Abstract
Early experience with epicardial imaging during surgical interventions for congenital heart disease (CHD) provided strong evidence that intraoperative echocardiography could guide surgical and anesthetic management in these patients. Since transesophageal echocardiography (TEE) began to be used intraoperatively in the late 1980s, numerous publications have documented its utility in the care of patients with CHD. Subsequent technologic advances—multiplane TEE imaging, the evolution of three-dimensional echocardiography, and the miniaturization of probes—have made it possible to comprehensively assess structural abnormalities, evaluate hemodynamics, and, importantly, appraise surgical results in most CHD patients. Identifying hemodynamically significant residual disease during congenital heart surgery and guiding surgical revision represent major contributions of TEE to perioperative care. Additionally, TEE adds value by providing real-time perioperative assessment of hemodynamics, volume status, and myocardial function. This monitoring helps direct anesthetic care intraoperatively and pharmacologic therapy in the immediate postoperative period. Finally, TEE can guide management planning and help characterize unexpected or unusual postoperative findings or problems.
This chapter provides an overview of the applications of TEE in the intraoperative care of pediatric patients with congenital and acquired heart disease and of adults with CHD, particularly regarding surgical, medical, and anesthetic management. Data on the cost-effectiveness, pitfalls, and limitations of intraoperative TEE are reviewed. Lastly, the role of TEE in the postoperative care of these patients is briefly addressed.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Intraoperative transesophageal echocardiography
- Postoperative transesophageal echocardiography
- TEE technology
- Congenital heart disease
- Adult congenital heart disease
- Monitoring
- Applications
- Limitations
- Pifalls
-
Describe the evolution of intraoperative echocardiography in pediatric and congenital heart disease (CHD)
-
Understand advances in transesophageal echocardiography (TEE) technology over time, particularly regarding applications in infants and children
-
Appreciate the clinical evidence supporting the benefits of TEE in surgical and medical management of children and of all patients with CHD
-
Be familiar with published data assessing the cost-effectiveness of TEE in the pediatric and adult congenital patient population
-
Recognize the limitations and pitfalls of intraoperative TEE, factors that may affect return-to-bypass decisions, and correlation between intraoperative and postoperative echocardiographic findings
-
Understand the applications of TEE in pediatric patients and adults with CHD in the postoperative setting
Introduction
In surgery for congenital heart disease (CHD), intraoperative echocardiography was initially performed using an epicardial approach [1]. However, since then, transesophageal echocardiography (TEE) has become the main imaging technique for both adult and pediatric patients undergoing interventions for congenital or acquired heart disease [2, 3]. Standards have been published for the echocardiographic assessment of children and adults by transesophageal two-dimensional (2D) and three-dimensional (3D) imaging [2,3,4,5].
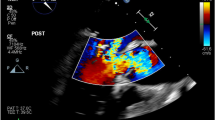
Developments in transducer technology have resulted in an evolution of TEE probes from sector-scanning monoplane (0°), to biplane (0°, 90°) and then multiplane (0°–180°) devices, and most recently to volume-scanning matrix-array probes that have enabled real-time 3D imaging (the latest advancement for this modality) (Fig. 18.1). The addition of more 2D imaging planes with better resolution, along with the evolution of 3D imaging, have advanced the detailed assessment of complex congenital cardiac defects by TEE [3].
Furthermore, all commercially available TEE probes integrate spectral and color flow Doppler capabilities; many offer enhanced imaging modes, such as tissue Doppler and speckle tracking echocardiography, that can better evaluate cardiac function and the severity of cardiac disease. Finally, the miniaturization of multiplane TEE probes for use in neonates and small infants affords a wider safety margin to prevent injury in these patients.
Currently, for the intraoperative assessment of CHD patients, most centers prefer to use multiplane TEE imaging because it enables detailed assessment of anatomy, hemodynamics, and function, with minimal probe manipulation. In children, monoplane or biplane imaging, when the only option available, is an acceptable, although less desirable, alternative to multiplane interrogation. Monoplane and biplane probes are less likely to be available today as many of these devices are deteriorating and may no longer be serviced. Epicardial echocardiography still remains a valuable adjunct to intraoperative TEE and as an alternative imaging approach when TEE is not feasible because of patient size constraints, inability to place the TEE probe, contraindications, or lack of equipment or expertise [6].
Evolution of Intraoperative Echocardiography in CHD
Epicardial Echocardiography
Intraoperative imaging during cardiac surgery was first described in in the early 1970s, initially via the epicardial approach by using M-mode echocardiography [7] and subsequently, 2D imaging was applied [8]. Initial efforts in intraoperative echocardiography in patients with CHD also explored the benefits of epicardial imaging. This involved placing a standard transthoracic imaging probe covered in a sterile sheath to the anterior surface of the heart in order to assess cardiac anatomy and function prior to the initiation and after separation from cardiopulmonary bypass (CPB). This allowed for confirmation of preoperative diagnoses and assessment of the adequacy of the surgical repair [9, 10]. Years of clinical experience supported the benefits of this imaging approach in the perioperative management of patients with CHD [11,12,13,14]. A distinct advantage of epicardial scanning over TEE , when both modalities are available, is that one can better image structures such as the pulmonary arteries, coronary arteries, ventricular outflow tracts, and to some extent the aortic arch by directly placing the imaging probe on them. However, important disadvantages of the epicardial approach relate to limited windows of interrogation, potential for hemodynamic alterations and rhythm abnormalities, risk of infection, and the need for the surgeon to have expertise in cardiovascular imaging. Intraoperative TEE overcomes many of these limitations.
Transesophageal Echocardiography
Early Developments
The first experience in TEE has been attributed to Franzin and colleagues in their publication in 1976 [15]. At the time it was recognized that cardiac imaging through the esophagus could benefit patients with limited transthoracic acoustic windows and this became the driving force for developing an alternate imaging approach. Accordingly, a 9 mm nonfocused 3.5 MHz transducer with M-mode technology was designed. The transducer was placed in a casing with rounded edges and attached to a coaxial cable permitting rotation. A few years later, later, in 1980, Matsumoto and colleagues applied transesophageal M-mode echocardiography to the intraoperative setting for assessment of ventricular function during cardiac surgery [16]. Hisanaga and colleagues from Japan subsequently published their experience after developing a TEE scanning system capable of obtaining cross-sectional images of the heart by using a 2D transducer (10 mm diameter, 2.25 MHz or 3.5 MHz) mounted on a flexible rotational shaft [17]. A year later, Hanrath and colleagues in Germany attached a phased-array ultrasound transducer to the tip of a flexible gastroscope [18] and thereafter the TEE technology gradually evolved.
Monoplane TEE
The clinical applications of real-time 2D TEE and color flow mapping in the immediate and early postoperative evaluation of the results of cardiac surgery were first reported in the 1980s [19]. Early experience in the intraoperative applications of TEE in CHD date back to the late 1980s. Cyran et al. first documented the safe and reliable use of an adult-sized TEE probe in older children and young adults undergoing surgical intervention for various congenital heart defects [20]. Kyo and associates, in conjunction with the Aloka/Corometrics Company in Japan, developed the first TEE probe specifically for infants and young children [21]. Using this monoplane (0°), 26-element, 5.0-MHz, phased-array transducer mounted on a 6.8-mm–diameter flexible gastroscope proved feasible and accurate in assessing small patients with CHD [22,23,24,25,26,27].
Early drawbacks of TEE technology were the suboptimal image quality from a small TEE probe with few elements and the need for probe manipulation to obtain multiple views because scanning was limited to transverse or horizontal planes [28]. Despite these shortcomings, several studies highlighted the benefits and accuracy of intraoperative TEE when compared to epicardial echocardiography in assessing a range of congenital cardiac lesions [29,30,31,32,33,34,35]. Specifically, TEE imaging did not interrupt surgery, distort cardiac structures, trigger dysrhythmias, produce hemodynamic alterations, or increase infection risk. Efforts thus continued into improving TEE technology for pediatric applications.
In the early 1990s, a new monoplane TEE transducer (5.0-MHz, phased-array, 48-element) was introduced that provided higher-resolution images, in addition to continuous-wave Doppler capabilities [36]. Concurrent refinements in Doppler processing improved the assessment of blood-flow velocities, jet direction, and the overall severity of obstructive/regurgitant disease.
Biplane TEE
The development of biplane probes with 48- and 64-element transducers, initially for adults in 1989 and later on suitable for children in the mid-1990s, enhanced the TEE examination by enabling imaging in both the transverse/horizontal (0°) and longitudinal/vertical (90°) planes [37,38,39,40,41]. The additional interrogation plane improved TEE diagnostic accuracy, particularly for disease affecting the ventricular outflow tracts [42].
Regardless of the advantages offered by biplane imaging, TEE still had several limitations. One was that the spectral Doppler angle of interrogation could not be optimally aligned with the direction of blood flow while imaging from the esophageal windows. Fortunately, manipulating existing single and biplane TEE probes in the transgastric and deep transgastric windows provided much more favorable angles for Doppler interrogation of ventricular outflow tracts and great arteries [43, 44].
Multiplane TEE
The initial clinical experience with multiplane TEE imaging in adults was reported in the early 1990s [45,46,47]. Following that, the availability of multiplane TEE imaging for children in the mid 1990s represented a major technological advancement over biplane imaging [48, 49]. The ability to acquire high-resolution images in an unlimited number of planes made possible a more comprehensive appraisal of complex cardiovascular malformations. The first pediatric multiplane probe (i.e., the mini-multiplane probe) was a 48-element, phased-array, single-frequency, 5.0-MHz transducer with a 7-mm shaft and a relatively small transducer tip (10.6 mm wide) that incorporated 2D, M-mode, and full Doppler capabilities [50, 51]. This probe, originally designed by Odelft BV (Delft, The Netherlands), was adapted for use on echocardiographic platforms produced by different manufacturers (refer to Chap. 2) [52].
There has been ongoing interest in further miniaturizing the multiplane TEE probes for use in neonates and small infants to afford a wider margin of safety against injury [53]. An early version, the Odelft neonatal micro-multiplane TEE probe, was a 7.5-MHz, 48-element transducer with an 8-mm–diameter probe tip mounted on a 5-mm gastroscope [54,55,56]. This probe allowed the examination of infants weighing as little as 2.5 kg without major complications. In the initial experience with one of the currently available commercial micro-multiplane TEE probes—the S8-3t (Philips Medical, Andover, MA, USA), a 32-element, phased-array, multifrequency, 3.2- to 7.4-MHz transducer with a 5.2-mm–diameter shaft and a small 7.5 mm wide transducer tip—the rate of successful insertion was high in infants, all of whom weighed at least 1.7 kg [57]. The device allowed high-quality diagnostic imaging without respiratory or hemodynamic compromise.
A prospective study compared the quality of images produced by the micro-multiplane TEE probe versus standard pediatric and adult multiplane TEE probes in 24 exams performed in 23 patients (median weight 11.7 kg, median age 3 years) [58]. The micro-TEE probe provided diagnostic image quality in the neonatal patients. The best image quality for this probe was in patients less than 10 kg; in children weighing 10–30 kg, standard-sized pediatric mini-multiplane TEE probe delivered better imaging.
Intracardiac Catheters
The off-label use of intracardiac echocardiography (ICE) catheters, when inserted through the nasal or oral route for TEE imaging in neonates and small infants, has been reported to provide clinically useful information in some cases. Currently, several of these catheters are commercially available, including the AcuNav Ultrasound Catheter (Siemens Medical Solutions, Malvern, PA, USA), which is a 64-element, phased-array, multifrequency, 5.5 to 10-MHz transducer with a diameter of 3.3 mm. Capabilities such as steering and echocardiographic modes vary among devices. In a series of 22 exams performed with the AcuNav Ultrasound Catheter in 17 infants (weight range 2.1–5.6 kg), most TEE studies were of diagnostic quality and occurred without complications [59]. This miniaturized device is capable of monoplane imaging (90°), as well as spectral and color flow Doppler modalities. The handle controls allow four-way catheter tip articulation with movement in two planes: anterior-posterior and left-right. Ferns et al. compared the micro-multiplane TEE transducer and the AcuNav ICE catheter in terms of efficacy, safety, ease of insertion, capabilities, utilization and cost. Indications for the exams after failed TTE included “examination of aortopulmonary shunt patency; pulmonary venous obstruction; atrial septal defect patency, flow direction and gradient; distal conduit patency; mechanism and severity of valve regurgitation; presence of thrombus or vegetation; presence, size, Doppler blood flow pattern, and pressure gradient of residual ventricular septal defect; residual valve obstruction; ventricular systolic function; and pulmonary hypertension”. The specific clinical information being sought was obtained in all cases regardless of imaging device. The AcuNav transducer was safe and easily inserted through the transnasal route without requiring muscle paralysis, but it provided limited echocardiographic views because of its single longitudinal plane [60]. The micro-TEE transducer was slightly more difficult to insert but had greater echocardiographic capabilities (full multiplanar imaging). The use of the AcuNav was associated with greater costs due to the need for shipping and sterilization, whereas the micro-TEE could be cared for as per the routine laboratory protocol for probe cleaning. In contrast to the AcuNav, the use of the micro-multiplane probe often required more sedation and paralysis. There were no major complications with the use of either transducer.
The principal advantage of the ICE catheter is its slender profile, which allows safe esophageal placement in very small infants. The chief disadvantage is that this catheter uses only a single, longitudinal (90°) imaging plane, which limits its effectiveness in imaging those types of cardiac defects for which additional imaging planes are important. Clearly the ability of the micro-multiplane device to image in multiple planes represents a significant advantage. Another important issue is that the AcuNav device has no thermal sensing, which raises concerns regarding safety. In recognition of all these issues, the micro-multiplane TEE probe is considered the preferred device at most centers for TEE imaging of the small neonate.
Three-Dimensional TEE
The use of a specialized matrix-array TEE probe to display a selected volume of the heart as a real-time 3D dataset was first reported in 2008 [61]. The 3D TEE probe not only has 3D capabilities but also has excellent 2D tomographic imaging as well as spectral/color Doppler, tissue Doppler, speckle tracking, and other features. Also, it allows for several different 2D TEE planes to be displayed simultaneously. The ability to freely rotate the 3D dataset on the ultrasound screen allows for the anatomy to be displayed from any perspective, including the surgical orientation [62,63,64]. This technology replaced previously available 3D probes, which relied on offline reconstruction of sequentially acquired 2D image planes, thus limiting the use of 3D TEE in the operating room.
