Abstract
Ultrasound-guided procedures, especially those that are for needle guidance, are all based on the learned skill of being able to track the needle tip the entire time, while it is in the patient under ultrasound imaging. By learning this critical skill, the physician should feel confident in the successful completion of both simple and more complicated, invasive procedures. Ultrasound-guided percutaneous drainage or aspiration of abnormal fluid collections is becoming standard of care in current clinical practice. Ultrasound guidance has led to reduced morbidity and mortality and decrease in length of stay and healthcare costs. Ultrasound-guided percutaneous drainage is minimally invasive and relatively inexpensive and has several advantages over CT including real-time guidance and lack of radiation.
This chapter will introduce the physician to both commonplace, relatively simple incision and drainage procedures of subcutaneous abscesses and hematomas and more rare, invasive procedures such as drainage of intra-abdominal fluid collections and placement of percutaneous drains into those fluid collections. The overall principle of this range of procedures is the same: ability to utilize ultrasound to visualize and guide a needle into any space of the body for successful completion of the procedure. Each of these procedures will be explained: indications, contraindications, equipment, procedure preparation, step-by-step procedure explanation, and complications. Pearls and pitfalls will also be discussed to help prevent the possible complications. Suggestions to integrate these skills into clinical practice and the evidence to support the procedures will be covered.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Ultrasound guidance
- Ultrasound procedures
- Percutaneous drainage
- Incision and drainage
- Intra-abdominal fluid drainage
Introduction
Patients with abscess or other abnormal fluid collection that require drainage are often evaluated in acute care settings. It has been well-documented that procedural guidance under ultrasound increases patient safety and patient satisfaction and decreases procedural time. With ultrasound guidance, there is also the benefit of seeing the fluid collection shrink in real time with aspiration. Another method of real-time procedural guidance is through interventional radiology or fluoroscopy, but that exposes the patient to large amounts of ionizing radiation. Because of the complex abdominal anatomy, it is even more critical to maintain needle visualization during the entirety of the procedure. Depending on the location of the abdominal fluid collection, ultrasound can be used for an ultrasound-guided nerve block for the analgesia in addition to being used for procedural guidance of fluid drainage.
Incision and Drainage of Subcutaneous Abscesses
Advantages of Ultrasound Guidance
Point-of-care ultrasound (POCUS) is a useful tool to differentiate superficial cellulitis and hematoma from abscess. Ultrasound is more sensitive for detection of subcutaneous abscesses compared to computed tomography (CT) without exposing the patient to potential harmful effects of radiation. A study by Gaspari et al. demonstrated that out of 65 patients undergoing both ultrasound and CT for evaluation of suspected abscess, ultrasound demonstrated sensitivity of 96.7% and specificity of 85.7% compared to CT sensitivity of 76.7% and specificity of 91.4% for diagnosis of abscess [1]. Additionally, the training necessary to accurately diagnose presence of abscess by POCUS is readily learned in as little as 30 minutes [2].
Anatomy
POCUS can be used to evaluate the skin, subcutaneous tissue, and fascia. Both superficial epidermis and dermis can be evaluated and appear as a hyperechoic layer on ultrasound. Subcutaneous tissue lies just deep to the dermis and can be visualized as hypoechoic fat lobules with hyperechoic septae (Fig. 11.1). The dense fibrous membrane is the fascial layer and usually appears as a linear hyperechoic layer. Veins are visualized as non-pulsatile, compressible anechoic structures with hyperechoic walls. Arteries are visualized as pulsatile, non-compressible anechoic structures with hyperechoic walls. Nerves appear as a small honeycomb, hyperechoic bundle. Special attention should also be given to the underlying muscle. Subcutaneous abscesses can start in the superficial layer of the skin and penetrate through muscle fascia.
Both superficial epidermis and dermis can be evaluated and appear as a hyperechoic layer on ultrasound. Subcutaneous tissue lies just deep to the dermis and can be visualized as hypoechoic fat lobules with hyperechoic septae. The dense fibrous membrane is the fascial layer and usually appears as a linear hyperechoic layer
Indications
Patients with localized erythema, increased warmth, swelling, and/or discomfort of an affected body part should undergo sonographic imaging to identify pathology such as cellulitis and abscess (Fig. 11.2). In the study by Squire et al., out of 18 cases in which clinical exam did not suggest abscess, but POCUS demonstrated evidence of anechoic fluid collection, ultrasound was accurate in 17/18 (94%) of cases confirmed by incision and drainage. This suggests that patients who are found to have anechoic fluid collections by POCUS concerning for abscess should undergo incision and drainage, even if the clinical examination suggests only superficial cellulitis without abscess [2].
Contraindications
The location of concern should be evaluated with POCUS to ensure that no neurovascular structures lie in the region of interest, which would in turn warrant an alternative method for incision and drainage [2]. In addition, color Doppler can be used to ensure there is no evidence of a necrotic or cancerous lymph node, aneurysm, or pseudoaneurysm (Figs. 11.3 and 11.4). Discretion should be used in bedside incision and drainage of abscess in patients on anticoagulation or with known coagulopathic states. Abscess located in muscle, known as pyomyositis, can present similarly with erythema, pain, swelling, and tenderness on palpation of the affected region (Fig. 11.5). Pyomyositis is generally drained in the operating room.
