Abstract
Familial dysautonomia (FD or Riley–Day syndrome, hereditary sensory and autonomic neuropathy type III) is a rare autosomal recessive disorder characterized by impaired development of primary sensory and autonomic neurons resulting in a severe neurological phenotype, which includes arterial baroreflex and chemoreflex failure with high frequency of sleep-disordered breathing and sudden death during sleep. Although a rare disease, FD represents a unique template to study the interactions between sleep-disordered breathing and abnormal chemo- and baroreflex function. In patients with FD, ventilatory responses to hypercapnia are reduced and to hypoxia are almost absent. In response to hypoxia, these patients develop paradoxical hypoventilation, hypotension, bradycardia, and potentially, death. Impaired ventilatory control due to chemoreflex failure achieves special relevance during sleep when conscious control of respiration is withdrawn. Overall, the prevalence of sleep-disordered breathing in FD is very high in adult (85%) and pediatric (95%) patients. Obstructive apnea events are more frequent in adults, whereas central apnea events are more severe and frequent in the pediatric population. The annual incidence rate of sudden death during sleep in patients with FD is 3.4 per 1000 person-year, compared to 0.5–1 per 1000 person-year of sudden unexpected death in epilepsy. In this chapter, we summarize recent developments in the understanding of sleep-disordered breathing in patients with FD, the risk factors for sudden death during sleep, and the specific therapeutic interventions that could prevent it.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
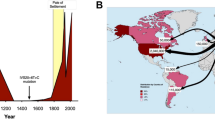
Familial dysautonomia (FD, also known as Riley–Day syndrome, hereditary sensory and autonomic neuropathy type III) is a rare autosomal recessive disease. It was first described in 1949 in children with Jewish Ashkenazi ancestry [1, 2]. The disease is caused by a founder mutation in the IkB kinase-associated protein gene (IKBKAP or ELP1) resulting in increased levels of mutant, defective, ELP-1 (IKAP) protein, mostly in central and peripheral nervous systems. Lack of functional ELP-1 causes impaired development of primary sensory and autonomic neurons [3,4,5,6] resulting in a severe neurological phenotype, which includes arterial baroreflex and chemoreflex failure with high frequency of sleep-disordered breathing and sudden death during sleep [7,8,9,10,11,12]. FD represents a unique template to study the interactions between sleep-disordered breathing and abnormal chemo- and baroreflex function. We summarize in this chapter recent developments in the understanding of sleep-disordered breathing in patients with FD, the risk factors for sudden death during sleep, and the specific interventions that could prevent it.
Phenotype of Familial Dysautonomia
ELP-1 deficiency in FD affects the development of primary sensory (afferent) neurons, resulting in a complex neurological phenotype. Impaired development of primary sensory nerves results in reduced pain and temperature sensation, absent deep tendon reflexes and gait ataxia [13], as well as optic neuropathy [14], and neurogenic dysphagia contributing to chronic lung disease [15, 16]. In addition, abnormal development of mechano- and chemosensory neurons results in baro- and chemoreflex failure with orthostatic hypotension, paroxysmal hypertension, and abnormal control of heart rate and ventilatory responses to hypoxia and hypercapnia [17, 18]. These contribute to early-onset target organ damage [2, 19, 20] and chronic respiratory disease.
Chemoreflex Failure
Physiology of Respiration and the Chemoreflex
The chemoreceptor reflex is a negative feedback mechanism that regulates ventilatory drive to maintain arterial pressures of oxygen (PaO2) and carbon dioxide (PaCO2) and pH within a narrow range. The afferent part of the chemoreflex includes peripheral multimodal chemoreceptor cells in the carotid body and central CO2-H+-sensing chemoreceptor neurons in the brainstem. Peripheral chemoreceptor cells in the carotid bodies, which derive from the neural crest, monitor the partial pressure of oxygen (pO2), pCO2, and pH in arterial blood. They synapse with nerve terminals of chemoreceptor neurons, with cell bodies in the petrosal ganglia of the glossopharyngeal nerve, which transmit chemosensory information to neurons in the nucleus of the solitary tract (NTS) in the medulla. These NTS neurons project to the pre-Bötzinger complex, a group of neurons that generates the rhythmic signals underlying the periodic drive for inspiration [21]. Neurons in the pre-Bötzinger complex project to neurons of the dorsal and ventral respiratory groups in the medulla, which control spinal motoneurons innervating respiratory muscles (diaphragm, intercostal and abdominal), as well as pre-motoneurons projecting to vagal (cranial nerve X) and hypoglossal (cranial nerve XII) motor neurons that control the upper airway muscles and tongue [22, 23].