At present, 3D echocardiography should be considered to complement, rather than replace, 2D imaging for the assessment of CHD. It should be utilized whenever feasible, although there is wide institutional variability in its use [4]. Currently, 3D TEE echocardiography is recommended for assessing specific congenital heart lesions (atrioventricular valve abnormalities, septal defects, aortic valve and left ventricular (LV) outflow tract disease, and complex abnormalities of cardiac connections), valvular regurgitation location and severity, and ventricular parameters [65,66,67,68,69]. As with most other forms of echocardiography, 3D TEE has yet to be tested in randomized controlled trials examining procedural success and TEE-related morbidity. However, 3D TEE has already been adopted into clinical practice to meet the need for more accurate diagnostic information; this is based upon the extremely favorable clinical experience and data from nonrandomized studies to date, as discussed later in this chapter and further detailed in Chaps. 23 an 24.
TEE Probe Selection
A variety of TEE probes are currently available for clinical use (Fig. 18.2). In pediatric patients, TEE probe selection relies primarily on two factors: patient weight and probe size. Vendors have suggested a minimum patient weight for the safe use of each of the probes in the pediatric age group as listed in Table 18.1. However, in clinical practice, probes are used extensively in infants and children below the recommended minimum weight [3, 70]. The risk-benefit ratio of using a particular TEE probe should be evaluated on a case-by-case basis, but the use of a probe size outside of the vendor recommendations may be safe when the probe is placed with minimal resistance. When possible in children weighing >25 kg (2D) or > 30 kg (3D), the adult TEE probes should be favored as they usually provide better image quality and, in the case of the 3D TEE probe, allows for the enhanced imaging mode.
Multiplane TEE Imaging Probes. The photograph displays four commercially available multiplane TEE devices. (a) Neonatal micro-multiplane probe, (b) pediatric mini-multiplane probe, (c) two-dimensional ‘adult’ or standard probe, (d) three-dimensional ‘adult’ probe. Source: From, Andropoulos DB, Stayer SA, Mossad EB, Miller-Hance WC. Anesthesia for Congenital Heart Disease, 3rd Ed. New Jersey: 2015; John Wiley and Sons; with kind permission of John Wiley and Sons
Although monoplane and biplane TEE probes are no longer supported or available at most centers, they may still be used in some countries. Accordingly, these are included in Table 18.1 as a reference and for comparison with more contemporary hardware. Also note that the dimensions listed and other details included in this table represent average values. The reader is referred to Chap. 2, and in particular to Table 2.1, for detailed information regarding individual manufacturers and currently available TEE probes. The slight differences in probe dimensions between these two Tables (2.1 and 18.1) can be accounted for by the more general nature of the data presented here.
Role of Intraoperative Echocardiography
An extensive experience over many years supports the utility of intraoperative echocardiography in the care of pediatric patients with congenital and acquired heart disease, as well as in adults with CHD [71,72,73]. Intraoperative imaging provides detailed anatomic and hemodynamic information before the planned surgical procedure, assesses the adequacy of the repair, and permits real-time monitoring of ventricular loading and performance (Table 18.2). Numerous reports of early and current TEE experience during surgery document the value of this imaging modality as a diagnostic tool and an aid to surgical decision-making [12, 26, 28, 29, 32, 33, 35, 36, 39, 41, 42, 74,75,76,77,78,79,80,81,82,83,84,85,86].
Impact on Surgical Management
Intraoperative echocardiography, whether epicardial, transesophageal, or both, can alter the surgical plan in ~1–13% of cases (Table 18.3) [83, 87,88,89,90,91,92,93,94]. The surgical alteration rate, although in some cases may be accounted by imperfect surgical planning, is an important benefit of TEE. Although the results of the preoperative examination may not alter the surgical plan, they do help to identify the optimal interrogation planes and provide baseline images for later comparison during the post-repair assessment. This accounts for the preferred approach at many centers to not only limit the TEE examination to the postoperative evaluation, but also perform preoperative imaging. The contemporary experience among institutions that routinely use intraoperative imaging during congenital heart surgery suggests a return-to-CPB rate of 3–7%. Even more compelling is the observation that failure to address significant residual disease can lead to morbidity and, in some cases, perioperative mortality in these patients [91,92,93,94,95].
Studies of intraoperative TEE have focused primarily on two of its potential applications: indicating when the preoperative surgical plan needs to be revised, and determining postoperatively whether immediate revision of the procedure is necessary. In an early series reported by Ungerleider et al. of 1000 patients treated at Duke University Medical Center between 1987 and 1994, an epicardial approach was initially used; in later cases, TEE was used instead of or in addition to epicardial imaging [87]. There was a 4.4% incidence of return to CPB for surgical revisions based on the echocardiographic findings. Most patients underwent a successful revision of the residual defect, defined as the elimination or amelioration of the defect. The value of intraoperative echocardiography was apparent even in this early report, in which the authors state that “it was not possible for the surgeon to predict the need for a revision based on his confidence of the repair.”
A retrospective review of the first 341 intraoperative studies performed at Texas Children’s Hospital from 1990 to 1995 indicated that the prebypass TEE altered the planned surgical procedure in 9.4% of cases [83]. Diagnostic categories in which TEE had the most impact on surgical procedures included ventricular septal defect associated with double-chambered right ventricle or subaortic membrane, isolated subaortic stenosis, atrioventricular valve dysfunction, single ventricle, and pulmonary atresia with ventricular septal defect. More often, however, TEE detected minor diagnostic findings that did not influence the surgical plan (but that may have informed subsequent care), as noted in 13.2% of the cohort. The postbypass TEE findings indicated the need for immediate reoperation in 8.2% of patients.
Randolph and colleagues at the Mayo Clinic studied the use of TEE during congenital heart surgery in patients of every age, from neonate to elderly, to define the impact on patient care and to determine the appropriate indications for intraoperative TEE in such patients [89]. In 13.8% of cases, TEE provided either unique prebypass information that led to changes in the planned surgical procedure (9.1%) or postbypass information that prompted immediate revision of hemodynamically significant defects (5.6%). Such TEE findings occurred most often in younger patients, during reoperations, and in those undergoing valve repairs and complex outflow tract reconstructions.
Yumoto and Katsuya at Nagoya University in Japan prospectively evaluated the utility of TEE as a diagnostic tool during cardiac surgery in children [90]. According to postoperative TEE findings, the surgical repair was judged inadequate in 2 out of 88 cases (3%), prompting the reinstitution of bypass and revision of the repair.
Sloth et al. in Denmark described their use of TEE in 532 consecutive children treated during a 5-year period, with TEE findings leading to return to CPB for reoperation in approximately 3% of patients [88]. Bettex et al. from Switzerland, in a two-center observational study among 865 patients less than 17 years old, found that TEE altered surgical management in 12.7% of cases, with return to CPB in 7.3% and changed medical management in 19.4% during the intraoperative period [91]. Ma et al. at the Paediatric Heart Center in Shanghai examined the utility of perioperative TEE in 350 children with CHD [92]. Preoperative TEE contributed additional findings or changed the diagnosis in 9.4% of patients, and these findings modified the planned surgical procedure in 6.6% of the study group. Residual problems or sequelae were detected by postoperative TEE in 16.3% of the cohort, resulting in 3.7% of patients undergoing immediate intervention or return to bypass for revision. More recent reports show fewer changes in the operative plan with alteration of the surgical plan based on preoperative TEE of less than 2%, but still a significant number of reinterventions with ~4–5% of patients requiring reinitiation of CPB [93, 94].
Several isolated case reports describe additional uses of intraoperative TEE in children. These include detecting cannulation complications during CPB, guiding the resection of cardiac tumors, evaluating pulmonary artery flow after the Fontan procedure, and identifying pericardial and pleural effusions and guiding their drainage [96,97,98,99,100,101].
In addition to being useful during CPB cases, TEE reportedly has benefits when used during other interventions such as video-assisted thoracoscopic procedures for CHD [102,103,104,105]. Furthermore, TEE is indispensable for guiding the placement of devices such as septal occluders or stents via the perventricular or direct approach in the operating room during hybrid procedures performed by the cardiothoracic surgeon and interventional cardiologist [106, 107].
Formal, rigorous scientific data regarding the impact of intraoperative TEE on clinical outcomes are lacking in children with congenital or acquired heart disease and in adults with CHD. Nonetheless, the cumulative experience from the above-mentioned studies and from others indicates that intraoperative TEE can improve the quality of the surgical intervention in these patients. Thus, intraoperative TEE represents the most common application of TEE in these patient groups. As such, TEE has become the standard of care in most centers that specialize in treating children and adults with CHD, in agreement with the indications outlined by various clinical practice guidelines [2, 3, 108,109,110,111,112,113,114].
Impact on Medical Management
As with surgical care, the literature also documents the value of TEE in guiding medical management and other aspects of perioperative care during surgery for congenital and other cardiovascular diseases in pediatric patients. The overall data, although limited, support the extended role of intraoperative TEE as a monitoring adjunct to facilitate anesthetic care, hemodynamic and pharmacologic management, medical decision-making, and selecting treatment strategies. Moreover, this imaging approach assists in the formulation of care plans during the immediate postoperative period by enabling, for example, the selection of suitable inotropic and vasoactive agents according to the echocardiographic findings after chest closure.
Guiding Catheter Placement
Central venous catheterization is an important aspect of perioperative care, providing for vascular access, blood sampling, and hemodynamic monitoring. TEE can facilitate percutaneous central venous catheter (CVC) placement by imaging the guidewire position before the insertion of a larger-bore catheter. This can avoid repeated attempts at cannulation and the resultant complications, particularly in young patients [115, 116].
Several reports describe the use of TEE in optimally placing the CVC tip in adults and children undergoing cardiovascular interventions [117,118,119]. A prospective randomized controlled clinical trial performed in 145 patients (age range, 1 day to 29 years) during cardiac surgery for CHD examined the usefulness of TEE in guiding proper depth of CVC insertion and confirming superior vena cava (SVC) cannulation [120]. Patients were randomly assigned to a TEE-guided catheter-placement group or to a control group in which the catheter was placed before the TEE probe was inserted. Correct CVC placement was defined as a catheter tip visible in the SVC at or above the SVC–right atrial junction and parallel to the SVC wall. This was determined by both preoperative TEE and chest radiography (CXR). The study showed than when TEE was used to guide CVC placement, the percentage of catheters correctly positioned was significantly higher than when anatomic landmarks were used (TEE serving as the end-point for correct tip position). However, when a CXR was used to determine catheter position, there was no difference between the groups in the rate of correct catheter placement. In spite of the lack of superiority of TEE to correctly position the catheter tip as compared to conventional techniques when CXR was used as the end-point, which according to the authors could be most likely explained by the different imaging modalities, the study suggested that TEE could guide CVC placement in congenital heart surgery.
Placing transthoracic intracardiac catheters is often necessary for hemodynamic monitoring in infants and children undergoing cardiac surgery [121, 122]. Anecdotal evidence suggests that TEE can verify the appropriate position of these catheters. The usefulness of intraoperative TEE has also been demonstrated for the placement and optimal positioning of circulatory support hardware (aortic and venous cannulae, mechanical support devices) and pulmonary artery catheters (refer to Chap. 20) [123].
Identifying Intracardiac Air and Confirming Cardiac Deairing
In contrast to blood, air bubbles within the heart and vasculature produce bright reflections on echocardiography, due to the unique acoustic properties of air (Chap. 1). Retained intracardiac air may account for significant morbidity during cardiac surgery, negatively affecting clinical outcomes. Air embolization to the coronary circulation may have immediate or late effects that can lead to myocardial dysfunction. This dysfunction, in turn, can prolong CPB time and require interventions such as institution or adjustment of inotropic support or other therapies [124, 125]. Other serious complications include those related to the presence of air in the systemic circulation—particularly the cerebral vasculature, with consequent neurologic injury [126, 127]. During congenital heart surgery, which frequently requires cardiotomy, TEE helps to ensure the adequacy of cardiac deairing before CPB is discontinued [128,129,130,131,132,133,134,135,136].
In patients undergoing repair of congenital heart defects, Greeley et al. described intramyocardial air as the presence of air within the wall of a myocardial segment supplied by a coronary artery branch, suggesting air embolization of this vessel [137]. The implications of this finding are that it could lead to regional wall motion abnormalities (RWMA), ventricular dysfunction, dysrhythmias, and hemodynamic instability during and after weaning from CPB. Identifying intramyocardial air by intraoperative TEE can help prevent hemodynamic instability by providing an opportunity to develop specific management strategies to eliminate the air.
TEE can also detect intracardiac air in beating-heart procedures performed without aortic cross-clamping, such as interventions in the right heart (e.g., RV to pulmonary artery conduit replacement), left heart (e.g., inflow cannula insertion during ventricular assist device placement), or single-ventricle palliation (e.g., RV graft placement during the Sano modification of the Norwood procedure). The concern during these interventions is the potential risk for paradoxical air embolization. In the case of right-heart surgery in patients with a biventricular circulation, air can be entrained into the left heart (left atrium or LV) across an intracardiac (interatrial or interventricular) communication. In other instances, air can be entrained directly into the left heart or single ventricle. In either case, air can enter the systemic circulation and potentially cause severe complications from air embolism to other organs.
Thus, for patients with a biventricular circulation who are undergoing right-sided beating-heart surgical interventions, it is useful to exclude intracardiac communications by TEE using all available modalities, including color flow Doppler and contrast echocardiography. Using a contrast agent, such as agitated saline or albumin, in combination with a simulated Valsalva maneuver in mechanically ventilated patients, facilitates the detection of intracardiac communications by revealing right-to-left intracardiac shunting. Although the reliability of contrast TEE in detecting intracardiac communications in patients with CHD has been questioned, continuous monitoring for intracardiac air during all beating-heart procedures may enhance patient safety [138].
Assessing Ventricular Loading Conditions
Manipulating ventricular preload is key to optimizing cardiac performance and is a major focus of hemodynamic management during cardiac surgery. Estimating ventricular filling in clinical practice is difficult and often requires obtaining various measurements by invasive and noninvasive techniques [139,140,141]. Echocardiography only permits the indirect measurement of pressures by Doppler methods. Methods of estimating ventricular preload from TEE data mostly focus on quantifying LV filling by examining echocardiographic indices such as LV end-diastolic area, volume, or both [142,143,144].