This is an example of a metastatic cancer lymph node. The usual architecture of a normal lymph node is disrupted. There is no central hilar blood flow. The blood flow is now on the periphery. There is no change in shape with graduated compression with the ultrasound transducer to suggest fluid contents
(a) This superficial circular mass is pulsatile with blood contents swirling. (b) With color Doppler, you see the swirling flow of the blood more clearly. This example illustrates the importance of using bedside ultrasound before an incision and drainage should be performed. It also shows the importance of using color Doppler to identify blood flow
Equipment and Probe Selection
The high-frequency (12–7 MHz) linear array probe is ideal for evaluation of superficial structures. Color Doppler can aid in identifying surrounding neurovascular structures. One percent lidocaine with or without epinephrine is a commonly used anesthetic. Chlorhexidine, a needle driver for blunt dissection, and a #11 blade scalpel should be readily available prior to starting the procedure. In more delicate areas or for smaller fluid collections, an 18- or 20-gauge needle attached to a 10 mL syringe can be used as an alternative to the #11 blade scalpel.
Of note, if the subcutaneous abscess is in a location of thick subcutaneous fat, such as the buttock, thigh, or abdominal wall, use of the low frequency curved array probe for deeper imaging may be helpful.
Preparation and Pre-procedural Evaluation
The patient should be positioned such that the affected area is easily accessible to the provider. Topical anesthetic, such as lidocaine-epinephrine-tetracaine gel, can be used over the affected area to minimize discomfort.
Procedure
Begin scanning away from the affected area to evaluate the patient’s normal anatomy. Scan the entire length of the affected area in both sagittal and transverse planes using the linear array probe. An abscess will appear as an anechoic fluid collection with hyperechoic contents often with posterior acoustic enhancement. This can be distinguished from cellulitis, which has a cobblestone appearance without fluid collection (Fig. 11.2). Gentle graded compression ensures a loculated fluid collection is not missed, and color Doppler flow can be used to confirm lack of vascularity (Fig. 11.6). Furthermore, graded compression may result in swirling of abscess contents. Comparison to the contralateral side can be useful. If a fluid collection is located, the boundaries, depth from the tissue surface, and estimated size of the cavity should be noted. The sonographic appearance of a hematoma is non-specific and is challenging to differentiate from an abscess [3].
Once the abscess and surrounding anatomy have been visualized, the affected area should be cleaned with chlorhexidine and subsequently anesthetized. The probe should be covered with a Tegaderm to minimize transmission of nosocomial infections, and gel should be placed over top of the probe. Under ultrasound guidance, a small stab incision should be made using a #11 blade scalpel, and blunt dissection with a needle driver can break up loculated fluid collections. Extensive abscesses may require irrigation with normal saline to aid in breakdown of loculations. In anatomically challenging locations or for small fluid collections, needle aspiration using an 18- or 20-gauge needle attached to a 10 mL syringe can be used as an alternative to using the #11 blade scalpel (Figs. 11.7 and 11.8). Ultrasound should be used after incision and drainage is complete to verify complete evacuation of the abscess cavity.
(a) In sensitive areas, such as the scrotum, or if the abscess is small, needle aspiration may be preferred. In this image, you see the needle in short axis as an echogenic dot (arrow) (out-of-plane technique). (b) With real-time ultrasound guidance and imaging, you can see the actively shrinking abscess as purulence is aspirated
Complications
Color Doppler can aid in the identification of neurovascular structures, lymph nodes, solid masses, etc. In addition, ultrasound should be used after the procedure to verify complete evacuation of the abscess cavity. A partially drained abscess may result in the need for further intervention.
Pearls and Pitfalls
-
1.
The use of color Doppler during the initial evaluation and real-time ultrasound guidance during the procedure can help avoid neurovascular complications.
-
2.
Purulent material in the abscess cavity may appear isoechoic, and therefore, the use of graded compression and color Doppler can help in identification of an abscess cavity (Fig. 11.9).
-
3.
Use of a larger 18-gauge needle is recommended for needle aspiration procedures, as purulent material may be difficult to aspirate when using a smaller gauge needle.
-
4.
When purulent material is too viscous for needle aspiration or if the abscess cavity is too large to adequately evaluate using needle aspiration, a #11 blade scalpel can be used to create a small stab incision to allow drainage.
-
5.
Be aware that necrotic lymph nodes appear similar to an abscess. Use gray-scale imaging and color Doppler imaging to evaluate for necrotic lymph nodes before performing an incision and drainage, and incision and drainage of necrotic lymph nodes is discouraged.
Especially in areas of high-fat content, such as the buttocks, thighs, and, for some patients, abdominal wall, abscesses can appear isoechoic and subtle to identify under ultrasound. Note that this abscess does not have the usual obvious characteristics of a classic abscess. Compression of the area with the transducer may cause swirling of the contents to reveal pus
Integration into Clinical Practice
Ultrasound-guided incision and drainage of abscess and hematoma provide definitive treatment. The features to distinguish abscess from cellulitis are easily learned and can help guide management decisions about the need for incision and drainage. Furthermore, ultrasound-guided drainage provides real-time visualization of the surrounding neurovascular structures which helps reduce the incidence of complications.
Evidence
Ultrasound-guided abscess drainages are technically uncomplicated and minimally invasive. In a study by Kjær et al., subcutaneous truncal abscesses were treated successfully in 93% of their patients [4]. This approach yielded high patient satisfaction and was well-tolerated with short healing times.
Ultrasound-guided breast abscess drainages have replaced open treatment of breast abscesses, with 97% resolution rate in puerperal abscesses and 81% resolution rate for nonpuerperal abscesses [5]. Needle drainage under ultrasound decrease pain and scar formation. The evidence for using ultrasound to directly guide abscess drainage makes it suitable for outpatient settings.