Central breathing networks are also modulated by input from mechanoreceptors sensing the stretch of the respiratory muscles (e.g., diaphragm) and lungs. Stretch receptors (mechano-sensors) in smooth muscle of bronchi and bronchioles send information via the vagus nerve to the pre-Bötzinger complex and other areas in the brainstem. Lung stretch-receptor afferents conveying signals to brainstem interneurons rhythmically inhibit the pre-Bötzinger complex and activate the lateral parafacial nucleus when lungs are inflated (inspiratory termination reflex) and conversely excite the pre-Bötzinger complex and inhibit the lateral parafacial nucleus when lungs are deflated. This feedback underlies the Hering-Breuer reflexes, essential in controlling inflation and deflation of the lungs.
In normal individuals, most of the respiratory control is exerted by brainstem neurons—central chemosensory neurons and glia located in the ventral parafacial nucleus and other regions respond to changes in partial pressure of CO2 (pCO2) and pH in the cerebrospinal fluid. These neurons project to the pre-Bötzinger complex – the primary neurons generating the essential periodic drive for inspiration – and other sites to coordinate the breathing cycle [21].
Breathing in humans is extremely sensitive to changes in the levels of pCO2 in arterial blood, as they directly affect acid-base balance. For instance, in healthy subjects, an increase in arterial pCO2 from 40 to 41 mmHg (~2.5%) stimulates central and peripheral chemoreceptors and increase minute ventilation from 5 to 7 liters (~40%). In contrast, under normal conditions, breathing is relatively insensitive to changes in levels of pO2 in arterial blood. However, when oxygen levels decrease and arterial pO2 is less than ~60 mmHg (e.g., high altitude or intense exercise), hypoxia becomes a powerful stimulus increasing ventilation at any given pCO2 level [24]. Decreases in pH (i.e., increases in H+ concentration) stimulate central and peripheral chemoreceptors resulting in hyperventilation. In healthy subjects, reductions in pO2 cause tachycardia and moderate increases in blood pressure, and both hypoxia and hypercapnia increase ventilatory drive and central sympathetic outflow. Baroreflex activation normally abolishes the increase in sympathetic activity induced by hypoxia, but not by hypercapnia [25,26,27].
Cardiorespiratory Consequences of Chemo- and Baroreflex Failure
Neurological disorders affecting central or peripheral chemoreceptor neurons can manifest with hypoxia and hypercapnia due to hypoventilation and most disturbingly episodes of apnea. In patients with FD, ventilatory responses to hypercapnia are reduced and to hypoxia are almost absent. In response to hypoxia, thee patients develop paradoxical hypoventilation, hypotension, bradycardia, and, potentially, death [7,8,9,10,11]. Impaired ventilatory control due to chemoreflex failure achieves special relevance during sleep when conscious control of respiration withdraws. Virtually all patients with FD have some degree of sleep-disordered breathing [9, 28,29,30], which is a risk factor for sudden unexpected death during sleep [12].
In patients with FD, cardiorespiratory responses to hypoxia and hypercapnia are markedly abnormal, likely due to impaired afferent chemo- and baroreflex neurons. Several investigations have consistently reported these responses [7,8,9,10,11]. Specifically, in patients with FD (Table 26.1):
-
(a)
Hypercapnia decreases the ventilatory response, instead of increasing it, as it occurs in normal subjects.
-
(b)
Hypoxia results in little or no increase in ventilatory response, rather than the marked increase seen in normal subjects.
-
(c)
During hypoxia and hypercapnia, patients with FD experience bradycardia and hypotension, with some patients experiencing convulsive syncope (frequently misdiagnosed as “grand mal seizures”), instead of tachycardia and a moderate increase in blood pressure as in normal subjects.
Studying six subjects with FD, Edelman and colleagues [8] described that sudden relief of hypoxemia (e.g., with the administration of intranasal 100% O2) was followed by complete apnea of variable duration (10–56 seconds) in four subjects, instead of only a mild decrease in ventilation (−40% in tidal volume) as in normal subjects. The apnea following the abrupt relief of hypoxia in some subjects with FD might be a consequence of cessation of the hypoxic drive from the peripheral chemoreceptors, suggesting that, at least in some patients, residual peripheral chemoreceptor function might remain.