Quantitative measures of LV volume can be obtained from 2D echocardiography by the Simpson method of summation of discs and tracing the endocardial border from an end-diastolic frame. Three-dimensional echocardiography using semiautomated software that tracks the endocardium throughout the cardiac cycle can reliably measure LV volume [145, 146]. Although this technique has been used with TEE, its use with transthoracic echocardiography (TTE) has been more thoroughly validated and produces a more accurate assessment of LV volumes, particularly for the highly variable geometry of structurally abnormal hearts encountered in CHD [147,148,149,150]. Intraoperative real-time 3D TEE assessment of LV volume is feasible in adults undergoing cardiac surgery [151, 152]. Although initially cumbersome and time-consuming, innovations in recent years have led to advancements in software automation facilitating this evaluation. It should be recognized that all echocardiographic measures of LV volume, whether by 2D or 3D, underestimate the volume compared with angiography and magnetic resonance imaging (MRI), and commonly used LV function measurements are load dependent [153,154,155].
Measuring ventricular areas and volumes is time-consuming in most cases, and can represent a potential distraction from patient care. This makes performing such measurements impractical in the operating room, until such time that accurate and rapidly automated techniques become more widely available. More often, qualitatively assessing low intravascular volume by echocardiography involves visualizing surrogate indicators such as a small LV end-diastolic cavity area with mid-cavitary obliteration in the transgastric midpapillary short-axis view (TG Mid Pap SAX; transducer angle ~0°–20°). Hypovolemia, vasodilation, severe aortic regurgitation, severe mitral regurgitation, and a ventricular septal defect can all manifest the same ejection pattern in this view. Low preload and low afterload are distinguished by the end-diastolic area; a small area during both end-diastole and end-systole suggests low preload. Conversely, a small LV end-systolic area with a normal area in end-diastole is more consistent with a low afterload pattern. In both cases, the LV may exhibit hyperdynamic systolic function.
Several studies have compared or correlated LV preload assessment by TEE with measurements of filling pressures. In one study, TEE provided a more sensitive method of detecting hypovolemia than traditional hemodynamic parameters of ventricular preload, such as central venous pressure and pulmonary capillary wedge pressure [156].
Data are limited regarding TEE-guided manipulations of ventricular preload in young patients with CHD. In a small number of pediatric patients weighing 3–15 kg who were undergoing elective repair of various congenital heart defects, Reich et al. attempted to determine whether TEE could identify alterations in cardiac filling resulting from manipulations of blood volume [157]. Changes in LV end-diastolic and end-systolic areas in the TG Mid Pap SAX view and hemodynamic data were assessed during several interventions after sternal closure. Measurements obtained at baseline, on phlebotomy, and after the reinfusion of blood showed that decreases in blood volume as small as 5–8% were associated with a reduction in LV end-diastolic area, as well as central venous and systemic arterial pressures. Thus, both qualitative and quantitative measurements documented changes in LV filling, thereby validating TEE as a useful monitor of cardiac preload in children.
Assessing Systolic Left Ventricular Function
Echocardiography allows qualitative and quantitative measurement of ventricular systolic function and contractility (for an in-depth discussion on the subject, refer to Chap. 5) (Fig. 18.3). Qualitative assessment of LV systolic function by TEE requires multiple imaging planes but relies primarily on the TG Mid Pap SAX view. Each of the six LV wall segments is examined for motion and thickening during systole, which can be suggestive of global or regional wall abnormalities. Normal systolic ventricular wall motion consists of inward motion with wall thickening of 50% from baseline. Each segment that shows abnormal LV wall motion during systole is graded as follows: (1) hypokinetic—the segment has less thickening and moves inward, (2) akinetic—the segment does not thicken or move, or (3) dyskinetic—the segment moves paradoxically during systole and does not thicken [68].
Evaluation of Left Ventricular Function by Echocardiography. Left ventricular function can be assessed using different techniques as displayed in the graphic. (a) Shortening fraction estimates systolic function using linear measurements of end-diastolic (EDD) and end-systolic (ESD) left ventricular (LV) chamber dimensions from a TG Mid Pap SAX view. (b) Fractional area change measures end-diastolic and end-systolic LV chamber areas from a TG Mid Pap SAX view. (c) Simpson’s method of discs uses ME four and two-chamber views to trace the endocardium at end-diastole (ED) and end-systole (ES). Integrated machine software divides the LV into slices to calculate the volume. (d) Tissue Doppler imaging of the lateral mitral valve annulus demonstrates a systolic velocity (S’) and two opposite directed velocities, in early diastole (E’) and late diastole (A’) (graphic representation from a DTG window). The S’ wave velocity provides an estimate of LV ejection fraction. IC isovolumetric contraction, IR isovolumetric relaxation. (e) Myocardial performance index (MPI) is measured using spectral Doppler of the aortic outflow and mitral inflow as described in this chapter (also refer to Chap. 5). AVV atrioventricular valve, ET ejection time, ICT isovolumic contraction time, IRT isovolumic relaxation time. (f) Strain and strain rate can be easily measured using speckle tracking (shown here for a ME LAX view) and peak longitudinal systolic strain displayed in a bull’s eye format. (g) Three-dimensional assessment of an endocardial cast derived from a 3D dataset can be analyzed to estimate LV volumes and ejection fraction. Source for (a–c, e and g): From, Vegas A. Perioperative Two-Dimensional Transesophageal Echocardiography: A Practical Handbook, 2nd Ed. New York: Springer; 2018; with kind permission of Springer Science and Business Media
Quantitative assessment of LV systolic function includes estimating stroke volume (SV) and ejection fraction (EF) [68, 158]. Both are commonly determined by using 2D echocardiography by the method of discs technique, which involves tracing the end-diastolic and end-systolic ventricular areas in a two-chamber or four-chamber view [159]. This technique is time-consuming and requires making assumptions about chamber shape, uniform global myocardial function, and loading conditions [151]. As described above, 3D echocardiography using semiautomated or more advanced software with tracking of the endocardium throughout the cardiac cycle can measure LV volume and EF. Newer imaging modalities such as tissue Doppler imaging, speckle tracking, and real-time 3D echocardiography (RT-3DE) have improved the assessment of LV systolic function [68]. Although the technology continues to evolve, the 3D assessment of cardiac chamber quantification continues to be time-consuming and as previously noted, not practical in the intraoperative setting.
Simple linear and area measures can be used as indices of LV systolic performance but should not be confused with measurements of EF. Fractional area change (FAC), for example, is a calculated index from area measurements:
The areas from which FAC is calculated are measured by tracing the LV endocardial border at end-diastole (ECG R wave) and end-systole (smallest cross-sectional area) from the midesophageal long-axis view (ME LAX; transducer angle ~120°–140°) or TG Mid Pap SAX cross-section. However, it is important to remember that FAC is not equivalent to EF, which is a volume measurement. Instead, FAC serves as another method for estimating ventricular systolic function.
In pediatric and adult patients, RT-3DE is feasible for volumetric analysis of the abnormal LV, allowing for accurate determination of volume and EF and being comparable to MRI measurements [145,146,147, 149, 150]. Evidence suggests that in patients with CHD, 3DE measures LV volume and function more accurately and reproducibly than 2D methods. Lu et al. reported that M-mode, 2D, and RT-3DE measurements all correlated well with MRI measurements, but the correlation was strongest for RT-3DE [146]. M-mode provides the most efficient assessment of LV indices, but the measurements are less accurate and reproducible than those made with 2D and 3D echocardiography. M-mode measurements are rarely performed in the intraoperative setting. Three-dimensional echocardiography using automated analysis is superior to M-mode and 2D echocardiography for measuring LV indices. Therefore, RT-3DE using the automated algorithm is the method of choice for obtaining LV indices, assuming 3D hardware and relevant software.
The myocardial performance index (MPI ; also known as the Tei index), a Doppler-derived parameter, has been used as a measure of global ventricular function (refer to Chap. 5). The index incorporates both systolic and diastolic time intervals and has been considered to reflect both, systolic and diastolic performance [160]. The MPI is defined as the sum of isovolumic contraction time (ICT) and isovolumic relaxation time (IRT) divided by ejection time (ET):
The longer the isovolumic times, the higher the MPI and the worse the ventricular performance.
The index can be measured for either the LV or RV from pulsed-wave Doppler interrogation of the respective AV valve and outflow tract or derived using tissue Doppler. For either ventricle, the sum of the ICT and IRT is derived from the Doppler interval between cessation and onset of flow across the respective atrioventricular valve (from end of the A wave to the beginning of the E wave) minus the ET. Studies have established normal values for both adults and children. The MPI index has been applied to the assessment of LV and RV function in patients with CHD, as well as in the evaluation of complex ventricular geometries [161,162,163]. It has also been used in the intraoperative setting to compare the cardiovascular effects of anesthetic agents in children with CHD [164]. Although there was initial enthusiasm for the MPI as a diagnostic and prognostic marker of various clinical conditions, recent studies have raised concerns regarding the reliability of this parameter when used for assessment of ventricular function [165]. There are also reservations regarding the use of this index in the setting of changing loading conditions [166].
Assessing Systolic Right Ventricular Function
There is increasing recognition that right ventricular (RV) systolic function has prognostic significance in various disease processes, including CHD [167,168,169]. This is especially relevant in those patients whose RV is the sole systemic ventricular chamber [170]. The current gold standard for noninvasive measurement of RV function is cardiac MRI, although echocardiography remains the most frequently used modality for evaluating the RV because of its readily and widespread availability. The complex shape and peristaltic motion of the RV makes its function more difficult to quantify than that of the LV, so RV assessment is frequently qualitative, often requiring multiple echocardiographic views [171]. Published echocardiographic guidelines for evaluating the RV have aided in standardizing practice [172]. Three-dimensional echocardiography can accurately estimate RV volume, but as in the case of the LV, this is also time-consuming and requires offline processing of an adequate 3D dataset [173,174,175,176,177,178,179]. Three-dimensional TEE assessments of RV volumes and function have shown excellent correlation with 3D TTE in patients with normal-sized and dilated RVs [180]. Advances in 3D automation may soon allow for improved efficiency and reproducibility in RV chamber quantification. When applied in conjunction with TEE, this promises to overcome the challenges posed by the limited time available to perform 3D RV analysis with the currently available methods.
Echocardiographic assessment of the RV begins with comparing the relative sizes of the ventricles. The normal RV is shaped differently than the LV. It appears triangular in long-axis (LAX) views and crescent-shaped in short-axis (SAX) views. The best correlation of measured RV volumes between 2D TTE and TEE has been obtained by using maximal SAX dimension and RV area measured in the midesophageal four-chamber view (ME 4-Ch). The recommended measurements for assessing RV size by 2D TTE include end-diastolic diameters measured at the basal and mid-cavity levels, end-diastolic length, and end-diastolic and end-systolic planimetered areas in apical four-chamber views. Qualitative rather than quantitative assessment of RV function is based on endocardial wall thickening and motion. Quantitative RV indices include FAC, tricuspid annular plane systolic excursion (TAPSE), and the myocardial performance index. It is important to remember that RV shape changes with pressure or volume overload, and this shape change must be accounted for when assessing RV function.
Assessing Diastolic Ventricular Function
There is increasing interest in the routine echocardiographic evaluation of diastolic function in both pediatric and adult patients, because abnormalities of ventricular relaxation and compliance are known to contribute to perioperative morbidity [181,182,183,184,185,186]. Such evaluations have relied heavily on the use of Doppler modalities, particularly spectral analysis, to examine LV filling alterations that may correlate with diastolic function (refer to Chap. 5).
Diastolic dysfunction plays a major role in many congenital and acquired disorders in the pediatric age group [187,188,189,190,191,192]. Unfortunately, there are several obstacles to evaluating diastolic function in young patients, including the many confounding variables that can interfere with Doppler assessment and interpretation of findings. Applying criteria developed for TTE to the TEE approach further magnifies these difficulties [193]. Thus, the use of TEE to assess diastolic function in children with CHD remains of limited utility and an important area of ongoing investigation [194,195,196,197].
Detecting Myocardial Ischemia
TEE is a sensitive tool for detecting and monitoring myocardial ischemia. Myocardial ischemia affects both global and regional systolic function. In detecting intraoperative ischemia, TEE findings suggestive of compromised coronary perfusion are more sensitive than ECG-detected ST-segment changes [198] or elevations of pulmonary capillary wedge pressure [199]. Therefore, the qualitative assessment of RWMA by TEE is widely used in the perioperative care of patients at risk for compromised coronary blood flow during cardiac or noncardiac surgery [200].
Although limited data are available, a few investigations have described the use of TEE to detect myocardial ischemia in children undergoing interventions that involve manipulating the coronary arteries [201]. Rouine-Rapp et al. prospectively studied neonates undergoing an arterial switch operation for transposition of the great arteries to determine whether RWMA, as identified by intraoperative TEE, indicated myocardial ischemia [202]. This investigation found that when multiple RWMA areas were present, the regional wall dysfunction persisted at the time of chest closure. Relative to those with normal wall motion after surgical repair, infants with RWMA had more postoperative ischemic events as indicated by Holter monitoring (ST-segment changes) and elevated cardiac troponin I levels, confirming the correlation between TEE-detected RWMA and myocardial ischemia. In more recent work, intraoperative coronary Doppler patterns obtained by TEE plus epicardial echocardiography have also been associated with clinical outcomes after the arterial switch operation [203, 204].
These observations validate the usefulness of TEE in the early diagnosis of compromised myocardial blood flow and support the perioperative use of this modality in infants and children at elevated risk of myocardial ischemia or infarction during congenital heart surgery. It is likely that this application would also benefit pediatric patients undergoing interventions for acquired cardiovascular disease and adults with CHD who may have comorbidities that affect coronary blood flow.
Impact on Anesthetic and Hemodynamic Management
An extensive literature supports the role of TEE in clinical decision-making in adult patients. Several studies have also demonstrated the benefits of TEE regarding hemodynamic monitoring and modifications of medical management in pediatric patients with congenital and acquired cardiovascular disease, as well as adults with CHD. These reports include experiences worldwide.
Specific changes in anesthetic management triggered by TEE may include, for example, the alternate selection of technique or drugs with a lesser impact on parameters such as myocardial function or systemic vascular tone, administration of intravenous fluid to optimize ventricular preload, initiation of inotropic agents as needed in the presence of myocardial dysfunction, and administration of vasopressors in hypotensive states associated with adequate ventricular volume and contractility.
