Abstract
Knowing the cancer genomic profile with underlying druggable molecular alterations is important for the optimal choice of cancer therapy. However, molecular analysis of tumor DNA can be limited by the availability of the cancer tissue, which has to be obtained from therapeutic or diagnostic procedures. Molecular analysis of liquid biopsies utilizing the circulating tumor cell-free DNA offers a minimally invasive and low-risk method that can be performed at multiple time points for molecular analysis. Molecular testing of cell-free DNA can be used in multiple clinically useful applications, such as identification of molecular targets for cancer therapy, assessment of cancer prognosis, monitoring of response to cancer therapy, monitoring of tumor molecular profiles in real time, and study target engagement when developing new therapies.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keyword
FormalPara Key Points-
Liquid biopsies are minimally invasive and can provide tumor DNA for molecular testing.
-
Molecular testing of cell-free DNA can help to determine cancer prognosis.
-
Molecular testing of cell-free DNA isolated from blood or other body fluids can identify targets for cancer therapy.
-
Serial molecular testing of cell-free DNA has potential as a tool for assessment of therapeutic response to cancer therapy.
-
Serial molecular testing of cell-free DNA can be used to study clonal evolution and mechanisms of therapeutic resistance.
-
Liquid biopsies have potential to be used in pharmacodynamic studies in clinical trials.
14.1 Introduction
Selection of an optimal treatment strategy requires detailed analysis of the cancer genome and identification of molecular targets for cancer therapy in each individual patient [1, 2]. Molecular testing of tumor samples obtained from diagnostic or therapeutic procedures remains the current standard of care. However, this approach has significant limitations because of tumor heterogeneity and the dynamic nature of tumor genotypes, which would mandate multiple biopsies from primary and metastatic sites at multiple time points [3, 4]. This is hardly feasible because of medical, ethical, financial and logistic considerations. To overcome these limitations, novel minimally invasive methods to detect pertinent molecular alterations in tumor DNA associated with less risk to the patient and lower cost are being developed. Mandel and Métais in 1948 noted the presence of cell-free nucleic acids (cfNA) in human blood [5, 6]. However, it took about six decades before reports were published on detection of oncogenic aberrations in blood-derived cell-free DNA (cfDNA) in patients with cancer [7]. Fragments of cfDNA can be detected in plasma, urine, cerebrospinal fluid (CSF), and other body fluids [5, 8,9,10,11,12,13,14,15,16,17,18,19,20]. These cfDNA fragments can be used for detection of underlying cancer-related molecular abnormalities, and such approach has become known as a liquid biopsy [12, 19, 21, 22]. In clinical trials, liquid biopsies can be used to identify targets for cancer therapy, to assess cancer prognosis, to assess efficacy of cancer therapy, to monitor cancer molecular profiles in real time and for assessment of target engagement. DNA or its fragments can enter the circulation by several distinct mechanisms, including release of nuclear and mitochondrial DNA from dying cells during either apoptosis or necrosis (Fig. 14.1). Other mechanisms of DNA release include autophagy and necroptosis [5, 23]. Fragments of cfDNA can vary in size substantially based on their mechanism of release. For instance, fragments of DNA released from apoptotic cells average around 160–180 bp in length, while the fragments of DNA from necrotic cells are usually longer. The average lengths of cfDNA fragments from apoptotic and necrotic processes, and their ratio, may be assessed as an important element of the DNA integrity index, which may have prognostic implications [24]. The cfDNA fragments are cleared from the circulation with half-lives ranging from 15 min to a few hours [21].
14.2 Methods for Molecular Testing of cfDNA
Sample collection and processing times can impact DNA integrity and accuracy of cfDNA assessment [5, 25]. Plasma is the most frequent source of circulating cfDNA, which is preferred to serum due to lower level of high molecular contamination by non-cancerous cfDNA from lysis of normal leukocytes. Because timely processing is among the most important factors to maintain cfDNA integrity, cell-stabilizing blood collection tubes, which allow sample processing to be delayed for several days, have become increasingly popular for collection of blood samples intended for cfDNA analysis [5, 26, 27]. Other materials, such urine, CSF or other body fluids are less cellular and arguably less prone to DNA degradation [10, 12, 18,19,20, 28].
The tumor-specific fraction also called circulating tumor DNA (ctDNA) of the total cfDNA can be identified by the presence of cancer-specific alterations, such as hot spot mutations, or through detection of cancer-specific epigenetic modifications such as methylation patterns [5, 9]. The tumor-specific fraction in plasma can vary from 0.01% to more than 90% [5]. Lower-stage tumors have lower levels of cfDNA shedding compared to advanced disease [29]. Therefore, highly sensitive methods are required for detection of cfDNA in early disease [29, 30].
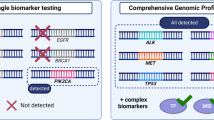
Polymerase chain reaction (PCR) approaches, or next-generation sequencing (NGS), has dominated molecular testing of cfDNA [5]. PCR methods include ARMS-Scorpion PCR (amplification refractory mutation system), PCR-SSCP (single-strand conformation polymorphism), ME-PCR (mutant enriched), MASA-PCR (mutant allele–specific amplification), PAP-A amplification (pyrophosphorolysis-activated polymerization allele-specific amplification), or RFLP-PCR (restriction fragment length polymorphism) or similar (Table 14.1) [31,32,33,34,35,36]. However, molecular testing of cfDNA requires very high sensitivity to detect specific alterations with very low allele fractions. Therefore, novel methods using digital PCR such as droplet-based systems or the use of beads, emulsions, amplification, and magnetics (BEAMing), or microfluidic assays, are increasingly used [17, 21, 37,38,39,40,41,42,43,44]. The most significant limitation of PCR is its inability to simultaneously detect a large spectrum of aberrations.
