Abstract
Hybrid procedures are becoming increasingly important, especially in the management of congenital heart lesions for which there are no ideal surgical or interventional options. This report describes a multicenter experience with perventricular muscular venticular septal defect (VSD) device closure.
Three groups of patients (n = 12) were identified: infants with isolated muscular VSDs (n = 2), neonates with aortic coarctation and muscular VSDs (n = 3) or patients with muscular VSDs and other complex cardiac lesions (n = 2), and patients with muscular VSDs and pulmonary artery bands (n = 5). Via a sternotomy or a subxyphoid approach, the right ventricle (RV) free wall was punctured under transesophageal echocardiography guidance. A guidewire was introduced across the largest defect. A short delivery sheath was positioned in the left ventricle cavity. An Amplatzer muscular VSD occluding device was deployed across the VSD. Cardiopulmonary bypass was needed only for repair of concomitant lesions, such as double-outlet right ventricle, aortic coarctation, or pulmonary artery band removal. No complications were encountered using this technique. Discharge echocardiograms showed either mild or no significant shunting across the ventricular septum. At a median follow-up of 12 months, all patients were asymptomatic and 2 patients had mild residual ventricular level shunts. Perventricular closure of muscular VSDs is safe and effective for a variety of patients with muscular VSDs.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Management of muscular ventricular septal defects (VSDs) remains suboptimal [11, 15, 16]. Isolated muscular VSDs are increasingly being successfully closed in the catheterization laboratory [9, 17]. However, when encountered in small infants or patients with poor vascular access, catheter closure remains challenging. Managing multiple muscular VSDs remains a challenge for both surgeons and interventionalists, sometimes culminating in the need for heart transplantation [11, 14, 15]. Left ventriculotomy or the division of multiple important right-sided muscle bands is associated with long-term morbidity [11, 15, 16]. On the other hand, placing several devices percutaneously across the ventricular septum during several sessions in the catheterization laboratory can also result in significant arrhythmias, hemodynamic compromise, tricuspid valve injury, or incomplete closures [17]. Furthermore, the presence of multiple muscular VSDs has been found to be an independent risk factor for early mortality after repair of complex congenital heart lesions such as double-outlet right ventricle (DORV) or transposition of the great arteries (TGA) [5, 12]. Therefore, eliminating this risk factor prior to complex repair is beneficial, especially if it can be done in one setting in the operating room.
Hybrid therapies aim to combine the advantages of surgical and interventional techniques in an effort to reduce the “invasiveness” (cardiopulmonary bypass, cardioplegic arrest, incisional trauma, groin vessel injury, risk to the tricuspid valve, etc.) of a given procedure [7]. The combination of interventional and surgical techniques has been tried before but with limited success. Cardiopulmonary bypass and cardioplegic arrest were needed in all cases and VSD devices were deployed under direct vision on the arrested heart [8, 10, 13, 14]. Results were not satisfactory, mainly due to residual shunting, with mortality rates ranging from 14 to 25%.
This report summarizes the combined experience with perventricular muscular VSD closure acquired by three separate groups actively engaged in hybrid techniques. The device used was the Amplatzer muscular VSD occluder (AGA Medical Corporation, Golden Valley, MN, USA [9], a self-expandable double-disc device made from nitinol wire mesh. The device size corresponds to the waist diameter of the device, with the length being 7 mm, corresponding to the thickness of the muscular septum in most infants and children.
Methods
This study started in September 2002. Informed consent was obtained from the patients’ guardians. The study was approved by each hospital investigation review board. Excluding one patient from Chile, this study was part of a Food and Drug Administration Investigation Device Exemption clinical trial.
Selection criteria were as follows:
-
Group 1: Small infants with muscular VSD(s) or patients with poor vascular access
-
Group 2: In addition to one or multiple muscular VSDs, the presence of cardiac lesions necessitating operative repair
-
Group 3: Patients with muscular VSDs and pulmonary artery (AA) bands
Standard pediatric cardiac surgical intra- and postoperative monitoring, protocols, and equipments were used.