Two previously mentioned studies, both of which included a large number of patients, evaluated the monitoring value of intraoperative TEE and the resulting changes in medical care [88, 91]. In one of these studies, Sloth et al. from Denmark collected data from 532 consecutive children who underwent heart surgery during a 5-year period [88]. Among these patients, TEE identified new information in 45%, and in 8% (43 out of 532), this information was instrumental in directing or changing medical management. The most frequent interventions were changes in inotropic strategy related to ventricular dysfunction and volume replacement. In the second study, Bettex et al. analyzed data from 865 intraoperative examinations performed at two specialized congenital heart surgery centers [91]. TEE assisted medical management in 19.4% of cases, leading to changes that optimized ventricular filling and pharmacologic therapy.
Cost-Effectiveness of Intraoperative TEE
The early experience with using epicardial imaging during congenital heart surgery not only showed its benefits for surgical management but also suggested that these benefits justified the costs involved [1]. Ungerleider and coworkers reported that the costs of performing intraoperative studies were offset by the savings in operating room time and, in some cases, the prevention of suboptimal results necessitating reoperation [10]. In a subsequent report, a more formal cost-benefit analysis showed that hospital costs were higher for patients who required a reoperation than for patients who underwent immediate revision prompted by echocardiographic findings [87]. These findings provide clear and compelling evidence of the financial benefits of intraoperative echocardiography.
Other studies have also examined the issue of cost-effectiveness of intraoperative TEE. Relatively early in the experience of intraoperative TEE, Benson and Cahalan performed a cost-benefit analysis involving various types of cardiac surgical patients, including those with CHD [205]. From published data regarding the effectiveness of TEE in identifying residual defects that required immediate revision during interventions for CHD in infants and children, their analysis showed a definite financial patient benefit per TEE study performed. In fact, among patients undergoing cardiac surgery, those with CHD derived the greatest overall financial benefit. Their analysis indicated that the financial gain associated with TEE was substantial, frequently outweighing the costs of repeat surgery.
Siwik et al. examined the costs and resources required in performing routine TEE services as an adjunct to congenital heart surgery in a case-controlled analysis of 63 children undergoing elective, complex intracardiac repairs [206]. This study concluded that the routine use of TEE in these children was cost-effective because it did not significantly increase echocardiography costs in the combined operative and postoperative periods. There was a trend toward fewer echocardiographic studies in the TEE group, suggesting that the routine use of TEE reduced the need for additional postoperative studies in the intensive care unit (ICU). This cost benefit was independent of any impact of TEE on clinical outcomes. No patient in this cohort required return to CPB, and surgical therapy was altered by TEE findings in 3% of patients. Complications from TEE were rare and self-limited, and they often occurred during probe placement or manipulation in smaller patients.
Randolph et al., in a large study of the value of TEE, estimated that an intraoperative TEE service would pay for itself, even without considering any benefits derived from the preoperative examination [89]. A retrospective review by Bettex et al. of 580 TEE studies performed over a period of 10 years in patients younger than 17 years (mean age 35 months) examined the cost-effectiveness of routine intraoperative TEE in pediatric cardiac surgery [207]. Thirty-three patients required reinitiation of CPB according to TEE findings. The study proposed a savings of $690 to $2190 per patient, based on conservative calculations assuming the cost of reoperation and complications related to a residual defect. This calculation probably underestimated the true cost-effectiveness of routine intraoperative TEE; a meta-analysis by Levin et al. showed that the cost-savings per TEE ranged from $194 to $4910, with a mean of $1930 [208].
In summary, although the number of formal investigations of this issue is relatively small, all published work to date has demonstrated substantial cost benefit from the use of TEE during congenital heart surgery, particularly in the pediatric population.
Limitations and Pitfalls of Intraoperative TEE
Despite ubiquitous and beneficial use, TEE has important limitations [209]. Whereas TTE involves transducer interrogation through different chest wall locations, allowing a comprehensive examination of cardiovascular structures, the gastroesophageal region restricts TEE transducer location, limiting the information that can be obtained in some cases. The confinement of the TEE probe can result in poor image quality, limited imaging windows, and suboptimal Doppler angle alignment in some patients. It is difficult to image by TEE far-field anterior structures and those obscured by the air-filled tracheobronchial tree, such as the distal left pulmonary artery, the transverse aortic arch, and the distal ascending aorta [2, 210, 211]. In addition, it might not be feasible to image vascular structures within the thorax, such as the upper SVC, innominate vein, and anomalous systemic and pulmonary veins. Therefore, epicardial echocardiography can complement TEE to visualize these structures [212]. Other potential challenges of intraoperative TEE are interpreting on-screen images under bright operating room lights, time constraints, and clinical conditions that may limit the ability to perform a comprehensive examination.
Potential pitfalls of TEE include failure to recognize important information and misinterpretation of data, leading to erroneous diagnoses. It is well-known that factors such as the immediate post-bypass catecholamine state, loading conditions, and myocardial function can interfere with the interpretation of echocardiographic findings, causing the imager to underestimate or overestimate the hemodynamic severity of the patient’s condition. The optimal conditions for hemodynamic assessment in most postoperative patients are those that reflect an equilibrium or steady state. The continuously changing nature of respiratory, hemodynamic, pharmacologic, and anesthesia-related interventions makes it challenging, if not nearly impossible, to accurately assess a patient’s hemodynamic status in the operating room. Thus, the findings from the intraoperative TEE should be interpreted in this context.
Return to Cardiopulmonary Bypass Decisions
Decisions regarding return to CPB are complex. They should not rely solely on TEE findings but should also integrate clinical information, level of inotropic support, hemodynamic data, and, very importantly, the risk-benefit ratio of a reintervention. In most cases, this decision involves clinical judgment based not only on the echocardiographic findings but also on factors such as the likelihood of obtaining an adequate or better result balanced against the risk of potential morbidity related to additional surgery, CPB, and myocardial ischemic time. In some situations, echocardiographic findings can predict the early need for reoperation, suggesting that revising the surgical procedure will be beneficial [213,214,215,216,217].
A report by Kausal et al. highlights some of the difficulties regarding return-to-CPB decisions [218]. This group explored the question of whether significant intraoperative right ventricular outflow tract (RVOT) gradients after tetralogy of Fallot repair represented an indication for revision in 166 patients (median age 7 years). “Significant” RVOT obstruction (gradient >40 mmHg, RV-to-LV pressure ratio > 85%) occurred in 35% of patients after the intervention. Only 12% of these patients had fixed RVOT obstruction, which required immediate surgical revision; the remaining 88% of patients had dynamic RVOT obstruction, which was not judged to require surgical reintervention. Interestingly, irrespective of the severity of the obstruction detected intraoperatively, outflow gradients declined sharply on follow-up (mean 18.5 months after surgery). No reoperations or late deaths were reported. The authors indicated that intraoperative echocardiography was helpful in distinguishing fixed from dynamic obstruction, thereby obviating needless revisions. They also concluded that in this patient group, dynamic RVOT gradients declined significantly irrespective of their initial severity. The implication of this study is that gradients by themselves, regardless of their severity, cannot be used in isolation to judge the need for surgical revision.
One of the major applications of intraoperative TEE is in the evaluation of residual intracardiac shunting after repair of ventricular septal defects (VSD) and assessment of the potential need to return to bypass. The finding of residual ventricular-level shunting can present a clinical dilemma in some cases regarding its hemodynamic significance and need for reoperation. A few studies have addressed this issue by examining frequency, significance, and implications of residual VSDs detected intraoperatively. Yang et al. noted a prevalence of residual shunting in a third of patients undergoing VSD closure (96 out of 294) [219]. However, most defects were insignificant, in fact, two-thirds closed by hospital discharge. The study suggested that a residual VSD that measures ≥4 mm or a shunt greater than 1.5:1 should be considered for immediate reoperation while a 3 mm defect requires additional information to determine hemodynamic significance. A retrospective review by Hanna et al. investigated the predictive value of the diagnosis of a residual VSD identified by intraoperative TEE in 690 patients who were followed longitudinally [215]. In their study, the detection of a residual shunt in the operating room was also a fairly common finding, occurring in 37% of the cohort. In the majority of cases, however, the defect was trivial and resolved spontaneously. The study found that the detection of a residual shunt at the site of the repair carried an overall positive predictive value of only 15% in the long term and noted that most residual defects need surgical intervention only rarely. These two studies provide data regarding the eventual course of residual shunts detected intraoperatively after VSD closure and support the clinical impression of the infrequent need to return to bypass in most cases.
Correlation of Intraoperative and Postoperative Echocardiographic Findings
Few data show a correlation between intraoperative and postoperative echocardiographic information, and some literature in fact points to disagreement in some cases [220, 221]. It is not altogether surprising that a discrepancy might exist between intraoperative and postoperative echocardiographic findings. As noted above, changing hemodynamic conditions in the operating room likely affect clinical findings, particularly assessments of valvar stenosis and regurgitation. Moreover, the quality of echocardiographic imaging can differ substantially between the intraoperative TEE and postoperative TTE studies. Finally, changes can occasionally occur in a surgical repair, even within a few days postoperatively, and these might also affect its echocardiographic appearance.
Lee et al. examined the validity of intraoperative TEE in predicting the severity of mitral regurgitation (MR) at follow-up in patients after complete repair of atrioventricular septal defects [220]. The MR severity was quantified as the ratio of the maximum MR jet area by color flow Doppler imaging to the left atrial area on 2D imaging, using biplane TEE after weaning from CPB but before chest closure. A discrepancy in the MR grade occurred in 47% of patients, with the majority having a higher MR grade on follow-up. This suggested that the MR grade as assessed by TEE immediately after surgery may not predict the degree of regurgitation at follow-up.
Honjo et al. evaluated 42 consecutive children who underwent valve repairs and identified significant discrepancies (disagreement in 64%) between the intraoperative TEE and postoperative TTE findings before hospital discharge [221]. In most cases, residual atrioventricular valve regurgitation was underestimated in the operating room, whereas there was reasonable agreement between intraoperative and postoperative estimates of aortic valve regurgitation.
A retrospective study aimed to examine the routine practice of predischage TTE after congenital heart surgery found that abnormal findings on this examination were very common (51%; 265 out of the 462 patients) [222]. The findings included valve regurgitation, hemodynamic obstruction, ventricular dysfunction, unintended shunt, or pericardial effusion. In some patients, the abnormalities were of greater than mild severity and were associated with adverse clinical events. When the results of intraoperative TEE at the conclusion of surgery were compared with TTE findings prior to hospital discharge, only fair to moderate concordance was identified. These results underscore the fact that postoperative TTE is often necessary, and rarely should intraoperative TEE be the only echocardiographic study obtained after surgery.
TEE for Evaluation in the Postoperative Setting
The role of TEE in the cardiac critical care unit and other postoperative settings has been extensively documented at many centers (refer to Chap. 19 for in depth discussion) [223,224,225,226,227,228,229,230,231]. The use of TEE in critically ill patients is more common in adults. Since children generally have more favorable transthoracic windows, adequate information can often be obtained by standard TTE. However, in postoperative pediatric patients, the superior resolution of TEE can facilitate morphologic and functional assessment when TTE is suboptimal because of lung interference, an open sternum, or the presence of bandages [232, 233].
Mechanical circulatory support in the pediatric age group has received increasing attention in recent years as size-appropriate hardware has become available. Applying existing technologies and novel devices can help address circulatory failure in patients with CHD and other disorders. The use of TEE in the operating room, critical care unit, or both facilitates care of these patients by aiding cannula and device positioning, assessing cardiac chamber decompression, evaluating ventricular loading conditions, and quantifying recovery of myocardial function (refer to Chap. 20) [234,235,236]. In addition, TEE can help optimize pharmacologic and other medical therapies and provide information regarding a patient’s readiness for weaning from support.
Although several investigations have documented the value of TEE in assessing cardiac output and systemic vascular resistance in critically ill adult patients, these types of assessments have not yet been validated in children [237, 238].
After congenital cardiac surgery, TEE can assist in the further characterization of unexpected or unusual findings or abnormalities that were suspected but not adequately defined by TTE. A subset of patients with an unanticipated or complicated immediate postoperative course may require further diagnostic evaluation; in some cases, the diagnostic capabilities of TEE can obviate the need for alternative, and sometimes more invasive, imaging studies [239].
The American College of Cardiology Foundation and the American Society of Echocardiography, in combination with key specialty and subspecialty societies, published an appropriateness review for the use of echocardiography in 2007 [240]. The report was subsequently updated in 2011 [241]. The writing groups rated clinical indications in adults (age 18 years or older) in both inpatient and outpatient clinical settings. These publications were based on the general assumption that TEE is used primarily as an adjunct or subsequent test to TTE, but indications for TEE as an initial or supplemental study were also considered. Intraoperative applications were not addressed by the writing group. With respect to postoperative indications for TEE, those generally considered appropriate by both, the working group and in recently published pediatric and congenital TEE guidelines, are listed in Table 18.4 [3, 242].
Data regarding the applications of TEE in children in the immediate postoperative period are quite limited, and indications comparable to those in the adult patient have not yet been clearly defined. Nonetheless, many situations are analogous to those encountered in adults, and the clinical experience suggests that TEE, when used in a judicious and appropriate manner, can provide real and important benefits in the postoperative and critical care settings (refer to Chap. 19).
Summary
The overwhelming contributions of TEE have led to this imaging tool becoming the standard of care for intraoperative assessment of most congenital heart repairs and surgical interventions for pediatric acquired heart disease at many centers. Extensive experience has documented a substantial overall impact on surgical decision-making and significant applications that include surgical planning, evaluating the intervention, and guiding surgical revision as necessary. Contributions to anesthetic care include real-time monitoring of ventricular filling and myocardial performance, ensuring adequate cardiac deairing, and optimizing hemodynamic management strategies. Intraoperative TEE assists in the formulation and optimization of plans for postoperative care and provides important postoperative information. Although it has not been formally assessed in a rigorous scientific manner, the experience regarding the intraoperative and postoperative contributions of TEE is compelling enough to conclude that this technology has a substantial positive impact on clinical outcome in pediatric patients and adults with CHD.
Questions and Answers
-
1.
All of the following devices allow imaging of the heart in transverse or horizontal planes EXCEPT
-
a.
Biplane TEE probe
-
b.
3D TEE Probe
-
c.
Micro-multiplane TEE probe
-
d.
Intracardiac catheter (ICE) when used via the transesophageal approach
-
e.
Monoplane TEE probe
-
a.
Answer: d
Explanation: All standard TEE imaging probes allow imaging in the transverse (horizontal or 0°) plane except for the ICE catheter, which incorporates a single longitudinal (vertical or 90°) imaging plane.
-
2.
