214–221.
Lafay-Cousin, L., Payne, E., Strother, D., et al. (2009). Goldenhar phenotype in a child with distal 22q11.2 deletion and intracranial atypical teratoid rhabdoid tumor. American Journal of Medical Genetics. Part A, 149A, 2855–2859.
Beddow, R. A., Smith, M., Kidd, A., et al. (2011). Diagnosis of distal 22q11.2 deletion syndrome in a patient with a teratoid/rhabdoid tumour. European Journal of Medical Genetics, 54, 295–298.
Toth, G., Zraly, C. B., Thomson, T. L., et al. (2011). Congenital anomalies and rhabdoid tumor associated with 22q11 germline deletion and somatic inactivation of the SMARCB1 tumor suppressor. Genes, Chromosomes & Cancer, 50, 379–388.
Chakrapani, A. L., White, C. R., Korcheva, V., et al. (2012). Congenital extrarenal malignant rhabdoid tumor in an infant with distal 22q11.2 deletion syndrome: The importance of SMARCB1. The American Journal of Dermatopathology, 34, e77–e80.
Wieser, R., Fritz, B., Ullmann, R., et al. (2005). Novel rearrangement of chromosome band 22q11.2 causing 22q11 microdeletion syndrome-like phenotype and rhabdoid tumor of the kidney. Human Mutation, 26, 78–83.
Miller, D. T., Adam, M. P., Aradhya, S., et al. (2010). Consensus statement: Chromosomal microarray is a first-tier clinical diagnostic test for individuals with developmental disabilities or congenital anomalies. American Journal of Human Genetics, 86, 749–764.
Rubio, A. (1997). March 1997—4 year old girl with ring chromosome 22 and brain tumor. Brain Pathology, 7, 1027–1028.
Sathyamoorthi, S., Morales, J., Bermudez, J., et al. (2009). Array analysis and molecular studies of INI1 in an infant with deletion 22q13 (Phelan-McDermid syndrome) and atypical teratoid/rhabdoid tumor. American Journal of Medical Genetics. Part A, 149A, 1067–1069.
Lindblom, A., Sandelin, K., Iselius, L., et al. (1994). Predisposition for breast cancer in carriers of constitutional translocation 11q;22q. American Journal of Human Genetics, 54, 871–876.
Doyen, J., Carpentier, X., Haudebourg, J., et al. (2012). Renal cell carcinoma and a constitutional T(11;22)(q23;q11.2): Case report and review of the potential link between the constitutional T(11;22) and cancer. Cancer Genetics, 205, 603–607.
Jackson, E. M., Shaikh, T. H., Zhang, F., et al. (2007). Atypical teratoid/rhabdoid tumor in a patient with Beckwith-Wiedemann syndrome. American Journal of Medical Genetics. Part A, 143A, 1767–1770.
El Kababri, M., Andre, N., Carole, C., et al. (2006). Atypical teratoid rhabdoid tumor in a child with neurofibromatosis 1. Pediatric Blood & Cancer, 46, 267–268.
Krous, H. F., Chadwick, A. E., Haas, E. A., et al. (2007). Congenital cerebellar malignant rhabdoid tumor in an infant with junctional epidermolysis bullosa. Pediatric and Developmental Pathology, 10, 481–486.
Modena, P., Sardi, I., Brenca, M., et al. (2013). Case report: Long-term survival of an infant syndromic patient affected by atypical teratoid-rhabdoid tumor. BMC Cancer, 13, 100-2407-13-100.
Heck, J. E., Wu, J., Lombardi, C., et al. (2013). Childhood cancer and traffic-related air pollution exposure in pregnancy and early life. Environmental Health Perspectives, 121, 1385.
Nicolaides, T., Tihan, T., Horn, B., et al. (2010). High-dose chemotherapy and autologous stem cell rescue for atypical teratoid/rhabdoid tumor of the central nervous system. Journal of Neuro-Oncology, 98, 117–123.
Cecen, E., Gunes, D., Uysal, K. M., et al. (2010). Atypical teratoid/rhabdoid tumor in an infant conceived by in vitro fertilization. Child's Nervous System, 26, 263–266.
Kallen, B., Finnstrom, O., Lindam, A., et al. (2010). Cancer risk in children and young adults conceived by in vitro fertilization. Pediatrics, 126, 270–276.
Lerner-Geva, L., Toren, A., Chetrit, A., et al. (2000). The risk for cancer among children of women who underwent in vitro fertilization. Cancer, 88, 2845–2847.
Plotkin, S. R., Blakeley, J. O., Evans, D. G., et al. (2013). Update from the 2011 international Schwannomatosis workshop: From genetics to diagnostic criteria. American Journal of Medical Genetics. Part A, 161A, 405–416.
MacCollin, M., Willett, C., Heinrich, B., et al. (2003). Familial Schwannomatosis: Exclusion of the NF2 locus as the germline event. Neurology, 60, 1968–1974.