Unlike PCR, NGS allows detection of multiple alterations across wider regions of the cancer genome. The specific regions of cfDNA can be analyzed by using targeted deep-sequencing techniques such as TAm-Seq (tagged amplicon deep sequencing) , Ion AmpliSeq, Safe-Seq (safe-sequencing system), CAPP-seq (cancer personalized profiling by deep sequencing), digital sequencing or other methods [8, 14, 45,46,47,48,49]. The most comprehensive techniques include whole-exome and whole-genome sequencing of plasma samples; however, these approaches are less reliable in samples with lower content of ctDNA [5, 45, 50, 51]. The advantages of PCR-based and NGS-based approaches are summarized in Table 14.2.
14.3 Identification of Molecular Targets for Treatment
The feasibility of molecular testing of cfDNA was tested by comparing its concordance with molecular testing of tumor tissue. In a pilot study of 18 patients with metastatic colorectal cancer who were candidates for surgical resection or radiofrequency ablation, oncogenic mutations (APC, TP53, PIK3CA, and KRAS) were assessed by direct sequencing in tumor tissue, and at least one mutation was identified in each unique tumor [21]. Subsequently, cfDNA isolated from plasma was tested with BEAMing digital PCR. The study demonstrated oncogenic mutations can be detected in cfDNA isolated from plasma in cancer patients.
Interesting insight about factors influencing concordance was offered by a study testing a cohort of patients with advanced breast cancer. First, there was 100% concordance (34 of 34 cases) between BEAMing- detected PIK3CA mutations in plasma cfDNA and in tumor tissues in a cohort with simultaneous plasma and tumor collection; however, the concordance decreased to 79% in the second cohort of 60 patients when tumor samples and plasma cfDNA were obtained at different time points [39]. The relationship between concordance and time between specimen collection has been demonstrated by other studies. For instance, results of a single institution study in 168 patients with advanced cancers demonstrated that targeted digital NGS of plasma cfDNA misses known mutations in 4 major oncogenes (TP53, EGFR, PIK3CA and ERBB2) in 22–33% if the interval between tumor tissue and plasma acquisition is 6 months or less compared to 31% to 39% if the interval between tumor tissue and plasma acquisition is more than 6 months [52]. In a study of 157 patients with advanced cancer that progressed on systemic therapy who were referred for treatment with experimental targeted therapies, a panel of 21 oncogenic mutations in the BRAF, EGFR, KRAS, and PIK3CA genes was assessed in plasma cfDNA by BEAMing technology. The results demonstrated acceptable concordance (BRAF, 91%; EGFR, 99%; KRAS, 83%; PIK3CA , 91%) with results of standard-of-care mutation analysis of primary or metastatic tumor tissue obtained during clinical care [38].
Thierry et al. tested KRAS and BRAF mutations in plasma-derived cfDNA from 106 patients with metastatic colorectal cancer using allele-specific quantitative PCR and compared results to standard-of-care testing of tumor tissue and demonstrated for plasma testing 100% specificity and sensitivity for the BRAF V600E mutation and 98% specificity and 92% sensitivity for the common KRAS mutations [53].
Forshew et al. [49] tested the TAm-Seq method for identification and monitoring of oncogenic mutations in plasma cfDNA. Investigators screened 5995 genomic bases in coding regions of TP53 and PTEN, and selected regions of EGFR, BRAF, KRAS, and PIK3CA for low-frequency mutations. The assay was able to detect mutations in cfDNA with sensitivity and specificity of >97%. Moreover, in one patient with synchronous primary cancers of the bowel and ovary, disease relapse was identified as being derived from the original ovarian tumor. A plasma sample collected at relapse revealed the TP53 mutation originally found in the ovarian primary tumor, whereas the colorectal cancer-associated mutations were not detected.
Newman et al. [48] developed CAPP-Seq, an ultrasensitive NGS-based method for quantifying tumor-derived plasma cfDNA by targeting recurrently mutated regions in the cancer of interest. In patients with non-small cell lung cancer, the CAPP-Seq method was able to detect cfDNA in 100% of patients with stage II–IV disease and 50% of patients with stage I disease. The method specificity was 96% for mutant allele fractions as low as 0.02%.
In addition, we performed a series of comparative studies, which demonstrated that concordance for plasma and tumor tissue samples collected non-synchronously in common metastatic cancers ranges from 80% to >90% for digital PCR technologies and from about 70% to 80% for NGS [8, 37, 38].
In a prospective study published by Sacher et al. [17] in metastatic non-small cell lung cancer (NSCLC) it was demonstrated that ddPCR testing for KRAS and EGFR mutations has high sensitivity (64%–86%) and specificity (100%) for initiating mutations. In addition, molecular testing of plasma-derived cfDNA was associated with shorter processing timelines compared to simultaneous molecular testing of tumor tissue.
Another study in patients with EGFR-mutated NSCLC previously treated with first generation EGFR tyrosine kinase inhibitors demonstrated that molecular testing of plasma cfDNA before starting on third generation EGFR inhibitor osimertinib reliably detects patients with EGFRT790M mutations who benefit from therapy with an objective response rate (ORR) of 63% [54]. However, in patients lacking plasma EGFRT790M mutations, the reported ORR to osimertinib was 46%, and the majority of patients with tumor shrinkage had EGFRT790M mutations detected in tumor tissue. These data suggest that molecular testing of cfDNA might be acceptable as an initial test; however, negative results for mutations of therapeutic interest may warrant tissue confirmation (Fig. 14.2).
