Abstract
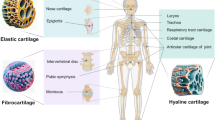
Chondral and osteochondral lesions are extremely challenging scenarios in orthopedic health due to their lack of regenerative and repair abilities. 3D bioprinting is an emerging technology with great applications in this field, as it can be used to build constructs that can mimic cartilage anatomy and physiology. 3D bioprinting is the process of dispensing a biocompatible material (bio-ink) in a precise layer-by-layer pattern, creating a three-dimensional cellular construct that preserves cell function and viability and can be expected to mimic the physiological behavior of the native tissue. It is a three-step process: preprinting, where a design is created using computer-aided design (CAD) software to generate a GCode, which is read by the 3D printer; bioprinting, where a cell-laden hydrogel is extruded in a layer-by-layer fashion creating a 3D rendering of the design; and post-printing, where a construct may be incubated and put through various analyses to evaluate properties of the construct and cell viability after undergoing the mechanical stress of printing. This chapter describes and illustrates the workflow of 3D printing and bioprinting, important considerations in the selection of biomaterials, criteria for an ideal bio-ink, and applications of 3D bioprinting in the field of medical research and healthcare and finally its application into cartilage repair.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
21.1 Introduction
Chondral and osteochondral lesions are extremely challenging scenarios in orthopedic health due to their lack of regenerative and repair abilities. 3D bioprinting is an emerging technology with great applications in this field, as it can be used to build constructs that can mimic cartilage anatomy and physiology. 3D bioprinting is the process of dispensing a biocompatible material (bio-ink) in a precise layer-by-layer pattern, creating a three-dimensional cellular construct that preserves cell function and viability and can be expected to mimic the physiological behavior of the native tissue. It is a three-step process: preprinting, where a design is created using computer-aided design (CAD) software to generate a GCode, which is read by the 3D printer; bioprinting, where a cell-laden hydrogel is extruded in a layer-by-layer fashion creating a 3D rendering of the design; and post-printing, where a construct may be incubated and put through various analyses to evaluate properties of the construct and cell viability after undergoing the mechanical stress of printing. This chapter describes and illustrates the workflow of 3D printing and bioprinting, important considerations in the selection of biomaterials, criteria for an ideal bio-ink, and applications of 3D bioprinting in the field of medical research and healthcare and finally its application into cartilage repair.
21.2 The Illustrations
The Basics of 3D Printing. 3D printing is a process in which a physical object is produced from a three-dimensional digital model, typically by laying down many successive thin layers of a material. A broad array of machines are available, and a wide variety of printing techniques can be implemented to create these objects. (a) A sample 3D printer, MakerBot Replicator+. © MakerBot Industries, LLC 2016 [1]. (b) Basic schematic for the process of 3D printing involving extrusion of the thermoplastic filament through a heated extruder head, fusing as deposited and solidifying resulting in a 3D construct on the print bed [2]
The Process of 3D Printing. (a) In the process of fused deposition modeling (FDM), a 3D image is rendered using computer-aided design (CAD) software, which is subsequently sent to the printer to create the final 3D construct. (b) In order to be printed, the filament (orange) is fed through a gear into a heated extruder head to achieve a molten state before being delivered via the nozzle. The extruder head temperature is adjusted as per the filament properties, allowing the filament to melt. As the melted filament is extruded through the nozzle and laid on the print bed, the room temperature cools down the filament, solidifying it to the shape it has been deposited in. (c) The printer then deposits successive cross sections of the material to produce the construct. Thermoplastics such as polycaprolactone (PCL), polylactic acid (PLA), and acrylonitrile butadiene styrene (ABS) are commonly used filaments for FDM [3]