One dramatic clinical consequence of these cardiorespiratory abnormalities is breath-holding episodes. These are relatively frequent in children with FD after crying or laughing and can result in severe hypotension, hypoxia, and decerebrate posturing before breathing resumes [31]. In addition, during respiratory infections, patients with FD have no compensatory tachypnea and can suffer hypotension and syncope in low-oxygen environments, such as high altitude, airplane travel (although modern airplane cabins are pressurized, partial pressure of O2 may be low), and underwater swimming [15].
Sleep-Disordered Breathing
Several studies, some performed decades ago, suggested high prevalence of sleep-disordered breathing in patients with FD [9, 10, 28, 29]. All studies had important limitations, including small sample size, inclusion of subjects before genetic confirmation of the disease was available, lack of end-tidal CO2 (EtCO2) measurements, selection bias due to inclusion of only symptomatic patients, and inclusion of either adult or pediatric patients only. To overcome these limitations we conducted a large comprehensive study reporting the results of in-hospital polysomnography from 75 consecutive adult and pediatric patients (with genetically confirmed IKBKAP mutation) performed regardless of the presence of sleep-related symptoms [30].
Overall, almost all adult (85%) and pediatric (95%) patients had some degree of sleep-disordered breathing [30]. Obstructive apnea events were more frequent in adults, whereas central apnea events were more severe and frequent in children. While the number of central events decreased with advancing age, the severity of hypoventilation (average and maximum EtCO2 levels) progressively worsened with age, suggesting that the mechanisms driving central events tended to have less influence as the brain matured.
The amygdala and hippocampus are specifically involved in breathing control and the pathophysiology of central apneas [32]. Because ELP-1 is required for the normal CNS development and is highly expressed in amygdala and hippocampus [33], it is possible that abnormal development and maturation of these regions may underlie the high frequency of central events during the pediatric years in FD. As these regions mature with age, central events become less frequent.
Not surprisingly, a higher apnea hypopnea index was associated with increased severity of hypoxia and hypoventilation. Notably, in 46% of patients hypoventilation and hypercapnia occurred with no accompanying apnea [30]. This finding has key clinical implications: episodes of hypercapnia not associated with apneas might be missed in polysomnography studies that do not include EtCO2 monitoring. Expert consensus guidelines now recommend EtCO2 monitoring in all sleep studies performed in patients with FD [15].
In addition to chemoreflex failure, additional factors contribute to sleep apnea and the rapid development of hypoxemia in patients with FD. Patients have craniofacial abnormalities with large tonsils and adenoids that predispose to upper airway obstruction, and a smaller thorax and vital capacity due to a physically smaller body habitus and limited chest wall expansion caused by kyphoscoliosis. Additionally, if anemia is present, oxygen-carrying capacity is decreased. Finally, gastroesophageal reflux, frequently present in FD, can cause reflex laryngeal closure resulting in apnea. This laryngeal closure reflex has been implicated in the pathogenesis of sudden-infant death syndrome [34, 35] and could potentially play a role in sleep-disordered breathing in FD. These factors may contribute to prolonged apnea, as well as poor tolerance of environments with low partial pressure of oxygen, such as pressurized airplane cabins and high altitude [15].
Sudden Unexpected Death During Sleep (SUDS)
The two most common causes of death in FD are sudden unexpected death during sleep (SUDS) and respiratory disorders. SUDS is defined as a sudden, unexpected, witnessed or unwitnessed, nontraumatic, and non-drowning death occurring during sleep, with or without evidence of a seizure. Until recently, the risk factors for SUDS in FD remained unidentified. In a recent study, we hypothesized that the high incidence of SUDS in patients with FD was linked to the presence of respiratory abnormalities during sleep. To test this hypothesis, we analyzed the clinical features and polysomnography findings of patients with FD who died suddenly during sleep and compared them to age- and sex-matched patients with FD who remained alive at the time of the study.