Finally, novel targeted NGS approaches covering a larger portion of the genome expanded ctDNA molecular diagnostics to include tumor mutation burden (TMB) testing in order to predict efficacy of PD-L1-based immune checkpoint inhibitors [55]. Early data suggest that high TMB in plasma cfDNA is an actionable marker predicting favorable outcomes for immune checkpoint inhibitors in NSCLC.
14.4 Assessment of Prognosis
The quantification of total and/or mutant cfDNA has been studied for prognosis assessment in various tumor types. Some studies demonstrated that, in cancer patients, higher levels of cfDNA are associated with higher risk of disease recurrence and progression [8, 21, 37, 38, 47, 52, 56,57,58,59]. In a study by Diehl et al. [21] in 18 colorectal cancer patients, the absence of cfDNA in plasma during the first follow-up visit after surgical resection was associated with 100% recurrence-free survival.
Early limited data suggested that persistence of TP53 mutations in plasma cfDNA of patients with stage II or III breast cancer that were in remission was associated with higher likelihood of disease recurrence; however, the small sample size precluded any definitive conclusion [32]. In a very preliminary study in 11 colorectal cancer patients who underwent surgery, primary tumors and corresponding plasma samples were screened for KRAS mutations and p16INK4a promoter hypermethylation [34]. On follow up, these alterations were identified in plasma cfDNA only from patients with disease recurrence.
The amount of mutant cfDNA has been found to be of prognostic significance. Spindler et al. [58] demonstrated the prognostic value of the amount of total cfDNA and KRAS mutant cfDNA in a study of 108 patients with metastatic colorectal cancer treated with third-line cetuximab and irinotecan. Patients with higher cfDNA levels had shorter progression-free survival (PFS; 2.1 vs. 4.4 months; P = 0.0015) and overall survival (OS; 3.6 vs. 10.4 months; P < 0.0001) than patients with lower cfDNA levels. Similarly, patients with higher levels of KRAS-mutant cfDNA had shorter PFS (1.8 vs. 2.3 months; P = 0.008) and OS (2.1 vs. 5 months; P = 0.0005) than patients with lower levels of KRAS-mutant cfDNA.
The previously mentioned study, which evaluated BEAMing for the detection of 21 mutations in BRAF, EGFR, KRAS, and PIK3CA in plasma cfDNA of 157 patients with advanced cancer, also examined the prognostic impact of the amount of mutated plasma cfDNA [38]. A higher percentage of mutant cfDNA (>1% [n = 67 patients] vs. ≤1% [n = 33 patients]), irrespective of mutation type, was associated with a shorter OS (5.5 vs. 9.8 months; P = 0.001), which was confirmed in a multivariable analysis. Similarly, 41 patients with >1% of KRAS mutant (codon 12 or 13) cfDNA had a shorter median OS than 20 patients with ≤1% of KRAS mutant cfDNA (4.8 vs. 7.3 months; P = 0.008). Significant differences in OS were not observed for mutations in other examined genes, likely due to the small sample size.
In another study of 246 patients with advanced non-small-cell lung carcinoma (NSCLC) treated with platinum and vinorelbine chemotherapy, the patients with detectable plasma KRAS mutant (codon 12 or 13) cfDNA had a shorter median OS (4.8 vs 9.5 months; P = 0.0002) and shorter median PFS (3.0 vs 5.6 months; P = 0.0043) than patients whose cancer expressed wild-type KRAS [59]. A multivariate analysis confirmed the independent prognostic value of KRAS mutant cfDNA in OS but not in PFS. Wang et al. [60] showed the negative prognostic effect of KRAS mutations (codon 12 or 13) in plasma cfDNA of 273 patients with advanced NSCLC. The median PFS of patients with a plasma KRAS mutation was 2.5 months, while that of patients with wild-type KRAS was 8.8 months (P < 0.001).
In a study of 44 pancreatic cancer patients, the 1-year survival rate was 0% in those with KRAS codon-12 mutations in cfDNA, and 24% in those with KRAS wild-type in cfDNA (P < 0.005), and plasma KRAS mutation status was the only independent prognostic factor (odds ratio, 1.51; 95% confidence interval [CI], 1.02–2.23) [36]. In 103 patients with melanoma receiving biochemotherapy, those with a BRAF mutation in serum cfDNA had significantly shorter OS than those that did not have the BRAF mutation in serum cfDNA (13 vs. 30.6 months, P = 0.039) [61].
The negative prognostic impact of increased levels of mutant cfDNA was supported by other studies in breast cancer, colorectal cancer, ovarian cancer, and other tumor types [62,63,64,65]. Furthermore, the presence of other tumor-related genomic cfDNA aberrations was associated with poor prognosis. Detection of loss of heterozygosity and microsatellite instability in cfDNA was associated with worse prognosis for patients with breast cancer, ovarian cancer, melanoma, lung cancer, or other tumor types [66,67,68,69].
14.5 Efficacy Assessment and Monitoring
The liquid biopsy could be used as a minimally invasive way to predict and monitor therapy response in real time (Fig. 14.3) [5]. Arguably, because of the relatively short half-life of cfDNA, its changes might indicate therapeutic response, or lack of there of, earlier than conventional imaging, which is typically done after several weeks or even months of therapy [70]. In addition, early data suggest that molecular testing of dynamic changes in ctDNA can help to differentiate progression from pseudo-progression in patients treated with immunotherapy [71].