What Is “Bio”-Printing?. 3D printing and 3D bioprinting follow the same working principle where a material is extruded to build a 3D construct. However, the former technique uses materials such as metal, thermoplastics, and resin, whereas 3D bioprinting involves the use of biocompatible materials (cell-laden bio-ink) to produce bioengineered structures. Briefly, live cells are mixed homogenously with a biocompatible hydrogel and dispensed layer by layer, creating a three-dimensional construct, as seen in standard 3D printing. The value of bioprinted constructs lies in the preservation of cell viability and function. Bioprinting can be applied to a multitude of disciplines, including regenerative medicine, pharmacokinetics, and basic cell biology. As with standard 3D printing, a variety of machinery, methods, and materials can be utilized [4]
The 3D Bioprinted Cube. A three-dimensional printed cube with porous faces demonstrates the versatility of bio-inks as a medium for 3D printing. Constructs with microstructures offer a greater surface area for cell attachment and proliferation and provide opportunity for targeted delivery of external stimuli, such as growth factors. In an operative setting, structures with flat surfaces are preferred as they are easy to handle. (a) CAD-rendered image of a cube (25 × 25 × 25 mm) with pores (2 × 2 mm) through top and bottom face. (b) Layer-by-layer extrusion of the bio-ink to print the rendered model. (c) Final 3D-printed construct [5]
Ideal Criteria for Hydrogel-Based Bio-Inks in 3D Bioprinting. An ideal biocompatible hydrogel meets five essential criteria: printability, to enable consistent and uniform extrusion of the hydrogel; ability to cross-link, to avoid deformation post-printing and hence contributing to a high construct integrity, that ensures wholeness or strength of a construct through its ability to withstand internal damage due to external environment; shape fidelity, to achieve a 3D construct true to the desired shape and structure; resistance to cytotoxic insult, to maximize therapeutic effect and avoid immunogenicity
Variability in Selection Criteria of Hydrogel-Based Bioprinted Constructs. Hydrogels are proposed to be the best candidates for use as a bio-ink due to their ability to mimic the physiological conditions of extracellular matrix as well as their feasible viscoelastic properties. Viscosity is key in achieving a good printability. A higher viscosity hydrogel exhibits a stronger resolution whereas a less viscous gel proves challenging to print due to instant deformation. One of the key criteria of an ideal bio-ink is shape fidelity, which represents how true a 3D printed construct is to its original design. Certain hydrogels tend to deform post-printing and hence an alternative composition may be required to reinforce the structure. Above is an image of two renditions of the same printing design using two different hydrogels: PF127 (strong shape fidelity) and alginate after cross-linking with calcium chloride (weak shape fidelity). A 3D bioprinted construct must be well cross-linked and maintain its integrity to allow cell proliferation and extracellular matrix formation within the desired structure. A construct with weak integrity may deform or collapse upon handling
Variable Resolution in 3D Bioprinting. Though largely dictated by the rendering software and the printer itself, the resolution of the final printed product can also vary with the type of hydrogel-based bio-ink being used. Using hydrogels is advantageous due to their biocompatibility, biodegradability, and the moist environment they provide facilitating ECM production. Hydrogels are also easily pliable, meaning they could be printed to create a wide range of resolutions by adjusting gel viscosity, nozzle diameter, printing speed, and extrusion pressure. Changing resolutions allow fine control of the ultrastructure of the construct influencing cell migration or accumulation depending on the desired type of tissue. For example, a more porous structure enables exchange of nutrients and provides larger surface area for cell attachment
Commonly Used Bio-Inks and Their Respective Properties. Key elements to be considered when choosing a bio-ink include the printability, cross-linking capacity, shape fidelity, and construct integrity of the medium, as well as its susceptibility to cytotoxic insult (see Figure 21.2.5). Alginate is an anionic polysaccharide that forms a viscous gum on binding with water, and is purified from brown seaweed. Alginate hydrogels have been particularly attractive in would healing, drug delivery, and tissue engineering applications owing to their biocompatibility, ease of gelation, and structural similarity with natural extracellular matrix (ECM). Collagen is a structural protein and a major component of the ECM. Type II collagen is the most predominant in articular and hyaline cartilage and plays an important role in providing tensile strength to the tissue. Since extrusion bioprinting requires the bio-ink to be self-supporting for layer-by-layer