This study was based on the New York University (NYU) FD Patient Registry, an ongoing, prospective study of the natural history of patients with FD. The study began in 1970 and contains clinical and diagnostic data, including cause of death, on 670 patients at the time of the study. Of these, 327 (49%) remained alive at the time of the study. All patients have genetic confirmation of FD; more than 99% are homozygous for the same founder mutation (6T>C change) in the IKBKAP gene. The majority of patients included in the Registry (above 50%) are from the United States. Patients are followed closely and seen at least once a year [2].
We found that the annual incidence rate of SUDS in patients with FD is 3.4 per 1000 person-year, compared to 0.5–1 per 1000 person-year of sudden unexpected death in epilepsy (SUDEP) [36]. The Registry search specifically identified 32 (14 women) patients with FD and SUDS who had undergone polysomnography in the 18-month period before death. SUDS occurred most frequently during the second and third decades of life (mean age at death was 29.3 ± 12.4 years old). Autopsy was available in six cases. All of them showed brainstem, spinal cord, and dorsal root ganglia atrophy, which are neuropathological hallmarks of FD [37, 38]. These six cases showed no structural cardiac pathology and no acute brain lesions that could otherwise explain their death. Most of them had nonspecific pulmonary congestion or focal hemorrhage, typically seen as a consequence, rather than a cause, of asphyxia.
Multivariable analysis disclosed that treatment with fludrocortisone, plasma potassium levels below 4 mEq/L, and untreated sleep apnea were factors independently associated with increased risk of SUDS in patients with FD. Conversely, treatment with nocturnal noninvasive ventilation was associated with a reduced risk of SUDS.
Taken together, these findings indicate that in patients with FD, sleep-disordered breathing with chemoreflex failure results in episodes of severe hypoxia, hypercapnia, hypotension, and bradycardia. In some patients, hypokalemia is an added factor, potentially contributing to fatal cardiac arrhythmias.
Therapeutic Implications
Noninvasive Ventilation
The finding that untreated sleep apnea and fludrocortisone are independent risk factors for SUDS in patients with FD has important therapeutic implications. Early identification of sleep abnormalities with polysomnography and implementation of noninvasive ventilation with CPAP or BiPAP when required are now encouraged in expert consensus guidelines for the diagnosis and management of respiratory disorders in FD [15].
Treatment with noninvasive ventilation not only decreases the risk of apneas, hypopneas, and sudden death during sleep but also improves daytime ventilatory responses, as recently described [39]. Indeed, treatment with nocturnal noninvasive ventilation in patients with FD results in a marked reduction in daytime arterial pCO2 suggesting that nocturnal noninvasive ventilation contributes to maintain arterial pCO2 levels during wakefulness by, perhaps, resetting the chemoreceptor to lower pCO2 levels.
Role of Potassium
The finding that potassium levels in the low range of normality and treatment with fludrocortisone were associated with SUDS was somewhat unexpected. Fludrocortisone (9α-fluorocortisol) is a synthetic mineralocorticoid that increases renal sodium and water reabsorption, expands intravascular volume, and increases blood pressure. Fludrocortisone for the treatment of orthostatic hypotension in patients with FD became widespread in the 1990s, sometimes at very high dosages (up to 0.6 mg/day). Hypokalemia is a very frequent side effect of fludrocortisone therapy [40]. Thus, it is likely that lower serum potassium levels in cases with SUDS were the result of fludrocortisone treatment. In the general population, hypokalemia and plasma potassium levels in the lower range of normality are independent risk factors for life-threatening arrhythmias and sudden cardiac death [41]. Of note, all drugs proven to reduce mortality and morbidity rates in patients with cardiovascular disease increase plasma potassium concentration [41]. Because specific potassium (TASK-1) channels are key components of the arterial chemoreceptors [42, 43], it is tempting to hypothesize that in patients with FD, lower potassium levels may worsen chemoreceptor failure. Indeed, dysfunction of the TASK-1 receptor in mice results in attenuated cardiorespiratory responses to hypoxia [42], a similar phenotype to that described in patients with FD.
Therefore, reduction or, when possible, discontinuation of fludrocortisone treatment is now recommended. Alternatives to fludrocortisone for the treatment of orthostatic hypotension include non-pharmacological measures and midodrine. Frequent monitoring of plasma potassium concentration during the first 2 weeks following discontinuation is recommended as some patients may develop hyperkalemia. Fludrocortisone discontinuation has other benefits, as long-term treatment with fludrocortisone is associated with target organ damage, including left ventricular hypertrophy and renal failure [44].
