Abstract
The pulmonary incidentaloma refers to a pulmonary lesion discovered on a radiographic study which is unrelated to the primary process. With the advent of high-resolution CT, pulmonary nodules as small as 1–2 mm are routinely diagnosed leading to a conundrum for clinicians as there are no formal guidelines, such as the Fleischner Society Guidelines, for those under 35 years of age. Furthermore, with the advent of the Image Gently campaign (Goske et al., Pediatr Radiol 41:461–66, 2011), more consideration is being given to avoiding unnecessary radiographic studies in the pediatric population. Since the prior edition of this chapter was published, this issue has garnered more attention culminating in the publication of recommendations from the Thoracic Imaging Committee of the Society for Pediatric Radiology (SPR) (Westra et al., Pediatr Radiol 45:628–33, 2015; Westra et al., Pediatr Radiol 45:634–39, 2015) regarding the management of the incidental pulmonary nodule.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Case Presentation
A 1.5 cm nodule (Fig. 22.1) was discovered at the base of the right lung in an otherwise healthy 17-year-old girl during an emergency room evaluation of abdominal pain. The radiologist recommended a follow-up chest CT be performed. This was completed 4 months later and was found to be normal. The abdominal pain resolved spontaneously while she was in the emergency room.
Definition
The pulmonary incidentaloma refers to a pulmonary lesion discovered on a radiographic study which is unrelated to the primary process. With the advent of high-resolution CT, pulmonary nodules as small as 1–2 mm are routinely diagnosed leading to a conundrum for clinicians as there are no formal guidelines, such as the Fleischner Society Guidelines, for those under 35 years of age. Furthermore, with the advent of the Image Gently campaign [1], more consideration is being given to avoiding unnecessary radiographic studies in the pediatric population. Since the prior edition of this chapter was published, this issue has garnered more attention culminating in the publication of recommendations from the Thoracic Imaging Committee of the Society for Pediatric Radiology (SPR) [2, 3] regarding the management of the incidental pulmonary nodule.
Where the Issue Stands Today
The incidence of pulmonary nodules in children is not known. One study of roughly 5000 pediatric patients undergoing abdominal CT scan diagnosed pulmonary nodules in only 1.2% [4]. Importantly, of the 1.2% of children with a nodule, only two were malignant, and both occurred in patients with a known malignancy and in nodules greater than, or equal to, 7 mm. Another study of 72 children undergoing trauma CT of the chest diagnosed nodules in 38% of patients [5]. These two studies very nearly represent all that is known about the incidence of the incidental pulmonary nodule in children.
When found, what do we know about the clinical importance of a nodule? Does it represent underlying malignancy? The available data to answer those questions is limited. A retrospective study of biopsied pulmonary nodules rendered a ratio of 1.4 benign to 1 primary malignancy of the lung to 11.6 metastatic lesions [6]. However, only nodules and masses which were excised were studied; therefore these patients likely had an increased risk profile necessitating the removal of the nodule or mass in the first place. This information cannot be extrapolated to the general population. This study suggests metastatic nodules or masses are relatively more common than primary lung cancer in the pediatric population. A retrospective single-institution study [7] of primary lung cancers concluded they are extremely rare (40 cases in 90 years) and almost always symptomatic at presentation.
