Abstract
Primary sclerosing cholangitis (PSC) is a chronic inflammatory liver disease, of unknown etiology, targeting cholangiocytes in any portion of the biliary system. Cholangiocarcinoma (CCA) is a feared complication of PSC, with a lifetime risk of 7–14%, no matter the duration of underlying PSC. Since a prominent fibrotic reaction closely abutting the bile ducts is a common trait of both PSC and CCA, PSC may be regarded as paradigmatic of the pathogenetic sequence leading from chronic inflammatory epithelial damage to malignant transformation. The risk of CCA is a major challenge in the management of PSC, raising several questions about disease surveillance, early tumor detection, prevention, and treatment. Herein, we discuss the critical issues of PSC-associated CCA, highlighting the need for a multimodal approach where recent advances in imaging studies, endoscopic procedures, and novel tumoral biomarkers are emphasized.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Cholangiocyte
- Bile ducts
- Dominant strictures
- Cholestasis
- Biliary fibrosis
- Biliary dysplasia
- Tumor reactive stroma
- Endoscopic retrograde cholangiopancreatography
- Magnetic resonance cholangiopancreatography
Primary Sclerosing Cholangitis: Background and Risk of Malignancies
Primary sclerosing cholangitis (PSC) is a chronic liver disease of unknown etiology but likely sustained by immune-mediated mechanisms, featuring ductopenic bile duct injury, cholestasis, peribiliary fibrosis, and associated multifocal strictures alternating with segmental ductal ectasia [1, 2]. Since PSC can target any segment of the biliary tree, including either the intrahepatic or the extrahepatic portions, PSC is currently divided into three main variants (or subtypes) according to the level and extent of biliary involvement (Table 10.1): classic PSC, small-duct PSC, and autoimmune hepatitis (AIH)-associated PSC.
A unique feature of PSC is its strong association with inflammatory bowel disease (IBD), with chronic ulcerative colitis (UC) comprising nearly 75–80% of these cases, while Crohn’s disease (CD) and indeterminate colitis comprise approximately 10–15% and 5–10%, respectively [3]. Although the clinical course of the disease is quite heterogeneous, most patients progress to end-stage liver disease and require liver transplantation (LT) [4]. Currently, PSC is still regarded as an “orphan” disease, given the lack of effective therapies in hindering disease progression. Though LT has significantly improved long-term survival of PSC patients with end-stage liver disease, up to 40–50% of deaths remain cancer-related and make PSC a bona fide premalignant condition [5]. Among cancers associated with PSC, cholangiocarcinoma (CCA) is the most diagnosed and lethal tumor, but PSC patients can also develop colorectal (especially when PSC is associated with UC) and gallbladder cancer [6]. Unlike other chronic liver diseases, the risk of hepatocellular carcinoma (HCC) is quite low, and it seems to be related to the progression to cirrhosis [7, 8].
Among the three anatomical subtypes of CCA, the one most commonly diagnosed in PSC patients is the perihilar form (pCCA ), as generally observed in CCA patients even in the absence of a PSC background. Morphologically, CCA frequently presents as an obstructive biliary stricture without evidence of a mass on cross-sectional imaging [9]. There are some important distinctive features of PSC-associated CCA. In PSC patients, the lifetime risk of CCA development is 7–14% (corresponding to a 400- to 1500-fold increase in respect to the general population), with a 10-year cumulative incidence of 7–9% according to multiple studies [10,11,12]. Interestingly, CCA development is not related to the duration of the disease, in contrast with what is generally observed with other primary liver malignancies, HCC in particular, commonly arising in a cirrhotic setting [6]. Of note, one third of the CCAs detected in PSC is diagnosed within the first year from the PSC diagnosis, thus suggesting that a long-standing disease becomes symptomatic because of the tumor [13]. Moreover, since PSC strikes young individuals, in their third to fifth decade, PSC-associated CCA develops about 20 years earlier than in CCA patients without PSC [8].
PSC-related factors predisposing to CCA are still largely unknown. A recent study indicates duration and severity of PSC, age at diagnosis, smoking, alcohol consumption, or a history of colorectal dysplasia as factors bearing an increased CCA risk [5]. On the other hand, small-duct PSC and pediatric patients have a low risk of CCA development [6, 14]. As aforementioned, PSC patients also have a lifetime risk of gallbladder cancer ranging from 3 to 14%, whereas patients with PSC and UC have a fourfold increased risk of colorectal cancer when compared to patients with UC alone. Among other epithelial cancers, the risk of developing HCC is also slightly increased, ranging from 0.3 to 2.8% [5].
Pathogenesis of PSC-Associated CCA: The Archetype of a Premalignant Condition Sustained by Fibroinflammatory Lesions
The pathogenesis of PSC involves both environmental and inherited factors, with a yet unidentified environmental trigger probably activating a persistent cholangiocyte injury in genetically predisposed individuals. This injury is associated with a pronounced accumulation of fibrotic tissue, which prevails on the inflammatory infiltrate, with the development of the typical “onion skin-like” lesions, the hallmark of the disease [1, 4]. These lesions are made up of activated fibroblasts and macrophages and by a concentric peribiliary deposition of new extracellular matrix (ECM) components, in particular collagen type I and fibronectin, which induce progressive narrowing of the damaged bile ducts, eventually resulting in ductopenia [4, 15]. Moreover, ECM components, by binding soluble mediators (growth factors, chemokines, cytokines) via low-affinity non-covalent interactions, create gradients that further stimulate recruitment of fibroblasts and inflammatory cells to the damaged ducts leading to cholangiocyte proliferation and neoangiogenesis [16].
