Abstract
Colorectal cancer is the second leading cause of cancer-related death in the Western world (Siegel et al. CA Cancer J Clin 68:7–30, 2018). One-half of patients with colorectal cancer will eventually develop metastatic disease. A subset of patients with disease localized to the liver are cured with surgical resection. Unfortunately, approximately 60% of patients will develop disease recurrence with nearly two-thirds having disease within the liver (Wei et al. Ann Surg Oncol 13:668–76, 2006; Wicherts et al. Ann Surg 248:994–1005, 2008; Choti et al. Ann Surg 235:759–66, 2002; Nanji et al. Ann Surg Oncol 20:295–304, 2013; House et al. J Am Coll Surgeons 210:744–52, 2010; Abdalla et al. Ann Surg 239:818–25, 2004). Techniques including nonanatomic parenchymal-sparing resections, success in induced hypertrophy of the remnant liver by portal vein embolization (PVE), and two-staged hepatectomy as well as associating liver partition and portal vein ligation (ALPPS) have enabled complete extirpation of colorectal liver metastasis (CRLM) at greater rates. Liver-directed therapy, including local and locoregional strategies, has allowed further treatment of liver lesions in distributions unfavorable for resection. Liver-directed therapy is often used in combination with resection with a goal to treat all visible tumors either by resection or tumor destruction with appropriate margins. Tumor recurrence after “curative” resection is a major problem. The majority of patients will die from recurrent disease, and liver metastases are the commonest cause of death for patients with colorectal cancer (House et al. J Am Coll Surgeons 210:744–52, 2010). Of patients who undergo liver resection, 50–75% will develop disease recurrence within 2 years after resection (Kun-Ming et al. World J Surg Oncol 12:155, 2014; Min-Su et al. Ann Surg Treat Res 87(1):14–21, 2014). Many recurrences are extra-hepatic; thus, adjuvant systemic treatment is standard of care after the management of CRLM.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
It is predicted that 140,250 new colorectal cancer cases will be diagnosed in the United States in 2018, with an estimated 50,630 cancer-related deaths [1]. Colorectal cancer is the second leading cause of cancer-related death in the Western world [1]. One-half of patients with colorectal cancer will eventually develop metastatic disease. A subset of patients with disease localized to the liver are cured with surgical resection. Unfortunately, approximately 60% of patients will develop disease recurrence with nearly two-thirds having disease within the liver [2,3,4,5,6,7]. Common extrahepatic sites of metastases include the thorax and peritoneum with metastatic patterns varying based on the site of primary tumor [8].
Techniques including nonanatomic parenchymal-sparing resections, success in induced hypertrophy of the remnant liver by portal vein embolization (PVE), and two-staged hepatectomy as well as associating liver partition and portal vein ligation (ALPPS) have enabled complete extirpation of colorectal liver metastasis (CRLM) at greater rates. Liver-directed therapy, including local and locoregional strategies, has allowed further treatment of liver lesions in distributions unfavorable for resection. Liver-directed therapy is often used in combination with resection with a goal to treat all visible tumors either by resection or tumor destruction with appropriate margins.
Tumor recurrence after “curative” resection is a major problem. The majority of patients will die from recurrent disease and liver metastases are the commonest cause of death for patients with colorectal cancer [6]. Of patients who undergo liver resection, 50–75% will develop disease recurrence within 2 years after resection [9, 10]. Many recurrences are extra-hepatic; thus, adjuvant systemic treatment is standard of care after the management of CRLM.
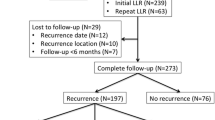
Following liver metastasectomy, 10-year survival rates of 20% have been reported [11]. Of note, this study analyzed patients treated prior to the introduction of modern chemotherapeutic agents. In a contemporary French multi-institutional retrospective cohort study including 2320 patients, Hallet et al. reported 5-year overall survival of 74.3% following hepatectomy in patients who did not have recurrence and 57.5% in patients with recurrent disease. Following hepatic metastasectomy, tumors recurred in 47.4% of patients at a median of 10 months follow-up. About 46.2% had intra-hepatic disease only and 31.8% combined intra- and extra-hepatic metastases. Pre-hepatectomy factors associated with increased rate of recurrence included node positive primary malignancy, more than three liver metastases, and largest metastasis greater than 4 cm. Patients with combined intra- and extra-hepatic recurrence had inferior outcomes with a 5-year overall survival rate of 44.3% compared with 60.8% for intra-hepatic recurrence alone and 64.3% for extra-hepatic recurrence alone. About 89.1% of patients presented within 3 years following initial hepatectomy. Authors emphasized the importance of highlighting to the patient that although extended survival is achievable, survivorship care is paramount, as repeat hepatectomy and further treatment may be needed moving forward [12].
Survivorship Care and Surveillance
There is limited data from which to recommend surveillance in patients with Stage IV colorectal cancer; however, the ability to address recurrent metastatic disease within the liver emphasizes the importance of close surveillance after metastasectomy. A key principle of surveillance is to monitor this high-risk patient cohort for recurrent disease. Timing and duration of follow-up is debatable. According to NCCN guidelines, patients with Stage IV colorectal cancer should be surveyed with a history and physical examination, and carcinoembryonic antigen (CEA) every 3–6 months for 2 years then every 6 months for a total of 5 years. A colonoscopy should be performed 1 year after colon resection, unless pre-operative colonoscopy was not completed due to an obstructing lesion, in which case a colonoscopy is recommended in 3–6 months. Further colonoscopic surveillance is dictated by findings. Computed tomography (CT) scan of the chest, abdomen, and pelvis is recommended at 3–6 month intervals for the first 2 years, then every 6–12 months for a total of 5 years [13].
