Abstract
Assessment of pulmonary function in infants and preschool children is a challenge, given the important changes that happen in the respiratory system in this age group and also the difficulty of achieving patient cooperation for performance of multiple tests. However, recent research has provided references values for different pulmonary function tests, which have improved the clinical approach in many respiratory diseases. Progress is focused on improving patient access to less invasive, readily available, and standardized pulmonary function tests.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Pulmonary Function in Infants
The respiratory system undergoes extraordinary changes in the first 2 years of life, in terms of its growth and functional development. Knowledge of the mechanical properties of the lungs in the first years of life was limited until the development of sophisticated equipment to measure respiratory function that was adapted for use with small children. Since then, it has been possible to understand the inherent aspects of normal respiratory function, as well as the effects of diverse pre- and postnatal injuries, besides treatments. It has been possible to determine physiopathological mechanisms, therapeutic mechanisms, and certain prognostics in children with distinct pathologies.
Although there are centers around the world that study pulmonary function, the application of the results to medical care has not been generalized for various reasons: (1) some of the physiological principles on which the methods are based are still not sufficiently understood; (2) the instruments for measurement are complex and costly; (3) the procedures are lengthy and require sedation of the patient; and (4) there is no standardized form of these methods. However, in certain clinical situations it is appropriate to measure pulmonary function in the first years of life (Table 8.1).
Measurement Conditions
Infants who are to be assessed through a functional respiratory study should fast for the previous 4 hours and be examined to rule out certain conditions in which the procedure is not advised, such as fever or the presence of secretions in the upper airway. The patient’s height and weight should be measured and the results should be compared with theoretical values. Prior to the procedure, 50–75 mg/kg of chloral hydrate is administered orally to induce a relaxed sleep, which in most cases lasts for 90–120 minutes. It is considered high-risk to administer this medication to patients with severe upper airway obstruction or those with some degree of hepatic, renal, or cardiac insufficiency.
The patient should be in a supine position during the study, with his or her head held straight in hyperextension. Small movements and flexing of the neck can alter the results and thus should be avoided. Arterial oxygen saturation and the heart rate are monitored continuously with an oximeter.
Methods
Measurement of Forced Expiratory Flow
Understandably, small children cannot perform maximum forced exhalations based on their total lung capacity for evaluation of the caliber of the peripheral airways. Different methods are used to prompt infants and small children to exhale forcibly. Deflation techniques, rapid thoracic compression at the tidal volume (RC-RTC), and rapid thoracoabdominal compression: RTC with preinsufflation are used to determine the magnitude of bronchial obstruction and variations in obstruction after administration of a bronchodilator or a bronchoconstrictor agent.
The deflation technique was the first to be developed, but it is no longer used, because it requires heavy sedation and intubation of the patient. Consequently, in this chapter, we discuss the other two methods.
Rapid Thoracoabdominal Compression Technique at Current Volume
Adler et al. (1978) and Taussig et al. (1982) described the rapid thoracoabdominal compression technique for determining the bronchial caliber in infants. It has been used to describe the normal growth and development of the airways in infancy, on the basis of which equations have been developed to establish the magnitude of bronchial obstruction, using a standard deviation score as a function of the sex and size of the subject. With this, the observed alterations in the functional response to the treatments applied in the respiratory clinic can be identified and evaluated.
The technique employs an inflatable vest inside another inextensible vest around the child’s chest and stomach, which goes from the armpits to the pubis, with the child’s arms outside both jackets. A reserve air tank connected to the inflatable jacket transmits air at the end of the inhalation, with sufficient pressure to produce rapid thoracoabdominal compression (Fig. 8.1). Expiratory flows are registered during forced exhalation by a pneumotachograph equipped with a facial mask, which hermetically covers the nose and mouth of the patient. The resulting flow/volume curve is graphed in real time on a computer screen. The curve characteristically presents a rapid rise in the expiratory flow until the peak expiratory flow (PEF) is reached, and then it gradually descends to a point below the one established as the functional residual capacity (FRC). The flow obtained at this point is termed VFRC. To determine the limitation in airflow, the maneuver is progressively repeated with more pressure on the jacket, ranging between +20 and +100 cm of water. The maximum flow at the FRC (VmaxFRC), which correlates with the airway caliber, is determined by applying the pressure that yields the highest VFRC values (Fig. 8.2).