Remarkably, in CCA, neoplastic bile ducts are embedded in a dense desmoplastic tissue populated by myofibroblasts (cancer-associated fibroblasts) and macrophages (tumor-associated macrophages), together with a variety of innate and adaptive immune cells, encompassing T lymphocytes, macrophages, and neutrophils, which reproduces the prominent fibroinflammatory reaction featuring PSC [17,18,19] (Fig. 10.1). This observation lends support to the concept that PSC is paradigmatic of the pathogenetic sequence from fibroinflammation to cancer, driven by a proficient microenvironment characterized by qualitative and quantitative changes in ECM components associated with a dense myofibroblast gathering (Fig. 10.2). Moreover, either pro-inflammatory mediators released in the periductal milieu or cholestasis cooperates with the inciting effects of the fibrotic stroma. IL-6, nitric oxide (NO), and reactive nitrogen and oxygen species induce DNA damage and promote epithelial cell proliferation while inhibiting apoptosis. TNF-α is also involved in the upregulation of inducible NO synthase.
Primary sclerosing cholangitis (a, c) and cholangiocarcinoma (b, d) share an exuberant fibrotic reaction embedding the bile ducts (a, b, Masson’s trichrome), densely populated by activated myofibroblasts laying closely adjacent to cholangiocytes (c, d, immunohistochemistry for alpha-smooth muscle actin). Magnification a, b, 100×; c, 200×; d, 400×
In primary sclerosing cholangitis (PSC), the histopathological sequence from fibroinflammation to biliary dysplasia and cancer (cholangiocarcinoma, CCA) is faithfully reproduced. The peribiliary microenvironment behaves as the main director of this sequence, sustained by ECM changes and prominent myofibroblast accumulation. Up-sided micrographs are derived from human liver biopsies immunostained by the biliary marker keratin-7. Magnification, 100×
Once cholangiocytes have gained a malignant phenotype, they release further growth factors, cytokines and chemokines acting as a feed-forward loop that potentiate CCA invasiveness [6]. The tumor necrosis factor-related apoptosis-inducing ligand (TRAIL), a pro-apoptotic death receptor agonist, might also be involved in the sequence PSC-CCA by activating a sublethal pro-apoptotic signaling that induces chromosomal instability [20]. Furthermore, cholestasis that may exert several effects on malignant transformation of the biliary epithelium has been shown, as related to the activation of receptor tyrosine kinases, such as the epidermal growth factor receptor leading to cell proliferation, and of cyclooxygenase-2 (COX-2), which, beyond promoting proliferation, stimulates angiogenesis and inhibits apoptosis [21, 22]. Of note, development of an abundant stromal reaction nearby the tumoral ducts (so-called tumor reactive stroma) is a common trait in many epithelial malignancies with pronounced invasive properties, including, beyond CCA, pancreatic ductal adenocarcinoma and invasive ductal breast carcinoma among others, where it provides a scaffold sustaining tumor cell dissemination [23]. However, the mechanisms underpinning the progressive course that culminate in cancer from fibrosis through dysplasia are largely uncharted, given the lack of experimental conditions able to model the PSC-CCA progression. Thus, the development of an animal model recapitulating this pathogenetic sequence is eagerly awaited, as a valuable tool to capture the pathways promoting biliary carcinogenesis and, possibly, to identify putative biomarkers detecting tumor onset in the earliest stages.
Clinical Presentation of PSC-Associated CCA: The Confounding Presence of Dominant Strictures
Early CCA diagnosis can be extremely challenging, as its clinical presentation is generally insidious. The diagnostic difficulty in detecting potential CCA is particularly true in patients with PSC. In fact, symptoms of PSC (fatigue, pruritus), or related to its complications, such as acute cholangitis (jaundice, fever, abdominal pain), eventually accompanied by weight loss and worsening of cholestatic laboratory profile, especially a sustained elevation in serum bilirubin and alkaline phosphatase (ALP), can be associated with CCA as well [8, 24].
In this respect, a major concern in PSC is the development of dominant strictures. Dominant strictures are focal high-grade biliary stenoses, generally defined as having a diameter ≤1.5 mm in the common bile duct or ≤1 mm in the right and left hepatic duct [25]. They occur in approximately 50% of patients with PSC and can be difficult to discriminate from CCA, either clinically or morphologically. Typically, recurrent episodes of bacterial cholangitis in a PSC patient are highly suggestive of a dominant stricture and may contribute to disease progression [26]. The relationship between CCA and dominant strictures can be perplexing, since CCA may arise from a dominant stricture, whereas, on the other hand, only 5% of dominant strictures have an underlying malignancy. When associated with a dominant stricture, CCA usually develops in the hilum or in the common bile duct, and, conversely, benign dominant strictures affect mainly the extrahepatic bile ducts [8].