Key Points
-
POCUS for the diagnosis or confirmation of a subcutaneous abscess is recommended in addition to physical examination due to concern of a suspected abscess being a mass, lymph node, aneurysm, etc.
-
For smaller abscesses, it is reasonable to use a large gauge needle to attempt aspiration and proceed to incision if necessary.
-
In-plane technique is always preferred, if possible, to ensure the needle tip does not injury nearby structures.
-
Always use color Doppler to evaluate abscesses to identify vascular or blood flow within the fluid collection.
Drainage of Subcutaneous Hematomas
Advantages of Ultrasound Guidance
POCUS is a useful tool to differentiate soft tissue swelling from hematoma, although differentiation of hematoma from abscess can be more challenging. Differentiation between a hematoma and an abscess will depend more on the clinical picture. Patients can also present with an infected hematoma, which may present with signs and symptoms of an abscess over an area of previous trauma or if the patient is prone to bleeding.
Anatomy
Pay close attention to surrounding structures, especially vasculature that may have been injured to cause the hematoma. After drainage of the hematoma that may have tamponade feeding vessels, bleeding may commence from the incision. It is also important to note the sonographic characteristics of the hematoma. Fresh blood may appear hyperechoic or isoechoic to the surrounding subcutaneous tissue, and as blood products break down over time, the blood may become anechoic with possible fibrin strands (Fig. 11.10).
This 4-day-old hematoma shows some heterogeneous contents, but it is mostly anechoic. It is important to incorporate clinical symptoms into diagnosing hematomas. As you can see with this image, this hematoma can certainly be confused for an abscess, but note there is no associated overlying cellulitis, which may give a clue to it being a hematoma
Indications
Patients with an area of fluctuance, induration, erythema, increased warmth, swelling, and/or discomfort should undergo ultrasound imaging to evaluate for underlying pathology. The differentiation of abscess and hematoma is largely clinical, with only very subtle differences by ultrasound. Hematoma should be clinically suspected in patient who present with history of trauma, easy bruising, thrombocytopenia, coagulopathy, anticoagulation, or recent surgery, although abscess remains on the differential diagnosis. When the pressure in the hematoma cavity exceeds that of the dermal and subdermal capillaries, there is increasing potential for overlying skin necrosis.
Contraindications
The contraindications for this procedure are very similar to those for draining abscesses. POCUS should be used to ensure that no neurovascular structures lie in the region of interest, which would warrant an alternative method for incision and drainage [2]. Use color Doppler to ensure the area in question is not a necrotic lymph node, aneurysm, or pseudoaneurysm. Discretion should be used when performing bedside incision and drainage of a hematoma in patients on anticoagulation or with known coagulopathic states, as bleeding is a concerning potential risk; patients should be counseled regarding the potential risk of bleeding prior to starting the procedure. Laboratory testing such as complete blood count to check platelet count and a coagulation panel (PTT and PT/INR) may be helpful prior to starting the procedure to further assess for bleeding risk.
Equipment and Probe Selection
As with evaluation of most superficial structures, the high-frequency (15–7 MHz) linear array probe is ideal. Color Doppler over the area in question can help identify surrounding neurovascular structures. One percent lidocaine with or without epinephrine is commonly used for anesthesia, although the use of lidocaine with epinephrine can help minimize potential bleeding if not otherwise contraindicated. Chlorhexidine, a needle driver for blunt dissection, a package of 4 × 4 inch gauze pads, and a #11 blade scalpel should be readily available. Compression dressing or an ACE bandage should also be considered for adequate pressure over the drained hematoma, since the hematoma may continue to ooze or re-bleed. The viscous nature of hematoma generally contraindicates use of needle drainage, but it is reasonable to start with a needle aspiration and convert to incision and drainage if necessary (Figs. 11.11 and 11.12).
Although the viscous nature of hematomas may preclude needle drainage, it is always reasonable to start with a needle drainage and convert to an incision if necessary. This is an example of a long-axis or in-plane technique, with visualization of the needle tip and the entire length of the needle that is in the patient. This is the preferred method for ultrasound-guided procedures. The dotted line outlines the needle and needle tip
Preparation and Pre-procedural Evaluation
The patient should be positioned such that the affected area is easily accessible to the provider. Topical anesthetic, such as lidocaine-epinephrine-tetracaine gel, can be used over the affected area to minimize discomfort. As mentioned previously, evaluation of the patient’s platelet count and coagulation studies may be indicated. Additionally, for larger hematomas, consider a type and screen and ensure that appropriate blood products are readily available, should a bleeding emergency result. Gauze impregnated with hemostatic agents or tranexamic acid can also be at bedside to assist with bleeding control.
Procedure
Evaluate the patient’s normal anatomy by initially scanning away from the affected area. Scan the entire length and width of involved area in two planes—both sagittal and transverse—using the linear array probe. Applying graded compression helps ensure a loculated fluid collection, which can be easily overlooked in the case of hematoma, is not missed. Application of color Doppler flow confirms lack of vascularity. If a fluid collection concerning for hematoma is located, note the boundaries, depth from the tissue surface, and estimated size of the cavity. The sonographic appearance of a hematoma is non-specific and is challenging to differentiate from an abscess [3].
The affected area should then be cleansed with chlorhexidine and subsequently anesthetized. The probe should be covered with a Tegaderm, and gel should be placed over top of the probe. Under ultrasound guidance, a minimal stab incision should be made using a #11 blade scalpel, and blunt dissection should be used to break up loculations, especially if there are clots or it is an infected hematoma (Fig. 11.13). Gauze pads can be used to apply pressure and evacuate any remaining clot. After incision and drainage is complete, verify complete evacuation of the hematoma cavity using ultrasonography.