Among adults with CHD, which of the following is considered one of the most frequent indications for TEE imaging
-
a.
Evaluating suspected intracardiac thrombus when TTE is nondiagnostic
-
b.
Routine evaluation of an asymptomatic patient with corrected ventricular septal defect who is lost to follow-up
-
c.
Evaluating native or prosthetic valve in a patient with transient fever
-
d.
Evaluating a patient with atrial flutter when anticoagulation is planned and cardioversion is being deferred
-
e.
Yearly evaluation of pulmonary regurgitation in an obese patient after tetralogy of Fallot repair
-
a.
Answer: a
Explanation: Among non perioperative indications, evaluating suspected intracardiac thrombus when TTE is nondiagnostic in the adult patient represents one of the most frequent indications for the use of the technology. Although TEE might be appropriate in certain adult patients with the other conditions listed, these in general represent less likely indications.
-
3.
All of the following statements with respect to three-dimensional TEE imaging are true EXCEPT
-
a.
Using the technology requires additional expertise over 2D imaging
-
b.
Probes capable of 3D imaging incorporate all features available in 2D imaging devices
-
c.
3D should replace 2D imaging in evaluating complex congenital heart disease
-
d.
3D TEE can be used to assess LV volume
-
e.
Measurements of LV volume are load dependent
-
a.
Answer: c
Explanation: 3D imaging should complement, rather than replace, 2D imaging in the assessment of CHD.
-
4.
Which of the following statements best describes the intraoperative TEE assessment of LV function
-
a.
Current technology allows expeditious quantitative evaluation
-
b.
Fractional area change can be equated to EF
-
c.
2D measurements of EF have the same accuracy and reproducibility as 3D methods
-
d.
Ejection fraction implies a volume measurement
-
e.
M-mode assessment of LV indices is as accurate as 2D and 3D echocardiography
-
a.
Answer: d
Explanation: Ejection fraction determinations rely on volumetric assessments. Although FAC serves as a method to estimate LV function, the parameter is derived from measurements of area, not volume, unlike EF. Current technology for the quantitative evaluation of LV systolic function is time-consuming; thus, in the intraoperative setting, functional assessment tends to be qualitative. In patients with CHD, 3D echocardiography provides better accuracy and reproducibility than 2D methods in measuring LV volume and function. M-mode is currently rarely use in the intraoperative setting and is the least accurate and reproducible technique compared with 2D and 3D imaging.
-
5.
Useful applications of TEE in perioperative management include
-
a.
Ensuring cardiac deairing before the aortic cross-clamp is removed
-
b.
Confirming the preoperative diagnosis
-
c.
Selecting appropriate inotropes and vasoactive drugs
-
d.
Excluding residual hemodynamically significant intracardiac shunts
-
e.
All of the above
-
a.
Answer: e
Explanation: TEE has been shown to be beneficial in all listed applications.
Abbreviations
- CHD:
-
Congenital heart disease
- CPB:
-
Cardiopulmonary bypass
- CVC:
-
Central venous catheter
- EF:
-
Ejection fraction
- FAC:
-
Fractional area change
- ICE:
-
Intracardiac echocardiography
- ICU:
-
Intensive care unit
- LAX:
-
Long-axis
- LV:
-
Left ventricle
- ME:
-
Midesophageal
- MR:
-
Mitral regurgitation
- MRI:
-
Magnetic resonance imaging
- RV:
-
Right ventricle, right ventricular
- RVOT:
-
Right ventricular outflow tract
- RWMA:
-
Regional wall motion abnormalities
- SAX:
-
Short-axis
- SV:
-
Stroke volume
- SVC:
-
Superior vena cava
- TEE:
-
Transesophageal echocardiography
- TG:
-
Transgastric
- TTE:
-
Transthoracic echocardiography
References
Gussenhoven EJ, van Herwerden LA, Roelandt J, Ligtvoet KM, Bos E, Witsenburg M. Intraoperative two-dimensional echocardiography in congenital heart disease. J Am Coll Cardiol. 1987;9:565–72.
Hahn RT, Abraham T, Adams MS, et al. Guidelines for performing a comprehensive transesophageal echocardiographic examination: recommendations from the American Society of Echocardiography and the Society of Cardiovascular Anesthesiologists. J Am Soc Echocardiogr. 2013;26:921–64.
Puchalski MD, Lui GK, Miller-Hance WC, et al. Guidelines for performing a comprehensive transesophageal echocardiographic examination in children and all patients with congenital heart disease: recommendations from the American Society of Echocardiography. J Am Soc Echocardiogr. 2019;32:173–215.
Simpson J, Lopez L, Acar P, et al. Three-dimensional echocardiography in congenital heart disease: an expert consensus document from the European Association of Cardiovascular Imaging and the American Society of Echocardiography. J Am Soc Echocardiogr. 2017;30:1–27.
Mitchell C, Rahko PS, Blauwet LA, et al. Guidelines for performing a comprehensive transthoracic echocardiographic examination in adults: recommendations from the American Society of Echocardiography. J Am Soc Echocardiogr. 2019;32:1–64.
Ozturk E, Cansaran Tanidir I, Ayyildiz P, et al. The role of intraoperative epicardial echocardiography in pediatric cardiac surgery. Echocardiography. 2018;35:999–1004.
Johnson ML, Holmes JH, Spangler RD, Paton BC. Usefulness of echocardiography in patients undergoing mitral valve surgery. J Thorac Cardiovasc Surg. 1972;64:922–34.
Spotnitz HM. Two-dimensional ultrasound and cardiac operations. J Thorac Cardiovasc Surg. 1982;83:43–51.
Ungerleider RM, Kisslo JA, Greeley WJ, Van Trigt P, Sabiston DC. Intraoperative prebypass and postbypass epicardial color flow imaging in the repair of atrioventricular septal defects. J Thorac Cardiovasc Surg. 1989;98:90–9.
Ungerleider RM, Greeley WJ, Sheikh KH, et al. Routine use of intraoperative epicardial echocardiography and Doppler color flow imaging to guide and evaluate repair of congenital heart lesions. A prospective study. J Thorac Cardiovasc Surg. 1990;100:297–309.
Ungerleider R. Decision making in pediatric cardiac surgery using intraoperative echo. Int J Card Imaging. 1989;4:33–5.
Hsu YH, Santulli T, Wong AL, Drinkwater D, Laks H, Williams RG. Impact of intraoperative echocardiography on surgical management of congenital heart disease. Am J Cardiol. 1991;67:1279–83.
Ungerleider RM. The use of intraoperative epicardial echocardiography with color flow imaging during the repair of complete atrioventricular septal defects. Cardiol Young. 1992;2:56–64.
Papagiannis J, Kanter RJ, Armstrong BE, Greeley WJ, Ungerleider RM. Intraoperative epicardial echocardiography during repair of tetralogy of Fallot. J Am Soc Echocardiogr. 1993;6:366–73.
Frazin L, Talano JV, Stephanides L, Loeb HS, Kopel L, Gunnar RM. Esophageal echocardiography. Circulation. 1976;54:102–8.
Matsumoto M, Oka Y, Strom J, et al. Application of transesophageal echocardiography to continuous intraoperative monitoring of left ventricular performance. Am J Cardiol. 1980;46:95–105.
Hisanaga K, Hisanaga A, Nagata K, Ichie Y. Transesophageal cross-sectional echocardiography. Am Heart J. 1980;100:605–9.
Hanrath P, Kremer P, Langenstein BA, Matsumoto M, Bleifeld W. [Transesophageal echocardiography. A new method for dynamic ventricle function analysis]. Dtsch Med Wochenschr 1981;106:523–525.
Kyo S, Takamoto S, Matsumura M, et al. Immediate and early postoperative evaluation of results of cardiac surgery by transesophageal two-dimensional Doppler echocardiography. Circulation. 1987;76:V113–21.
Cyran SE, Kimball TR, Meyer RA, et al. Efficacy of intraoperative transesophageal echocardiography in children with congenital heart disease. Am J Cardiol. 1989;63:594–8.
Kyo S, Koike K, Takanawa E, et al. Impact of transesophageal Doppler echocardiography on pediatric cardiac surgery. Int J Card Imaging. 1989;4:41–2.
Ritter SB, Thys D. Pediatric transesophageal color flow imaging: smaller probes for smaller hearts. Echocardiography. 1989;6:431–40.
Ritter SB, Hillel Z, Narang J, Lewis D, Thys D. Transesophageal real-time Doppler flow imaging in congenital heart disease: experience with a new pediatric transducer probe. Dyn Cardiovasc Imaging. 1989;2:92–6.
Ritter SB. Transesophageal echocardiography in children: new peephole to the heart. J Am Coll Cardiol. 1990;16:447–50.
Ritter SB. Pediatric transesophageal color flow imaging 1990: the long and short of it. Echocardiography. 1990;7:713–25.
Stümper OF, Elzenga NJ, Hess J, Sutherland GR. Transesophageal echocardiography in children with congenital heart disease: an initial experience. J Am Coll Cardiol. 1990;16:433–41.
Ritter SB. Transesophageal real-time echocardiography in infants and children with congenital heart disease. J Am Coll Cardiol. 1991;18:569–80.
Roberson DA, Muhiudeen IA, Silverman NH. Transesophageal echocardiography in pediatrics: technique and limitations. Echocardiography. 1990;7:699–712.
Muhiudeen IA, Roberson DA, Silverman NH, Haas G, Turley K, Cahalan MK. Intraoperative echocardiography in infants and children with congenital cardiac shunt lesions: transesophageal versus epicardial echocardiography. J Am Coll Cardiol. 1990;16:1687–95.
Stümper O, Kaulitz R, Sreeram N, et al. Intraoperative transesophageal versus epicardial ultrasound in surgery for congenital heart disease. J Am Soc Echocardiogr. 1990;3:392–401.
Sreeram N, Stümper OF, Kaulitz R, Hess J, Roelandt JR, Sutherland GR. Comparative value of transthoracic and transesophageal echocardiography in the assessment of congenital abnormalities of the atrioventricular junction. J Am Coll Cardiol. 1990;16:1205–14.
Roberson DA, Muhiudeen IA, Cahalan MK, Silverman NH, Haas G, Turley K. Intraoperative transesophageal echocardiography of ventricular septal defect. Echocardiography. 1991;8:687–97.
Roberson DA, Muhiudeen IA, Silverman NH, Turley K, Haas GS, Cahalan MK. Intraoperative transesophageal echocardiography of atrioventricular septal defect. J Am Coll Cardiol. 1991;18:537–45.
Wienecke M, Fyfe DA, Kline CH, et al. Comparison of intraoperative transesophageal echocardiography to epicardial imaging in children undergoing ventricular septal defect repair. J Am Soc Echocardiogr. 1991;4:607–14.
Muhiudeen IA, Roberson DA, Silverman NH, Haas GS, Turley K, Cahalan MK. Intraoperative echocardiography for evaluation of congenital heart defects in infants and children. Anesthesiology. 1992;76:165–72.
Muhiudeen I, Silverman N. Intraoperative transesophageal echocardiography using high resolution imaging in infants and children with congenital heart disease. Echocardiography. 1993;10:599–608.
Omoto R, Kyo S, Matsumura M, et al. Bi-plane color transesophageal Doppler echocardiography (color TEE): its advantages and limitations. Int J Card Imaging. 1989;4:57–8.
Seward JB, Khandheria BK, Edwards WD, Oh JK, Freeman WK, Tajik AJ. Biplanar transesophageal echocardiography: anatomic correlations, image orientation, and clinical applications. Mayo Clin Proc. 1990;65:1193–213.
Gentles TL, Rosenfeld HM, Sanders SP, Laussen PC, Burke RP, van der Velde ME. Pediatric biplane transesophageal echocardiography: preliminary experience. Am Heart J. 1994;128:1225–33.
Lam J, Neirotti RA, Lubbers WJ, et al. Usefulness of biplane transesophageal echocardiography in neonates, infants and children with congenital heart disease. Am J Cardiol. 1993;72:699–706.
O’Leary PW, Hagler DJ, Seward JB, et al. Biplane intraoperative transesophageal echocardiography in congenital heart disease. Mayo Clin Proc. 1995;70:317–26.
Xu J, Shiota T, Ge S, et al. Intraoperative transesophageal echocardiography using high-resolution biplane 7.5 MHz probes with continuous-wave Doppler capability in infants and children with tetralogy of Fallot. Am J Cardiol. 1996;77:539–42.
Hoffman P, Stümper O, Rydelwska-Sadowska W, Sutherland GR. Transgastric imaging: a valuable addition to the assessment of congenital heart disease by transverse plane transesophageal echocardiography. J Am Soc Echocardiogr. 1993;6:35–44.
Muhiudeen IA, Silverman NH, Anderson RH. Transesophageal transgastric echocardiography in infants and children: the subcostal view equivalent. J Am Soc Echocardiogr. 1995;8:231–44.
Flachskampf FA, Hoffmann R, Verlande M, Schneider W, Ameling W, Hanrath P. Initial experience with a multiplane transoesophageal echo-transducer: assessment of diagnostic potential. Eur Heart J. 1992;13:1201–6.
Roelandt JR, Thomson IR, Vletter WB, Brommersma P, Bom N, Linker DT. Multiplane transesophageal echocardiography: latest evolution in an imaging revolution. J Am Soc Echocardiogr. 1992;5:361–7.
Seward JB, Khandheria BK, Freeman WK, et al. Multiplane transesophageal echocardiography: image orientation, examination technique, anatomic correlations, and clinical applications. Mayo Clin Proc. 1993;68:523–51.
Tardif JC, Schwartz SL, Vannan MA, Cao QL, Pandian NG. Clinical usefulness of multiplane transesophageal echocardiography: comparison to biplanar imaging. Am Heart J. 1994;128:156–66.
Yvorchuk KY, Sochowski RA, Chan KL. A prospective comparison of the multiplane probe with the biplane probe in structure visualization and Doppler examination during transesophageal echocardiography. J Am Soc Echocardiogr. 1995;8:111–20.
Cromme-Dijkhuis AH, Djoa KK, Bom N, Hess J. Pediatric transesophageal echocardiography by means of a miniature 5-MHz multiplane transducer. Echocardiography. 1996;13:685–9.
Djoa KK, De Jong N, Cromme-Dijkhuis AH, Lancée CT, Bom N. Two decades of transesophageal phased array probes. Ultrasound Med Biol. 1996;22:1–9.