Interestingly, in a study of post-treatment surveillance of patients with CRLM, frequency of surveillance imaging did not correlate with time to second procedure or median survival. Those who were scanned at 3–4 months intervals had a median survival of 43 months, compared to 54 months in those who were scanned once per year [14]. Positron emission tomography-magnetic resonance imaging (PET-MRI) has recently been investigated for CRLM detection. It was found to be superior to CT (p = 0.003) and PET-CT (p = 0.02) in detection of CRLM, especially those ≤1 cm in size, but not significantly different from MRI (p = 0.23) [15]. Other imaging modalities may be considered for surveillance purposes; however, these are not standard of care.
There is no evidence to recommend routine imaging or CEA beyond 5 years of follow-up. Considering cost and ease, it is not unreasonable to monitor long-term survivors with annual CEA levels. If serial CEAs show elevation, a workup including physical examination, colonoscopy, and CT of the chest, abdomen, and pelvis should be performed. When these investigations do not yield results, a PET-CT should be considered. Alternatively, repeat cross-sectional imaging should be performed in 3 months [13]. Recommendations provided by various organizations are displayed in Table 42.1 [13, 17,18,19,20,20]. Timing and duration should ultimately be determined by individual patient risk profile and performance status. The European Society for Medical Oncology (ESMO) emphasizes social, financial, and emotional aspects as well as functional outcomes to maximize survivors long-term well-being overall [17, 18].
Approach
The strategy in management of patients with liver recurrence after prior hepatectomy is similar to those who initially present with CRLM. Patients should be re-staged to evaluate for other sites of metastatic disease or local recurrence. This should consist of clinical examination, laboratory investigations including liver and renal functional tests, CEA level, as well as a CT or MRI of the abdomen, pelvis, and chest. PET-CT can add additional information on equivocal lesions. In patients with initial occurrence of CRLM, PET-CT should not be done routinely as it rarely changes surgical management [21]. However, PET-CT may detect occult metastatic disease and decrease the number of futile operative procedures; therefore, in the high-risk cohort of patients with recurrent CRLM, PET-CT should be considered [22]. The consensus of a multidisciplinary committee involving surgeons, medical and radiation oncologist, interventional radiologists, and pathologists should drive treatment. Patient co-morbidities, performance status, previous surgical, locoregional, and systemic treatments, residual liver volume and function must be considered and will cumulatively dictate the treatment strategy.
First, one must determine if the patient has potentially resectable disease. If disease is resectable and the patient is an appropriate operative candidate, repeat hepatectomy should be discussed. Residual liver volume and quality must be carefully evaluated, particularly in patients who have had significant exposure to chemotherapy. It is well established that irinotecan and oxaliplatin induce steatohepatitis, sinusoidal obstruction, and periportal inflammation that can affect ability to perform large resections by impairing function of the liver remnant. These hepatic changes can negatively impact outcomes, with increased risk of liver failure and death [24,25,26,26]. When concerned, pre-operative biopsy of normal liver should be performed, and liver volumes should be calculated on imaging.
If disease is unresectable, patient wishes must be reviewed, with prolongation of survival, improved tumor-related symptoms, cessation of tumor progression, and maintained quality of life reasonable goals. The armamentarium of treatment options for palliation has expanded significantly with many systemic, locoregional, and local treatments available. Re-biopsy may be indicated for molecular and genetic analysis to drive newer targeted and immunotherapies (Fig. 42.1).
Surgery
Hepatectomy is the standard of care for those patients with initial presentation of resectable colorectal metastasis and remains the most well studied potentially curative treatment [7]. When disease recurs in the liver after previous resection, re-resection should be considered. In fact, 20–30% of patients will be surgical candidates with disease amendable to surgery [27, 28]. One must consider patient performance status and assess for adequate hepatic reserve. Additionally, surgeons should expect these to be challenging cases with abdominal and perihepatic adhesions, altered liver anatomy with variations in position of vasculature and the biliary system secondary to previous operations and liver regeneration. Longer surgery times, greater risk of operative bleeding, increased risk of organ damage, and postoperative complications have been reported [3].
The SEPTRA-C2T Phase II randomized control trial supports the use of bioresorbable membranes to reduce abdominal and perihepatic adhesions in two-stage hepatectomy. These results can likely be extrapolated to re-resection, as this study included repeat hepatectomy up to 6 months [29]. Authors showed a 33% decrease in time to complete liver mobilization and the proportion of patients with one or more complications was half that observed in the control group [29].
The first series of repeat hepatectomy was reported as early as 1989 [30]. Since then, many centers have published their results, with survival rates of 29–70%, mortality of less than 3%, and perioperative complications comparable to initial resection [27, 28, 32,33,34,34]. A bi-institutional analysis of repeat liver resections for recurrent CRLM including 126 patients showed 1-, 3-, and 5-year survival rates of 86%, 51%, and 34%, respectively [35]. Favorable outcomes likely reflect careful selection of patients with limited disease and favorable tumor biology, the majority of patients in this study (71%) underwent minor liver-resections. Nanji et al. in a population-based study of 1310 patients who underwent hepatic resection for CRLM with 6% (n = 78) undergoing repeat resection, showed comparable short-term postoperative outcomes with trends towards higher rates of postoperative mortality and readmission rates although these were not statistically significant. Median overall-survival was 86 months and cancer-specific survival 74 months from time of initial liver resection. 5-year overall survival from time of first resection was 60% [36]. A systematic review of repeat hepatectomy for CRLM, included 22 observational studies with a total of 1610 patients reporting a recurrence rate of 64% at median follow-up of 32 months. Median overall survival was 35 months, with 3- and 5-year survival rates of 55% and 42%, respectively [37]. As mentioned, parenchymal-preserving strategies with initial hepatectomy, afford further options for subsequent operation in the case of liver recurrence.