While the highest pressures have no limit in relation to airflow in healthy infants, this is not the case in patients with bronchial obstruction, where much less pressure is required. Abrupt falls in airflow are attributed to glottic or pharyngeal closure, and they can be corrected according to the correct location in the neck. At least three acceptable and reproducible curves are obtained with maximum FRC values that do not vary by more than 10%, and VmaxFRC is the average of the three values. The curves obtained with this method are “partial,” given that they are based not on the total pulmonary capacity but, rather, on the end of the inspiration at the current volume.
Rapid Thoracoabdominal Compression Technique at a Volume with Previous Insufflation
A modification of the technique described above has recently been developed to obtain, in a noninvasive way, better forced expiratory curves. The equipment used is similar to that used for the other technique, with the addition of an insufflation system to take the patient close to his or her total pulmonary capacity immediately before the thoracoabdominal compression (Fig. 8.3).
The insufflation system consists of an external source of air, valves to automatically occlude the airway or a Y connector for manual insufflation, and a safety valve to control the insufflation pressure. The jacket reaches maximum pressure in 70–100 milliseconds. Given that there is a small delay between insufflation and compression, it is a common practice to activate the compression 10–100 milliseconds before releasing the occlusion of the airway. One of the main discrepancies among users has been the application of different insufflation pressures to reach higher volumes. However, there is a consensus in the application of 30 cm of water pressure for older infants and 20 cm of water pressure for newborns and premature babies. The inspiratory flow is established at 1.5 times the current flow. The real pressure at the level of the mouth is monitored in real time so that the operator can adjust the flows and optimize the pressure being administered. There are also disparate criteria in the ventilation pattern before the forced expiration. The pulmonary insufflation rate depends on the lung volume and flow magnitude, while the volume reached for a standard pressure is directly proportional to the infant’s level of respiratory compliance. Most authors suggest 2–5 successive insufflations until pressure and volume plateaus are reached.
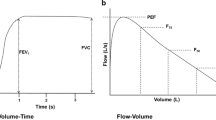
The most relevant functional parameters are obtained on the basis of the “maximum” forced curve of volume/time and flow/volume (Fig. 8.4)—namely, the forced vital capacity (FVC), forced expiratory volume (FEV) in 0.5 seconds (FEV0.5), and forced expiratory flow at 25–75% of FVC (FEF25–75). Other parameters that can be considered are the expiratory flows at 50%, 75%, and 85% of FVC, and FEV0.4 in small children. The parameters that are reported are those that are obtained on the basis of the “best curve,” and at least two values that do not differ by more than 10% should be used, with the better value reported. Similarly, the results refer to theoretical values.
Analysis of Breathing at Current Volume
Analysis of the curves obtained during current breathing is useful for functional respiratory assessment of infants, given that they yield greater variability and lower levels of specificity. However, there are different parameters that can be obtained from observing the flow curves/tidal volumes that allow for establishment of obstructive and low-compliance patterns (Fig. 8.5).
Simply by the airtight mask being placed on the patient’s face and attached to the pneumotachograph, the flow and volume signals are integrated to determine:
-
(a)
Parameters that are altered in pulmonary elastic retraction disorders: the rate between the peak expiratory flow and current volume (PEF/Vc)
-
(b)
Parameters that vary with obstructive pathologies: the percentages of volume and time to reach PEF
Some epidemiological studies have considered these measurements because of their technical simplicity in comparison with other methods.
Measurement of Respiratory Mechanics
Respiratory mechanics can be assessed by dynamic or passive methods. The respiratory cycle is not interrupted during measurements done with dynamic methods, whereas it is interrupted with use of passive methods. Body plethysmography and pressure/volume curves are dynamic methods. The main advantages of these methods are their greater sensitivity and specificity. Pressure/volume curves are particularly useful to optimize mechanical respiratory assistance in ventilated patients. However, dynamic methods are not widely used, because they require sophisticated personnel and intubation of the patient.