Boyd, C., Smith, M. J., Kluwe, L., et al. (2008). Alterations in the SMARCB1 (INI1) tumor suppressor gene in familial Schwannomatosis. Clinical Genetics, 74, 358–366.
Hadfield, K. D., Newman, W. G., Bowers, N. L., et al. (2008). Molecular characterisation of SMARCB1 and NF2 in familial and sporadic Schwannomatosis. Journal of Medical Genetics, 45, 332–339.
Hulsebos, T. J., Plomp, A. S., Wolterman, R. A., et al. (2007). Germline mutation of INI1/SMARCB1 in familial Schwannomatosis. American Journal of Human Genetics, 80, 805–810.
Swensen, J. J., Keyser, J., Coffin, C. M., et al. (2009). Familial occurrence of schwannomas and malignant rhabdoid tumour associated with a duplication in SMARCB1. Journal of Medical Genetics, 46, 68–72.
Raisanen, J., Biegel, J. A., Hatanpaa, K. J., et al. (2005). Chromosome 22q deletions in atypical teratoid/rhabdoid tumors in adults. Brain Pathology, 15, 23–28.
Voisin, M. R., Ovenden, C., Tsang, D. S., et al. (2019). Atypical teratoid/rhabdoid sellar tumor in an adult with a familial history of a germline SMARCB1 mutation: Case report and review of the literature. World Neurosurgery, 127, 336–345. https://doi.org/10.1016/j.wneu.2019.04.083
Ho, B., Johann, P. D., Grabovska, Y., et al. (2020). Molecular subgrouping of atypical teratoid/rhabdoid tumors-a reinvestigation and current consensus. Neuro-Oncology, 22(5), 613–624. https://doi.org/10.1093/neuonc/noz235
Hasselblatt, M., Thomas, C., Nemes, K., et al. (2020). Tyrosinase immunohistochemistry can be employed for the diagnosis of atypical teratoid/rhabdoid tumours of the tyrosinase subgroup (ATRT-TYR). Neuropathology and Applied Neurobiology, 46(2), 186–189. https://doi.org/10.1111/nan.12560
Hasselblatt, M., Oyen, F., Gesk, S., et al. (2009). Cribriform neuroepithelial tumor (CRINET): A nonrhabdoid ventricular tumor with INI1 loss and relatively favorable prognosis. Journal of Neuropathology and Experimental Neurology, 68, 1249–1255.
Ibrahim, G. M., Huang, A., Halliday, W., et al. (2011). Cribriform neuroepithelial tumour: Novel clinicopathological, ultrastructural and cytogenetic findings. Acta Neuropathologica, 122, 511–514.
Arnold, M. A., Stallings-Archer, K., Marlin, E., et al. (2013). Cribriform neuroepithelial tumor arising in the lateral ventricle. Pediatric and Developmental Pathology, 16, 301–307.
Gasparini, P., Facchinetti, F., Boeri, M., et al. (2011). Prognostic determinants in epithelioid sarcoma. European Journal of Cancer, 47, 287–295.
Sullivan, L. M., Folpe, A. L., Pawel, B. R., et al. (2013). Epithelioid sarcoma is associated with a high percentage of SMARCB1 deletions. Modern Pathology, 26, 385–392.
Cheng, J. X., Tretiakova, M., Gong, C., et al. (2008). Renal medullary carcinoma: Rhabdoid features and the absence of INI1 expression as markers of aggressive behavior. Modern Pathology, 21, 647–652.
Elwood, H., Chaux, A., Schultz, L., et al. (2011). Immunohistochemical analysis of SMARCB1/INI-1 expression in collecting duct carcinoma. Urology, 78, 474.e1–474.e5.
Kaeser, M. D., Aslanian, A., Dong, M. Q., et al. (2008). BRD7, a novel PBAF-specific SWI/SNF subunit, is required for target gene activation and repression in embryonic stem cells. The Journal of Biological Chemistry, 283, 32254–32263.
Olave, I., Wang, W., Xue, Y., et al. (2002). Identification of a polymorphic, neuron-specific chromatin remodeling complex. Genes & Development, 16, 2509–2517.
Wang, W., Cote, J., Xue, Y., et al. (1996). Purification and biochemical heterogeneity of the mammalian SWI-SNF complex. The EMBO Journal, 15, 5370–5382.
Panwalkar, P., Pratt, D., Chung, C., et al. (2020). SWI/SNF complex heterogeneity is related to polyphenotypic differentiation, prognosis, and immune response in rhabdoid tumors. Neuro-Oncology, 22(6), 785–796. https://doi.org/10.1093/neuonc/noaa004
Metts, J. L., Park, S. I., Soares, B. P., Fong, C., Biegel, J. A., & Goldsmith, K. C. (2017). Concurrent myeloid sarcoma, atypical teratoid/rhabdoid tumor, and hypereosinophilia in an infant with a germline SMARCB1 mutation. Pediatric Blood & Cancer, 64, 9. https://doi.org/10.1002/pbc.26460
Biegel, J. A., Busse, T. M., & Weissman, B. E. (2014). SWI/SNF chromatin remodeling complexes and cancer. American Journal of Medical Genetics. Part C, Seminars in Medical Genetics, 166C(3), 350–366. https://doi.org/10.1002/ajmg.c.31410
Knutson, S. K., Warholic, N. M., Wigle, T. J., et al. (2013). Durable tumor regression in genetically altered malignant rhabdoid tumors by inhibition of methyltransferase EZH2. Proceedings of the National Academy of Sciences of the United States of America, 110, 7922–7927.