Description of the Technique
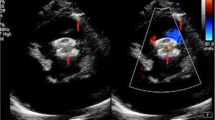
The heart was approached via a median sternotomy or a subxyphoid minimally invasive incision without sternotomy. Under continuous transesophageal echocardiography (TEE) guidance, the best location for right ventricular (RV) puncture was chosen, paying being attention away from any papillary muscles but far enough from the septum so as to approach it from a perpendicular angle with the needle and wire (Fig. 1). A 5-0 polypropelene purse-string was placed at the chosen location. An 18-guage needle (Cook, Bloomington, IN, USA) was introduced into the RV cavity and a 0.035-in. angled glide wire (Boston Scientific, Medi-Tech, Natick, MA, USA) was passed through the needle and manipulated into the left ventricular (LV) cavity through the defect. A 7- to 10-Fr short (8-13 cm) introducer sheath with a dilator was fed over the wire and carefully advanced into the LV cavity. Care must be taken to keep the tip of the dilator in the middle of the LV cavity (monitored by TEE) because it could perforate the LV free wall. The dilator was removed and the sheath tip positioned in the LV cavity. The appropriate device size was chosen to be 1 or 2 mm larger than the VSD size as assessed by color doppler TEE. The device was presoaked in nonheparinized patient’s blood for 10 minutes to allow for the tiny fenestrations of the nitinol mesh to thrombose. The device was then screwed to the cable and pulled inside a 6- to 9-Fr loader under blood seal to prevent any air bubbles. The device was advanced inside the short delivery sheath until it was seen by TEE to be close to the tip of the delivery sheath. The LV disc was deployed in the mid-LV cavity by gentle retraction of the sheath over the cable. The entire assembly (cable/sheath) was withdrawn gently until the LV disc was against the septum. Further retraction of the sheath over the cable would deploy the waist inside the septum. Continuous TEE to confirm the device position is of extreme importance. Once the position was confirmed, further retraction of the sheath to expand the RV disc was performed. If the device position was satisfactory, the device was released by counterclockwise rotation of the cable using the pin vise. A complete TEE study in multiple planes was done to confirm device placement and assess for residual shunting and any obstruction or regurgitation induced by the device.
(A) Four-chamber view of a mid- to posterior muscular ventricular septal defect (VSD) via intraoperative transesophageal echocardiography (TEE). LA, left atrium; LV, left ventricule; RA, right atrium; RV, right ventricule. (B) Color Doppier flow across the VSD. (C) Using a forceps tip, the right ventricular free wall is probed to determine the shortest distance from the free wall to the VSD, staying away from the anterior papillary muscle of the tricuspid valve. (D) A needle is introduced into the right ventricular cavity and a guidewire manipulated into the left ventricle. (E) An introducer sheath is passed over a dilator and positioned into the left ventricular cavity. (F) The device is pushed into the sheath and the LV disc deployed by gently retracting the sheath. (G) The RV disc is similarly deployed, but the device is still attached to the delivery cable. This allows for TEE confirmation of valve function and VSD closures, as well as recapture of the device into the sheath (by advancing the sheath), necessary. (H) Final confirmation of lack of shunting.
Results
Table 1 lists the clinical details. Six patients have been presented previously [6]. The procedure was attempted in 13 patients and was successful in 12. One 3-kg neonate with a large high posterior muscular VSD was converted from a perventricular approach to an open-heart approach due to the inability to open the RV disc without impingement of the septal leaflet of the tricuspid valve. The repair was successfully completed surgically. One patient with a posterior muscular VSD had a peratrial approach with complete closure after attempts to cross the VSD via a perventricular approach were unsuccessful. There were no intraoperative complications. One patient needed reintubation for pulmonary reperfusion injury secondary to a PA band takedown. One neonate with CoA/VSD had postoperative mediastinitis that required sternal plating and a prolonged intensive care unit stay. At a median follow-up of 12 months (range, 3-23), all patients were asymptomatic. One patient in group 3 has mild to moderate shunting across separate small apical defects, and one mild patient has mild shunting across the edge of the device. Neither patient has echocardiographic or clinical evidence of significant congestive heart failure, volume overload, or pulmonary hypertension.