Resection may be of benefit in the setting of concurrent extrahepatic disease. Leung et al. in their retrospective review of 219 patients who underwent hepatectomy for CRLM and resection of synchronous extrahepatic disease showed that long-term survival was possible but that true cure was rare [38]. Pulmonary colorectal metastases are amendable to resection when the primary tumor has been resected for cure (R0) and complete resection of lung disease with maintenance of adequate lung function is attainable. Additionally, re-resection of pulmonary lesions may be considered in select patients [13]. Five-year overall survival of 49% has been reported for re-resection of hepatic and pulmonary metastasis [39]. Other modalities for management of pulmonary metastases include ablative techniques and stereotactic beam radiation therapy (SBRT) both of which are potential treatment options for liver disease and will be discussed further.
There are scenarios where even when disease is resectable, this may not be the best option for the patient. Passot et al. looked at outcomes comparing RAS mutation status, with mutated RAS representing 15–35% of colorectal cancer patients. They defined three high-risk factors associated with poor prognosis: largest liver metastasis >3 cm, more than seven cycles of pre-operative chemotherapy, and node positive primary tumor. Those patients with all three factors were found to have a median survival of only 22 months with no 4-year survivors. Their survival outcomes are comparable to patients treated with modern chemotherapy alone leading authors to conclude that hepatectomy may be ill advised in patients with this mutational status [40]. Additionally, RAS mutations have been associated with a higher incidence of extra-hepatic brain, bone and lung relapse, reflective of poor tumor biology [41, 42].
Similarly, BRAF mutations, reported in 2–4% of CRLM, are poor prognostic biomarkers associated with worse survival outcomes after liver resection [43,44,44]. The low frequency of this mutation in resected CRLM is likely attributable to the fact that BRAF mutant colorectal cancer patients more commonly develop peritoneal metastases and less frequency liver-limited disease and are therefore often are not amenable to surgical metastasectomy [44]. In a multicenter trial from Italy, patients who underwent liver resection for CRLM with available mutational status data were analyzed. BRAF mutants had the worst recurrence free and overall survival, 5.7 and 22.6 months, respectively [42]. As we begin to better understand tumor genomics, mutational status should be considered in clinical decision making of CRLM management.
Systemic Treatment
Systemic chemotherapy plays an important role in the multimodal treatment of CRLM. With disease recurrence that is unresectable the realistic goal of systemic treatment is palliative. Modern chemotherapeutic and biologics have resulted in prolonged median overall survival in patients with CRLM between 29 and 37 months [45, 46]. Standard first-line combinations include cytotoxics 5-fluorouracil or capecitabine in combination with oxaliplatin (FOLFOX or CAPOX) or irinotecan (FOLFIRI). A 3-drug combination (FOLOXIRI) can be considered in younger patients with good performance status, but it is associated with significant toxicity. Targeted agents including bevacizumab for RAS mutants and bevacizumab, cetuximab, or panitumumab for RAS wild-type tumors are now standard of care.
Generally intensive first line strategies are used for a period followed by less intensive, maintenance therapy, until progression. The CAIRO3 study, a Phase III multicenter randomized controlled trial, assessed capecitabine plus bevacizumab maintenance therapy following six cycles of intensive first line treatment, CAPOX-bevacizumab. This regimen was found to be effective without compromising quality of life [47].
Testing for mismatch-repair (MMR) status is indicated, as immunotherapy is an option in a subset of patients based on genetic status. Le et al. evaluated pembrolizumab, an antiprogrammed death 1 immune checkpoint inhibitor, in patients with treatment refractory metastatic colorectal cancer. MMR-deficient colorectal cancer was compared to MMR-proficient colorectal cancer and MMR-deficient other primary cancers. Immune-related objective response rate and immune-related progression-free survival rates were reported as 40% and 78%, respectively, for MMR-deficient colorectal cancer patients, superior to MMR-proficient patients, 0% and 11%, respectively. Similar results were observed for MMR-deficient noncolorectal cancer [48]. Newer targeted therapies and clinical trials of such may be options for patients and should be explored for treatment refractory patients.
Once tumors become chemo-refractory, survival estimates are poor, 4–5 months [50,51,51]. Palliative chemotherapy was once the only option; however, locoregional strategies have been investigated in patients with chemo-refractory disease with reasonable results. Options include ablation, hepatic artery infusion (HAI) chemotherapy, radioembolization (90Y), transarterial embolization (bland or chemo), and SBRT (Fig. 42.2).
Locoregional Therapy
Ablation
Ablation includes radiofrequency, microwave, cryoablation, and irreversible electroporation. It is a locoregional alternative to resection that can be used with curative or palliative intent. If complete ablation can be performed, which may be more parenchymal sparing for certain tumors, especially in patients who have previously undergone liver resection, this treatment option can be potentially curative. Under image guidance, ablation can be performed percutaneously, laparoscopically, or by open surgery destroying liver tumors without removing them. Ideal candidates are patients with inadequate liver function, anatomic distribution incompatible with resection, or significant comorbid conditions making resection less desirable. Complications range from low-grade fevers, transient elevations of liver function tests and abdominal pain to hemorrhage, abscess, biloma, biliary fistula, hepatic insufficiency, arteriovenous fistulas, portal vein thromboses, diaphragmatic hernia, tumor implantation, and thermal injury to surrounding structures [52]. A standardized post ablation protocol has not been defined. Both laboratory (CEA) and imaging (contrast enhanced ultrasound, CT, MRI, or PET-CT) surveillance at 1 and 3 months is recommended to ensure complete treatment, followed by return to previous surveillance protocol.