Diagnosis of PSC-Associated CCA: Critical Issues and Multimodal Approach
With the improvement of surgical resection and LT techniques for locally advanced CCA, early detection of this tumor when arising in a PSC background is crucial to improve patient prognosis. As there is no clear relationship between PSC duration and CCA development, patients with a recent PSC diagnosis should be also screened for biliary malignancy with the combined use of laboratory tests, cross-sectional imaging, and endoscopic techniques, along with conventional and, possibly, new biomarkers to be tested in serum and eventually in bile and in other biological fluids [6, 8].
Laboratory Tests and Serum Biomarkers
CCA usually presents with rapid worsening of liver biochemistries (mostly ALP and eventually total bilirubin), eventually leading to clinical deterioration (pruritus, jaundice, weight loss, acute cholangitis) in an otherwise stable PSC patient [27].
Among conventional serum biomarkers, carbohydrate antigen (CA) 19-9 , a membrane glycolipid expressed by tumoral duct cells, is the most associated with CCA, though studies addressing its role in PSC patients are scarce. In addition, CA19-9 has significant variability in sensitivity and specificity depending on the cutoff value. The optimal cutoff is 129 U/mL, showing a sensitivity of 78% and a specificity of 98%, though 1/3 of PSC patients with increased levels of CA19-9 above this cutoff are not diagnosed with CCA. Importantly, serum levels of CA19-9 are influenced by the allelic variants of fucosyltransferase (FUT). Two different FUT genotypes, 2 and 3, that determine the Lewis blood group, catalyze the final steps of CA19-9 biosynthesis. Based on these genotypes, distinct groups with low, intermediate, and high expression of CA19-9 can be identified, indicating FUT2/3 genotype-dependent cutoff values for CA19-9 as a means to improve its sensitivity by reducing the false positives [27,28,29]. Noteworthy is the observation that 7–10% of the general population is Lewis blood antigen-negative and lacks expression of CA19-9 [30]; thus, normal or undetectable levels of CA19-9 do not effectively rule out the possibility of CCA. Another factor that can limit the clinical usefulness of CA19-9 in PSC patients is bacterial cholangitis, which is responsible for marked though transient increase in CA19-9 serum levels [31], while dominant strictures seem to have less effect on biomarker expression [32].
Serum CEA is another biomarker of interest, as it is not influenced by bacterial cholangitis and dominant strictures, possesses a higher specificity than CA19-9, and potentially could be used to predict survival after CCA resection. However, compared with CA19-9, CEA has a lower sensitivity, as it is increased, for instance, by cigarette smoking (a well-established risk factor for CCA development). Similar to CA19-9, CEA levels are influenced by FUT genotype. Of note, measurement of both CA19-9 and CEA has been proposed to improve early diagnosis of CCA [8].
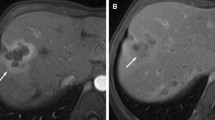
Imaging techniques are a critically important asset for CCA diagnosis, as the detection of morphological abnormalities in the biliary tree is a prerequisite for endoscopic procedures, as discussed in detail elsewhere in this book (Chap. 7, Viragh K et al.). In brief, ultrasonography (US) is a common first-line test and has a sensitivity of 57% and specificity of 94% in this context. However, while US is particularly useful in detecting mass lesions, the infiltrating or intraductal morphological phenotype of CCA can be difficult to appreciate, especially in a background of PSC [27, 33]. Magnetic resonance imaging (MRI) has a much higher sensitivity than US and has become the technique of choice for both diagnosis and staging of CCA. The combination of MRI with magnetic resonance cholangiopancreatography (MRCP) provides the most accurate noninvasive method to study the biliary tree and to unveil tumoral infiltration. More features suggestive of a neoplastic behavior can be identified by dynamic contrast-enhancement MRI, magnetic resonance angiography, and diffusion-weighted imaging (DWI), which permits recognition of distant metastases, involvement of the vascular bed, and distinction of CCA from HCC [33, 34]. Computed tomography (CT) can characterize mass lesions, investigate tissue invasion with involvement of regional lymph nodes, and detect the presence of extrahepatic dissemination in CCA, but its sensitivity and specificity is reduced in the setting of PSC-associated CCA (75% and 85%, respectively) [27, 33, 35].
18F-Fluoro-deoxyglucose (18F-FDG) positron emission tomography (PET), eventually complemented with CT (PET/CT), can be a valuable approach to detect early, small biliary tumors and metastases. In particular, PET is useful to discriminate CCA from dominant strictures in PSC patients. A high tissue uptake index (SUVmax/liver ≥3.3) is a good parameter for CCA diagnosis, with sensitivity and specificity of both around 90%, while an index <2.4 seems to rule out CCA [36]. Major drawbacks of this technique are (i) the increased number of false positives in conditions of ongoing tissue inflammation due to bacterial cholangitis or intense background disease activity and (ii) the lack of accuracy in detecting perihilar tumors, both of which are unfortunately common events in PSC.