fabrication, collagen, which has a relatively lower viscosity, is mixed with alginate for structural reinforcement. Pluronic F127 gels are widely used as drug carriers due to their low toxicity and reverse thermal gelation, making it highly printable. But since it cross-links only via hydrogen bonding, the printed construct has no integrity and easily deforms if handled. Gelatin methacrylate (GelMA) is a photopolymerizable seminatural hydrogel comprised of modified gelatin with methacrylic anhydride, and it is an attractive biomaterial for cell-based studies and tissue engineering applications. Studies have shown that 3D printed constructs using GelMA hydrogel have the ability to maintain strict control and care of the microenvironment and exhibit long-term cell viability
Commonly Used Bio-Ink Materials: Alginate and Cross-Linking. (a, b) Alginate is an anionic polysaccharide derived from brown seaweed. Due to its ability to allow the transmission of chemical signals to cells in developing tissue, alginate closely replicates native extracellular matrix (ECM), making it an attractive option for scaffolding material in tissue engineering applications [6, 7]
Commonly Used Bio-Ink Materials: Alginate and Cross-Linking. (a) In order to induce the formation of reinforcing calcium cross-links, sodium alginate is exposed to a calcium chloride solution (CaCl2/CaSO4). These cations link the monomers to form polymers resulting in gelation [8]. Longer duration of exposure to cross-linking agents may be more toxic to the cells; hence scaffolds are typically cross-linked only for a few minutes depending on the type of hydrogel and the size of the construct. (b, c) Maintenance of cell viability is demonstrated by the preponderance of live cells (green) over nonviable cells after the biomaterial is allowed to incubate at 37 °C and 5% CO2 for 1 week
Commonly Used Bio-Ink Materials: Alginate with Collagen II. (a) Molecular structure of collagen II, one of the major components of native extracellular matrix (ECM) [9]. (b, c) Alginate-based hydrogels can be reinforced with collagen II to resist breakdown of cross-links during 3D printing with bio-inks. However, this comes at the price of moderately reduced fidelity and integrity, as well as drastically reduced printability. Adding other components to the hydrogel such as nanocellulose or constructing an additional synthetic scaffold structure that can reinforce the bioprinted structure could overcome these limitations [10]
Commonly Used Bio-Ink Materials: Pluronic F127. (a) Pluronic F127 is a widely used thermo-reversible polymer in drug delivery systems that gels at higher temperatures (37 °C) and liquefies at lower temperatures (4 °C). Though Pluronic F127 confers good printability, this benefit is balanced by relatively weak structural integrity of the final printed product [11]. (b) However, this weak structural integrity is beneficial in the use of Pluronic F127 as a “sacrificial” bio-ink. Sacrificial materials are highly water soluble at certain temperatures and can act as useful support materials to 3D print in. Printing in a sacrificial bath avoids overhangs or deformations by giving the construct a little extra time to cross-link, and as the construct cross-links or strengthens, the bath can be washed away [12]
Commonly Used Bio-Ink Materials: Gelatin Methacrylate. Gelatin methacrylate (GelMA) is a seminatural, photopolymerizable hydrogel comprised of a modified gelatin with methacrylic anhydride. With moderate printability, shape fidelity, and construct integrity, GelMA provides a well-balanced option as a hydrogel for cell-based studies and a feasible bio-ink for 3D bioprinting and tissue engineering applications [13]
Cation-Induced Gelation of Hydrogel-Based Bio-Ink. (a) Hydrogel-based bio-inks composed of gellan and alginate can be prompted to undergo gelation by the addition of cations. These cations form ionic bonds between the monomers creating a strong, cross-linked polymer. (b) Sacrificial bio-inks can be used as cation reservoirs to trigger this gelation process in the permanent 3D bioprinted graft [14]
Fiber Reinforcement: A Shift in the Paradigm of Biofabrication. (a) Researchers have begun to utilize separate materials for structural support and cell delivery, to produce viable bioprinting constructs. These constructs exhibit favorable mechanical characteristics closely mimicking those of the native tissue. Furthermore, the hydrogel is supported by the thermoplastic material, which allows a broader range of hydrogel types to be used (relative to bioprinting of hydrogels alone). (b, c) Thermoplastic polymers serve as skeletal structures into which hydrogels composed of varying cell types and/or bioactive factors can be embedded in an organized, sustainable fashion [15]