No randomized data is available comparing ablation to resection for CRLM or CRLM recurrence. A meta-analysis including 13 studies published between 2003 and 2011 compared radiofrequency ablation to surgical resection finding inferior overall survival and disease-free survival with ablation [53]. Otto et al., in a prospective nonrandomized trial of radiofrequency ablation compared to resection in early CRLM amenable to surgery found that survival did not depend on the treatment modality, but that local recurrence was significantly higher after ablation (32% vs. 4%, p < 0.001) [54]. Similarly, when compared to surgical re-resection, ablation results in shorter progression free survival (10.2 vs. 4.3 months, p = 0.002); however, median overall survival was reported as the same, 33.3 months. Ablation is associated with shorter hospital stay (1 vs. 5 days, p = 2 × 10−10) and post-procedure morbidity has been reported as significantly lower (12.1% vs. 38.7%, p = 0.021) [55]. So long as a complete ablation can be performed, the results would be expected to be similar to an adequately performed resection.
Synergy of ablative techniques with other treatment modalities has been demonstrated. Combining intra-operative ablation with resection in cases that would otherwise be unresectable has shown favorable results [56]. The CLOCC trial, a prospective randomized trial comparing systemic therapy alone to systemic therapy in combination with ablation with or without surgical resection for unresectable CRLM, demonstrated both improved progression free survival and overall survival with combination therapy (p = 0.01) [57]. The therapeutic debate continues for CRLM amenable to resection; however, ablation has established a role and is particularly appealing in cases of CRLM recurrence when resection may be particularly challenging if not impossible.
Hepatic Arterial Infusion (HAI) Chemotherapy
HAI of chemotherapy, specifically floxuridine (FUDR), is possible through a surgically implantable subcutaneous pump connected to a catheter placed in the gastroduodenal artery. Hepatic lesions derive the majority of their blood supply from hepatic arterial inflow in comparison to normal liver parenchyma, receiving majority of blood from the portal vein, thus maximizing treatment effects. HAI treatment is complex and requires multidisciplinary skills in placement and management. The chemotherapeutic agent of choice, FUDR, is ideal because of its high first pass extraction in the liver. This enables high doses of treatment with minimal systemic exposure [58]. Biliary toxicities can be significant. The administration of dexamethasone through the pump has been found to decrease rates; however, it is important to closely monitor liver function tests while receiving treatment [59]. Other complications include thrombosis, dislodgement, extra-hepatic perfusion, incomplete perfusion, pump malfunction, pocket infection, hematoma, pump migration, catheter occlusion, dislodgement, erosion, arterial hemorrhage [60].
Ammori et al. reported a decade of experience with HAI in combination with systemic therapy for conversion of unresectable CRLM. Despite extensive disease, 25% of patients responded sufficiently to undergo resection or ablation of their CRLM. During the study period, 14 patients underwent repeat resection or ablation for recurrence. Median 5-year survival from pump placement was 59 months in the conversion group compared to 16 months in the nonconversion group (p < 0.001) [61]. With combination HAI and systemic chemotherapy for unresectable CRLM, conversion rates as high as 47% have been reported [62].
Randomized controlled trials are needed in the assessment of HAI treatments to better define their role in the current era of systemic chemotherapeutics. In patients with unresectable CRLM HAI given in conjunction with systemic chemotherapy can improve response rates and increase the number of patients who go onto liver resection. Currently, HAI chemotherapy should be considered in patient with disease confined to the liver who have progressed on first line chemotherapy.
Selective Internal Radiation Therapy (SIRT)
Selective internal radiation therapy (SIRT) or radioembolization with yttrium-90 (90Y), a high-radiation beta-emitter bonded to resin or glass microspheres, has been used in tumors refractory to chemotherapy. Colorectal cancer cells are highly radiosensitive and tumors have increased microvascular density; therefore, delivery of intra-arterial brachytherapy results in high tumoral concentrations based on the principle that the blood supply of hepatic tumors is different than normal liver parenchyma. Segmental or lobar delivery can be utilized.
SIRT for liver tumors was first reported in 1965 [63]. It utilization for salvage therapy has shown consistent results with median overall survival of 10.5 months reported in several studies [65,66,67,67]. Common side effects include fatigue, abdominal pain, and nausea. Importantly, low rates of biochemical toxicity have been reported. Providers should be aware of uncommon, but serious side effects including radiation induced gastric ulcers, lymphocytopenia, jaundice, cholecystitis, lung toxicity, hepatic abscess, radiation hepatitis, and liver failure [68].