Another possible diagnosis is an infected hematoma. A hematoma that later becomes infected. Note the heterogeneous contents of this infected hematoma. There is also thickened skin overlying this fluid collection. The patient had presented with signs and symptoms of an abscess with a history of trauma in this area. This fits with an infected hematoma
Complications
Bleeding is a potential complication associated with this procedure. Caution is advised in patients with a known bleeding diathesis or on anticoagulation. There may be persistent oozing from the incision site. It is advised to apply a compression dressing after the incision and drainage.
Pearls/Pitfalls
-
1.
Use of color Doppler pre-procedure and real-time sonographic evaluation during the procedure can help avoid potential neurovascular complications.
-
2.
Use of graded compression and color Doppler can help in identification of a subtle hematoma.
-
3.
Hematomas are often comprised of viscous, clotted blood which is not amenable to needle drainage. Use of a #11 blade scalpel is recommended instead.
-
4.
Do not underestimate the potential for blood loss in patients with known coagulopathy or in those patient predisposed to bleeding diatheses. Take appropriate precautions, and use lidocaine with epinephrine when possible to help minimize this potential complication.
-
5.
If there is infection superimposed onto the hematoma, there may be blood, purulent drainage after the incision. Treat like an abscess and prescribe antibiotics.
Evidence
Sonographic guidance of hematomas has multiple benefits including exact positioning of the needle tip, surveying surrounding anatomy to avoid vessels, clots, soft tissue, and/or thickened synovium in the case of joint aspirations [6]. The procedure is fast and easy to perform. Because no ionizing radiation is used, this imaging modality for procedure guidance is safe for pregnant women and children [6].
This method of procedure guidance can also serve as an adjunct to other imaging-guided procedures. Reijnen et al. describe a case in which a symptomatic pseudoaneurysm was treated with endovascular repair, and ultrasound-guided needle aspiration of the hematoma was implemented [7]. The patient had no complications or recurrence of the hematoma.
Key Points
-
As in the case with subcutaneous abscesses, hematomas also warrant ultrasound evaluation because of other diagnoses and the risk of infection.
-
For large hematomas, especially in patients with coagulopathy, order pre-procedural laboratory studies and consider and type and screen.
-
It is advised to place a compression dressing over the incised area to assist with any residual oozing and drainage.
Aspiration of Symptomatic Renal Cysts
Advantages of Ultrasound Guidance
POCUS is a useful tool to differentiate simple cysts from solid or complex renal masses. The kidney is one of the most common sites of cysts in the body, with a prevalence of 20–50% in the general population with an estimated increased incidence with age [8,9,10,11].
Anatomy
POCUS should be used to evaluate the characteristics of the cyst and its surrounding anatomy prior to starting the procedure. The kidney, colon, liver (on the right), spleen (on the left), and adjacent lung should be readily identified, as these structures need to be avoided during the procedure. Renal vessels and ureter should also be identified and avoided.
Indications
Most simple renal cysts are asymptomatic incidental findings and should be left untreated. Occasionally, they may become very large. If large enough, they may cause pain, hematuria, obstructive uropathy, and even hypertension [10, 11]. It is in the latter cases when aspiration is indicated. Note that recurrence after aspiration is high and this is mostly performed to determine if the patients’ symptoms are in fact caused by mass effect from the cyst. The differentiation between a simple cyst, a complex cyst, and a solid renal mass is based on imaging findings. The sonographic characteristics of a simple cyst are an anechoic lumen, well-defined back wall, acoustic enhancement deep to the cyst, and no measurable wall thickness (Figs. 11.14 and 11.15).
Any time there is deviation from the description of a simple renal cyst, it is considered a complex renal cyst. In this example, the patient has polycystic kidney disease. There appears to be clusters of simple-appearing cysts, but there is also a large complex, fluid-filled renal cyst on the right side of this ultrasound image
Contraindications
POCUS and color Doppler should be used to ensure that no vascular structures, septations, thick wall, or echogenic material lies within the cystic lesion of interest. These findings mean the cyst is complex or, in fact, a solid mass. If this is the case, it should not be drained and warrants additional advanced imaging (CT/MRI) to exclude an alternate pathology such as renal cell carcinoma. Patients on anticoagulation or with known coagulopathic states are high risk, as bleeding is a concerning potential complication. All patients should be counseled regarding the potential risk of bleeding prior to starting any invasive procedure. Injury to the kidney and adjacent structures such as the ureter or colon is a possibility. These risks are minimized with the adequate use of image guidance, such as ultrasound.
Equipment and Probe Selection
As with evaluation of most deep structures, a lower-frequency, 5–2 MHz, curved array probe is ideal. Color Doppler over the lesion in question can help assess the characteristics of the cyst. Chlorhexidine, sterile towels, sterile probe cover, a needle driver for blunt dissection, a package of 4 × 4 inch and 2 × 2 inch gauze pads, an #11 blade scalpel, a 20 or 40 cc syringe, and a 19G centesis needle (7 or 14 cm length depending on the body habitus of the patient) should be readily available. One percent lidocaine with or without epinephrine is commonly used for anesthesia.
Preparation and Pre-procedural Evaluation
Evaluation of the patient’s platelet count and coagulation studies is advised. The patient should be positioned prone, and the posterior flank of the affected side should be sterilely prepared with chlorhexidine and draped with sterile towels. The ultrasound probe should be covered with a sterile probe cover, and sterile gel should be used.