Discussion
The first successful case of intraoperative perventricular device closure on the beating heart in an infant was reported in 1998 [2]. Subsequently, this technique’s safety has been validated in animal experiments [3, 4], and it has even been successfully applied for perventricular membranous VSD closure in animals [1].
Using the technique described here, we have identified four groups of congenital heart disease patients that can be better managed with a hybrid approach. This is the largest reported series of perventricular muscular VSD device closure. The technique does not require cardiopulmonary bypass (CPB) support or full stemotomy. The heart can be approached via small incisions, thus providing the possibility of performing a large variety of peratrial or perventricular procedures. The technique is simple and requires mainly excellent collaboration between echocardiographer, surgeon, and interventionalist. Although not formally measured, the time needed to cross the VSD and position the device was less than 30 minutes in all cases. This compares very favorably with the much longer procedure times when the equivalent maneuver is attempted in the catheterization laboratory. The advantages of this technique over standard surgical techniques include avoidance or reduction of CPB time. Other advantages include avoidance of transection of the moderator band or other RV muscle bundles, immediate confirmation of adequate closure, and avoidance of any ventricular incisions. The technique is not limited by low weight or vascular access problems. Particularly in malformations with unusual septal planes, such as DORV or TGA, the percutaneous retrograde approach to cross muscular VSDs can be very challenging if not impossible. This technique eliminates that issue because the septum is approached from a perpendicular and not a parallel (i.e., tricuspid valve) plane. As opposed to a percutaneous approach, the perventricular approach offers a “straight shot” at the lesion to be addressed, with no wire kinks or loops to be negotiated by the sheath or the device. Delivery of self-expandable valves may also be simplified by this technique [18].
Based on our data, we believe that palliating symptomatic infants with large muscular VSDs with PA banding is not indicated anymore. Irrespective of weight, these infants can undergo perventricular VSD closure if they are not candidates for a percutaneous approach. This approach is also indicated for neonates with aortic coarctation and large muscular VSDs, where a “one-stage” repair via sternotomy can be applied. The technique also offers the possibility to do a one-stage PA band takedown, identify all VSDs under nonbanded conditions, and close them using the perventricular approach. However, in this setting, severely hypertrophied RV muscle bundles can make the recognition of the true VSD margins difficult and render the correct deployment of the RV disc more challenging. Muscular VSDs that are in close proximity to atrioventricular valves, such as high posterior muscular VSDs present a unique challenge. As seen in one of the patients, they may be better approached via a peratrial puncture, allowing the wire and the device to glide under the tricuspid subvalvar apparatus. The muscular septal thickness is typically only 4 or 5 mm. The waist of the current Amplatzer muscular VSD occluder is 7 mm long, making it too long for this location, with likely interference with tricuspid or mitral valve function, seen in the one patient in whom the technique was unsuccessful. A custom-made device may alleviate this problem in the future.
The limitations of this study include a small patient sample, short follow-up, and the lack of randomization.
In conclusion, this multicenter study demonstrates that perventricular muscular VSD closure is safe and effective for a variety of patients with muscular VSDs. With advances in introducer and robotic technologies, peratrial or perventricular procedures may be performed via port approaches.