The Metastatic colorectal cancer liver metastases Outcomes after RadioEmbolization (MORE) study included 606 patients reporting a median overall survival from the first treatment with 90Y of 9.6 months. Performance status, tumor burden, number of previous chemotherapeutics, liver function, and no extra-hepatic disease predicted better survival. The collection period predated utilization of biologic chemotherapy agents and included a large proportion (35%) of patients with extra-hepatic disease who benefit less from liver-directed therapy (7.4 vs. 12.1 month survival; p < 0.001) [69]. Hickey et al. in a multi-institutional review of 531 patients reported median overall survival from diagnosis of primary colorectal tumor of 48.7 months, from diagnosis of CRLM of 37.7 months, and from 90Y treatment of 10.6 months. Again, outcomes were significantly better without extra-hepatic disease 14.4 months vs. 6.6 months (p < 0.001). Of note, 18% of patients had prior hepatic resection, 14% of patients had prior ablation, and 4% prior transarterial chemoembolization (TACE) [64]. Combined analysis of three multicenter randomized phase 3 trials, FOXFIRE, SIRFLOX, and FOXFIRE-Global showed that addition of SIRT to first-line chemotherapy for patient with liver-only or liver-dominant CRLM resulted in equivalent survival [70]. Given the results of these studies SIRT, and in particular 90Y microspheres, should be considered in highly selected patients with chemotherapy-refractory disease and predominant hepatic metastases.
The use of SIRT in down-staging for resection has been reported with favorable results [71, 72]. Conversion to resection has been reported at rates of 9–85%; however, most series include population with mixed primary pathologies and are biased by patient selection [73,74,74]. With the combined benefits of selective tumor treatment and induction of hypertrophy of untreated liver segments, the role of SIRT in down-staging should be further explored. Of note, traditional perfusion of hepatic segments cannot be assumed following previous liver resection; therefore, SIRT treatment and subsequent resection in the case of CRLM recurrence must be carefully planned.
TACE
Another transarterial treatment modality, TACE, targets tumor ischemia by embolization with delivery of intraarterial chemotherapy. TACE is most commonly used for unresectable hepatocellular carcinoma, but both bland hepatic artery embolization and TACE have been used for local control after CRLM progression during systemic chemotherapy. A randomized controlled trial of 70 patients compared drug-eluting beads with irinotecan (DEBIRI) in combination with FOLFOX to systemic chemotherapy alone showing improved overall response rate (76% vs. 60% at 6 months, p = 0.05) and median progression-free survival (15.3 vs. 7.6 months) with the addition of TACE [75]. Subsequent systematic review, including this study as well as 5 observational studies, of TACE with the use DEBIRI for unresectable CRLM reported improvement in median survival from 15 to 25 months [76]. This treatment is indicated after failure of other modalities, and more recently in conjunction with other locoregional treatments.
Stereotactic Bean Radiation Therapy (SBRT)
SBRT has enabled delivery of greater combined doses of radiation over the course of fewer treatments with local-control results comparable to resection with far fewer risks. Outcomes of SBRT for CRLM in a 60 patient cohort reported local control of 50% at 1-year and 26% at 4-years [77]. The results of the international multi-institutional RSSearch® Patient Registry, which included 427 patients with liver metastasis, CRLM being the most common (44%), showed a median overall survival of 27 months with 76% 1-year survival [78]. Risk of recurrence correlates with increased tumor size as well as dose regimen with documented tumor control of greater than 80% when optimized [79]. Radiation has also been used as salvage therapy for bilateral CRLM not amenable to second-stage hepatectomy [80].
Systematic prospective studies are required to further endorse this treatment option in the setting of CRLM. Currently SBRT can be considered in carefully selected patients or in the setting of a clinical trial. The benefits of this treatment modality include the short treatment time course with delivery over only a few fractions, the lack of need for recovery, as well as a favorable toxicity profile.
Conclusion
In summary, approximately 60% of patients with treated CRLM will develop disease recurrence. Of these, two-thirds will have recurrent liver metastases. Overall survival of 74.3% following hepatectomy in patients without recurrence and 57.5% in patients with recurrent disease have been reported by Hallet et al. in the era of contemporary chemotherapy [12]. The ability to address recurrent metastatic disease within the liver justifies close surveillance after metastasectomy with frequent clinical encounters, tumor markers, and imaging based on local guidelines. Intra-hepatic recurrence should be approached similarly to the initial presentation of CRLM. Re-staging must be performed to assess both intra- and extra-hepatic disease burden. In the case of liver recurrence amenable to resection hepatectomy should be considered, taking into account patient performance status and volume of the future liver remnant. Systemic therapy will play a role for all patients, with new targeted therapies and clinical trials providing options for chemorefractory disease. Liver-directed therapies including ablation, HAI chemotherapy, SIRT, TACE, and SBRT provide a large armamentarium of options for palliation. With continuously evolving treatment options, multidisciplinary care is critical in CRLM recurrence.
References
Siegel RL, Miller KD, Jemal A. Cancer statistics, 2018. CA Cancer J Clin. 2018;68:7–30.
Wei AC, Greig PD, Grant D, et al. Survival after hepatic resection for colorectal metastases: a 10-year experience. Ann Surg Oncol. 2006;13:668–76.
Wicherts DA, Miller R, de Haas RJ, et al. Long-term results of two stage hepatectomy for irresectable colorectal cancer liver metastases. Ann Surg. 2008;248:994–1005.
Choti MA, Sitzmann JV, Tiburi MF, et al. Trends in long-term survival following liver resection for hepatic colorectal metastases. Ann Surg. 2002;235:759–66.
Nanji S, Cleary S, Ryan P, et al. Up-front hepatic resection for metastatic colorectal cancer results in favorable long-term survival. Ann Surg Oncol. 2013;20:295–304.
House MG, Ito H, Gonen M, et al. Survival after hepatic resection for metastatic colorectal cancer: trends in outcomes for 1,600 patients during two decades at a single institution. J Am Coll Surgeons. 2010;210:744–52. 752–745.