Concept of dynamic tracking of circulating tumor DNA (ctDNA) to assess response to therapy. Blue line indicates % variant allele frequency (VAF) in the circulation and red line the sum of target lesions per RECIST criteria (please note that increase at time points 2 and 3 indicate pseudoprogression)
In a study of 1060 patients with advanced NSCLC treated with gefitinib, EGFR mutations were detected in primary tumors and corresponding plasma samples [72]. ORR were 76.9% (95% CI, 65.4–85.5) for patients with detected mutations in both tumor and plasma and 59.5% (95% CI, 43.5–73.7) for patients with mutation in the tumor but not in plasma, which demonstrated that EGFR mutation status could be assessed in cfDNA and serve as a positive predictive biomarker for targeted therapy.
In contrast, another study assessed BRAF mutations in plasma cfDNA from 160 patients with advanced cancer and known BRAF status from archival tumor samples [57]. Patients whose archival tumor samples had a BRAFV600 mutation (n = 51) received therapy with a BRAF and/or MEK inhibitor. The time to treatment failure (TTF) of 13 patients with a BRAFV600 mutations in the tumor but not in plasma obtained before therapy was significantly longer than that of 38 patients whose baseline plasma cfDNA had a BRAFV600 mutation (13.1 vs. 3.0 months; P = 0.001). The absence of BRAFV600–mutant cfDNA also was associated with longer TTF (HR, 0.31; P = 0.004) in multivariate analysis.
Dynamic tracking of ctDNA was investigated in a prospective study of 52 patients with metastatic breast cancer [40]. The plasma cfDNA was monitored to qualitatively and quantitatively assess disease progression and treatment response and compare with levels of circulating tumor cells (CTC), tumor marker cancer antigen 15-3 (CA15-3), and computed tomography (CT) imaging. The cfDNA was detected by identification of the same PIK3CA and TP53 mutations and structural variations as were found in the tumor tissues. The levels of cfDNA in plasma generally correlated well with the treatment response assessed by CT imaging (as defined by Response Evaluation Criteria in Solid Tumors) [73, 74]. However, two patients in this study had discordant correlations. In 10 of the 19 patients who experienced disease progression, the cfDNA levels increased at one or more consecutive time points, on average 5 months before progressive disease was observed on imaging. Moreover, the cfDNA was found to be a more accurate biomarker for monitoring metastatic disease than CTCs, CA 15-3, or CT imaging.
Another study with 72 patients with advanced NSCLC examined the dynamic changes in cfDNA EGFR mutations as a predictor of response to EGFR tyrosine-kinase inhibitor targeted therapy [75]. Failure to clear plasma EGFR mutations after EGFR tyrosine kinase inhibitors (TKIs) was an independent predictor for shorter PFS (hazard ratio [HR] 1.97, P = 0.001) and OS (HR 1.82, P = 0.036). The EGFR mutations were detected by ddPCR in serial plasma samples of non-small cell lung cancer patients treated with erlotinib [76]. The study demonstrated the disappearance of EGFR mutations in exon 19 and 21 and the emergence of EGFRT790M resistance mutations several weeks before radiographic disease progression.
Other studies showed that patients with advanced cancers and decrease in ctDNA on therapy compared to those with no change or increase have favorable therapeutic outcomes such as TTF [8, 9, 19]. However, it remains unclear how to translate these findings to the individualized treatment of cancer patients.
Overall, dynamic tracking of ctDNA appears to be reliable in scenarios where the cancer is heavily dependent on the alterations included in ctDNA assays (e.g. testing for BRAF mutation in non-Langerhans malignant histiocytosis); however, ctDNA efficacy monitoring seems to be more complicated in tumors with more heterogeneous molecular profiles [18, 37].
14.5.1 Molecular Profiling in Real-Time and Assessment of Target Engagement
Implementing principles of personalized medicine and targeted therapy into routine oncology practice provides an important shift in the treatment of advanced cancers. In metastatic disease, a chronic course is no longer unusual, and patients can survive for many years [77]. However, despite the significant initial therapeutic effect of targeted therapy, the vast majority of patients eventually develop resistance and experience tumor progression. The tumor adaptive resistance results from acquisition of mutations in the targeted genes or signaling pathways of cancer cells under therapeutic selective pressure. The mutations causing resistance also can be present in the infrequent subclones of pretreatment tumor cells and can predict the further failure of targeted therapy [3, 5, 78, 79].
The mechanisms of resistance are often known; however, since routine multiple sequential biopsies are not performed, we have no tools to describe these mechanisms at the level of an individual patient. Both intrinsic and adaptive resistance can occur because of pre-existing or acquired molecular abnormalities, such as emergence of KRAS mutations on treatment with EGFR monoclonal antibodies in metastatic colorectal cancer, or emergence of EGFRT790M mutations which cause resistance to EGFR TKIs in non-small cell lung cancer [42, 54]. Lastly, ALK mutations L1196M or C1156Y mediates adaptive resistance to crizotinib in NSCLC with ALK rearrangement, and mutations in NRAS, MEK, and BRAF amplification indicate resistance to BRAF inhibitor vemurafenib in BRAF-mutant melanoma [80,81,82]. Because liquid biopsies can be obtained at low cost at multiple time points, they offer a useful tool for monitoring molecular changes associated with resistance to certain cancer therapies.