Procedure
Scan the entire length and width of the involved area and surrounding tissues in two planes—both sagittal and transverse—using the curved array probe. Localize the structures you want to avoid, and choose the safest, usually the shortest, route of access from the skin to the cyst. Following the administration of local anesthesia, perform a small skin nick with a #11 blade, and separate the subcutaneous soft tissues with a needle driver. Then, under direct ultrasound guidance, advance the centesis needle through the skin nick, subcutaneous tissues, into the retroperitoneum and into the cyst. Once you see the tip of the needle within the cyst, you can aspirate (Fig. 11.16). If clear fluid is aspirated, advance the outer catheter of the centesis needle, remove the sharp, and dispose it safely. Attach the 40 or 60 ml syringe to the catheter, and aspirate as much fluid as possible. Stop if the fluid becomes hemorrhagic or when you feel resistance and see a significant reduction in the size of the cyst on ultrasound. Then, remove the catheter, and place a 2 × 2 gauze and small Tegaderm over the incision. The patient should be observed for 1 hour to ensure no significant pain, discomfort, or change in vital signs, which may be signs or symptoms of a complication.
Example of an ultrasound-guided abdominal cyst drainage. (Reproduced from book: Velasco and Hood [21]. [Figure 7.3, p. 91])
Complications
Bleeding, injury to the kidney, and injury to adjacent organs as well as infection are the potential complications of this procedure. With adequate patient selection, sterile preparation, and appropriate use of image guidance, these are greatly minimized.
Pearls/Pitfalls
-
1.
Asymptomatic simple renal cysts should not be aspirated.
-
2.
The ultrasound characteristics of a simple renal cyst are an anechoic lumen, well-defined back wall, acoustic enhancement deep to the cyst, and no measurable wall thickness. Care should be taken with gain settings to avoid creating false echoes or septations as well as eliminating actual ones.
-
3.
A cystic renal lesion with a thick wall, septations (particularly if nodular), internal debris, or internal color Doppler flow is not a simple cyst and warrants further workup.
-
4.
Use of real-time sonographic evaluation and color Doppler pre-procedure to assess the characteristics of a cystic renal mass can help avoid potential complications, such as potentially rupturing a renal cell carcinoma.
-
5.
Use of color Doppler and real-time sonographic evaluation during the procedure can help avoid potential complications, such as injury to adjacent organs/structures.
-
6.
Symptomatic cysts that arise from other organs such as the liver or adnexa should not be intervened on and may warrant additional imaging as well as specialty consultations. Cystic masses in children always warrant further workup.
-
7.
Do not underestimate the potential for blood loss in patients with known coagulopathy or in those patients predisposed to bleeding diatheses. Take appropriate precautions to help minimize this potential complication.
-
8.
If the patient’s symptoms disappear following aspiration of the renal cyst and later recurs and the patient becomes symptomatic again, consultation to interventional radiology (for sclerotherapy) or urology (for open or laparoscopic decortication) is advised for definitive treatment.
Integration into Clinical Practice
Ultrasound-guided aspiration of renal cysts is an important tool to assess if a patient’s symptoms of chronic pain, hematuria, hypertension, and/or obstructive uropathy are in fact caused by mass effect due to a large simple cyst. Note that the majority of simple renal cysts are incidental findings and asymptomatic. Asymptomatic simple renal cysts, regardless of their size, should not be treated. Real-time ultrasound-guided aspiration provides visualization of the surrounding organs and structures which helps greatly reduce the incidence of complications. Following aspiration, simple cysts often recur. If symptoms develop again with cyst recurrence, definitive treatment can be provided by interventional radiology (sclerotherapy) or urology (decortication). If this is not an option, intermittent ultrasound-guided aspiration after symptomatic recurrences may be considered to provide symptom relief. The features to distinguish a simple renal cyst from a complex cyst or solid mass are easily learned and can help guide management decisions about the need for aspiration or subspecialty workup and consultation.
Evidence
Ultrasound-guided renal cyst drainage is seen effective for ameliorating symptoms of discomfort, and the high safety profile of this image-guided procedure lends itself well for repeated drainages [9]. With further treatment techniques, such as injection of ethanol for sclerotherapy of the renal cyst epithelium, ultrasound guidance can also be used. Classic treatment is decortication through open surgery or laparoscopy, but Mohsen et al. treated 60 patients with simple renal cyst aspiration and immediate injection of ethanol for sclerotherapy via ultrasound with success [12, 13]. If there is concern for renal cyst leakage or rupture, fluoroscopy or CT can be used as adjuncts to ultrasound [14].
Key Points
-
Most renal cysts are simple, and their small size does not warrant intervention.
-
Renal cysts are drained for the comfort of the patient secondary to their large size.
-
Thorough pre-procedural evaluation of the structures surrounding the cyst and the best, shortest approach should be pursued.
-
If the renal cysts are not simple, ultrasound-guided drainage should not be pursued until the lesion is further evaluated.
Aspiration and Drainage of Intraperitoneal Fluid Collections
Advantages of Ultrasound Guidance
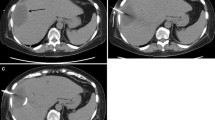
Despite the great advances in diagnostic imaging, there will still be a few instances when the aspiration of a fluid collection is needed to verify a diagnosis and guide therapy. If serous fluid is aspirated and cultures are negative, a seroma can be confirmed (Figs. 11.17 and 11.18). Other examples are the aspiration of pus, which confirms an abscess and may yield the specific pathogen to direct antibiotic therapy (Figs. 11.19 and 11.20); the aspiration of bile, which confirms a biloma (Fig. 11.21); and the aspiration of fluid with highly elevated lipase and amylase which confirms a pancreatic pseudocyst (Fig. 11.22).