Abdalla EK, Vauthey JN, Ellis LM, et al. Recurrence and outcomes following hepatic resection, radiofrequency ablation, and combined resection/ablation for colorectal liver metastases. Ann Surg. 2004;239:818–25.
Riihimaki M, Hemminki A, Sundquist J, et al. Patterns of metastasis in colon and rectal cancer. Sci Rep. 2016;6:29765.
Kun-Ming C, Tsung-Han W, Chih-Hsien C, Wei-Chen L, Jy-Ming C, Jinn-Shiun C, Jeng-Yi W. Prognostic significance of the number of tumors and aggressive surgical approach in colorectal cancer hepatic metastasis. World J Surg Oncol. 2014;12:155.
Min-Su P, Nam-Joon Y, Sang-Yong S, Tae Y, Suk-Won S, Young Rok C, Ki H, Geun H, Kyoung Bun L, et al. Histopathologic factors affecting tumor recurrence after hepatic resection in colorectal liver metastases. Ann Surg Treat Res. 2014;87(1):14–21.
Tomlinson JS, Jarnagin WR, DeMatteo RP, et al. Actual 10-year survival after resection of colorectal liver metastases defines cure. J Clin Oncol. 2007;25:4575–80.
Hallet J, Sa Cunha A, Adams R, et al. Factors influencing recurrence following initial hepatectomy for colorectal liver metastases. BJS. 2016;103:1366–76.
NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines): Colon Cancer. Version 2.2018, March 14, 2018. Available at: https://www.nccn.org/professionals/physician_gls/pdf/colon.pdf.
Hyder O, Dodson RM, Mayo SC, et al. Post-treatment surveillance of patients with colorectal cancer with surgically treated liver metastases. Surgery. 2013;154:256–65.
Lee DH, Lee JM, Hur BY, et al. Colorectal cancer liver metastases: diagnostic performance and prognostic value of PET/MR imaging. Radiology. 2016;280:782–92.
Steele S, Chang G, Hendren S, et al. Practice guideline for the surveillance of patients after curative treatment of colon and rectal cancer. Dis Colon Rectum. 2015;58:713–25.
Glynne-Jones R, Wyrwicz L, Tiret E, et al. Rectal cancer: ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2017;28:iv22–40.
Van Cutsem E, Cervantes A, Nordlinger B, et al. Metastatic colorectal cancer: ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2014;25:ii1–9.
Watanabe T, Muro K, Ajioka Y, et al. Japanese Society for Cancer of the Colon and Rectum (JSCCR) guidelines 2016 for the treatment of colorectal cancer. Int J Clin Oncol. 2018;23:1–34.
Cancer Care Ontario: Colorectal Cancer Follow-up Care Pathway Map. Version 2018.03, March 14, 2018. Available at: https://www.cancercareontario.ca/sites/ccocancercare/files/assets/DPMColorectalFollowUp.pdf.
Moulton CA, Gu CS, Law CH, et al. Effect of PET before liver resection on surgical management for colorectal adenocarcinoma metastases: a randomized clinical trial. JAMA. 2014;311:1863–9.
Fernandez FG, Drebin JA, Linehan DC, et al. Five-year survival after resection of hepatic metastases from colorectal cancer in patients screened by positron emission tomography with F-18 fluorodeoxyglucose (FGG-PET). Ann Surg. 2004;240:438–47.
Fernandez FG, Ritter J, Goodwin JW, Linehan DC, Hawkins WG, Strasberg SM. Effect of steatohepatitis associated with irinotecan or oxaliplatin pretreatment on resectability of hepatic colorectal metastases. J Am Coll Surg. 2005;200:845–53.
Vauthey JN, Pawlik TM, Ribero D, et al. Chemotherapy regimen predicts steatohepatitis and an increase in 90-day mortality after surgery for hepatic colorectal metastases. J Clin Oncol. 2006;24:2065–72.
Zorzi D, Laurent A, Pawlik TM, Lauwers GY, Vauthey JN, Abdalla EK. Chemotherapy-associated hepatotoxicity and surgery for colorectal liver metastases. Br J Surg. 2007;94:274–86.
Morris-Stiff G, Tan YM, Vauthey JN. Hepatic complications following preoperative chemotherapy with oxaliplatin or irinotecan for hepatic colorectal metastases. Eur J Surg Oncol. 2008;34:609–14.
De Jong MC, Pulitano C, Ribero D, et al. Rates and patterns of recurrence following curative intent surgery for colorectal liver metastasis: an international multi-institutional analysis of 1669 patients. Ann Surg. 2009;250:440–8.
Butte JM, Gonen M, Allen PJ, et al. Recurrence after partial hepatectomy for metastatic colorectal cancer: the potentially curative role of salvage re-resection. Ann Surg Oncol. 2015;22:2761–71.
Dupre A, Lefranc A, Buc E, et al. Use of bioresorbable membranes to reduce abdominal and perihepatic adhesions in 2-stage hepatectomy of liver metastases form colorectal cancer: results of a prospective, randomized controlled phase II trial. Ann Surg. 2013;258:30–6.
Lange JF, Leese T, Casting D, Bismuth H. Repeat hepatectomy for recurrent malignant tumors of the liver. Surg Gynecol Obstet. 1989;169:119–26.
Adair RA, Young AL, Cockbain AJ, et al. Repeat hepatic resection for colorectal liver metastases. Br J Surg. 2012;99:1278–83.
Pinson CW, Wright JK, Chapman WC, et al. Repeat hepatic surgery for colorectal cancer metastasis to the liver. Ann Surg. 1996;223:765–73. discussion 773–6
Lee H, Choi SH, Cho YB, et al. Repeat hepatic resection in patients with colorectal liver metastases. World J Gastroenterol. 2015;21:2124–30.