3D Bioprinting of Articular Cartilage Tissues: Zonal Variations. Zonal consideration in articular cartilage is an essential consideration when bioprinting articular cartilage tissues. (a) Moving from superficial to deep articular cartilage (AC), there is a distinct change in collagen orientation, as well as a gradual increase in hyaluronic acid (HA0) levels and decrease in oxygen (O2) levels. (b) There is a significant increase in the presence of glycosaminoglycan (GAG) in the middle and deep layers of AC relative to the more superficial layers. (c) Proteoglycan 4 (PRG4) and (d) developmental endothelial locus 1 (Den-1) are present in high levels in the superficial zone and thus may serve as suitable zone-specific markers. (e) Cartilage intermediate-layer protein (CILP) and (f) Jagged 1 (JAG1) expression are seen predominantly in the middle and deep zones of AC [16]
Potential Strategy for Replicating the Collagenous Structural Architecture of Articular Cartilage. (a) Double arrow indicates the directions of increasing anisotropy and deviation of collagen fibrils from the “magic angle” (m.a.) towards both superficial and deep zone. This results in a shortening of T2 with increasing anisotropy. Bright structures in the polarized light microscopy image (left) reveal arranged structures. The m.a. (54.7°) is indicated with the direction of the B0 field. This imaging technique, based on the orientation of the collagen fibrils, can detect disease at an early stage before macroscopic changes in tissue appear, and employ tissue-engineered components to prevent an irreversible onset of the disease. (b) 3D rendering of the collagen fibril structure and (c) 3D rendering of the collagenous structure as a base for overlying bioprinted medium [17]
Post-print Enhancement of 3D Bioprinted Constructs. The addition of extracellular matrix components in the form of micronized biocartilage (Arthrex™) can enhance cell proliferation within the printed construct. The constructs can be further enhanced by post-print exposure of the construct to growth factors, such as transforming growth factor beta-3 (TGF-β3) [14]
3D Bioprinted Tracheal Tissue: An Exemplary Application of Cartilaginous 3D Bioprinting. (a) CAD-rendered scaffold for cartilaginous tracheal tissue. (b) Printed scaffold, preimplantation. (c, d) Printed scaffold successfully seeded with cartilaginous tissue, 4 weeks in vivo. (e) Demonstration of normal cartilage growth in a tracheal replacement graft when chondrocytes are separated from the tracheal lumen by an intervening membrane. When no such membrane exists, there is a propensity for inflammation and stenosis. These findings are important for future construction and implantation of tracheal replacement grafts
3D Bioprinted Meniscus: Future Directions. A top view (a) and side view (b) of a 3D bioprinted construct of a sheep meniscus. The construct was printed using the 3D Discovery bioprinter from regenHU (Switzerland). Alginate-nanocellulose hydrogel mixture was used as a bio-ink. The construct shape was retained post-printing and the cells remained viable [18]
21.3 Take-Home Message
Cartilage defects prove difficult to manage clinically and surgically due to their avascular structure. Its limited regenerative capacity poses yet another obstacle in the development of long-term solutions for repairing cartilage defects. With the hope of developing more long-standing solutions, many researchers have turned to tissue-engineering cartilage de novo by means of 3D bioprinting. Using 3D bioprinting, various biocompatible materials can be assembled in a highly precise manner, mimicking the ultrastructure and biomechanical properties of target tissue, to produce a personalized, patient-specific construct. Biomaterials can be seeded with extracellular “cues” to promote target tissue type behavior, 3D printed and fabricated to form any complex shape required to fit the patient’s defect. Due to the lack of vascularity and lymphatic supply, cartilage may seem like an ideal and relatively simpler candidate for 3D bioprinting. However, its characteristic zonal architecture makes it challenging to reproduce cartilage, artificially. In order to resolve these challenges, in-depth preclinical studies are required to assess the viability of 3D bioprinted cartilage grafts in vivo, prior to clinical translation. Although relatively recent, the field of three-dimensional bioprinting is rapidly advancing and shows enormous potential for developing more personalized and concrete solutions to overcome long-standing medical challenges.
References
MakerBot. MakerBot® replicator 2 brochure. Online. http://downloads.makerbot.com/replicator2/MakerBot_Replicator2_brochure.pdf. Accessed 21 July 2019.