Note the hyperechoic needle (arrowhead) in this ultrasound-guided needle drainage of an abdominal wall seroma. (Reproduced from book: Velasco and Vaince [22]. [Figure 6.10, p. 77])
Needle drainage of an intra-abdominal abscess with ultrasound guidance. (Reproduced from book: Velasco and Hood [21]. [Figure 7.26, p. 101])
The classic management of intraperitoneal abscesses used to be conservative (antibiotic management only) or operative drainage. With the widespread use of ultrasound for abdominal imaging starting in the 1970s and CT in the 1980s, the idea of non-surgical, image-guided management of these was introduced [15, 16]. This is now widely accepted as the treatment of choice, whenever feasible, for both spontaneous and post-surgical intraperitoneal abscesses. Percutaneous image-guided abscess drainage is associated with decreased morbidity, decreased length of drainage, and decreased hospital stay, when compared to open surgery [15, 16]. Also, the avoidance of surgery and anesthesia makes this a very cost-effective procedure [16].
Anatomy
POCUS should be used to evaluate the location of the loculated fluid collection and its surrounding anatomy prior to starting the procedure. The small bowel, colon, kidneys, liver, and gall bladder, spleen, pancreas, and/or adjacent lung/diaphragm should be readily identified, as these structures need to be avoided during the procedure. Color Doppler should be used to ensure that there are no intervening vascular structures. If the target is a liver abscess, a route through some intervening liver parenchyma is preferred, to avoid capsular rupture and spillage of abscess contents into the peritoneal cavity.
Indications
Patients who present with fever, leukocytosis, +/− abdominal pain, and a localized intra-abdominal fluid collection seen on cross-sectional imaging (Ultrasound, CT, MRI) should be evaluated for the possibility of percutaneous image-guided aspiration or drain placement. The use of ultrasound has the advantage over CT in that it does not expose the patient or the operator to ionizing radiation. In some instances, overshadowing gas from bowel or within the collection itself may interfere with ultrasound imaging. In these latter cases, CT guidance may be preferred.
Contraindications
Patients on anticoagulation or with known coagulopathic states are high risk, as bleeding is a concerning potential complication; all patients should be counseled regarding the potential risk of bleeding prior to starting any invasive procedure. Injury to the bowel and adjacent solid organs or nearby vessels is a possibility. These risks are minimized with the adequate use of image guidance. On instances where there is interposing bowel or other structures, it may not be possible to perform the procedure safely. Large-volume ascites is a relative contraindication. A paracentesis may be needed prior to addressing the drainage of the loculated fluid collection.
Equipment and Probe Selection
As with evaluation of most deep structures, a lower-frequency, 5–2 MHz, curved array probe is ideal. Color Doppler over and around the fluid collection in question may help identify surrounding organs/structures. Chlorhexidine, sterile towels, sterile probe cover, a needle driver for blunt dissection, a package of 4 × 4 inch and 2 × 2 inch gauze pads, an #11 blade scalpel, a 40 or 60 cc syringe, and a 19G centesis needle (7 or 14 cm length depending on the body habitus of the patient and the depth of the fluid collection) should be readily available, as well as a specimen container to collect a sample of the aspirate. For fluid collections 5 cm or larger in diameter, a 0.035in or 0.038in guidewire, an 8 or 10 Fr all-purpose drain, and a 3.0 non-absorbable suture will be needed. One percent lidocaine with or without epinephrine is commonly used for local anesthesia. If placing a long-term drain is anticipated, intravenous pain medication such as morphine or fentanyl are advised if possible, to help provide adequate pain control.
Preparation and Pre-procedural Evaluation
Evaluation of the patient’s platelet count and coagulation studies is advised. The patient should be positioned in a way that facilitates access to the affected peritoneal space. The skin overlying the fluid collection should then be sterilely prepared with chlorhexidine and draped with sterile towels. The ultrasound probe should be covered with a sterile probe sheath.
Procedure
Scan the entire length and width of the involved area and surrounding tissues in two planes—both sagittal and transverse—using the curved array probe. Localize the structures you want to avoid (bowel, adjacent organs, nearby vessels), and choose the safest, most direct, usually the shortest, route of access from the skin to the peritoneal fluid collection. Following the administration of local anesthesia, perform a small skin nick with the #11 blade, and separate the subcutaneous soft tissues with the needle driver. Then, under direct ultrasound guidance, advance the centesis needle through the skin nick, subcutaneous tissues, into the peritoneum and into the fluid collection (Fig. 11.23). Once you see the tip of the needle within the collection, you can aspirate (Fig. 11.24). If fluid is aspirated, advance the outer catheter of the centesis needle, remove the sharp, and dispose of it safely. Attach the 40 or 60 ml syringe to the catheter, and aspirate as much fluid as possible. Stop if the fluid becomes hemorrhagic or when you feel resistance and see a significant reduction in the size of the fluid collection on ultrasound. Then, remove the catheter, and place a 2 × 2 gauze and small Tegaderm over the incision. The patient should be closely monitored for a minimum of 2 h to ensure he/she suffers no significant pain, discomfort, or change in vital signs, which may be signs/symptoms of a complication.