Saiura A, Yamamoto J, Koga R, et al. Favorable outcome after repeat resection for colorectal liver metastases. Ann Surg Oncol. 2014;21:4293–9.
Petrowsky H, Gonen M, Jarnagin W, et al. Second liver resections are safe and effective treatment for recurrent hepatic metastases from colorectal cancer: a bi-institutional analysis. Ann Surg. 2002;235:863–71.
Nanji S, Tsang ME, Wei X, et al. Outcomes after repeat hepatic resection for recurrent metastatic colorectal cancer: a population-based study. Am J Surg. 2017;213:1053–9.
Lam VWT, Pang T, Laurence JM, et al. A systematic review of repeat hepatectomy for recurrent colorectal liver metastases. J Gastrointest Surg. 2013;17:1312–21.
Leung U, Gonen M, Allen P, et al. Colorectal cancer liver metastases and concurrent extrahepatic disease treated with resection. Ann Surg. 2017;265:158–65.
Bellier J, De Wolf J, Hebbar M, et al. Repeated resections of hepatic and pulmonary metastasis from colorectal cancer provide long-term survival. World J Surg. 2018;42(4):1171–9.
Passot G, Denbo JW, Yamashita S, et al. Is hepatectomy justified for patients with RAS mutant colorectal liver metastases? An analysis of 524 patients undergoing curative liver resection. Surgery. 2017;161:332–40.
Kemeny N, Chou J, Capanu M, et al. KRAS mutation influences recurrence patterns in patients undergoing hepatic resection of colorectal metastases. Cancer. 2014;120:3965–71.
Schirripa M, Bergamo F, Cremolini C, et al. BRAF and RAS mutations as prognostic factors in metastatic colorectal cancer patients undergoing liver resection. Br J Cancer. 2015;9:1921–8.
Teng HW, Huang YC, Lin JK, et al. BRAF mutation is a prognostic biomarker for colorectal liver metastectomy. J Surg Oncol. 2012;106:123–9.
Yaeger R, Cereck A, Chou JF, et al. BRAF mutation predicts for poor outcomes after metastectomy in patients with metastatic colorectal cancer. Cancer. 2014;120:2316–24.
Heinemann V, von Weikersthal LF, Decker T, et al. FOLFIRI plus cetuximab versus FOLFIRI plus bevacizumab as first-line treatment for patients with metastatic colorectal cancer (FIRE-3): a randomised, open-label, phase 3 trial. Lancet Oncol. 2014;15:1065–75.
Cremolini C, Loupakis F, Antoniotti C, et al. FOLFOXIRI plus bevacizumab versus FOLFIRI plus bevacizumab as first-line treatment of patients with metastatic colorectal cancer: updated overall survival and molecular subgroup analysis of the open-label, phase 3 TRIBE study. Lancet Oncol. 2015;16:1306–15.
Simkens LH, van Tinteren H, ten Tije AJ, et al. Maintenance treatment with capecitabine and bevacizumab in metastatic colorectal cancer (CAIRO3): a phase 3 randomised controlled trial of the Dutch colorectal cancer group. Lancet. 2015;9:1843–52.
Le CT, Uram JN, Wang H, et al. PD-1 blockade in tumors with mismatch-repair deficiency. N Engl J Med. 2015;372:2509–20.
Grothey A, Van Cutsem E, Sobrero A, et al. Regorafenib monotherapy for previously treated metastatic colorectal cancer (CORRECT): an international, multicentre, randomised, placebo-controlled, phase 3 trial. Lancet. 2013;381:303–12.
Karapetis CS, Khambata-Ford S, Jonker DJ, et al. K-ras mutations and benefit from cetuximab in advanced colorectal cancer. N Engl J Med. 2008;359:1757–65.
Jonker DJ, O’Callaghan CJ, Karapetis CS, et al. Cetuximab for the treatment of colorectal cancer. N Engl J Med. 2007;357:2040–8.
Gervais DA, Goldberg SN, Brown DB, et al. Society of interventional radiology position statement on percutaneous radiofrequency ablation for the treatment of liver tumors. J Vasc Interv Radiol. 2009;20:S42–7.
Weng M, Zhang Y, Zhou D, et al. Radiofrequency ablation versus resection for colorectal liver metastases: a meta-analysis. PLoS One. 2012;7:e45493.
Otto G, Duber C, Hoppe-Lotichius M, et al. Radiofrequency ablation as first-line treatment in patients with early colorectal liver metastases amenable to surgery. Ann Surg. 2010;251:796–803.
Dupre A, Jones RP, Diaz-Nieto R, et al. Curative-intent treatment of recurrent colorectal liver metastases: a comparison between ablation and resection. Eur J Surg Oncol. 2017;43:1901–7.
Van Amerongen MJ, van der Stok EP, Futterer JJ, et al. Short term and long term results of patients with colorectal liver metastases undergoing surgery with or without radiofrequency ablation. Eur J Surg Oncol. 2016;42:523–30.
Ruers T, Van Coevorden F, Punt CJ, et al. Local treatment of unresectable colorectal liver metastases: results of a randomized phase II trial. J Natl Cancer Inst. 2017;109:djx015.
Ensminger WD, Gyves JW. Clinical pharmacology of hepatic arterial chemotherapy. Semin Oncol. 1983;10:176–82.
Kemeny N, Conti JA, Cohen A, et al. Phase II study of hepatic arterial floxuridine, leucovorin, and dexamethasone for unresectable liver metastases from colorectal carcinoma. J Clin Oncol. 1994;12:2288–95.