Burkhardt C, Freigassner P, Weber O, Imgrund P, Hampel S. Fused filament fabrication (FFF) of 316L green parts for the MIM process. Deposition Technologies. World Powder Metallurgy; 2016.
Schematics of building a tubular organ module by bioprinting. Organ printing: understanding and employing multicellular self-assembly. University of Missouri; 2007. Online. http://organprint.missouri.edu/www/. Accessed 21 July 2019.
Bioprinting applications. SE 3D (permission granted by Dr. Mayasari Lim) Education. 2016. Online. Accessed 21 July 2019.
Ahlfeld T, Köhler T, Czichy C, Lode A, Gelinsky M. A methylcellulose hydrogel as support for 3D plotting of complex shaped calcium phosphate scaffolds. Gels. 2018;4(3):68.
Alginates in food: sodium alginate uses in food. Culinary Physics. 2014.
Matin A, Shafi H, Wang M, Khan Z, Gleason K, Rahman F. Reverse osmosis membranes surface-modified using an initiated chemical vapor deposition technique show resistance to alginate fouling under cross-flow conditions: filtration & subsequent characterization. Desalination. 2016;379:108–17.
Calcium promotes the solidification of alginate networks. Deconstructed Apple Pie. Discover Magazine. 2014. Accessed 21 July 2019.
The RCSB PDB “molecule of the month”: Collagen. D.S. Goodsell. RCSB PDB. 2000.
Lee BR, Hwang JW, Choi YY, Wong SF, Hwang YH, Lee DY, Lee S-H. In situ formation and collagen-alginate composite encapsulation of pancreatic islet spheroids. Biomaterials. 2012;33(3):837–45.
Young-seok J, Park W, Park H, Lee D, Na K. Thermo-sensitive injectable hydrogel based on the physical mixing of hyaluronic acid and Pluronic F-127 for sustained NSAID delivery. Carbohydr Polym. 2017;156:403–8.
Houben A, Van Hoorick J, Van Erps J, Thienpont H, Van Vlierberghe S, Dubruel Pl. Indirect rapid prototyping: opening up unprecedented opportunities in scaffold design and applications. Ann Biomed Eng. 2017;45:58–83.
Rose J, Pacelli S, El Haj A, Dua H, Hopkinson A, White L, Rose F. Gelatin-based materials in ocular tissue engineering. Materials. 2014;7(4):3106–35.
Kesti M, Eberhardt C, Pagliccia G, Kenkel D, Grande D, Boss A, Zenobi-Wong M. Bioprinting complex cartilaginous structures with clinically compliant biomaterials. Adv Funct Mater. 2015;25(48):7406–17.
Schuurman W, Khristov V, Pot M, van Weeren P, Dhert W, Malda J. Bioprinting of hybrid tissue constructs with tailorable mechanical properties. Biofabrication. 2011;3(2):1–7.
Klein T, Malda J, Sah R, Hutmacher D. Tissue engineering of articular cartilage with biomimetic zones. Tissue Eng Part B Rev. 2009;15(2):143–57.
Nieminen M, Rieppo J, Toyras J, Hakumaki J, Silvennoinen J, Hyttinen H, Jurvelin J. T2 relaxation reveals spatial collagen architecture in articular cartilage: a comparative quantitative MRI and polarized light microscopy study. Magn Resonan Med. 2001;46:487–93.
Markstedt K, Mantas A, Tournier I, Martínez Ávila H, Hägg D, Gatenholm P. 3D bioprinting human chondrocytes with nanocellulose–alginate bioink for cartilage tissue engineering applications. Biomacromolecules. 2015;16(5):1489–96.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2021 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Reed, T.F., Swami, P.N., Mustapich, T.L., Grande, D.A. (2021). The Illustrative 3D Bioprinting in Cartilage Repair. In: Goyal, D.R. (eds) The Illustrative Book of Cartilage Repair. Springer, Cham. https://doi.org/10.1007/978-3-030-47154-5_21
Download citation
DOI: https://doi.org/10.1007/978-3-030-47154-5_21
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-47153-8
Online ISBN: 978-3-030-47154-5
eBook Packages: MedicineMedicine (R0)