Endoscopic procedures such as endoscopic retrograde cholangiopancreatography (ERCP) remain an important part of PSC management, in particular when imaging results are uncertain or tissue sampling is needed [37]. Dominant strictures represent the most common indication for endoscopic biliary procedures in PSC, as these lesions require careful exclusion of malignancy along with local treatment via balloon dilation and/or stenting [37, 38]. Biliary intraductal brushing can be performed during ERCP to evaluate for possible malignancy; despite a high specificity (>95%), however, it has poor sensitivity (5–40%) [39]. Thus, to improve diagnostic accuracy of conventional cytology, biliary brushing has been coupled with fluorescence in situ hybridization (FISH) assessing for chromosomal instability [39, 40], resulting in a specificity of nearly 100% and an increase in sensitivity up to 45–49% [41]. Of note, sensitivity can reach 76–89% if supported by analysis of the tumor suppressor gene p16 (by evaluating the deletion of the 9p21 locus) [41, 42]. Detection of polysomy by FISH either in multiple areas of the biliary tree (multifocal) or in consecutive endoscopic procedures (serial) has been associated with a higher risk of CCA than when detected in unifocal or single samples [43, 44].
Endoscopic ultrasound (EUS) is another available technique to evaluate dominant strictures (as well as lymphadenopathy), having the advantage of lower morbidity than ERCP [39]. A meta-analysis performed in biliary obstructions of different etiologies showed that EUS had an overall sensitivity of 78% and a specificity of 84% in detecting malignancy [45]. Sensitivity and specificity could be further improved by combining EUS with fine needle aspiration (FNA), though patients who underwent EUS-FNA would be excluded from LT according to the Mayo Clinic protocol because of the risk of tumor seeding [46]. Additional studies are needed to better understand the role of EUS in this setting [39].
Another useful technique that has drawn increasing interest is cholangioscopy, as it allows direct visualization of the biliary mucosa to detect suspicious lesions such as nodules, ulcers, polyps, or projections and to collect tissue samples [47]. A cholangioscopic finding of dilated, tortuous subepithelial vessels is a highly suggestive feature of malignancy, though it can also be present in PSC without dysplasia [40]. Similarly, cholangioscopic biopsies are relatively limited by their small size. Notably, it is important to recognize that most studies have been conducted so far with the first-generation devices. Given the introduction of the new (third-generation) high-resolution cholangioscope (Spyglass DS™, Boston Scientific Corp., Natick, MA, USA) that provides a more thorough inspection of the mucosal profile, further studies will be needed to reassess the diagnostic accuracy of this technique, its cost-efficacy, and the rate of adverse events [39].
Novel Tumoral Biomarkers
Given the limitations of conventional serum biomarkers and noninvasive techniques, there is a need to identify novel disease biomarkers aimed at improving the early detection of CCA, eventually beyond serum sampling. These include anti-glycoprotein 2 (GP2), bile and urine biomarkers, and extracellular vesicles.
Anti-GP2 is a secretory IgA autoantibody targeting proteins predominantly expressed by exocrine pancreatic cells that can be found in PSC patients, especially those with the classic variant involving the large bile ducts, where it likely associates with poor outcomes (meaning early death or shorter LT-free survival), and this effect was primarily dependent upon development of CCA. Among the several isoforms, the combined use of anti-GP21 and anti-GP24 IgA seems more sensitive than using only one isoform, and the detection of anti-GP23 IgG seems related with a higher risk of CCA development in PSC patients. Notably, the presence of anti-GP2 IgA could identify a subset of PSC patients with a severe disease phenotype, as its association with PSC/CCA is not related with duration of disease, older age at diagnosis, and serum levels of bilirubin [8, 48]. Thus, anti-GP2 IgA may be regarded as novel tool enabling early diagnosis of PSC-associated CCA, but further studies are awaited to figure out its possible role for prioritizing LT in high-risk PSC patients [8, 48]. Another panel that has been proposed with the aim of discriminating benign from malignant biliary strictures includes pyruvate kinase M2, cytokeratin 19 fragment, mucin 5 AC, and gamma glutamyl-transferase [8].
Another biological sample that can be harnessed for prognostic/diagnostic purposes in PSC is bile [28]. Bile and urine proteome analysis have shown interesting results, with combined analysis having a sensitivity of 72% and a specificity of 96% [8]. One fundamental issue with bile collection is that it requires ERC (or other invasive means of biliary access). This is a subject of active investigation deserving consideration in future studies [28, 49].
In addition to soluble factors, cholangiocytes may secrete extracellular vesicles (EVs) as a means of cell-to-cell communication. EVs contain proteins, lipids, and nucleic acids, such as micro-ribonucleic acids (miRNAs) and long noncoding RNAs (lncRNAs). In malignant cholangiocytes, a miRNA of interest is miRNA-195, which is mutually exchanged by neoplastic and stromal cells, as it is constitutionally downregulated in both cell types and, thus, could be involved in tumorigenesis. On the other hand, trafficking of lncRNA seems related more with CCA progression. EVs produced by cancer cells contain a range of pro-invasive factors normally not released by healthy cholangiocytes. Their assessment in the so-called liquid biopsy might provide a novel noninvasive tool for early detection of CCA [49, 50].