Passive methods include single- and multiple-occlusion techniques, which assess changes in flow or volume in relation to changes in pressure at the level of the mouth during periods of relaxation of the respiratory muscles, triggered by the Hering–Breuer reflex in the occlusion of the airway at the end of the inspiration. The time constant of the respiratory system is thus determined on the basis of the slope of the flow/volume curve. The compliance and resistance of the respiratory system are then calculated. Passive methods are simple, rapid, and noninvasive, although they assess the entire respiratory system and not just the lungs.
Measurement of Lung Volume
FRC is defined as the volume of gas that remains in the lungs after a passive exhalation. It is the result of the balance between the force of elastic lung retraction and the expansive capacity of the rib cage. It is also the easiest method for obtaining precise and reproducible lung volume values when the patient is incapable of cooperating. The FRC is increased when air is trapped (obstructive pathologies), and it is lower in patients with restrictive pathologies. Consequently, determining the FRC allows us to differentiate these processes functionally. It also provides an objective parameter for following lung growth and development, although it does not provide information about the number or size of the alveoli.
The FRC can be quantified by two methods, which are discussed in the following sections.
Body Plethysmography
The principle of this technique is the same as that of plethysmography in older children and adults. The child is placed in a supine position in a hermetic box (plethysmograph) while breathing through a facial mask connected to a pneumotachograph. At the end of an inspiration current, the circuit is closed for 6–10 seconds, making the child breathe against the closed system. As the pressure in the lung decreases and its volume increases, the opposite occurs in the plethysmograph. The FRC is determined by applying Boyle’s law (the product of pressure (P) and volume (V) are always constant in a closed system at a constant temperature: P × V = P’ x V’). This technique measures all of the gas in the thoracic cavity, which is the areas that communicate with the airway and the areas that do not. As we saw before, the plethysmograph can also determine the airway resistance.
Multiple-Breath Washout
The multiple-breath washout (MBW) method is based on dilution of a marker gas to a known concentration in an unknown volume (the FRC) over multiple current breaths. This can be done in two ways:
-
MBW using gases that are not involved in the gas exchange and are not absorbed into the blood flow or secreted by the tissues (helium or sulfur hexafluoride): The patient inhales a gas mixture with the gas marker until it reaches an equilibrium concentration (the same concentration for inhaling and exhaling). From this moment on, the patient begins to breathe environmental air (the washout principal phase) and the gas marker is lowered until it reaches a concentration lower than 2.5% of its initial concentration.
-
Nitrogen MBW: The patient washes out the N2 in his or her lungs by inhaling 100% O2 in multiple breaths.
The child should be asleep (not necessarily sedated) in order to obtain a stable breathing pattern. An airtight facial mask is placed on the child’s face, covering the mouth and nose. The mask is connected to the pneumotachograph and a mass spectrometer (or an ultrasonic transducer), which quantifies the concentration of the gases. The FRC is reported in millimeters as the average of three technically acceptable maneuvers with values that do not differ by more than 10%. There are different reference values for gas dilution methods using N2 or He, as well as for the plethysmography method.
Lung Clearance Index
The Lung Clearance Index (LCI) can be determined with the gas dilution technique, which evaluates the distribution or degree of homogeneity of pulmonary ventilation. A high index indicates obstruction of the small airways. This reflects a nonhomogeneous ventilator pattern, which slows the N2 (or marker gas) lavage at those zones with air trapping. This index is calculated by dividing the volume of exhaled volume (until the marker gas has been washed out and reaches a concentration of one fortieth of its initial concentration) by the FRC. A clearance index under 7.8 is considered normal regardless of the patient’s sex, age, height, and weight. Its measurement is simple and noninvasive, and it has low variability and good reproducibility. The measurements are done three times, the FRC is noted, and the average lung clearance index of the three maneuvers is calculated. Because this method gives information about the peripheral airway (also called the “silent zones”), its clinical utility has been studied more extensively in patients with cystic fibrosis. It has been shown that this parameter is altered before the appearance of symptoms, making it possible to explore different therapeutic choices at an early stage. In the same way, the studies conducted in these patients have shown good correlation with the changes in high-resolution computerized tomography. Its usefulness in asthma and in chronic newborn lung diseases has been discussed, and it is still under investigation.