Conclusions
The interactions between sleep disorders and autonomic nervous system abnormalities inducing potentially fatal cardiovascular consequences are increasingly recognized in a variety of neurological disorders [45,46,47,48]. In FD, discoveries in the last decade have defined the phenotype of the disease, characterized by deafferentation resulting in baroreflex and chemoreflex failure with a high frequency of sleep disordered breathing and SUDS [2, 12, 30]. The recent identification of specific risk factors for SUDS has resulted in the widespread implementation of noninvasive ventilation and reduction or discontinuation of fludrocortisone therapy [12]. Noninvasive ventilation in FD may also have the potential of reversing daytime hypercapnia [39].
A number of questions regarding the pathophysiology of sleep-disordered breathing in FD remain. Chemoreceptor failure should result in central sleep apnea, which is the phenotype in children, but not in adults with FD who have predominantly obstructive sleep apnea. Other factors, such as upper airway abnormalities or interactions between the chemoreceptor signals and upper airway regulation might be responsible and need to be studied. Airway stretch mechanosensing neurons are important for maintaining normal breathing in adults. Functional ablation of mechanosensing neurons in mice abolishes Hering-Breuer reflexes and causes apnea, respiratory failure, and death [49, 50], not unlike the phenotype of FD. It is likely that mechanical signals from airway-innervating sensory neurons are also impaired in FD, but this has not been specifically studied neither in patients nor in animal models of FD [51, 52]. Further investigation of the ventilatory responses during sleep in patients with FD and elucidation of the role of potassium in chemoreceptor function may prove valuable to identify novel therapeutic approaches.
References
Riley CM, Day RL, Greeley DM, Langford WS. Central autonomic dysfunction with defective lacrimation; report of five cases. Pediatrics. 1949;3(4):468–78.
Norcliffe-Kaufmann L, Slaugenhaupt SA, Kaufmann H. Familial dysautonomia: history, genotype, phenotype and translational research. Prog Neurobiol. 2017;152:131–48.
Blumenfeld A, Slaugenhaupt SA, Axelrod FB, Lucente DE, Maayan C, Liebert CB, et al. Localization of the gene for familial dysautonomia on chromosome 9 and definition of DNA markers for genetic diagnosis. Nat Genet. 1993;4(2):160–4.
Slaugenhaupt SA, Blumenfeld A, Gill SP, Leyne M, Mull J, Cuajungco MP, et al. Tissue-specific expression of a splicing mutation in the IKBKAP gene causes familial dysautonomia. Am J Hum Genet. 2001;68(3):598–605.
Mezey E, Parmalee A, Szalayova I, Gill SP, Cuajungco MP, Leyne M, et al. Of splice and men: what does the distribution of IKAP mRNA in the rat tell us about the pathogenesis of familial dysautonomia? Brain Res. 2003;983(1–2):209–14.
Hunnicutt BJ, Chaverra M, George L, Lefcort F. IKAP/Elp1 is required in vivo for neurogenesis and neuronal survival, but not for neural crest migration. PLoS One. 2012;7(2):e32050.
Filler J, Smith AA, Stone S, Dancis J. Respiratory control in familial dysautonomia. J Pediatr. 1965;66:509–16.
Edelman NH, Cherniack NS, Lahiri S, Richards E, Fishman AP. The effects of abnormal sympathetic nervous function upon the ventilatory response to hypoxia. J Clin Invest. 1970;49(6):1153–65.
McNicholas WT, Rutherford R, Grossman R, Moldofsky H, Zamel N, Phillipson EA. Abnormal respiratory pattern generation during sleep in patients with autonomic dysfunction. Am Rev Respir Dis. 1983;128(3):429–33.
Guilleminault C, Mondini S, Greenfield M. Abnormal respiratory pattern generation during sleep in patients with autonomic dysfunction. Am Rev Respir Dis. 1984;129(3):512–3.
Bernardi L, Hilz M, Stemper B, Passino C, Welsch G, Axelrod FB. Respiratory and cerebrovascular responses to hypoxia and hypercapnia in familial dysautonomia. Am J Respir Crit Care Med. 2003;167(2):141–9.
Palma JA, Norcliffe-Kaufmann L, Perez MA, Spalink CL, Kaufmann H. Sudden unexpected death during sleep in familial dysautonomia: a case-control study. Sleep. 2017;40(8):zsx083.