References
Z Amin JM Berry DA Danford (2001) ArticleTitleIntraoperative closure of perimembranous ventricular septal defects without cardiopulmonary bypass. Preliminary results of the perventricular approach Circulation 104 II–710
Z Amin JM Berry JE Foker AP Rocchini JL Bass (1998) ArticleTitleIntraoperative closure of muscular ventricular septal defect in a canine model and application of the technique in a baby J Thorac Cardiovasc Surg 115 1374–14376 Occurrence Handle9628681
Z Amin X Gu JM Berry et al. (1999) ArticleTitleNew device for closure of muscular ventricular septal defects in a canine model Circulation 100 320–328 Occurrence Handle10411859
Z Amin X Gu JM Berry et al. (1999) ArticleTitlePerventricular closure of ventricular septal defects without cardiopulmonay bypass Ann Thorac Surg 68 149–154 Occurrence Handle10.1016/S0003-4975(99)00519-6 Occurrence Handle10421131
M Aoki JM Forbess RA Jonas JE Mayer SuffixJr AR Castaneda (1994) ArticleTitleResults of biventricular repair for double-outlet right ventricle J Thorac Cardioyasc Surg 1.07 338–350
EA Bacha QL Cao JP Starr et al. (2003) ArticleTitlePerventricular device closure of muscular ventricular septal defects on the beating heart: technique and results J Thorac Cardiovasc Surg 126 1718–1723 Occurrence Handle10.1016/S0022-5223(03)01043-2 Occurrence Handle14688678
EA Bacha ZM Hijazi QL Cao et al. (2004) ArticleTitleHybrid pediatric cardiac surgery Pediatr Cardiol . .
RR Chaturvedi DF Shore M Yacoub AN Redington (1996) ArticleTitleIntraoperative apical ventricular septal defect closure using a modified Rashkind double umbrella Heart 76 367–369 Occurrence Handle8983687
M Chessa M Carminati QL Cao et al. (2002) ArticleTitleTranscatheter closure of congenital and acquired muscular ventricular septal defects using the Amplatzer device J Invas Cardiol 14 322–327
SB Fishberger ND Bridges JF Keane et al. (1993) ArticleTitleCongenital heart disease: intraoperative device closure of ventricular septal defects Circulation 88 II205–II209 Occurrence Handle8222155
T Kitagawa LA Durham RS Mosca EL Bove (1998) ArticleTitleTechniques and results in the management of multiple ventricular septal defects J Thorac Cardiqvasc Surg 115 848–856
S Kleinert T Sano RG Weintraub et al. (1997) ArticleTitleAnatomic features and surgical strategies in double-outlet right ventricle Circulation 96 1233–1239 Occurrence Handle9286954
B Murzi GL Bonanomi S Giusti et al. (1997) ArticleTitleSurgical closure of muscular VSD using double umbrella devices (intraoperative VSD device closure) Bur J Cardiothorac Surg 12 450–455 Occurrence Handle10.1016/S1010-7940(97)00086-9
M Okubo LN Benson D Nykanen et al. (2001) ArticleTitleOutcomes of intraoperative device closure of muscular ventricular septal defects Ann Thorac Surg 12 416–423 Occurrence Handle10.1016/S0003-4975(01)02829-6
F Seddio VM Reddy DB McElhinney et al. (1999) ArticleTitleMultiple ventricular septal defects: how and when should they be repaired? J Thorac Cardiovasc Surg 117 134–140 Occurrence Handle9869767
A Serraf F Lacour-Gayet J Bruniaux et al. (1992) ArticleTitleSurgical management of isolated multiple ventricular septal defects. Logical approach in 130 cases J Thorac Cardiovasc Surg 103 437–442 Occurrence Handle1545542
DJ Waight EA Bacha M Kahana et al. (2002) ArticleTitleCatheter therapy of Swiss cheese ventricular septal defects using the Amplatzer muscular VSD occluder Cathet Cardiovasc Intervent 55 355–361 Occurrence Handle10.1002/ccd.10124
JQ Zhou AF Corno CH Huber P Tozzi LK Segesser Particlevon (2003) ArticleTitleSelf-expandable valved stent of large size: off-bypass implantation in pulmonary position Eur J Cardio-Thorac Surg 24 212–216 Occurrence Handle10.1016/S1010-7940(03)00178-7
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bacha, E., Cao, QL., Galantowicz, M. et al. Multicenter Experience with Perventricular Device Closure of Muscular Ventricular Septal Defects. Pediatr Cardiol 26, 169–175 (2005). https://doi.org/10.1007/s00246-004-0956-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00246-004-0956-2