Study of the Diffusing Capacity of the Lung for Carbon Monoxide
Castillo et al. (2006) described determination of the diffusing capacity of the lung for carbon monoxide (DLCO), using the single-breath technique adapted for infants and small children. The test consists of placing the child (after sedation) in a supine position, breathing through a mask connected to a pneumotachograph and a mass spectrometer. As in the rapid thoracoabdominal compression technique at high volumes, the airway is insufflated at 20 cm of water pressure with a gaseous mixture (0.3% CO, 5% He, 21% O2, and the rest N2). The lungs remain insufflated for 6 seconds to diffuse the carbon, after which the child can exhale passively. The measurement principle is similar to that used to determine carbon monoxide diffusion in adults. The alveolar volume (AV) is determined by the gas dilution technique using He as the marker gas, and the diffusion capacity of the alveolar–capillary membrane is determined by measuring the concentration of exhaled carbon. The measurements are done three times and the AV and CO diffusion are noted. The value considered is the average of three technically acceptable measurements with values that do not differ from each other by more than 10%. Because anemia or polycythemia alter CO diffusion values, Hb must be determined beforehand in order to correct for altered carbon monoxide diffusion. With this method, the physiological shape of the surface that is available for gas exchange can be evaluated; therefore, alveolar growth and development can be studied without use of anatomopathological studies. Studies conducted in premature babies have shown a change in normal alveolar development. These children present an AV that is similar to that seen in term children, but they have a smaller area for gas exchange because the alveoli are larger and fewer in number. This technique may be useful in extremely premature patients to evaluate alveolar growth and development, as well as responses to different treatments. Besides this, the technique may be used to valuate children with lung hypoplasia, for follow-up of children treated with lung resections early in life, or in patients with necrotized parenchymal areas. Finally, this technique provides an objective parameter to establish a diagnosis and follow-up of interstitial diseases during the first years of life. However, commercial equipment to measure carbon monoxide diffusion in infants has not been developed yet, and its use is currently restricted to research practices.
Fraction of Exhaled Nitric Oxide
Measurement of the fraction of exhaled nitric oxide (FeNO) has recently emerged as a tool for evaluating, managing, and diagnosing asthma. Its determination is simple and it gives information about eosinophilic inflammation in the airway noninvasively. High nitric oxide levels are related to the increase of eosinophils in induced sputum, bronchoalveolar lavage, and bronchial biopsy materials. Atopic and asthmatic adults and children present high levels, which drop after anti-inflammatory treatment. Technically, determination of the fractional exhaled nitric oxide is done using a chemiluminescent analyzer. In infants it can be performed through the “current breathing technique” and the measurement can be done online (in real time) or offline (when the air is kept in a hermetic bag and is measured afterward). When the child is asleep (it can also be done during spontaneous sleep), the values for 1 minute are registered while the child breathes at his or her current breathing volume through a facial mask connected to a pneumotachograph and the fractional exhaled nitric oxide analyzer. It is reported as the average result of three technically accepted maneuvers with results that do not differ from each other by more than 10%. For this technique, the normal values considered are between 2 and 8 particles per billion (ppb).
Pulmonary Function in Preschool Children
Spirometry
Children aged 2–5 years present particular challenges for conducting pulmonary function tests, including lack of attention and cooperation, besides fear of the equipment that is used.
A variable to consider is the fact that preschool children exhale lung volumes faster than adults; therefore, evaluations of FEV0.4, FEV0.5, and FEV0.75 are more important. Besides this, because of the smaller volumes that these subjects move, the equipment should include minimum dead space.
In the past, it was thought that children were incapable of acceptably carrying out the FVC maneuver and achieving maximum inspiration and expiration, because of lack of attention and concentration, besides low tolerance of frustration. This is why spirometry reference tables such as the Polgar and Knudson tables do not include measurements for children under 110 cm in height or under 6 years of age. Consequently, the reference values for small children have been extrapolated from those for older children.
However, the first spirometry studies of healthy 3- to 6-year-old children have been published in recent years. The measurement of pulmonary function takes into account the recommendations that (1) this should be done by an experienced technician, and (2) time should be taken prior to the procedure to explain what it involves and to demonstrate the maneuver.