Surveillance Programs: Still Searching for the Way to Go
One of the main issues concerning the risk of CCA in PSC has been the lack of an effective evidence-based surveillance protocol to monitor these patients. There are a number of questions that must be addressed before establishing an effective program, including (a) how frequently surveillance should be performed, (b) the tools (radiological and laboratory) with which surveillance should be conducted, and (c) how to risk stratify patients for tumor development (e.g., are there some patients who need not undergo CCA surveillance or who need it more frequently than other PSC patients?) [27].
To help address this uncertainty, a study was undertaken in a large population of PSC patients undergoing annual imaging with US, CT, or MRI/MRCP coupled with annual CA19-9 testing, with further evaluation by MRI/MRCP and/or ERCP if any newly identified biliary lesion. Taking this approach, PSC patients in the surveillance group were found to have a significantly higher 5-year overall survival (68% vs 20%, p < 0.001) and a significantly lower rate of CCA-related adverse events (32% vs 75%, P < 0.001) compared to those without a regular surveillance [51]. Based primarily on the findings of this study, published in 2018, a CCA surveillance protocol was published in 2019 by the American Gastroenterological Association recommending the combination of imaging and CA19-9 for CCA surveillance [27]. Of the imaging modalities available, MRCP (with intravenous contrast, if possible) and US appeared to have the best performance characteristics [51]. Further considerations regarding cancer surveillance in PSC are discussed elsewhere [5, 8, 27]. Large prospective studies would be useful to identify the best surveillance strategy, with the ultimate goal of improving early diagnosis when CCA is more likely to be eligible for curative treatment (e.g., surgery, LT) [27, 51].
Treatment: LT Is Often the Most Convenient Approach for PSC-Associated CCA
PSC patients with a new CCA diagnosis should undergo a multidisciplinary evaluation to choose the best treatment option based on the tumor stage. Surgical resection and LT are the only potentially curative options for early-stage CCA. If the patient is eligible for resection, surgery is the first-line approach in all CCA subtypes. Patients with intrahepatic CCA can undergo resection of the involved segments or lobe, whereas distal CCA usually involves a pancreatoduodenectomy. In pCCA, based on tumor extension, resection can involve the intra- and extrahepatic bile ducts and the ipsilateral liver, the gallbladder, and the involved regional lymph nodes. Unfortunately, the 3-year survival rate is still quite low (<20%), even when a resection with negative tumor margins is achieved. Moreover, PSC-associated CCAs are rarely diagnosed at an early stage, with most patients presenting with advanced and unresectable disease and reduced functional liver mass caused by the underlying disease.
LT is an option for patients with unresectable disease, and it is particularly attractive in PSC patients as it removes the “oncogenic field effect” exerted by the underlying chronic fibroinflammation. In this regard, patient selection is crucial to achieve the best possible outcomes and to ensure the optimal organ allocation. Data from the Nordic Liver Transplant Center based on a cohort of 53 CCA patients (34 with PSC/CCA) shows a 5-year survival of 58% when patients were selected based on a TNM stage ≤2 and a CA19-9 level ≤100 U/mL, regardless of tumor localization [52]. A 5-year survival rate up to 70% can be achieved in patients with early-stage pCCA if neoadjuvant chemoradiation is performed, although less than 10% of patients are indeed eligible candidates [53]. Another procedure for patients with unresectable pCCA eventually eligible for LT is the Mayo Clinic protocol. In this multimodal approach, patients undergo external beam radiation therapy, followed by 2 weeks of brachytherapy and then abdominal exploration for staging. Intravenous 5-fluorouracil is administered for chemosensitization during radiotherapy, and capecitabine is administered afterward until LT is performed. Following this protocol, a 5-year survival of 74% was reported in the first study [53], and similar results were reproduced in a larger multicenter study in which, notably, more than two thirds of patients had a PSC-associated CCA [54].
Beyond surgery, there are currently no data regarding specific treatment of PSC/CCA in more advanced stages, and the reader may refer to the relative chapters discussed elsewhere in the present book. Whether PSC/CCA harbors specific molecular signatures possibly behaving as actionable targets is a subject deserving attention by future studies. In fact, given the growing number of potential targets emerging in CCA, patients with unresectable PSC/CCA can be an ideal subset to be considered for enrolment in clinical trials [54, 55].
Summary and Future Directions
The close association of CCA with PSC provides a unique opportunity to unravel the intricate mechanisms by which a chronic inflammatory epithelial lesion with prominent scarring progresses through dysplasia and, in some cases, carcinoma. Although this area has been actively investigated in the past few decades, several challenges remain. For instance, the approach to surveillance remains an area of uncertainty, and discriminating CCA from a DS still often poses a diagnostic conundrum. From a therapeutic perspective, LT remains the most definitive treatment for CCA, but in some cases, this is not an option, in part because PSC-associated CCA is a difficult-to-diagnose disease in early stages. Future efforts are eagerly awaited to identify reliable predictive biomarkers of PSC progression and associated carcinogenesis as well as effective tailored therapies.