Macefield VG, Norcliffe-Kaufmann L, Gutierrez J, Axelrod FB, Kaufmann H. Can loss of muscle spindle afferents explain the ataxic gait in Riley-Day syndrome? Brain. 2011;134(Pt 11):3198–208.
Mendoza-Santiesteban CE, Palma JA, Hedges TR 3rd, Laver NV, Farhat N, Norcliffe-Kaufmann L, et al. Pathological confirmation of optic neuropathy in familial dysautonomia. J Neuropathol Exp Neurol. 2017;76(3):238–44.
Kazachkov M, Palma JA, Norcliffe-Kaufmann L, Bar-Aluma BE, Spalink CL, Barnes EP, et al. Respiratory care in familial dysautonomia: systematic review and expert consensus recommendations. Respir Med. 2018;141:37–46.
Palma JA, Spalink C, Barnes EP, Norcliffe-Kaufmann L, Kaufmann H. Neurogenic dysphagia with undigested macaroni and megaesophagus in familial dysautonomia. Clin Auton Res. 2018;28(1):125–6.
Norcliffe-Kaufmann L, Axelrod F, Kaufmann H. Afferent baroreflex failure in familial dysautonomia. Neurology. 2010;75(21):1904–11.
Norcliffe-Kaufmann L, Palma JA, Kaufmann H. Mother-induced hypertension in familial dysautonomia. Clin Auton Res. 2016;26(1):79–81.
Palma JA, Norcliffe-Kaufmann L, Fuente-Mora C, Percival L, Mendoza-Santiesteban C, Kaufmann H. Current treatments in familial dysautonomia. Expert Opin Pharmacother. 2014;15(18):2653–71.
Goldberg L, Bar-Aluma BE, Krauthammer A, Efrati O, Sharabi Y. Ambulatory blood pressure profiles in familial dysautonomia. Clin Autonom Res. 2018;28(4):385–90.
Del Negro CA, Funk GD, Feldman JL. Breathing matters. Nat Rev Neurosci. 2018;19(6):351–67.
Yang CF, Feldman JL. Efferent projections of excitatory and inhibitory preBotzinger Complex neurons. J Comp Neurol. 2018;526(8):1389–402.
Revill AL, Vann NC, Akins VT, Kottick A, Gray PA, Del Negro CA, et al. Dbx1 precursor cells are a source of inspiratory XII premotoneurons. elife. 2015;4 https://doi.org/10.7554/eLife.12301.
Hoiland RL, Howe CA, Coombs GB, Ainslie PN. Ventilatory and cerebrovascular regulation and integration at high-altitude. Clin Auton Res. 2018;28(4):423–35.
Somers VK, Mark AL, Zavala DC, Abboud FM. Contrasting effects of hypoxia and hypercapnia on ventilation and sympathetic activity in humans. J Appl Physiol. 1989;67(5):2101–6.
Somers VK, Mark AL, Zavala DC, Abboud FM. Influence of ventilation and hypocapnia on sympathetic nerve responses to hypoxia in normal humans. J Appl Physiol (1985). 1989;67(5):2095–100.
Somers VK, Mark AL, Abboud FM. Interaction of baroreceptor and chemoreceptor reflex control of sympathetic nerve activity in normal humans. J Clin Invest. 1991;87(6):1953–7.
Gadoth N, Sokol J, Lavie P. Sleep structure and nocturnal disordered breathing in familial dysautonomia. J Neurol Sci. 1983;60(1):117–25.
Weese-Mayer DE, Kenny AS, Bennett HL, Ramirez JM, Leurgans SE. Familial dysautonomia: frequent, prolonged and severe hypoxemia during wakefulness and sleep. Pediatr Pulmonol. 2008;43(3):251–60.
Singh K, Palma JA, Kaufmann H, Tkachenko N, Norcliffe-Kaufmann L, Spalink C, et al. Prevalence and characteristics of sleep-disordered breathing in familial dysautonomia. Sleep Med. 2018;45:33–8.
Maayan C, Katz E, Begin M, Yuvchev I, Kharasch VS. Laughter is not always funny: breath-holding spells in familial dysautonomia. Clin Pediatr (Phila). 2015;54(2):174–8.
Lacuey N, Zonjy B, Londono L, Lhatoo SD. Amygdala and hippocampus are symptomatogenic zones for central apneic seizures. Neurology. 2017;88(7):701–5.