An example of ultrasound-guided needle aspiration of an intra-abdominal cyst. (Reproduced from book: Velasco and Hood [21]. [Figure 7.23, p. 100])
An abscess that is 4 cm or larger in diameter will require prolonged drainage over a few days (usually up to 1 week) to completely resolve. In these cases, place the centesis needle within the collection under ultrasound guidance, as described above (Fig. 11.25). Then, once the tip of the needle is confirmed within the collection with ultrasound, advance the outer catheter of the centesis needle, remove the sharp needle, and dispose of it safely. Advance the guidewire through the catheter and coil it within the collection. Confirm adequate position of the wire with ultrasound. Then, exchange the catheter over the wire for the 8 or 10 Fr all-purpose drain. Confirm the adequate position of the drain with ultrasound, and remove the wire. Attach the drain to a suction bulb, and secure the drain with a suture. Place a sterile dressing over the dermatotomy. The patient should be observed for a minimum of 2 h to ensure he/she suffers no significant pain, discomfort, or change in vital signs, which may be signs/symptoms of a complication. Daily irrigation of the drain (to avoid clogging) with 5–10 cc of sterile saline is recommended.
This image shows real-time needle guidance under ultrasound to drain an intra-abdominal abscess. (Reproduced from book: Velasco and Hood [21]. [Figure 7.5, p. 92])
Complications
Bleeding, injury to the bowel, and injury to adjacent solid organs/structures as well as infection are potential complications of this procedure. With adequate patient selection, sterile preparation, and appropriate use of image guidance, these are minimized. During drain placement, inherent risks include the spread of abscess to the adjacent spaces or organs, transient bacteremia, or frank sepsis [17]. Other possible complications are abscess recurrence (when incompletely drained) and persistent output through the all-purpose drain. The latter may be a sign of a fistulous connection to the bowel, biliary tree (in the case of a biloma), or pancreatic duct (in the case of a pancreatic pseudocyst).
Pearls and Pitfalls
-
1.
Use of real-time sonographic evaluation and color Doppler pre-procedure to assess the location of the loculated fluid collection can help avoid potential complications.
-
2.
POCUS should be used to identify the small bowel, colon, kidneys, liver, and gall bladder, spleen, pancreas, and/or adjacent lung/diaphragm. These structures must be avoided during the procedure.
-
3.
Color Doppler should be used to ensure that there are no intervening vascular structures.
-
4.
If there is no safe route of access into the fluid collection, do not do it. Certain abscesses will require surgical management or prolonged antibiotic treatment.
-
5.
If the target is a liver abscess, a route through some intervening liver parenchyma is preferred, to avoid capsular rupture and spillage of abscess contents into the peritoneal cavity (Fig. 11.26).
-
6.
In the presence of free intraperitoneal fluid, a paracentesis may be required prior to the aspiration/drain placement.
-
7.
Overshadowing gas from bowel or within the collection itself may interfere with US imaging. In these cases, CT guidance may be preferred.
-
8.
An abscess that is 4 cm or larger in diameter will require prolonged drainage over a few days (usually up to 1 week) to completely resolve. In these cases, aspiration alone will usually not suffice and placement of a drain is required.
-
9.
Persistent output through the all-purpose drain (>1 week) may be a sign of a fistulous connection to the bowel, biliary tree (in the case of a biloma) (Fig. 11.27), or pancreatic duct (in the case of a pancreatic pseudocyst).
-
10.
If a fistula is suspected, additional imaging (such as a fistulogram) and evaluation by surgery are recommended.
-
11.
Do not underestimate the potential for blood loss in patients with known coagulopathy or in those patients predisposed to bleeding diatheses. Take appropriate precautions to help minimize this potential complication.
-
12.
Be prepared to treat the patient for frank sepsis in the event this develops acutely, immediately following the procedure.
Ultrasound-guided needle (green arrows) aspiration of a liver lesion (denoted with T). (Reproduced from book: Velasco and Hood [21]. [Figure 7.18, p. 98])
Needle (white arrow) drainage of large biloma under ultrasound guidance. (Reproduced from book: Velasco and Hood [21]. [Figure 7.27, p. 101])
Integration into Clinical Practice
Ultrasound-guided aspiration of loculated intra-abdominal fluid collections is an important tool to verify diagnosis and guide therapy. Depending on the characteristics of the aspirated fluid, the source or cause of the fluid collection can be identified. Not only can ultrasound help guide the needle and the guidewire to the area of interest, but also watch real-time aspiration and drainage, and guide placement of percutaneous drains (Fig. 11.28a,b).
(a, b) Examples of percutaneous cholecystostomy drains with placement confirmed via ultrasound. (Reproduced from book: Velasco and Hood [21]. [Figures 7.6, p. 92 and 7.34, p. 104])
Real-time ultrasound-guided aspiration/drain placement provides visualization of the surrounding organs and structures which helps greatly reduce the incidence of complications. If the window of access is not clear into the fluid collection, STOP and reconsider. CT may be a better guiding tool in this case. Complex cases will need subspecialty consultation to interventional radiology, and some inaccessible collections will require surgery. Be prepared to handle potential complications if these were to occur. Persistent output through the all-purpose drain, greater than 1 week, may be a sign of a fistulous connection. Additional imaging and surgical consultation may be warranted in these cases.
Evidence
Kassi et al. have shown that percutaneous image-guided drainage through ultrasound is feasible and effective for the treatment of abdominopelvic abscesses with a success rate of 78% [18]. Although not explained in this section, endoscopic ultrasound-guided drainage has been the standard of care for drainage of pancreatic pseudocysts [19] (Fig. 11.29). Ultrasound guidance also serves the imaging guidance modality of choice for pregnant women and children who have intra-abdominal abscesses that are amenable to percutaneous drainage [20].