Abbreviations
- AIH:
-
Autoimmune hepatitis
- ALP:
-
Alkaline phosphatase
- CA:
-
Carbohydrate antigen
- CCA:
-
Cholangiocarcinoma
- CD:
-
Crohn’s disease
- COX:
-
Cyclooxygenase
- CT:
-
Computer tomography
- DWI:
-
Diffusion-weighted imaging
- ECM:
-
Extracellular matrix
- ERCP:
-
Endoscopic retrograde cholangiopancreatography
- EUS:
-
Endoscopic ultrasound
- EV:
-
Extracellular vesicle
- F-FDG:
-
F-Fluoro-deoxyglucose
- FISH:
-
Fluorescence in situ hybridization
- FNA:
-
Fine needle aspiration
- FUT:
-
Fucosyltransferase
- GP2:
-
Glycoprotein 2
- HCC:
-
Hepatocellular carcinoma
- IBD:
-
Inflammatory bowel disease
- lncRNA:
-
Long noncoding RNA
- LT:
-
Liver transplantation
- miRNA:
-
Micro-ribonucleic acid
- MRCP:
-
Magnetic resonance cholangiopancreatography
- MRI:
-
Magnetic resonance imaging
- NO:
-
Nitric oxide
- pCCA:
-
Perihilar cholangiocarcinoma
- PET:
-
Positron emission tomography
- PSC:
-
Primary sclerosing cholangitis
- TRAIL:
-
Tumor necrosis factor-related apoptosis-inducing ligand
- UC:
-
Ulcerative colitis
- US:
-
Ultrasonography
References
Lazaridis KN, LaRusso NF. Primary Sclerosing Cholangitis. N Engl J Med. 2016 Sep 22;375(12):1161–70;
Lindor KD, Kowdley KV, Harrison ME. ACG clinical guideline: primary sclerosing cholangitis. Am J Gastroenterol. 2015;110:646–59.
Boonstra K, Van Erpecum KJ, Van Nieuwkerk KMJ, Drenth JPH, Poen AC, Witteman BJM, Tuynman HARE, Beuers U, Ponsioen CY. Primary sclerosing cholangitis is associated with a distinct phenotype of inflammatory bowel disease. Inflamm Bowel Dis. 2012;18:2270–6.
Karlsen TH, Folseraas T, Thorburn D, Vesterhus M. Primary sclerosing cholangitis – a comprehensive review. J Hepatol. 2017;67:1298–323.
Fung BM, Lindor KD, Tabibian JH. Cancer risk in primary sclerosing cholangitis: Epidemiology, prevention, and surveillance strategies. World J Gastroenterol. 2019 Feb 14;25(6):659-671.
Bonato G, Cristoferi L, Strazzabosco M, Fabris L. Malignancies in primary sclerosing cholangitis--a continuing threat. Dig Dis. 2015;33:140–8.
Zenouzi R, Weismüller TJ, Hübener P, et al. Low risk of hepatocellular carcinoma in patients with primary sclerosing cholangitis with cirrhosis. Clin Gastroenterol Hepatol. 2014;12:1733–8.
Song J, Li Y, Bowlus CL, Yang GX, Leung PSC, Gershwin ME. Cholangiocarcinoma in patients with primary sclerosing cholangitis (PSC): a comprehensive review. Clin Rev Allergy Immunol. 2019; https://doi.org/10.1007/s12016-019-08764-7.
Rizvi S, Gores GJ. Pathogenesis, diagnosis, and management of cholangiocarcinoma. Gastroenterology. 2013;145:1215–29.
Burak K, Angulo P, Pasha TM, Egan K, Petz J, Lindor KD. Incidence and risk factors for cholangiocarcinoma in primary sclerosing cholangitis. Am J Gastroenterol. 2004;99:523–6.
Claessen MMH, Vleggaar FP, Tytgat KMAJ, Siersema PD, van Buuren HR. High lifetime risk of cancer in primary sclerosing cholangitis. J Hepatol. 2009;50:158–64.
Quinn KP, Tabibian JH, Lindor KD. Clinical implications of serial versus isolated biliary fluorescence in situ hybridization (FISH) polysomy in primary sclerosing cholangitis. Scand J Gastroenterol. 2017;52:377–81.
Chung BK, Karlsen TH, Folseraas T. Cholangiocytes in the pathogenesis of primary sclerosing cholangitis and development of cholangiocarcinoma. BBA - Mol Basis Dis. 2018;1864:1390–400.
Singal AK, Stanca CM, Clark V, Dixon L, Levy C, Odin JA, Fiel MI, Friedman SL, Bach N. Natural history of small duct primary sclerosing cholangitis: a case series with review of the literature. Hepatol Int. 2011;5:808–13.
Mederacke I, Hsu CC, Troeger JS, Huebener P, Mu X, Dapito DH, Pradere J-P, Schwabe RF. Fate tracing reveals hepatic stellate cells as dominant contributors to liver fibrosis independent of its aetiology. Nat Commun. 2013;4:2823.