An example of emerging resistance mutations in response to targeted therapy is the acquisition of tumor KRAS mutations in codons 12, 13, or 61 in patients with advanced colorectal cancer treated with anti-EGFR monoclonal antibodies cetuximab or panitumumab [42, 43]. Two landmark studies have shown the possibility of detecting and monitoring these emerging KRAS mutations in patients with colorectal cancer in cfDNA by using BEAMing technology [42, 43]. Testing of serum cfDNA from 28 colorectal cancer patients receiving panitumumab showed that 9 of 24 patients whose tumor and cfDNA were initially KRAS wild-type had developed detectable cfDNA KRAS mutations [43]. Interestingly, multiple KRAS cfDNA mutations were detected in three individuals. The appearance of mutations generally occurred between 5 and 6 months following initiation of treatment. In the second study, emergence of KRAS aberrations was found in tumor tissue samples from metastatic sites obtained after initiation of therapy [42]. Corresponding plasma samples also showed emergence of KRAS mutations in cfDNA, which may have occurred as early as 10 months before radiographic progression [42]. Furthermore, our group at MD Anderson Cancer Center, using BEAMing technology, reported acquired KRAS and/or EGFR ectodomain mutations in 44% (27/62) and 8% (5/62) of plasma samples from patients with advanced colorectal cancer treated with cetuximab or panitumumab, respectively [83]. KRAS codon 61 and 146 mutations were predominant (33% and 11%, respectively).
Even if the candidate-gene techniques to monitor emerging resistance mutations to various targeted therapeutics provide promising results, such approaches have substantial drawbacks, most notably the requirement for prior knowledge of mechanisms of resistance and corresponding mutations. Application of unbiased approaches for detecting emergence of resistant cancer cell subclones using NGS technologies directly on the plasma samples could overcome these limitations. A proof-of-principle study by Murtaza et al. [45] monitored cancer clonal evolution and the acquisition of secondary resistance mutations to various anticancer treatments in serial plasma samples from six patients with advanced breast, ovarian, or lung cancer using unbiased whole-exome sequencing. Follow-up intervals were 1–2 years, and the exome sequencing was performed on two to five plasma samples in each patient. The results revealed emergence of distinct secondary mutations, such as an activating mutation in PIK3CA after paclitaxel, a truncating mutation in RB1 after cisplatin, a truncating mutation in MED1 after tamoxifen and trastuzumab and a splicing mutation in GAS6 after subsequent treatment with lapatinib in the same patient, and an EGFR T790M mutation after treatment with gefitinib. The results of this study established that exome-wide analysis of cfDNA could complement standard biopsy to detect mutations associated with acquired resistance to therapeutic agents in advanced cancers. However, it should be noted that the detected mutant allele fractions for the aberrations were rather high (3%–45%), which can limit the applicability of such an approach to a limited subset of patients.
Recently, molecular testing of cfDNA was tested as a tool to assess pharmacodynamic endpoints in clinical trials. One of the examples was an early phase development of a novel switch pocket KIT and PDGFR inhibitor ripretinib [84]. Serial collections of blood samples from patients treated with ripretinib showed significant decrease in KIT-mutated ctDNA confirming on-target effects of therapy.
14.6 Conclusions
Liquid biopsy offers an attractive tool for identification of molecular targets for cancer therapy, determination of prognosis, assessment of response to anticancer therapy, real-time monitoring of cancer molecular profiles, and assessment of target engagement. Liquid biopsies are increasingly accepted as a clinical tool to detect molecular targets for cancer therapy; however, the clinical utility of other applications, such as dynamic tracking during therapy, remain to be proven in prospective studies. Furthermore, cfDNA consists of both nonmalignant and tumor DNA, and the tumor DNA fraction can be relatively small. This issue increases the demand for higher sensitivity testing, which is associated with higher cost and often prevents some more comprehensive approaches such as whole-genome or -exome NGS.
Key Expert Opinion Points
-
Knowing the cancer genomic profile with underlying druggable molecular alterations is important for the optimal choice of cancer therapy.
-
Molecular analysis of tumor DNA can be limited by the availability of the cancer tissue, which has to be obtained from therapeutic or diagnostic procedures.
-
Molecular analysis of liquid biopsies utilizing the circulating tumor cell-free DNA offers a minimally invasive and low-risk method that can be performed at multiple time-points for molecular analysis.
-
Molecular testing of cell-free DNA can be used in multiple clinically useful applications, such as identification of molecular targets for cancer therapy, assessment of cancer prognosis, monitoring of response to cancer therapy, monitoring of tumor molecular profile in real time and study target engagement when developing new therapies.
References
Rodon J, Soria JC, Berger R, et al. Genomic and transcriptomic profiling expands precision cancer medicine: the WINTHER trial. Nat Med. 2019;25:751–8.
Meric-Bernstam F, Brusco L, Shaw K, et al. Feasibility of large-scale genomic testing to facilitate enrollment onto genomically matched clinical trials. J Clin Oncol. 2015;33:2753–62.
Gerlinger M, Rowan AJ, Horswell S, et al. Intratumor heterogeneity and branched evolution revealed by multiregion sequencing. N Engl J Med. 2012;366:883–92.
Janku F. Tumor heterogeneity in the clinic: is it a real problem? Ther Adv Med Oncol. 2014;6:43–51.
Polivka J Jr, Pesta M, Janku F. Testing for oncogenic molecular aberrations in cell-free DNA-based liquid biopsies in the clinic: are we there yet? Expert Rev Mol Diagn. 2015;15:1631–44.
Mandel P, Metais P. Les Acides Nucleiques Du Plasma Sanguin Chez Lhomme. Cr Soc Biol. 1948;142:241–3.
Diehl F, Li M, Dressman D, et al. Detection and quantification of mutations in the plasma of patients with colorectal tumors. Proc Natl Acad Sci U S A. 2005;102:16368–73.