Sloth E, Hasenkam JM, Sørensen KE, et al. Pediatric multiplane transesophageal echocardiography in congenital heart disease: new possibilities with a miniaturized probe. J Am Soc Echocardiogr. 1996;9:622–8.
Lam J, Neirotti RA, Hardjowijono R, Blom-Muilwijk CM, Schuller JL, Visser CA. Transesophageal echocardiography with the use of a four-millimeter probe. J Am Soc Echocardiogr. 1997;10:499–504.
Shiota T, Lewandowski R, Piel JE, et al. Micromultiplane transesophageal echocardiographic probe for intraoperative study of congenital heart disease repair in neonates, infants, children, and adults. Am J Cardiol. 1999;83:292–5.
Rice MJ, Sahn DJ. Transesophageal echocardiography for congenital heart disease--who, what, and when. Mayo Clin Proc. 1995;70:401–2.
Scohy TV, Gommers D, Jan ten Harkel AD, Deryck Y, McGhie J, Bogers AJ. Intraoperative evaluation of micromultiplane transesophageal echocardiographic probe in surgery for congenital heart disease. Eur J Echocardiogr. 2007;8:241–6.
Zyblewski SC, Shirali GS, Forbus GA, et al. Initial experience with a miniaturized multiplane transesophageal probe in small infants undergoing cardiac operations. Ann Thorac Surg. 2010;89:1990–4.
Pushparajah K, Miller OI, Rawlins D, Barlow A, Nugent K, Simpson JM. Clinical application of a micro multiplane transoesophageal probe in congenital cardiac disease. Cardiol Young. 2012;22:170–7.
Bruce CJ, O’Leary P, Hagler DJ, Seward JB, Cabalka AK. Miniaturized transesophageal echocardiography in newborn infants. J Am Soc Echocardiogr. 2002;15:791–7.
Ferns S, Komarlu R, Van Bergen A, Multani K, Cui VW, Roberson DA. Transesophageal echocardiography in critically ill acute postoperative infants: comparison of AcuNav intracardiac echocardiographic and microTEE miniaturized transducers. J Am Soc Echocardiogr. 2012;25:874–81.
Sugeng L, Shernan SK, Salgo IS, et al. Live 3-dimensional transesophageal echocardiography initial experience using the fully-sampled matrix array probe. J Am Coll Cardiol. 2008;52:446–9.
Vegas A, Meineri M. Core review: three-dimensional transesophageal echocardiography is a major advance for intraoperative clinical management of patients undergoing cardiac surgery: a core review. Anesth Analg. 2010;110:1548–73.
Lang RM, Badano LP, Tsang W, et al. EAE/ASE recommendations for image acquisition and display using three-dimensional echocardiography. J Am Soc Echocardiogr. 2012;25:3–46.
Simpson J, Miller O, Bell A, Bellsham-Revell H, McGhie J, Meijboom F. Image orientation for three-dimensional echocardiography of congenital heart disease. Int J Cardiovasc Imaging. 2012;28:743–53.
Faletra FF, Nucifora G, Ho SY. Real-time 3-dimensional transesophageal echocardiography of the atrioventricular septal defect. Circ Cardiovasc Imaging. 2011;4:e7–9.
Cossor W, Cui VW, Roberson DA. Three-dimensional echocardiographic en face views of ventricular septal defects: feasibility, accuracy, imaging protocols and reference image collection. J Am Soc Echocardiogr. 2015;28:1020–9.
Silvestry FE, Cohen MS, Armsby LB, et al. Guidelines for the echocardiographic assessment of atrial septal defect and patent foramen ovale: from the American Society of Echocardiography and Society for Cardiac Angiography and Interventions. J Am Soc Echocardiogr. 2015;28:910–58.
Lang RM, Badano LP, Mor-Avi V, et al. Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr. 2015;28:1–39.e14.
Zoghbi WA, Adams D, Bonow RO, et al. Recommendations for noninvasive evaluation of native valvular regurgitation: a report from the American Society of Echocardiography developed in collaboration with the Society for Cardiovascular Magnetic Resonance. J Am Soc Echocardiogr. 2017;30:303–71.
Toole BJ, Slesnick TC, Kreeger J, et al. The miniaturized multiplane micro-transesophageal echocardiographic probe: a comparative evaluation of its accuracy and image quality. J Am Soc Echocardiogr. 2015;28:802–7.
Miller-Hance WC, Silverman NH. Transesophageal echocardiography (TEE) in congenital heart disease with focus on the adult. Cardiol Clin. 2000;18:861–92.
Russell IA, Rouine-Rapp K, Stratmann G, Miller-Hance WC. Congenital heart disease in the adult: a review with internet-accessible transesophageal echocardiographic images. Anesth Analg. 2006;102:694–723.
Kamra K, Russell I, Miller-Hance WC. Role of transesophageal echocardiography in the management of pediatric patients with congenital heart disease. Paediatr Anaesth. 2011;21:479–93.
Stümper O, Fraser AG, Elzenga N, et al. Assessment of ventricular septal defect closure by intraoperative epicardial ultrasound. J Am Coll Cardiol. 1990;16:1672–9.
Fyfe DA, Kline CH, Sade RM, Greene CA, Gillette PC. The utility of transesophageal echocardiography during and after Fontan operations in small children. Am Heart J. 1991;122:1403–15.
Fyfe DA, Kline CH. Transesophageal echocardiography for congenital heart disease. Echocardiography. 1991;8:573–86.
Lam J, Neirotti RA, Nijveld A, Schuller JL, Blom-Muilwijk CM, Visser CA. Transesophageal echocardiography in pediatric patients: preliminary results. J Am Soc Echocardiogr. 1991;4:43–50.
Stumper O. Transesophageal echocardiography: a new diagnostic method in paediatric cardiology. Arch Dis Child. 1991;66:1175–7.
Stümper O, Kaulitz R, Elzenga NJ, et al. The value of transesophageal echocardiography in children with congenital heart disease. J Am Soc Echocardiogr. 1991;4:164–76.
Tee SD, Shiota T, Weintraub R, et al. Evaluation of ventricular septal defect by transesophageal echocardiography: intraoperative assessment. Am Heart J. 1994;127:585–92.
Shuler CO, Fyfe DA, Sade R, Crawford FA. Transesophageal echocardiographic evaluation of cor triatriatum in children. Am Heart J. 1995;129:507–10.
Stevenson JG. Role of intraoperative transesophageal echocardiography during repair of congenital cardiac defects. Acta Paediatr Suppl. 1995;410:23–33.
Bezold LI, Pignatelli R, Altman CA, et al. Intraoperative transesophageal echocardiography in congenital heart surgery. The Texas Children’s Hospital experience. Tex Heart Inst J. 1996;23:108–15.
Bengur AR, Li JS, Herlong JR, Jaggers J, Sanders SP, Ungerleider RM. Intraoperative transesophageal echocardiography in congenital heart disease. Semin Thorac Cardiovasc Surg. 1998;10:255–64.
Kavanaugh-McHugh A, Tobias JD, Doyle T, Heitmiller ES, Meagher C. Transesophageal echocardiography in pediatric congenital heart disease. Cardiol Rev. 2000;8:288–306.
Lim DS, Dent JM, Gutgesell HP, Matherne GP, Kron IL. Transesophageal echocardiographic guidance for surgical repair of aortic insufficiency in congenital heart disease. J Am Soc Echocardiogr. 2007;20:1080–5.
Ungerleider RM, Kisslo JA, Greeley WJ, et al. Intraoperative echocardiography during congenital heart operations: experience from 1,000 cases. Ann Thorac Surg. 1995;60:S539–42.
Sloth E, Pedersen J, Olsen KH, Wanscher M, Hansen OK, Sørensen KE. Transoesophageal echocardiographic monitoring during paediatric cardiac surgery: obtainable information and feasibility in 532 children. Paediatr Anaesth. 2001;11:657–62.
Randolph GR, Hagler DJ, Connolly HM, et al. Intraoperative transesophageal echocardiography during surgery for congenital heart defects. J Thorac Cardiovasc Surg. 2002;124:1176–82.
Yumoto M, Katsuya H. Transesophageal echocardiography for cardiac surgery in children. J Cardiothorac Vasc Anesth. 2002;16:587–91.
Bettex DA, Schmidlin D, Bernath MA, et al. Intraoperative transesophageal echocardiography in pediatric congenital cardiac surgery: a two-center observational study. Anesth Analg. 2003;97:1275–82.
Ma XJ, Huang GY, Liang XC, et al. Transoesophageal echocardiography in monitoring, guiding, and evaluating surgical repair of congenital cardiac malformations in children. Cardiol Young. 2007;17:301–6.
Guzeltas A, Ozyilmaz I, Tanidir C, et al. The significance of transesophageal echocardiography in assessing congenital heart disease: our experience. Congenit Heart Dis. 2014;9:300–6.
Jijeh AM, Omran AS, Najm HK, Abu-Sulaiman RM. Role of intraoperative transesophageal echocardiography in pediatric cardiac surgery. J Saudi Heart Assoc. 2016;28:89–94.
Stevenson JG, Sorensen GK, Gartman DM, Hall DG, Rittenhouse EA. Transesophageal echocardiography during repair of congenital cardiac defects: identification of residual problems necessitating reoperation. J Am Soc Echocardiogr. 1993;6:356–65.
Komai H, Naito Y, Fujiwara K, Uemura S. The benefits of surgical atrial septostomy guided by transesophageal echocardiography in pediatric patients. J Thorac Cardiovasc Surg. 1999;118:758–9.
Kawahito S, Kitahata H, Tanaka K, et al. Intraoperative management of a pediatric patient undergoing cardiac tumor resection with the aid of transesophageal and epicardial echocardiography. Anesth Analg. 1999;88:1048–50.
Kawahito S, Kitahata H, Tanaka K, Nozaki J, Oshita S. Intraoperative evaluation of pulmonary artery flow during the Fontan procedure by transesophageal Doppler echocardiography. Anesth Analg. 2000;91:1375–80.
Chen TH, Chan KC, Cheng YJ, Wang MJ, Tsai SK. Bedside pericardiocentesis under the guidance of transesophageal echocardiography in a 13-month-old boy. J Formos Med Assoc. 2001;100:620–2.
Boddu K, Vavilala MS, Stevenson JG, Lam AM. The use of transesophageal echocardiography to facilitate removal of a thoracic nail. Anesth Analg. 2002;95:624–6.
Nitta K, Kawahito S, Kitahata H, Nozaki J, Katayama T, Oshita S. Two unusual complications associated with cardiopulmonary bypass for pediatric cardiac surgery detected by transesophageal echocardiography after decannulation. Paediatr Anaesth. 2008;18:325–9.
Lavoie J, Burrows FA, Gentles TL, Sanders SP, Burke RP, Javorski JJ. Transoesophageal echocardiography detects residual ductal flow during video-assisted thoracoscopic patent ductus arteriosus interruption. Can J Anaesth. 1994;41:310–3.
Lavoie J, Javorski JJ, Donahue K, Sanders SP, Burke RP, Burrows FA. Detection of residual flow by transesophageal echocardiography during video-assisted thoracoscopic patent ductus arteriosus interruption. Anesth Analg. 1995;80:1071–5.
Ho AC, Tan PP, Yang MW, et al. The use of multiplane transesophageal echocardiography to evaluate residual patent ductus arteriosus during video-assisted thoracoscopy in adults. Surg Endosc. 1999;13:975–9.
Ho AC, Chen CK, Yang MW, Chu JJ, Lin PJ. Usefulness of intraoperative transesophageal echocardiography in the assessment of surgical repair of pediatric ventricular septal defects with video-assisted endoscopic techniques in children. Chang Gung Med J. 2004;27:646–53.
Bacha EA, Cao QL, Galantowicz ME, et al. Multicenter experience with perventricular device closure of muscular ventricular septal defects. Pediatr Cardiol. 2005;26:169–75.
Gan C, An Q, Lin K, et al. Perventricular device closure of ventricular septal defects: six months results in 30 young children. Ann Thorac Surg. 2008;86:142–6.
Fyfe DA, Ritter SB, Snider AR, et al. Guidelines for transesophageal echocardiography in children. J Am Soc Echocardiogr. 1992;5:640–4.
Practice guidelines for perioperative transesophageal echocardiography. A report by the American Society of Anesthesiologists and the Society of Cardiovascular Anesthesiologists Task Force on Transesophageal Echocardiography. Anesthesiology. 1996;84:986–1006.
Cheitlin MD, Alpert JS, Armstrong WF, et al. ACC/AHA guidelines for the clinical application of echocardiography. A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee on Clinical Application of Echocardiography). Developed in collaboration with the American Society of Echocardiography. Circulation. 1997;95:1686–744.
Cheitlin MD, Armstrong WF, Aurigemma GP, et al. ACC/AHA/ASE 2003 Guideline update for the clinical application of echocardiography: summary article: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (ACC/AHA/ASE Committee to Update the 1997 Guidelines for the Clinical Application of Echocardiography). Circulation. 2003;108:1146–62.
Stevenson JG. Utilization of intraoperative transesophageal echocardiography during repair of congenital cardiac defects: a survey of North American centers. Clin Cardiol. 2003;26:132–4.
Ayres NA, Miller-Hance W, Fyfe DA, et al. Indications and guidelines for performance of transesophageal echocardiography in the patient with pediatric acquired or congenital heart disease: report from the task force of the Pediatric Council of the American Society of Echocardiography. J Am Soc Echocardiogr. 2005;18:91–8.
American Society of Anesthesiologists and Society of Cardiovascular Anesthesiologists Task Force on Transesophageal Echocardiography. Practice guidelines for perioperative transesophageal echocardiography. An updated report by the American Society of Anesthesiologists and the Society of Cardiovascular Anesthesiologists Task Force on Transesophageal Echocardiography. Anesthesiology. 2010;112:1084–96.
Sawchuk C, Fayad A. Confirmation of internal jugular guide wire position utilizing transesophageal echocardiography. Can J Anaesth. 2001;48:688–90.
Mahmood F, Sundar S, Khabbaz K. Misplacement of a guidewire diagnosed by transesophageal echocardiography. J Cardiothorac Vasc Anesth. 2007;21:420–1.
Andropoulos DB. Transesophageal echocardiography as a guide to central venous catheter placement in pediatric patients undergoing cardiac surgery. J Cardiothorac Vasc Anesth. 1999;13:320–1.
Chaney MA, Minhaj MM, Patel K, Muzic D. Transoesophageal echocardiography and central line insertion. Ann Card Anaesth. 2007;10:127–31.