There is no consensus about the benefits of using a nasal clip in open-circuit spirometry. It can depend on the experience of the technician who conducts the study, and its use can be decided for each individual patient to obtain the best FVC reading. The maneuvers are repeated until three acceptable curves have been obtained. The study should be brief, lasting no more than 15 minutes. Different interactive programs can be used with games on the spirometry screen to facilitate acquisition of adequate curves. If the patient cries during the study, there should be no further attempt, and the test should instead be done at another opportunity.
The maneuvers that are considered unacceptable are the ones in which:
-
The maximum flow cannot be clearly identified.
-
The expiratory effort stops abruptly at a point where it is less than 25% of the maximum flow.
-
The expiratory flow lasts for less than 1 second.
-
The child’s inspiration is not greater than his or her current volume.
-
There is a high degree of variability.
With these criteria, acceptable spirometry results are obtained in more than 80% of studied 3- to 6-year-old children, including both healthy children and those affected by different pathologies.
Forced Oscillation Technique
Advances have been made in the clinical study of pulmonary function using the forced oscillation technique (FOT), as described by Arthur DuBois in 1956. The necessary equipment to conduct this procedure is readily accessible and easy to use, and it requires a minimum of cooperation on the part of the patient. The child puts on the mouthpiece and the nasal clip, and breathes at his or her current volume for 17 seconds while holding his or her cheeks with both hands. The equipment creates a pulsating airflow at different oscillation frequencies, which may be measured in one maneuver, or each frequency can be studied in an individual maneuver. In this way, the resistance is measured and then calculated using a mathematical model of compliance. This technique measures the resistance of the entire respiratory system and provides information to ascertain if the resistance is increased in the central or peripheral airway. The bronchodilator response can be evaluated; if the resistance measured at 5 Hz falls by at least 30% of the basal value, the bronchodilator response is considered positive. The limitation of the forced oscillation technique is the difficulty in distinguishing between an obstructive pattern and a restrictive pattern. The main advantage of the technique is that it requires a minimum of cooperation from the patient; therefore, it can be used in patients while they sleep, with patients under mechanical ventilatory assistance, and also in children who are too young for acquisition of an acceptable result using the forced capacity maneuver. In the same way, it is a valid method to study patients with a collapsed airway, as can happen in cystic fibrosis or emphysema. In these cases, it is the ideal method to assess the bronchodilator response. In 2004, the European Respiratory Society published a standardization of the methodology, with recommendations for its clinical use, and stated that the diagnostic capacity of the method is equal to that of spirometry in patients with obstructive disorders.
Interrupter Resistance Technique
The interrupter resistance (Rint) technique allows noninvasive measurement of the resistance of the respiratory system while being normally breathing. Its main advantages are its simplicity, the need for minimal patient cooperation, and the fact that it requires only a small portable apparatus.
Among its principles are concepts that were first described in 1927, when it was proposed to estimate alveolar pressure by rapid occlusion of the airway during the respiratory cycle at rest, supposing that alveolar pressure will be equal to the pressure in the mouth.
The respiratory cycle is interrupted briefly (for <100 milliseconds) in the occlusion technique. The resistance (Rint) and pressure/flow rate are calculated from how the pressure rate changes in comparison with the flow evaluated in the respiratory airway before or after the occlusion (depending on the technique). While occlusion can be done during inspiration or expiration, both the American Thoracic Society and the European Respiratory Society recommend measurement during expiration.
Both entities have standardized norms to measure the mechanical properties of the respiratory system through occlusion techniques.
Hyperactivity Studies in Preschool Children
Forced oscillation and multiple occlusion are alternatives to spirometry to assess bronchial hyperactivity in preschool children. The two techniques used with uncooperative children—the transcutaneous oxygen pressure measurement and the tracheal auscultation method–merit certain attention. In this last test, the parameter to be determined is called PCwheeze, and it is defined as the concentration of bronchoconstrictor substance with which wheezing is heard in the trachea and lung fields. With the transcutaneous oxygen measurement method, the value in question is the concentration of methacholine that causes a 5% fall from the baseline value or an increase of 50% in the baseline heart frequency.
Sources
American Thoracic Society, European Respiratory Society. ATS/ERS statement: raised volume forced expirations in infants guidelines for current practice. Am J Respir Crit Care Med. 2005;172:1463–71.
Adler SM, Wohl MEB 1978 Flow-volume relationships at low lung volumes in healthy newborn infants. Pediatrics 61:636–40.