Ultrasound-guided needle (white arrow) biopsy aspiration of a pancreatic lesion. The dotted lines denote the needle track. (Reproduced from article: D’Onofrio et al. [23]. [Figure 1, p. 3])
Key Points
-
Drainage of intra-abdominal fluid collections for analysis assists with medical management without more invasive operative management.
-
In larger fluid collections, placement of a percutaneous drain for prolonged drainage may be necessary.
-
Persistent output from a percutaneous drain may suggest formation of a fistula.
-
In patients with a bleeding diathesis or coagulopathy, it is important to review pre-procedural laboratory studies and consider type and screen.
References
Gaspari R, Dayno M, Briones J, Blehar D. Comparison of computerized tomography and ultrasound for diagnosing soft tissue abscesses. Crit Ultrasound J. 2012;4(1):5.
Squire B, Fox J, Anderson C. ABSCESS: applied bedside sonography for convenient evaluation of superficial soft tissue infections. Acad Emerg Med. 2005;12(7):601–6.
Wicks J, Silver T, Bree R. Gray scale features of hematomas: an ultrasonic spectrum. AJR Am J Roentgenol. 1978;131(6):977–80.
Kjær S, Rud B, Bay-Nielsen M. Ultrasound-guided drainage of subcutaneous abscesses on the trunk is feasible. Dan Med J. 2013;60(4):A4601.
Christensen AF, Al-Suliman N, Nielsen KR, et al. Ultrasound-guided drainage of breast abscesses: results in 151 patients. Br J Radiol. 2005;78:186–8.
Szopinski KT, Smigielski R. Safety of sonographically guided aspiration of intramuscular, bursal, articular and subcutaneous hematomas. Eur J Radiol. 2012;81(7):1581–3.
Reijnen MMPJ, de Rhoter W, Zeebregts CJ. Treatment of a symptomatic popliteal pseudoaneurysm using a stent-graft and ultrasound-guided evacuation of the hematoma. Emerg Radiol. 2008;16(2):167–9.
Rané A. Laparoscopic management of symptomatic simple renal cysts. Int Urol Nephrol. 2004;36:5–9.
Skolarikos A, Laguna M, de la Rosette J. Conservative and radiological management of simple renal cysts: a comprehensive review. BJU Int. 2012;110:170–8.
Hemal A. Laparoscopic management of renal cystic disease. Urol Clin North Am. 2001;28:115–26.
Okan B, Nalbant I, Can Sener N, Yesil S, et al. Management of renal cysts. JSLS. 2015;19(1):e2014.00097.
Okeke A, Mitchelmore A, Keeley F, Timoney A. A comparison of aspiration and sclerotherapy with laparoscopic de-roofing in the management of symptomatic simple renal cysts. BJU Int. 2003;92:610–3.
Mohsen T, Gomha MA. Treatment of symptomatic simple renal cysts by percutaneous aspiration and ethanol sclerotherapy. BJU Int. 2005;96(9):1369–72.
Lohela P. Ultrasound-guided drainages and sclerotherapy. Eur Radiol. 2001;12(2):288–95.
Gerzof S, Robbins A, Johnson W, Birkett D, et al. Percutaneous catheter drainage of abdominal abscesses: a five-year experience. N Engl J Med. 1981;305(12):653–7.
Johnson W, Gerzof S, Robbins A, Nabseth D. Treatment of abdominal abscesses: comparative evaluation of operative drainage versus percutaneous catheter drainage guided by computed tomography or ultrasound. Ann Surg. 1981;194(4):510–20.
Lorenz J, Thomas J. Complications of percutaneous fluid drainage. Semin Interv Radiol. 2006;23(2):194–204.
Kassi F, Dohan A, Soyer P, et al. Predictive factors for failure of percutaneous drainage of postoperative abscess after abdominal surgery. Am J Surg. 2014;207(6):915–21.
Mandai K, Uno K, Yasuda K. Endoscopic ultrasound-guided drainage of postoperative intra-abdominal abscesses. World J Gastroenterol. 2015;21(11):3402–8.
Patel J, Siriwardana HP, Hammond T, et al. Successful ultrasound-guided drainage of an intra-abdominal collection in late pregnancy. Case Rep. 2017;2017:bcr-2017-219479.
Velasco JM, Hood K. Percutaneous ultrasound guidance techniques and procedures. In: Hagopian E, Machi J, editors. Abdominal ultrasound for surgeons. New York: Springer New York; 2014. p. 89–107.
Velasco JM, Vaince F. Abdominal wall anatomy, pathology, and intervention. In: Hagopian E, Machi J, editors. Abdominal ultrasound for surgeons. New York: Springer New York; 2014. p. 71–88.
D’Onofrio M, Beleù A, De Robertis R. Ultrasound-guided percutaneous procedures in pancreatic diseases: new techniques and applications. Eur Radiol Exp. 2019;3(1):2.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Situ-LaCasse, E., Javedani, P., Devis, P., Arif-Tiwari, H. (2020). Ultrasound-Guided Percutaneous Drainage Procedures. In: Adhikari, S., Blaivas, M. (eds) The Ultimate Guide to Point-of-Care Ultrasound-Guided Procedures . Springer, Cham. https://doi.org/10.1007/978-3-030-28267-7_11
Download citation
DOI: https://doi.org/10.1007/978-3-030-28267-7_11
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-28265-3
Online ISBN: 978-3-030-28267-7
eBook Packages: MedicineMedicine (R0)