Chaverra M, George L, Mergy M, Waller H, Kujawa K, Murnion C, et al. The familial dysautonomia disease gene IKBKAP is required in the developing and adult mouse central nervous system. Dis Model Mech. 2017;10(5):605–18.
Cummings KJ. Aspiring to inspire - serotonin, the laryngeal chemoreflex and the sudden infant death syndrome. Exp Physiol. 2016;101(7):790.
Horne RSC. Cardiovascular autonomic dysfunction in sudden infant death syndrome. Clin Auton Res. 2018;28(6):535–43.
Tomson T, Nashef L, Ryvlin P. Sudden unexpected death in epilepsy: current knowledge and future directions. Lancet Neurol. 2008;7(11):1021–31.
Pearson J, Pytel BA, Grover-Johnson N, Axelrod F, Dancis J. Quantitative studies of dorsal root ganglia and neuropathologic observations on spinal cords in familial dysautonomia. J Neurol Sci. 1978;35(1):77–92.
Cohen P, Solomon NH. Familial dysautonomia; case report with autopsy. J Pediatr. 1955;46(6):663–70.
Kaufmann H, Norcliffe-Kaufmann L, Palma JA. Improvement of daytime hypercapnia with nocturnal non-invasive ventilation in familial dysautonomia. Clin Auton Res. 2019;29(2):255–6.
Chobanian AV, Volicer L, Tifft CP, Gavras H, Liang CS, Faxon D. Mineralocorticoid-induced hypertension in patients with orthostatic hypotension. N Engl J Med. 1979;301(2):68–73.
Kjeldsen K. Hypokalemia and sudden cardiac death. Exp Clin Cardiol. 2010;15(4):e96–9.
Trapp S, Aller MI, Wisden W, Gourine AV. A role for TASK-1 (KCNK3) channels in the chemosensory control of breathing. J Neurosci. 2008;28(35):8844–50.
Buckler KJ. TASK channels in arterial chemoreceptors and their role in oxygen and acid sensing. Pflugers Arch. 2015;467(5):1013–25.
Norcliffe-Kaufmann L, Axelrod FB, Kaufmann H. Developmental abnormalities, blood pressure variability and renal disease in Riley Day syndrome. J Hum Hypertens. 2013;27(1):51–5.
Fink AM, Bronas UG, Calik MW. Autonomic regulation during sleep and wakefulness: a review with implications for defining the pathophysiology of neurological disorders. Clin Auton Res. 2018;28(6):509–18.
Chiaro G, Calandra-Buonaura G, Cecere A, Mignani F, Sambati L, Loddo G, et al. REM sleep behavior disorder, autonomic dysfunction and synuclein-related neurodegeneration: where do we stand? Clin Auton Res. 2018;28(6):519–33.
Silvani A. The link between narcolepsy and autonomic cardiovascular dysfunction: a translational perspective. Clin Auton Res. 2018;28(6):545–55.
Palma JA. Autonomic dysfunction in sleep disorders: introduction to the series. Clin Auton Res. 2018;28(6):507–8.
Physiology GC. Mechanosensor of lung inflation identified. Nature. 2017;541(7636):165–6.
Nonomura K, Woo SH, Chang RB, Gillich A, Qiu Z, Francisco AG, et al. Piezo2 senses airway stretch and mediates lung inflation-induced apnoea. Nature. 2017;541(7636):176–81.
Lefcort F, Mergy M, Ohlen SB, Ueki Y, George L. Animal and cellular models of familial dysautonomia. Clin Auton Res. 2017;27(4):235–43.
Heras-Garvin A. Basic research and model systems in familial dysautonomia: what do we know and what’s next? Clin Auton Res. 2017;27(4):211–2.
Conflict of Interests
The authors report no conflict of interests related to this chapter.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2021 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Palma, JA., Kaufmann, H. (2021). Familial Dysautonomia. In: Chokroverty, S., Cortelli, P. (eds) Autonomic Nervous System and Sleep. Springer, Cham. https://doi.org/10.1007/978-3-030-62263-3_26
Download citation
DOI: https://doi.org/10.1007/978-3-030-62263-3_26
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-62262-6
Online ISBN: 978-3-030-62263-3
eBook Packages: MedicineMedicine (R0)