Wang, X., Lee, R. S., Alver, B. H., et al. (2017). SMARCB1-mediated SWI/SNF complex function is essential for enhancer regulation. Nature Genetics, 49(2), 289–295. https://doi.org/10.1038/ng.3746
Erkek, S., Johann, P. D., Finetti, M. A., et al. (2019). Comprehensive analysis of chromatin states in atypical teratoid/rhabdoid tumor identifies diverging roles for SWI/SNF and Polycomb in gene regulation. Cancer Cell, 35(1), 95–110.e8. https://doi.org/10.1016/j.ccell.2018.11.014
Santen, G. W., Aten, E., Sun, Y., et al. (2012). Mutations in SWI/SNF chromatin remodeling complex gene ARID1B cause Coffin-Siris syndrome. Nature Genetics, 44, 379–380.
Santen, G. W., Aten, E., Vulto-van Silfhout, A. T., et al. (2013). Coffin-Siris syndrome and the BAF complex: Genotype-phenotype study in 63 patients. Human Mutation, 34, 1519.
Tsurusaki, Y., Okamoto, N., Ohashi, H., et al. (2013). Coffin-Siris syndrome is a SWI/SNF complex disorder. Clinical Genetics, 85, 548.
Tsurusaki, Y., Okamoto, N., Ohashi, H., et al. (2012). Mutations affecting components of the SWI/SNF complex cause Coffin-Siris syndrome. Nature Genetics, 44, 376–378.
Wieczorek, D., Bogershausen, N., Beleggia, F., et al. (2013). A comprehensive molecular study on Coffin-Siris and Nicolaides-Baraitser syndromes identifies a broad molecular and clinical spectrum converging on altered chromatin remodeling. Human Molecular Genetics, 22, 5121.
Wolff, D., Endele, S., Azzarello-Burri, S., et al. (2012). In-frame deletion and missense mutations of the C-terminal helicase domain of SMARCA2 in three patients with Nicolaides-Baraitser syndrome. Molecular Syndromology, 2, 237–244.
Van Houdt, J. K., Nowakowska, B. A., Sousa, S. B., et al. (2012). Heterozygous missense mutations in SMARCA2 cause Nicolaides-Baraitser syndrome. Nature Genetics, 44, 445–449. S1.
Moertel, C. L., Biegel, J. A., Dahlheime, T. R. et al. (2009). Report of a Patient with Constitutional Missense Mutation of INI1/SMARCB1, Coffin-Siris Phenotype and Schwannomatosis. Poster Presented at the Children's Tumor Foundation NF Conference, Portland Oregon, 3-6 June 2009.
Geller, J. I., Leslie, N. D., Yin, H. (2012). Malignant rhabdoid tumor. http://emedicine.medscape.com/article/99308. Accessed 1 October 2013.
Plotkin, S. R., Bredella, M. A., Cai, W., et al. (2012). Quantitative assessment of whole-body tumor burden in adult patients with Neurofibromatosis. PLoS One, 7, e35711.
Foulkes, W. D., Kamihara, J., Evans, D. G. R., et al. (2017). Cancer surveillance in Gorlin syndrome and Rhabdoid tumor predisposition syndrome. Clinical Cancer Research, 23(12), e62–e67. https://doi.org/10.1158/1078-0432.CCR-17-0595
Forest, F., David, A., Arrufat, S., et al. (2012). Conventional chondrosarcoma in a survivor of rhabdoid tumor: Enlarging the spectrum of tumors associated with SMARCB1 germline mutations. The American Journal of Surgical Pathology, 36, 1892–1896.
Bhatt, M. D., Al-Karmi, S., Druker, H., et al. (2019). Second rhabdoid tumor 8 years after treatment of atypical teratoid/rhabdoid tumor in a child with germline SMARCB1 mutation. Pediatric Blood & Cancer, 66(3), e27546. https://doi.org/10.1002/pbc.27546
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2021 The Editor(s) (if applicable) and The Author(s) under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Biegel, J.A., Roth, J.J. (2021). Rhabdoid Tumors. In: Malkin, D. (eds) The Hereditary Basis of Childhood Cancer. Springer, Cham. https://doi.org/10.1007/978-3-030-74448-9_3
Download citation
DOI: https://doi.org/10.1007/978-3-030-74448-9_3
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-74446-5
Online ISBN: 978-3-030-74448-9
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)