Janku F, Zhang S, Waters J, et al. Development and validation of an ultra-deep next-generation sequencing assay for testing of plasma cell-free DNA from patients with advanced cancer. Clin Cancer Res. 2017;23(18):5648–56.
Liu L, Toung JM, Jassowicz AF, et al. Targeted methylation sequencing of plasma cell-free DNA for cancer detection and classification. Ann Oncol. 2018;29(6):1445–53.
Pan W, Gu W, Nagpal S, Gephart MH, Quake SR. Brain tumor mutations detected in cerebral spinal fluid. Clin Chem. 2015;61:514–22.
Shi W, Lv C, Qi J, et al. Prognostic value of free DNA quantification in serum and cerebrospinal fluid in glioma patients. J Mol Neurosci. 2012;46:470–5.
Wang Y, Springer S, Zhang M, et al. Detection of tumor-derived DNA in cerebrospinal fluid of patients with primary tumors of the brain and spinal cord. Proc Natl Acad Sci U S A. 2015;112:9704–9.
Lanman RB, Mortimer SA, Zill OA, et al. Analytical and clinical validation of a digital sequencing panel for quantitative, highly accurate evaluation of cell-free circulating tumor DNA. PLoS One. 2015;10:e0140712.
Odegaard JI, Vincent JJ, Mortimer S, et al. Validation of a plasma-based comprehensive cancer genotyping assay utilizing orthogonal tissue- and plasma-based methodologies. Clin Cancer Res. 2018;24(15):3539–49.
Zill OA, Banks KC, Fairclough SR, et al. The landscape of actionable genomic alterations in cell-free circulating tumor DNA from 21,807 advanced cancer patients. Clin Cancer Res. 2018;24:3528–38.
Zill OA, Greene C, Sebisanovic D, et al. Cell-free DNA next-generation sequencing in pancreatobiliary carcinomas. Cancer Discov. 2015;5(10):1040–8.
Sacher AG, Paweletz C, Dahlberg SE, et al. Prospective validation of rapid plasma genotyping for the detection of EGFR and KRAS mutations in advanced lung cancer. JAMA Oncol. 2016;2(8):1014–22.
Hyman DM, Diamond EL, Vibat CR, et al. Prospective blinded study of BRAFV600E mutation detection in cell-free DNA of patients with systemic histiocytic disorders. Cancer Discov. 2015;5:64–71.
Fujii T, Barzi A, Sartore-Bianchi A, et al. Mutation-enrichment next-generation sequencing for quantitative detection of KRAS mutations in urine cell-free DNA from patients with advanced cancers. Clin Cancer Res. 2017;23:3657–66.
Husain H, Nykin D, Bui N, et al. Cell-free DNA from ascites and pleural effusions: molecular insights into genomic aberrations and disease biology. Mol Cancer Ther. 2017;16:948–55.
Diehl F, Schmidt K, Choti MA, et al. Circulating mutant DNA to assess tumor dynamics. Nat Med. 2008;14:985–90.
Mouliere F, Robert B, Arnau Peyrotte E, et al. High fragmentation characterizes tumour-derived circulating DNA. PLoS One. 2011;6:e23418.
Jahr S, Hentze H, Englisch S, et al. DNA fragments in the blood plasma of cancer patients: quantitations and evidence for their origin from apoptotic and necrotic cells. Cancer Res. 2001;61:1659–65.
Lapin M, Oltedal S, Tjensvoll K, et al. Fragment size and level of cell-free DNA provide prognostic information in patients with advanced pancreatic cancer. J Transl Med. 2018;16:300.
El Messaoudi S, Rolet F, Mouliere F, Thierry AR. Circulating cell free DNA: preanalytical considerations. Clin Chim Acta. 2013;424:222–30.
Warton K, Yuwono NL, Cowley MJ, McCabe MJ, So A, Ford CE. Evaluation of streck BCT and PAXgene stabilised blood collection tubes for cell-free circulating DNA studies in plasma. Mol Diagn Ther. 2017;21:563–70.
Wong D, Moturi S, Angkachatchai V, et al. Optimizing blood collection, transport and storage conditions for cell free DNA increases access to prenatal testing. Clin Biochem. 2013;46:1099–104.
Janku F, Vibat CR, Kosco K, et al. BRAF V600E mutations in urine and plasma cell-free DNA from patients with Erdheim-Chester disease. Oncotarget. 2014;5:3607–10.
Cohen JD, Li L, Wang Y, et al. Detection and localization of surgically resectable cancers with a multi-analyte blood test. Science. 2018;359:926–30.
Chan KCA, Woo JKS, King A, et al. Analysis of plasma Epstein-Barr virus DNA to screen for nasopharyngeal cancer. New Engl J Med. 2017;377:513–22.
Board RE, Wardley AM, Dixon JM, et al. Detection of PIK3CA mutations in circulating free DNA in patients with breast cancer. Breast Cancer Res Treat. 2010;120:461–7.
Chen Z, Feng J, Buzin CH, et al. Analysis of cancer mutation signatures in blood by a novel ultra-sensitive assay: monitoring of therapy or recurrence in non-metastatic breast cancer. PLoS One. 2009;4:e7220.
Wang JY, Hsieh JS, Chang MY, et al. Molecular detection of APC, K-ras, and p53 mutations in the serum of colorectal cancer patients as circulating biomarkers. World J Surg. 2004;28:721–6.
Frattini M, Gallino G, Signoroni S, et al. Quantitative and qualitative characterization of plasma DNA identifies primary and recurrent colorectal cancer. Cancer Lett. 2008;263:170–81.