Fabris L, Cadamuro M, Cagnin S, Strazzabosco M, Gores GJ. Liver matrix in benign and malignant biliary tract disease. Semin Liver Dis. 2020; https://doi.org/10.1055/s-0040-1705109.
O’Hara SP, Karlsen TH, NF LR. Cholangiocytes and the environment in primary sclerosing cholangitis: where is the link? Gut. 2017;66:1873 LP–1877.
Kamihira T, Shimoda S, Nakamura M, Yokoyama T, Takii Y, Kawano A, Handa M, Ishibashi H, Gershwin ME, Harada M. Biliary epithelial cells regulate autoreactive T cells: implications for biliary-specific diseases. Hepatology. 2005;41:151–9.
Xu B, Broome U, Ericzon BG, Sumitran-Holgersson S. High frequency of autoantibodies in patients with primary sclerosing cholangitis that bind biliary epithelial cells and induce expression of CD44 and production of interleukin 6. Gut. 2002;51:120–7.
Takeda K, Kojima Y, Ikejima K, et al. Death receptor 5 mediated-apoptosis contributes to cholestatic liver disease. Proc Natl Acad Sci. 2008;105:10895–900.
Yoon JH, Canbay AE, Werneburg NW, Lee SP, Gores GJ. Oxysterols induce cyclooxygenase-2 expression in cholangiocytes: implications for biliary tract carcinogenesis. Hepatology. 2004;39:732–8.
Yoon JH, Gwak GY, Lee HS, Bronk SF, Werneburg NW, Gores GJ. Enhanced epidermal growth factor receptor activation in human cholangiocarcinoma cells. J Hepatol. 2004;41:808–14.
Cadamuro M, Stecca T, Brivio S, Mariotti V, Fiorotto R, Spirli C, Strazzabosco M, Fabris L. The deleterious interplay between tumor epithelia and stroma in cholangiocarcinoma. Biochim Biophys Acta Mol basis Dis. 2018;1864:1435–43.
Dyson JK, Beuers U, Jones DEJ, Lohse AW, Hudson M. Seminar primary sclerosing cholangitis. Lancet. 2018;391:2547–59.
Hilscher MB, Tabibian JH, Carey EJ, Gostout CJ, Lindor KD. Dominant strictures in primary sclerosing cholangitis: a multicenter survey of clinical definitions and practices. Hepatol Commun. 2018;2:836–44.
Pohl J, Ring A, Stremmel W, Stiehl A. The role of dominant stenoses in bacterial infections of bile ducts in primary sclerosing cholangitis. Eur J Gastroenterol Hepatol. 2006;18:69–74.
Bowlus CL, Lim JK, Lindor KD. AGA clinical practice update on surveillance for hepatobiliary cancers in patients with primary sclerosing cholangitis: expert review. Clin Gastroenterol Hepatol. 2019;17:2416–22.
Wannhoff A, Gotthardt DN. Recent developments in the research on biomarkers of cholangiocarcinoma in primary sclerosing cholangitis. Clin Res Hepatol Gastroenterol. 2019 Jun;43(3):236–243.
Wannhoff A, Hov JR, Folseraas T, et al. FUT2 and FUT3 genotype determines CA19-9 cut-off values for detection of cholangiocarcinoma in patients with primary sclerosing cholangitis. J Hepatol. 2013;59:1278–84.
Nehls O, Gregor M, Klump B. Serum and bile markers for cholangiocarcinoma. Semin Liver Dis. 2004;24:139–54.
Sinakos E, Saenger AK, Keach J, Kim WR, Lindor KD. Many patients with primary sclerosing cholangitis and increased serum levels of carbohydrate antigen 19-9 do not have cholangiocarcinoma. Clin Gastroenterol Hepatol. 2011;9:434–9.
Wannhoff A, Rupp C, Friedrich K, et al. Inflammation but not biliary obstruction is associated with carbohydrate antigen 19-9 levels in patients with primary sclerosing cholangitis. Clin Gastroenterol Hepatol. 2015;13:2372–9.
Jhaveri KS, Hosseini-Nik H. MRI of cholangiocarcinoma. J Magn Reson Imaging. 2015;42:1165–79.
Chapman R, Fevery J, Kalloo A, Nagorney DM, Boberg KM, Shneider B, Gores GJ; American Association for the Study of Liver Diseases. Diagnosis and management of primary sclerosing cholangitis. Hepatology. 2010 Feb;51(2):660–78.
Charatcharoenwitthaya P, Enders FB, Halling KC, Lindor KD. Utility of serum tumor markers, imaging, and biliary cytology for detecting cholangiocarcinoma in primary sclerosing cholangitis. Hepatology. 2008;48:1106–17.
Sangfelt P, Sundin A, Wanders A, Rasmussen I, Karlson BM, Bergquist A, Rorsman F. Monitoring dominant strictures in primary sclerosing cholangitis with brush cytology and FDG-PET. J Hepatol. 2014;61:1352–7.
Aabakken L, Karlsen TH, Albert J, et al. Role of endoscopy in primary sclerosing cholangitis: European Society of Gastrointestinal Endoscopy (ESGE) and European Association for the Study of the Liver (EASL) clinical guideline. Endoscopy. 2017;49:588–608.