Hsu JH, Wang CK, Hung CW, Wang SS, Cheng KI, Wu JR. Transesophageal echocardiography and laryngeal mask airway for placement of permanent central venous catheter in cancer patients with radiographically unidentifiable SVC-RA junction: effectiveness and safety. Kaohsiung J Med Sci. 2007;23:435–41.
Andropoulos DB, Stayer SA, Bent ST, et al. A controlled study of transesophageal echocardiography to guide central venous catheter placement in congenital heart surgery patients. Anesth Analg. 1999;89:65–70.
Gold JP, Jonas RA, Lang P, Elixson EM, Mayer JE, Castaneda AR. Transthoracic intracardiac monitoring lines in pediatric surgical patients: a ten-year experience. Ann Thorac Surg. 1986;42:185–91.
Flori HR, Johnson LD, Hanley FL, Fineman JR. Transthoracic intracardiac catheters in pediatric patients recovering from congenital heart defect surgery: associated complications and outcomes. Crit Care Med. 2000;28:2997–3001.
Rimensberger PC, Beghetti M. Pulmonary artery catheter placement under transoesophageal echocardiography guidance. Paediatr Anaesth. 1999;9:167–70.
Eguchi S, Bosher LH. Myocardial dysfunction resulting from coronary air embolism. Surgery. 1962;51:103–11.
Goldfarb D, Bahnson H. Early and late effects on the heart of small amounts of air in the coronary circulation. J Thorac Cardiovasc Surg. 1963;46:368–78.
Borger MA, Peniston CM, Weisel RD, Vasiliou M, Green RE, Feindel CM. Neuropsychologic impairment after coronary bypass surgery: effect of gaseous microemboli during perfusionist interventions. J Thorac Cardiovasc Surg. 2001;121:743–9.
Fearn SJ, Pole R, Burgess M, Ray SG, Hooper TL, McCollum CN. Cerebral embolisation during modern cardiopulmonary bypass. Eur J Cardiothorac Surg. 2001;20:1163–7.
Duff HJ, Buda AJ, Kramer R, Strauss HD, David TE, Berman ND. Detection of entrapped intracardiac air with intraoperative echocardiography. Am J Cardiol. 1980;46:255–60.
Oka Y, Moriwaki KM, Hong Y, et al. Detection of air emboli in the left heart by M-mode transesophageal echocardiography following cardiopulmonary bypass. Anesthesiology. 1985;63:109–13.
Topol EJ, Humphrey LS, Borkon AM, et al. Value of intraoperative left ventricular microbubbles detected by transesophageal two-dimensional echocardiography in predicting neurologic outcome after cardiac operations. Am J Cardiol. 1985;56:773–5.
Diehl JT, Ramos D, Dougherty F, Pandian NG, Payne DD, Cleveland RJ. Intraoperative, two-dimensional echocardiography-guided removal of retained intracardiac air. Ann Thorac Surg. 1987;43:674–5.
Meloni L, Abbruzzese PA, Cardu G, et al. Detection of microbubbles released by oxygenators during cardiopulmonary bypass by intraoperative transesophageal echocardiography. Am J Cardiol. 1990;66:511–4.
Orihashi K, Matsuura Y, Hamanaka Y, et al. Retained intracardiac air in open heart operations examined by transesophageal echocardiography. Ann Thorac Surg. 1993;55:1467–71.
Dalmas JP, Eker A, Girard C, et al. Intracardiac air clearing in valvular surgery guided by transesophageal echocardiography. J Heart Valve Dis. 1996;5:553–7.
Orihashi K, Matsuura Y, Sueda T, Shikata H, Mitsui N, Sueshiro M. Pooled air in open heart operations examined by transesophageal echocardiography. Ann Thorac Surg. 1996;61:1377–80.
Hoka S, Okamoto H, Yamaura K, Takahashi S, Tominaga R, Yasui H. Removal of retained air during cardiac surgery with transesophageal echocardiography and capnography. J Clin Anesth. 1997;9:457–61.
Greeley WJ, Kern FH, Ungerleider RM, Kisslo JA. Intramyocardial air causes right ventricular dysfunction after repair of a congenital heart defect. Anesthesiology. 1990;73:1042–6.
Cassorla L, Miller-Hance WC, Rouine-Rapp K, Reddy VM, Hanley FL, Silverman NH. Reliability of intraoperative contrast transesophageal echocardiography for detecting interatrial communications in patients with other congenital cardiovascular malformations. Am J Cardiol. 2003;91:1027–31.
Tousignant CP, Walsh F, Mazer CD. The use of transesophageal echocardiography for preload assessment in critically ill patients. Anesth Analg. 2000;90:351–5.
Buhre W, Buhre K, Kazmaier S, Sonntag H, Weyland A. Assessment of cardiac preload by indicator dilution and transoesophageal echocardiography. Eur J Anaesthesiol. 2001;18:662–7.
Stoddard MF, Longaker RA, Calzada N. Left atrial inflow propagation rate: a new transesophageal echocardiographic index of preload. J Am Soc Echocardiogr. 2002;15:1057–64.
Cheung AT, Savino JS, Weiss SJ, Aukburg SJ, Berlin JA. Echocardiographic and hemodynamic indexes of left ventricular preload in patients with normal and abnormal ventricular function. Anesthesiology. 1994;81:376–87.
Swenson JD, Harkin C, Pace NL, Astle K, Bailey P. Transesophageal echocardiography: an objective tool in defining maximum ventricular response to intravenous fluid therapy. Anesth Analg. 1996;83:1149–53.
Hofer CK, Ganter MT, Rist A, Klaghofer R, Matter-Ensner S, Zollinger A. The accuracy of preload assessment by different transesophageal echocardiographic techniques in patients undergoing cardiac surgery. J Cardiothorac Vasc Anesth. 2008;22:236–42.
Bu L, Munns S, Zhang H, et al. Rapid full volume data acquisition by real-time 3-dimensional echocardiography for assessment of left ventricular indexes in children: a validation study compared with magnetic resonance imaging. J Am Soc Echocardiogr. 2005;18:299–305.
Lu X, Xie M, Tomberlin D, et al. How accurately, reproducibly, and efficiently can we measure left ventricular indices using M-mode, 2-dimensional, and 3-dimensional echocardiography in children. Am Heart J. 2008;155:946–53.
Balluz R, Liu L, Zhou X, Ge S. Real-time three-dimensional echocardiography for quantification of ventricular volumes, mass, and function in children with congenital and acquired heart diseases. Echocardiography. 2013;30:472–82.
Altmann K, Shen Z, Boxt LM, et al. Comparison of three-dimensional echocardiographic assessment of volume, mass, and function in children with functionally single left ventricles with two-dimensional echocardiography and magnetic resonance imaging. Am J Cardiol. 1997;80:1060–5.
van den Bosch AE, Robbers-Visser D, Krenning BJ, et al. Real-time transthoracic three-dimensional echocardiographic assessment of left ventricular volume and ejection fraction in congenital heart disease. J Am Soc Echocardiogr. 2006;19:1–6.
Riehle TJ, Mahle WT, Parks WJ, Sallee D, Fyfe DA. Real-time three-dimensional echocardiographic acquisition and quantification of left ventricular indices in children and young adults with congenital heart disease: comparison with magnetic resonance imaging. J Am Soc Echocardiogr. 2008;21:78–83.
Grossgasteiger M, Hien MD, Graser B, et al. Assessment of left ventricular size and function during cardiac surgery. An intraoperative evaluation of six two-dimensional echocardiographic methods with real-time three-dimensional echocardiography as a reference. Echocardiography. 2013;30:672–81.
Meris A, Santambrogio L, Casso G, Mauri R, Engeler A, Cassina T. Intraoperative three-dimensional versus two-dimensional echocardiography for left ventricular assessment. Anesth Analg. 2014;118:711–20.
Smith MD, MacPhail B, Harrison MR, Lenhoff SJ, DeMaria AN. Value and limitations of transesophageal echocardiography in determination of left ventricular volumes and ejection fraction. J Am Coll Cardiol. 1992;19:1213–22.
Laser KT, Bunge M, Hauffe P, et al. Left ventricular volumetry in healthy children and adolescents: comparison of two different real-time three-dimensional matrix transducers with cardiovascular magnetic resonance. Eur J Echocardiogr. 2010;11:138–48.
Shimada YJ, Shiota T. A meta-analysis and investigation for the source of bias of left ventricular volumes and function by three-dimensional echocardiography in comparison with magnetic resonance imaging. Am J Cardiol. 2011;107:126–38.
Swenson JD, Bull D, Stringham J. Subjective assessment of left ventricular preload using transesophageal echocardiography: corresponding pulmonary artery occlusion pressures. J Cardiothorac Vasc Anesth. 2001;15:580–3.
Reich DL, Konstadt SN, Nejat M, Abrams HP, Bucek J. Intraoperative transesophageal echocardiography for the detection of cardiac preload changes induced by transfusion and phlebotomy in pediatric patients. Anesthesiology. 1993;79:10–5.
Poortmans G, Schüpfer G, Roosens C, Poelaert J. Transesophageal echocardiographic evaluation of left ventricular function. J Cardiothorac Vasc Anesth. 2000;14:588–98.
Lopez L, Colan SD, Frommelt PC, et al. Recommendations for quantification methods during the performance of a pediatric echocardiogram: a report from the Pediatric Measurements Writing Group of the American Society of Echocardiography Pediatric and Congenital Heart Disease Council. J Am Soc Echocardiogr. 2010;23:465–95.
Tei C. New non-invasive index for combined systolic and diastolic ventricular function. J Cardiol. 1995;26:135–6.
Eidem BW, Tei C, O’Leary PW, Cetta F, Seward JB. Nongeometric quantitative assessment of right and left ventricular function: myocardial performance index in normal children and patients with Ebstein anomaly. J Am Soc Echocardiogr. 1998;11:849–56.
Eidem BW, O’Leary PW, Tei C, Seward JB. Usefulness of the myocardial performance index for assessing right ventricular function in congenital heart disease. Am J Cardiol. 2000;86:654–8.
Roberson DA, Cui W. Right ventricular Tei index in children: effect of method, age, body surface area, and heart rate. J Am Soc Echocardiogr. 2007;20:764–70.
Ikemba CM, Su JT, Stayer SA, et al. Myocardial performance index with sevoflurane-pancuronium versus fentanyl-midazolam-pancuronium in infants with a functional single ventricle. Anesthesiology. 2004;101:1298–305.
Fernandes JMG, de Oliveira RB, Rivera IR, et al. Clinical value of myocardial performance index in patients with isolated diastolic dysfunction. Cardiovasc Ultrasound. 2019;17:17.
Moller JE, Poulsen SH, Egstrup K. Effect of preload alternations on a new Doppler echocardiographic index of combined systolic and diastolic performance. J Am Soc Echocardiogr. 1999;12:1065–72.
Davlouros PA, Niwa K, Webb G, Gatzoulis MA. The right ventricle in congenital heart disease. Heart. 2006;92(Suppl 1):i27–38.
Roche SL, Redington AN. The failing right ventricle in congenital heart disease. Can J Cardiol. 2013;29:768–78.
Friedberg MK, Reddy S. Right ventricular failure in congenital heart disease. Curr Opin Pediatr. 2019;5:604–10.
Brida M, Diller GP, Gatzoulis MA. Systemic right ventricle in adults with congenital heart disease: anatomic and phenotypic spectrum and current approach to management. Circulation. 2018;137:508–18.
Kasper J, Bolliger D, Skarvan K, Buser P, Filipovic M, Seeberger MD. Additional cross-sectional transesophageal echocardiography views improve perioperative right heart assessment. Anesthesiology. 2012;117:726–34.
Rudski LG, Lai WW, Afilalo J, et al. Guidelines for the echocardiographic assessment of the right heart in adults: a report from the American Society of Echocardiography endorsed by the European Association of Echocardiography, a registered branch of the European Society of Cardiology, and the Canadian Society of Echocardiography. J Am Soc Echocardiogr. 2010;23:685–713.
Lu X, Nadvoretskiy V, Bu L, et al. Accuracy and reproducibility of real-time three-dimensional echocardiography for assessment of right ventricular volumes and ejection fraction in children. J Am Soc Echocardiogr. 2008;21:84–9.
Grewal J, Majdalany D, Syed I, Pellikka P, Warnes CA. Three-dimensional echocardiographic assessment of right ventricular volume and function in adult patients with congenital heart disease: comparison with magnetic resonance imaging. J Am Soc Echocardiogr. 2010;23:127–33.
Leibundgut G, Rohner A, Grize L, et al. Dynamic assessment of right ventricular volumes and function by real-time three-dimensional echocardiography: a comparison study with magnetic resonance imaging in 100 adult patients. J Am Soc Echocardiogr. 2010;23:116–26.
Tamborini G, Marsan NA, Gripari P, et al. Reference values for right ventricular volumes and ejection fraction with real-time three-dimensional echocardiography: evaluation in a large series of normal subjects. J Am Soc Echocardiogr. 2010;23:109–15.
Dragulescu A, Grosse-Wortmann L, Fackoury C, Mertens L. Echocardiographic assessment of right ventricular volumes: a comparison of different techniques in children after surgical repair of tetralogy of Fallot. Eur Heart J Cardiovasc Imaging. 2012;13:596–604.
Maffessanti F, Muraru D, Esposito R, et al. Age-, body size-, and sex-specific reference values for right ventricular volumes and ejection fraction by three-dimensional echocardiography: a multicenter echocardiographic study in 507 healthy volunteers. Circ Cardiovasc Imaging. 2013;6:700–10.
Renella P, Marx GR, Zhou J, Gauvreau K, Geva T. Feasibility and reproducibility of three-dimensional echocardiographic assessment of right ventricular size and function in pediatric patients. J Am Soc Echocardiogr. 2014;27:903–10.
Fusini L, Tamborini G, Gripari P, et al. Feasibility of intraoperative three-dimensional transesophageal echocardiography in the evaluation of right ventricular volumes and function in patients undergoing cardiac surgery. J Am Soc Echocardiogr. 2011;24:868–77.
Nishimura RA, Tajik AJ. Evaluation of diastolic filling of left ventricle in health and disease: Doppler echocardiography is the clinician’s Rosetta Stone. J Am Coll Cardiol. 1997;30:8–18.
Schmitz L, Koch H, Bein G, Brockmeier K. Left ventricular diastolic function in infants, children, and adolescents. Reference values and analysis of morphologic and physiologic determinants of echocardiographic Doppler flow signals during growth and maturation. J Am Coll Cardiol. 1998;32:1441–8.