Yamada T, Nakamori S, Ohzato H, et al. Detection of K-ras gene mutations in plasma DNA of patients with pancreatic adenocarcinoma: correlation with clinicopathological features. Clin Cancer Res. 1998;4:1527–32.
Castells A, Puig P, Mora J, et al. K-ras mutations in DNA extracted from the plasma of patients with pancreatic carcinoma: diagnostic utility and prognostic significance. J Clin Oncol. 1999;17:578–84.
Janku F, Huang HJ, Fujii T, et al. Multiplex KRASG12/G13 mutation testing of unamplified cell-free DNA from the plasma of patients with advanced cancers using droplet digital polymerase chain reaction. Ann Oncol. 2017;28:642–50.
Janku F, Angenendt P, Tsimberidou AM, et al. Actionable mutations in plasma cell-free DNA in patients with advanced cancers referred for experimental targeted therapies. Oncotarget. 2015;6:12809–21.
Higgins MJ, Jelovac D, Barnathan E, et al. Detection of tumor PIK3CA status in metastatic breast cancer using peripheral blood. Clin Cancer Res. 2012;18:3462–9.
Dawson SJ, Tsui DW, Murtaza M, et al. Analysis of circulating tumor DNA to monitor metastatic breast cancer. N Engl J Med. 2013;368:1199–209.
Mohrmann L, Huang H, Hong DS, et al. Liquid biopsies using plasma exosomal nucleic acids and plasma cell-free DNA compared with clinical outcomes of patients with advanced cancers. Clin Cancer Res. 2017;24(1):181–8.
Misale S, Yaeger R, Hobor S, et al. Emergence of KRAS mutations and acquired resistance to anti-EGFR therapy in colorectal cancer. Nature. 2012;486:532–6.
Diaz LA Jr, Williams RT, Wu J, et al. The molecular evolution of acquired resistance to targeted EGFR blockade in colorectal cancers. Nature. 2012;486:537–40.
Cai X, Janku F, Zhan Q, Fan JB. Accessing genetic information with liquid biopsies. Trends Genet. 2015;31:564–75.
Murtaza M, Dawson SJ, Tsui DW, et al. Non-invasive analysis of acquired resistance to cancer therapy by sequencing of plasma DNA. Nature. 2013;497:108–12.
Carreira S, Romanel A, Goodall J, et al. Tumor clone dynamics in lethal prostate cancer. Sci Transl Med. 2014;6:254ra125.
Bettegowda C, Sausen M, Leary RJ, et al. Detection of circulating tumor DNA in early- and late-stage human malignancies. Sci Transl Med. 2014;6:224ra24.
Newman AM, Bratman SV, To J, et al. An ultrasensitive method for quantitating circulating tumor DNA with broad patient coverage. Nat Med. 2014;20:548–54.
Forshew T, Murtaza M, Parkinson C, et al. Noninvasive identification and monitoring of cancer mutations by targeted deep sequencing of plasma DNA. Sci Transl Med. 2012;4:136ra68.
Chan KC, Jiang P, Zheng YW, et al. Cancer genome scanning in plasma: detection of tumor-associated copy number aberrations, single-nucleotide variants, and tumoral heterogeneity by massively parallel sequencing. Clin Chem. 2013;59:211–24.
Heitzer E, Ulz P, Belic J, et al. Tumor-associated copy number changes in the circulation of patients with prostate cancer identified through whole-genome sequencing. Genome Med. 2013;5:30.
Schwaederle M, Husain H, Fanta PT, et al. Use of liquid biopsies in clinical oncology: pilot experience in 168 patients. Clin Cancer Res. 2016;22:5497–505.
Thierry AR, Mouliere F, El Messaoudi S, et al. Clinical validation of the detection of KRAS and BRAF mutations from circulating tumor DNA. Nat Med. 2014;20:430–5.
Oxnard GR, Thress KS, Alden RS, et al. Association between plasma genotyping and outcomes of treatment with osimertinib (AZD9291) in advanced non-small-cell lung cancer. J Clin Oncol. 2016;34:3375–82.
Gandara DR, Paul SM, Kowanetz M, et al. Blood-based tumor mutational burden as a predictor of clinical benefit in non-small-cell lung cancer patients treated with atezolizumab. Nat Med. 2018;24:1441–8.
Hashad D, Sorour A, Ghazal A, Talaat I. Free circulating tumor DNA as a diagnostic marker for breast cancer. J Clin Lab Anal. 2012;26:467–72.
Janku F, Huang HJ, Claes B, et al. BRAF mutation testing in cell-free DNA from the plasma of patients with advanced cancers using a rapid, automated molecular diagnostics system. Mol Cancer Ther. 2016;15:1397–404.
Spindler KL, Pallisgaard N, Vogelius I, Jakobsen A. Quantitative cell-free DNA, KRAS, and BRAF mutations in plasma from patients with metastatic colorectal cancer during treatment with cetuximab and irinotecan. Clin Cancer Res. 2012;18:1177–85.
Nygaard AD, Garm Spindler KL, Pallisgaard N, Andersen RF, Jakobsen A. The prognostic value of KRAS mutated plasma DNA in advanced non-small cell lung cancer. Lung Cancer. 2013;79:312–7.
Wang S, An T, Wang J, et al. Potential clinical significance of a plasma-based KRAS mutation analysis in patients with advanced non-small cell lung cancer. Clin Cancer Res. 2010;16:1324–30.
Shinozaki M, O’Day SJ, Kitago M, et al. Utility of circulating B-RAF DNA mutation in serum for monitoring melanoma patients receiving biochemotherapy. Clin Cancer Res. 2007;13:2068–74.