European Association for the Study of the Liver. EASL clinical practice guidelines: management of cholestatic liver diseases. J Hepatol. 2009;51:237–67.
Fung BM, Tabibian JH. Biliary endoscopy in the management of primary sclerosing cholangitis and its complications. Liver Res. 2019;3:106–17.
Tabibian JH. Advanced endoscopic imaging of indeterminate biliary strictures. World J Gastrointest Endosc. 2015;7:1268.
Gonda TA, Glick MP, Sethi A, et al. Polysomy and p16 deletion by fluorescence in situ hybridization in the diagnosis of indeterminate biliary strictures. Gastrointest Endosc. 2012;75:74–9.
Boldorini R, Paganotti A, Andorno S, Orlando S, Mercalli F, Orsello M, Ballarè M, Magnani C, Sartori M. A multistep cytological approach for patients with jaundice and biliary strictures of indeterminate origin. J Clin Pathol. 2015;68:283–7.
Fritcher EGB, Kipp BR, Voss JS, Clayton AC, Lindor KD, Halling KC, Gores GJ. Primary sclerosing cholangitis patients with serial polysomy fluorescence in situ hybridization results are at increased risk of cholangiocarcinoma. Am J Gastroenterol. 2011;106:2023–8.
Eaton JE, Barr Fritcher EG, Gores GJ, Atkinson EJ, Tabibian JH, Topazian MD, Gossard AA, Halling KC, Kipp BR, Lazaridis KN. Biliary multifocal chromosomal polysomy and cholangiocarcinoma in primary sclerosing cholangitis. Am J Gastroenterol. 2015;110:299–309.
Garrow D, Miller S, Sinha D, Conway J, Hoffman BJ, Hawes RH, Romagnuolo J. Endoscopic ultrasound: a meta-analysis of test performance in suspected biliary obstruction. Clin Gastroenterol Hepatol. 2007; https://doi.org/10.1016/j.cgh.2007.02.027.
Navaneethan U, Njei B, Venkatesh P, et al. Endoscopic ultrasound in the diagnosis of cholangiocarcinoma as the etiology of biliary strictures: a systematic review and meta-analysis. Gastroenterol Rep. 2015; https://doi.org/10.1093/GASTRO/GOU057.
Seo DW, Lee SK, Yoo KS, Kang GH, Kim MH, Suh DJ, Il MY. Cholangioscopic findings in bile duct tumors. Gastrointest Endosc. 2000;52:630–4.
Jendrek ST, Gotthardt D, Nitzsche T, et al. Anti-GP2 IgA autoantibodies are associated with poor survival and cholangiocarcinoma in primary sclerosing cholangitis. Gut. 2017;66:137–44.
Rizvi S, Eaton J, Yang JD, Chandrasekhara V, Gores GJ. Emerging technologies for the diagnosis of perihilar cholangiocarcinoma. Semin Liver Dis. 2018;38:160–9.
Arbelaiz A, Azkargorta M, Krawczyk M, et al. Serum extracellular vesicles contain protein biomarkers for primary sclerosing cholangitis and cholangiocarcinoma. Hepatology. 2017;66:1125–43.
Ali AH, Tabibian JH, Nasser-Ghodsi N, Lennon RJ, DeLeon T, Borad MJ, Hilscher M, Silveira MG, Carey EJ, Lindor KD. Surveillance for hepatobiliary cancers in patients with primary sclerosing cholangitis. Hepatology. 2018;67:2338–51.
Friman S, Foss A, Isoniemi H, Olausson M, Höckerstedt K, Yamamoto S, Karlsen TH, Rizell M, Ericzon B-G. Liver transplantation for cholangiocarcinoma: Selection is essential for acceptable results. Scand J Gastroenterol. 2011;46:370–5.
Rosen CB, Heimbach JK, Gores GJ. Liver transplantation for cholangiocarcinoma. Transpl Int. 2010;23:692–7.
Darwish Murad S, Kim WR, Harnois DM, et al. Efficacy of neoadjuvant chemoradiation, followed by liver transplantation, for perihilar cholangiocarcinoma at 12 US centers. Gastroenterology. 2012;143:88–98.
Rizvi S, Khan SA, Hallemeier CL, Kelley RK. Cholangiocarcinoma — evolving concepts and therapeutic strategies. Nat Rev Clin Oncol. 2017;15:95–111.
Hirschfield GM, Karlsen TH, Lindor KD, Adams DH. Primary sclerosing cholangitis. Lancet. 2013;382:1587–99.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2021 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Cagnin, S., Tabibian, J.H., Fabris, L. (2021). PSC-Associated Cholangiocarcinoma: Diagnostic and Therapeutic Considerations. In: Tabibian, J.H. (eds) Diagnosis and Management of Cholangiocarcinoma. Springer, Cham. https://doi.org/10.1007/978-3-030-70936-5_10
Download citation
DOI: https://doi.org/10.1007/978-3-030-70936-5_10
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-70935-8
Online ISBN: 978-3-030-70936-5
eBook Packages: MedicineMedicine (R0)