Aurora P, Gustafsson P, Bush A, Lindblad A, et al. Multiple breath inert gas washout as a measure of ventilation distribution in children with cystic fibrosis. Thorax. 2004;59(12):1068–73.
Balinotti J, Chakr V, Tiller C, Kimmel R, et al. Growth of lung parenchyma in infants and toddlers with chronic lung disease of infancy. Am J Respir Crit Care Med. 2010;181(10):1093–7.
Balinotti JE, Tiller CJ, Llapur CJ, Jones MH, et al. Growth of the lung parenchyma early in life. Am J Respir Crit Care Med. 2009;179(2):134–7.
Castillo A, Llapur CJ, Martinez T, Kisling J, et al. Measurement of single breath–hold carbon monoxide diffusing capacity in healthy infants and toddlers. Pediatr Pulmonol. 2006;41(6):544–50.
Delacourt C, Lorino H, Fuhrman C, Herve-Guillot M, Reinert P, Harf A, Housset B. Comparison of the forced oscillation technique and the interrupter technique for assessing airway obstruction and its reversibility in children. Am J Respir Crit Care Med. 2001;164(6):965–72.
Dubois AB, Botelho SY, Comroe JH Jr. A new method for measuring airway resistance in man using a body plethysmograph: values in normal subjects and in patients with respiratory disease. J Clin Invest. 1956 Mar;35(3):327–335.
Dubois AB, Brody AW, Lewis DH, Burgess BF Jr. Oscillation mechanics of lungs and chest in man. J Appl Physiol. 1956 May;8(6):587–594.
Hellinckx J, Cauberghs M, De Boeck K, Demedts M. Evaluation of impulse oscillation system: comparison with forced oscillation technique and body plethysmography. Eur Respir J. 2001;18(3):564–70.
Hoo AF, Dezateux C, Hanrahan JP, Cole TJ, Tepper RS, Stocks J. Sex-specific prediction equations for VmaxFRC in infancy: a multicenter collaborative study. Am J Respir Crit Care Med. 2002;165:1084–92.
Horsley AR, Gustafsson PM, Macleod KA, Saunders C, et al. Lung clearance index is a sensitive, repeatable and practical measure of airways disease in adults with cystic fibrosis. Thorax. 2008;63:135–40.
Jones MH, Castile R, Davis S, Kisling J, et al. Forced expiratory flows and volumes in infants: normative data and lung growth. Am J Respir Crit Care Med. 2000;161:353–9.
Morgan WJ, Geller DE, Tepper RS, et al. Partial expiratory flow–volume curves in infants and young children. Pediatr Pulmonol. 1988;5:232–43.
Nystad W, Samuelsen S, Nafstad P, Edvardsen E, Stensrud T, Jaakkola J. Feasibility of measuring lung function in preschool children. Thorax. 2002;57:1021–7.
Stam H, Van den Beek A, Grunberg K, Stijnen T, et al. Pulmonary diffusing capacity at reduced alveolar volumes in children. Pediatr Pulmonol. 1996;21:84–9.
Taussig LM, Landau LI, Godfrey S, Arad I. Determinants of forced expiratory flows in newborn infants. J Appl Physiol. 1982;53:1220–7.
Tepper RS, Morgan WJ, Cota K, et al. Expiratory flow limitation in infants with bronchopulmonary dysplasia. J Pediatr. 1986a;109:1040–6.
Tepper RS, Morgan WJ, Cota K, et al. Physiologic growth and development of the lung during the first year of life. Am Rev Respir Dis. 1986b;134:513–9.
Tepper RS, Reister T. Forced expiratory flows and lung volumes in normal infants. Pediatr Pulmonol. 1993;15:357–61.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Teper, A., Kofman, C., Colom, A. (2020). Evaluation of Pulmonary Function in Infants and Preschool Children. In: Bertrand, P., Sánchez, I. (eds) Pediatric Respiratory Diseases. Springer, Cham. https://doi.org/10.1007/978-3-030-26961-6_8
Download citation
DOI: https://doi.org/10.1007/978-3-030-26961-6_8
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-26960-9
Online ISBN: 978-3-030-26961-6
eBook Packages: MedicineMedicine (R0)