Silva JM, Silva J, Sanchez A, et al. Tumor DNA in plasma at diagnosis of breast cancer patients is a valuable predictor of disease-free survival. Clin Cancer Res. 2002;8:3761–6.
Lefebure B, Charbonnier F, Di Fiore F, et al. Prognostic value of circulating mutant DNA in unresectable metastatic colorectal cancer. Ann Surg. 2010;251:275–80.
Trevisiol C, Di Fabio F, Nascimbeni R, et al. Prognostic value of circulating KRAS2 gene mutations in colorectal cancer with distant metastases. Int J Biol Markers. 2006;21:223–8.
Swisher EM, Wollan M, Mahtani SM, et al. Tumor-specific p53 sequences in blood and peritoneal fluid of women with epithelial ovarian cancer. Am J Obstet Gynecol. 2005;193:662–7.
Schwarzenbach H, Eichelser C, Kropidlowski J, Janni W, Rack B, Pantel K. Loss of heterozygosity at tumor suppressor genes detectable on fractionated circulating cell-free tumor DNA as indicator of breast cancer progression. Clin Cancer Res. 2012;18:5719–30.
Kuhlmann JD, Schwarzenbach H, Wimberger P, Poetsch M, Kimmig R, Kasimir-Bauer S. LOH at 6q and 10q in fractionated circulating DNA of ovarian cancer patients is predictive for tumor cell spread and overall survival. BMC Cancer. 2012;12:325.
Fujimoto A, O’Day SJ, Taback B, Elashoff D, Hoon DS. Allelic imbalance on 12q22-23 in serum circulating DNA of melanoma patients predicts disease outcome. Cancer Res. 2004;64:4085–8.
Sozzi G, Conte D, Mariani L, et al. Analysis of circulating tumor DNA in plasma at diagnosis and during follow-up of lung cancer patients. Cancer Res. 2001;61:4675–8.
Husain H, Melnikova VO, Kosco K, et al. Monitoring daily dynamics of early tumor response to targeted therapy by detecting circulating tumor DNA in urine. Clin Cancer Res. 2017;23:4716–23.
Lee JH, Long GV, Menzies AM, et al. Association between circulating tumor DNA and pseudoprogression in patients with metastatic melanoma treated with anti-programmed cell death 1 antibodies. JAMA Oncol. 2018;4:717–21.
Douillard JY, Ostoros G, Cobo M, et al. Gefitinib treatment in EGFR mutated caucasian NSCLC: circulating-free tumor DNA as a surrogate for determination of EGFR status. J Thorac Oncol. 2014;9:1345–53.
Eisenhauer EA, Therasse P, Bogaerts J, et al. New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer. 2009;45:228–47.
Therasse P, Arbuck SG, Eisenhauer EA, et al. New guidelines to evaluate the response to treatment in solid tumors. European Organization for Research and Treatment of Cancer, National Cancer Institute of the United States, National Cancer Institute of Canada. J Natl Cancer Inst. 2000;92:205–16.
Tseng JS, Yang TY, Tsai CR, et al. Dynamic plasma EGFR mutation status as a predictor of EGFR-TKI efficacy in patients with EGFR-mutant lung adenocarcinoma. J Thorac Oncol. 2015;10:603–10.
Oxnard GR, Paweletz CP, Kuang Y, et al. Noninvasive detection of response and resistance in EGFR-mutant lung cancer using quantitative next-generation genotyping of cell-free plasma DNA. Clin Cancer Res. 2014;20:1698–705.
Normanno N, Rachiglio AM, Roma C, et al. Molecular diagnostics and personalized medicine in oncology: challenges and opportunities. J Cell Biochem. 2013;114:514–24.
Crowley E, Di Nicolantonio F, Loupakis F, Bardelli A. Liquid biopsy: monitoring cancer-genetics in the blood. Nat Rev Clin Oncol. 2013;10:472–84.
Ramos P, Bentires-Alj M. Mechanism-based cancer therapy: resistance to therapy, therapy for resistance. Oncogene. 2015;34:3617–26.
Choi YL, Soda M, Yamashita Y, et al. EML4-ALK mutations in lung cancer that confer resistance to ALK inhibitors. N Engl J Med. 2010;363:1734–9.
Long GV, Fung C, Menzies AM, et al. Increased MAPK reactivation in early resistance to dabrafenib/trametinib combination therapy of BRAF-mutant metastatic melanoma. Nat Commun. 2014;5:5694.
Mao M, Tian F, Mariadason JM, et al. Resistance to BRAF inhibition in BRAF-mutant colon cancer can be overcome with PI3K inhibition or demethylating agents. Clin Cancer Res. 2013;19:657–67.
Morelli MP, Overman MJ, Dasari A, et al. Characterizing the patterns of clonal selection in circulating tumor DNA from patients with colorectal cancer refractory to anti-EGFR treatment. Ann Oncol. 2015;26:731–6.
Smith BD, Kaufman MD, Lu WP, et al. Ripretinib (DCC-2618) is a switch control kinase inhibitor of a broad spectrum of oncogenic and drug-resistant KIT and PDGFRA variants. Cancer Cell. 2019;35:738–51.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Janku, F. (2020). Incorporating Circulating Biomarkers into Clinical Trials. In: Yap, T.A., Rodon, J., Hong, D.S. (eds) Phase I Oncology Drug Development. Springer, Cham. https://doi.org/10.1007/978-3-030-47682-3_14
Download citation
DOI: https://doi.org/10.1007/978-3-030-47682-3_14
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-47681-6
Online ISBN: 978-3-030-47682-3
eBook Packages: MedicineMedicine (R0)