Bernard F, Denault A, Babin D, et al. Diastolic dysfunction is predictive of difficult weaning from cardiopulmonary bypass. Anesth Analg. 2001;92:291–8.
Swaminathan M, Nicoara A, Phillips-Bute BG, et al. Utility of a simple algorithm to grade diastolic dysfunction and predict outcome after coronary artery bypass graft surgery. Ann Thorac Surg. 2011;91:1844–50.
Border WL, Michelfelder EC, Glascock BJ, et al. Color M-mode and Doppler tissue evaluation of diastolic function in children: simultaneous correlation with invasive indices. J Am Soc Echocardiogr. 2003;16:988–94.
Nagueh SF, Smiseth OA, Appleton CP, et al. Recommendations for the evaluation of left ventricular diastolic function by echocardiography: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr. 2016;29:277–314.
Gidding SS, Snider AR, Rocchini AP, Peters J, Farnsworth R. Left ventricular diastolic filling in children with hypertrophic cardiomyopathy: assessment with pulsed Doppler echocardiography. J Am Coll Cardiol. 1986;8:310–6.
Olivier M, O’Leary PW, Pankratz VS, et al. Serial Doppler assessment of diastolic function before and after the Fontan operation. J Am Soc Echocardiogr. 2003;16:1136–43.
McMahon CJ, Nagueh SF, Pignatelli RH, et al. Characterization of left ventricular diastolic function by tissue Doppler imaging and clinical status in children with hypertrophic cardiomyopathy. Circulation. 2004;109:1756–62.
Fazio G, Pipitone S, Iacona MA, et al. Evaluation of diastolic function by the tissue Doppler in children affected by non-compaction (letter). Int J Cardiol. 2007;116:e60–2.
Harahsheh A, Aggarwal S, Pettersen MD, L’Ecuyer T. Diastolic function in anthracycline-treated children. Cardiol Young. 2015;25:1130–5.
Yim DL, Jones BO, Alexander PM, d’Udekem Y, Cheung MM. Effect of anti-heart failure therapy on diastolic function in children with single-ventricle circulations. Cardiol Young. 2015;25:1293–9.
Castello R, Pearson AC, Lenzen P, Labovitz AJ. Evaluation of pulmonary venous flow by transesophageal echocardiography in subjects with a normal heart: comparison with transthoracic echocardiography. J Am Coll Cardiol. 1991;18:65–71.
Margossian R, Sleeper LA, Pearson GD, et al. Assessment of diastolic function in single-ventricle patients after the Fontan procedure. J Am Soc Echocardiogr. 2016;29:1066–73.
Nadorlik H, Stiver C, Khan S, et al. Correlations between echocardiographic systolic and diastolic function with cardiac catheterization in biventricular congenital heart patients. Pediatr Cardiol. 2016;37:765–71.
Mawad W, Friedberg MK. The continuing challenge of evaluating diastolic function by echocardiography in children: developing concepts and newer modalities. Curr Opin Cardiol. 2017;32:93–100.
DiLorenzo M, Hwang WT, Goldmuntz E, Ky B, Mercer-Rosa L. Diastolic dysfunction in tetralogy of Fallot: comparison of echocardiography with catheterization. Echocardiography. 2018;35:1641–8.
Smith JS, Cahalan MK, Benefiel DJ, et al. Intraoperative detection of myocardial ischemia in high-risk patients: electrocardiography versus two-dimensional transesophageal echocardiography. Circulation. 1985;72:1015–21.
van Daele ME, Sutherland GR, Mitchell MM, et al. Do changes in pulmonary capillary wedge pressure adequately reflect myocardial ischemia during anesthesia? A correlative preoperative hemodynamic, electrocardiographic, and transesophageal echocardiographic study. Circulation. 1990;81:865–71.
Moisés VA, Mesquita CB, Campos O, et al. Importance of intraoperative transesophageal echocardiography during coronary artery surgery without cardiopulmonary bypass. J Am Soc Echocardiogr. 1998;11:1139–44.
Balaguru D, Auslender M, Colvin SB, Rutkowski M, Artman M, Phoon CK. Intraoperative myocardial ischemia recognized by transesophageal echocardiography monitoring in the pediatric population: a report of 3 cases. J Am Soc Echocardiogr. 2000;13:615–8.
Rouine-Rapp K, Rouillard KP, Miller-Hance W, et al. Segmental wall-motion abnormalities after an arterial switch operation indicate ischemia. Anesth Analg. 2006;103:1139–46.
Wong D, Golding F, Hess L, et al. Intraoperative coronary artery pulse Doppler patterns in patients with complete transposition of the great arteries undergoing the arterial switch operation. Am Heart J. 2008;156:466–72.
Nield LE, Dragulescu A, MacColl C, et al. Coronary artery Doppler patterns are associated with clinical outcomes post-arterial switch operation for transposition of the great arteries. Eur Heart J Cardiovasc Imaging. 2018;19:461–8.
Benson MJ, Cahalan MK. Cost-benefit analysis of transesophageal echocardiography in cardiac surgery. Echocardiography. 1995;12:171–83.
Siwik ES, Spector ML, Patel CR, Zahka KG. Costs and cost-effectiveness of routine transesophageal echocardiography in congenital heart surgery. Am Heart J. 1999;138:771–6.
Bettex DA, Prêtre R, Jenni R, Schmid ER. Cost-effectiveness of routine intraoperative transesophageal echocardiography in pediatric cardiac surgery: a 10-year experience. Anesth Analg. 2005;100:1271–5.
Levin DN, Taras J, Taylor K. The cost effectiveness of transesophageal echocardiography for pediatric cardiac surgery: a systematic review. Paediatr Anaesth. 2016;26:682–93.
Seward JB, Khandheria BK, Oh JK, Freeman WK, Tajik AJ. Critical appraisal of transesophageal echocardiography: limitations, pitfalls, and complications. J Am Soc Echocardiogr. 1992;5:288–305.
Konstadt SN, Reich DL, Quintana C, Levy M. The ascending aorta: how much does transesophageal echocardiography see? Anesth Analg. 1994;78:240–4.
Khandheria BK, Seward JB, Tajik AJ. Critical appraisal of transesophageal echocardiography: limitations and pitfalls. Crit Care Clin. 1996;12:235–51.
Dragulescu A, Golding F, Van Arsdell G, et al. The impact of additional epicardial imaging to transesophageal echocardiography on intraoperative detection of residual lesions in congenital heart surgery. J Thorac Cardiovasc Surg. 2012;143:361–7.
Kim HK, Kim WH, Hwang SW, et al. Predictive value of intraoperative transesophageal echocardiography in complete atrioventricular septal defect. Ann Thorac Surg. 2005;80:56–9.
le Polain de Waroux JB, Pouleur AC, Robert A, et al. Mechanisms of recurrent aortic regurgitation after aortic valve repair: predictive value of intraoperative transesophageal echocardiography. JACC Cardiovasc Imaging. 2009;2:931–9.
Hanna BM, El-Hewala AA, Gruber PJ, Gaynor JW, Spray TL, Seliem MA. Predictive value of intraoperative diagnosis of residual ventricular septal defects by transesophageal echocardiography. Ann Thorac Surg. 2010;89:1233–7.
Stern KW, White MT, Verghese GR, Del Nido PJ, Geva T. Intraoperative echocardiography for congenital aortic valve repair: predictors of early reoperation. Ann Thorac Surg. 2015;100:678–85.
Redlin M, Miera O, Habazettl H, et al. Incidence and echocardiographic predictors of early postoperative right ventricular dysfunction following left ventricular assist implantation in paediatric patients. Interact Cardiovasc Thorac Surg. 2017;25:887–91.
Kaushal SK, Radhakrishanan S, Dagar KS, et al. Significant intraoperative right ventricular outflow gradients after repair for tetralogy of Fallot: to revise or not to revise. Ann Thorac Surg. 1999;68:1705–12.
Yang SG, Novello R, Nicolson S, et al. Evaluation of ventricular septal defect repair using intraoperative transesophageal echocardiography: frequency and significance of residual defects in infants and children. Echocardiography. 2000;17:681–4.
Lee HR, Montenegro LM, Nicolson SC, Gaynor JW, Spray TL, Rychik J. Usefulness of intraoperative transesophageal echocardiography in predicting the degree of mitral regurgitation secondary to atrioventricular defect in children. Am J Cardiol. 1999;83:750–3.
Honjo O, Kotani Y, Osaki S, et al. Discrepancy between intraoperative transesophageal echocardiography and postoperative transthoracic echocardiography in assessing congenital valve surgery. Ann Thorac Surg. 2006;82:2240–6.
Shoiab I, Danford DA, Li L, Abdullah I, Hammel JM, Kutty S. Predischarge transthoracic echocardiography after surgery for congenital heart disease: a routine with a reason. J Am Soc Echocardiogr. 2015;28:1030–5.
Oh JK, Seward JB, Khandheria BK, et al. Transesophageal echocardiography in critically ill patients. Am J Cardiol. 1990;66:1492–5.
Font VE, Obarski TP, Klein AL, et al. Transesophageal echocardiography in the critical care unit. Cleve Clin J Med. 1991;58:315–22.
Foster E, Schiller NB. The role of transesophageal echocardiography in critical care: UCSF experience. J Am Soc Echocardiogr. 1992;5:368–74.
Khoury AF, Afridi I, Quinones MA, Zoghbi WA. Transesophageal echocardiography in critically ill patients: feasibility, safety, and impact on management. Am Heart J. 1994;127:1363–71.
Poelaert J, Schmidt C, Van Aken H, Colardyn F. Transoesophageal echocardiography in critically ill patients. A comprehensive approach. Eur J Anaesthesiol. 1997;14:350–8.
Hüttemann E, Schelenz C, Kara F, Chatzinikolaou K, Reinhart K. The use and safety of transoesophageal echocardiography in the general ICU—a minireview. Acta Anaesthesiol Scand. 2004;48:827–36.
Hüttemann E. Transoesophageal echocardiography in critical care. Minerva Anestesiol. 2006;72:891–913.
Ananthasubramaniam K, Jaffery Z. Postoperative right atrial compression by extracardiac hematoma: transesophageal echocardiographic diagnosis in the critically ill patient. Echocardiography. 2007;24:661–3.
Arntfield R, Lau V, Landry Y, Priestap F, Ball I. Impact of critical care transesophageal echocardiography in medical-surgical ICU patients: characteristics and results from 274 consecutive examinations. J Intensive Care Med. 2018;35(9):896–902.
Wolfe LT, Rossi A, Ritter SB. Transesophageal echocardiography in infants and children: use and importance in the cardiac intensive care unit. J Am Soc Echocardiogr. 1993;6:286–9.
Marcus B, Wong PC, Wells WJ, Lindesmith GG, Starnes VA. Transesophageal echocardiography in the postoperative child with an open sternum. Ann Thorac Surg. 1994;58:235–6.
Scheinin SA, Radovancevic B, Ott DA, Nihill MR, Cabalka A, Frazier OH. Postcardiotomy LVAD support and transesophageal echocardiography in a child. Ann Thorac Surg. 1993;55:529–31.
Kocabas S, Askar FZ, Yagdi T, Engin C, Ozbaran M. Anesthesia for ventricular assist device placement in pediatric patients: experience from a single center. Transplant Proc. 2013;45:1009–12.
Crowley J, Cronin B, Essandoh M, D’Alessandro D, Shelton K, Dalia AA. Transesophageal echocardiography for Impella placement and management. J Cardiothorac Vasc Anesth. 2019;33:2663–8.
Baillard C, Cohen Y, Fosse JP, Karoubi P, Hoang P, Cupa M. Haemodynamic measurements (continuous cardiac output and systemic vascular resistance) in critically ill patients: transoesophageal Doppler versus continuous thermodilution. Anaesth Intensive Care. 1999;27:33–7.
Feinberg MS, Hopkins WE, Davila-Roman VG, Barzilai B. Multiplane transesophageal echocardiographic Doppler imaging accurately determines cardiac output measurements in critically ill patients. Chest. 1995;107:769–73.
Patel JK, Glatz AC, Ghosh RM, et al. Accuracy of transesophageal echocardiography in the identification of postoperative intramural ventricular septal defects. J Thorac Cardiovasc Surg. 2016;152:688–95.
Douglas PS, Khandheria B, Stainback RF, et al. ACCF/ASE/ACEP/ASNC/SCAI/SCCT/SCMR 2007 Appropriateness criteria for transthoracic and transesophageal echocardiography: a report of the American College of Cardiology Foundation Quality Strategic Directions Committee Appropriateness Criteria Working Group, American Society of Echocardiography, American College of Emergency Physicians, American Society of Nuclear Cardiology, Society for Cardiovascular Angiography and Interventions, Society of Cardiovascular Computed Tomography, and the Society for Cardiovascular Magnetic Resonance endorsed by the American College of Chest Physicians and the Society of Critical Care Medicine. J Am Coll Cardiol. 2007;50:187–204.
Douglas PS, Garcia MJ, Haines DE, et al. ACCF/ASE/AHA/ASNC/HFSA/HRS/SCAI/SCCM/SCCT/SCMR 2011 Appropriate Use Criteria for Echocardiography. A Report of the American College of Cardiology Foundation Appropriate Use Criteria Task Force, American Society of Echocardiography, American Heart Association, American Society of Nuclear Cardiology, Heart Failure Society of America, Heart Rhythm Society, Society for Cardiovascular Angiography and Interventions, Society of Critical Care Medicine, Society of Cardiovascular Computed Tomography, and Society for Cardiovascular Magnetic Resonance. J Am Coll Cardiol. 2011;57:1126–66.
McGuinness GA, Schieken RM, Maguire GF. Endocarditis in the newborn. Am J Dis Child. 1980;134:577–80.
Acknowledgments
The authors would like to gratefully acknowledge Isobel A. Russell, MD for her expertise and contribution to this chapter and co-authorship in the prior edition.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2021 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Miller-Hance, W.C., Vegas, A. (2021). Intraoperative and Postoperative Applications. In: Wong, P.C., Miller-Hance, W.C. (eds) Transesophageal Echocardiography for Pediatric and Congenital Heart Disease. Springer, Cham. https://doi.org/10.1007/978-3-030-57193-1_18
Download citation
DOI: https://doi.org/10.1007/978-3-030-57193-1_18
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-57192-4
Online ISBN: 978-3-030-57193-1
eBook Packages: MedicineMedicine (R0)