Allen PJ, Nissan A, Picon AI, et al. Technical complications oand durability of hepatic artery infusion pumps for unresectable colorectal liver metastases: an institutional experience of 544 consecutive cases. J Am Coll Surg. 2005;201:57–65.
Ammori JB, Kemeny NE, Fong Y, et al. Conversion to complete resection and/or ablation using hepatic artery infusional chemotherapy in patients with unresectable liver metastases from colorectal cancer: a decade of experience at a single institution. Ann Surg Oncol. 2013;20:2901–7.
D’Angelica MI, Correa-Gallego C, Paty PB, et al. Phase II trial of hepatic artery infusional and systemic chemotherapy for patients with unresectable hepatic metastases from colorectal cancer: conversion to resection and long-term outcomes. Ann Surg. 2015;261:353–60.
Ariel IM. Treatment of inoperable primary pancreatic and liver cancer by the intra-arterial administration of radioactive isotopes (y90 radiating microspheres). Ann Surg. 1965;162:267–78.
Hickey R, Lewandowski RJ, Prudhomme T, et al. 90Y radioembolization of colorectal hepatic metastases using glass microspheres: safety and survival outcomes from a 531-patient multicenter study. J Nucl Med. 2016;57:665–71.
Saxena A, Meteling B, Kapoor J, Golani S, Morris DL, Bester L. Is yttrium-90 radioembolization a viable treatment option for unresectable, chemorefractory colorectal cancer liver metastases? A large single-center experience of 302 patients. Ann Surg Oncol. 2015;22:794–802.
Lewandowski RJ, Memon K, Mulcahy MF, et al. Twelve-year experience of radioembolization for colorectal hepatic metastases in 214 patients: survival by era and chemotherapy. Eur J Nucl Med Mol Imaging. 2014;41:1861–9.
Kennedy AS, Coldwell D, Nutting C, et al. Resin 90Y-microsphere brachytherapy for unresectable colorectal liver metastases: modern USA experience. Int J Radiat Oncol Biol Phys. 2006;65:412–25.
Riaz A, Awais R, Salem R. Side effects of yttrium-90 radioembolization. Front Oncol. 2014;4:198.
Kennedy AS, Ball D, Cohen SJ, et al. Multicenter evaluation of the safety and efficacy of radioembolization in patients with unresectable colorectal liver metastases selected as candidates for (90)Y resin microspheres. J Gastrointest Oncol. 2015;6:134–42.
Wasan HS, Gibbs P, Sharma NK, et al. First-line selective internal radiotherapy plus chemotherapy versus chemotherapy alone in patients with liver metastases from colorectal cancer (FOLFIRE, SIRFLOX, and FOXFIRE-Global): a combined analysis of three multicentre, randomised, phase 3 trials. Lancet Oncol. 2017;18:1159–71.
Braat MNGJA, Samim M, van den Bosch MAAJ, et al. The role of 90Y-radioembolization in downstaging primary and secondary hepatic malignancies: a systematic review. Clin Transl Imaging. 2016;4:283–95.
Justinger C, Kouladouros K, Gartner D, et al. Liver resection after selective internal radiotherapy (SIRT): proof of concept, intial survival, and safety. J Surg Oncol. 2015;112:436–42.
Whitney R, Tatum C, Hahl M, et al. Safety of hepatic resection in metastatic disease to the liver after yttrium-90 therapy. J Surg Res. 2011;166:236–40.
Moir JA, Burns J, Barnes J, et al. Selective internal radiation therapy for liver malignancies. Br J Surg. 2015;102:1533–40.
Martin RC 2nd, Scoggins CR, Schreeder M, et al. Randomized controlled trial of irinotecan drug-eluting beads with simultaneous FOLFOX and bevacizumab for patients with unresectable colorectal liver-limited metastases. Cancer. 2015;121:3649–58.
Richardson AJ, Laurence JM, Lam VW. Transarterial chemoembolization with irinotecan beads in the treatment of colorectal liver metastases: as ystematic revie. J Vasc Interv Radiol. 2013;24:1209–17.
McPartlin A, Swaminath A, Wang R, et al. Long-term outcomes of phase 1 and 2 studies of SPBRT for hepatic colorectal metastases. Int J Radiat Oncol Biol Phys. 2017;99:388–95.
Mahadevan A, Blanck O, Lanciano R, et al. Stereotactic body radiotherapy (SBRT) for liver metastasis – clinical outcomes from the international multi-institutional RSSearch® patient registry. Radiat Oncol. 2018;13:26.
Rule W, Timmerman R, Tong L, et al. Phase I dose-escalation study of stereotactic body radiotherapy in patients with hepatic metastases. Ann Surg Oncol. 2011;18:1081–7.
Colbert LE, Cloyd JM, Koay EJ, et al. Proton beam radiation as salvage therapy for bilateral colorectal liver metastases not amenable to second-stage hepatectomy. Surgery. 2017;161:1543–8.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Anderson, B., Fields, R.C. (2020). Prognosis and Management of Recurrent Metastatic Colorectal Cancer. In: Correia, M., Choti, M., Rocha, F., Wakabayashi, G. (eds) Colorectal Cancer Liver Metastases. Springer, Cham. https://doi.org/10.1007/978-3-030-25486-5_42
Download citation
DOI: https://doi.org/10.1007/978-3-030-25486-5_42
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-25485-8
Online ISBN: 978-3-030-25486-5
eBook Packages: MedicineMedicine (R0)