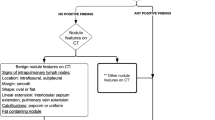
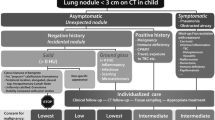
The prognostic implications of the imaging characteristics of pulmonary nodules are also limited. A review of the available data by the Thoracic Imaging Committee of the SPR [2] reveals linear or ground-glass opacifications are more likely to represent infection or inflammation rather than underlying malignancy. They conclude, however, not enough is known about the natural course of the solid pulmonary nodule to confidently state how size, shape, margin, or calcification speaks to the risk of underlying malignancy. There are some findings classically considered benign which can enter into a holistic evaluation of the patient when a nodule is diagnosed such as uniform calcification, features consistent with a pleural lymph node or macroscopic fat containing lesion representing a hamartoma. However, these imaging features should take on a secondary role relative to the clinical history of the patient. Although there are no clear numbers, it is suspected radiologists are over-recommending follow-up studies for pulmonary nodules which are almost certainly benign. Prior to making a recommendation, one should consider radiation is not benign and has demonstrable risks associated with it [8]. Furthermore there are no clear guidelines to follow. The 2017 update of the Fleischner Society guidelines [9] state for children and adults under 35 years of age, “these guidelines are not appropriate for such patients…management decisions should be made on a case-by-case basis.” Thus without clear guidelines, it is reasonable for the radiologist to be the driving force behind the initial management of these incidentalomas as they are likely among the few providers familiar (within the bounds of our current limited knowledge) with the likelihood serious disease lurks in the background. Given the medical literature is not definitive about the incidence, natural course, characteristics, or appropriate follow-up criteria for pulmonary incidentalomas, it is incumbent upon the radiologist to first ensure the right study is being ordered for the child and will answer the clinical question posed. Reasonable consideration should be given to alternatives that do not utilize ionizing radiation such as ultrasound or MRI. A 2009 study of pediatric chest CTs in a tertiary care center [10] noted the chest CT had a low yield of clinically relevant findings in patients with diffuse lung disease and in acquired focal lung disease. However, it was more useful in further evaluation of congenital lung disease. If a CT scan is clinically indicated, tissue not relevant to the clinical question should not be imaged. Finally, when a nodule is diagnosed, members of the Society for Pediatric Radiology (SPR) Thoracic Imaging Committee have supplied a flow chart for consideration (Fig. 22.2). They note that although “all authors are members of the Society for Pediatric Radiology (SPR) Thoracic Imaging Committee, the opinions expressed … are solely those of the authors and are not endorsed by the SPR” [3].
This flow chart was published by members of the Society for Pediatric Radiology (SPR) Thoracic Imaging Committee as a “conceptual framework for the diagnostic management of a lung nodule measuring up to 3 cm in diameter on CT in a child” [3]. It is provided here with permission of the authors who note that it is provided as the authors’ personal opinion and is not endorsed by the SPR
The primary branch point is based on the history of the patient. If there is any history of respiratory symptomatology, malignancy, immunocompromise, or risk factors for infectious or inflammatory etiologies, care and imaging follow-up should be individualized. If the nodule is truly incidental, the patient has none of the above risk factors, and if the nodule contains classically benign features, the members of the Society for Pediatric Radiology (SPR) Thoracic Imaging Committee recommend no further work-up [3]. If the nodule does not contain classically benign imaging features, the patient is placed in the individualized care category, and a discussion with the patient’s provider and the patient’s family should ensue.
Ideally this discussion will discuss the paucity of data regarding incidental pulmonary nodules, the lack of an evidence-based guideline, the real risk associated with repeat imaging or tissue sampling, and the risk factors the patient carries for malignancy (if any). Only after this discussion should a recommendation for follow-up evaluation be rendered.
Conclusion
The pulmonary incidentaloma remains a quandary for clinicians. There is a marked lack of data regarding their natural course yet a heightened risk of over-radiating or over-sampling children for a lesion which, in the correct patient population, is overwhelmingly likely to be benign. The incidentaloma provides an ideal opportunity for the radiologist to practice the ALARA (as low as reasonably achievable) principle following a discussion with the stakeholders in the patient’s care and ultimately utilize the consultant function of a Radiologist or Pulmonologist for the benefit of the patient. Chest CT should not be used merely to avoid medicolegal risk because of the potential harm to the patient. Medicine is both art and science. For now, the evaluation of the pulmonary incidentaloma is more art than science.
References
Goske MJ, Applegate KE, Bulas D, et al. Image gently: progress and challenges in CT education and advocacy. Pediatr Radiol. 2011;41:461–6.
Westra SJ, Brody AS, Mahani MG, et al. The incidental pulmonary nodule in a child. Part 1: recommendations from the SPR Thoracic Imaging Committee regarding characterization, significance and follow-up. Pediatr Radiol. 2015;45:628–33.
Westra SJ, Thacker PG, Podberesky DJ, et al. Part 2: commentary and suggestions for clinical management, risk communication and prevention. Pediatr Radiol. 2015;45:634–9.
Breen M, Zurakowski D, Lee EY. Clinical significance of pulmonary nodules detected on abdominal CT in pediatric patients. Pediatr Radiol. 2015;45:1753–60.
Samim A, Littooij AS, van den Heuvel-Eibrink MM, et al. Frequency and characteristics of pulmonary nodules in children at computed tomography. Pediatr Radiol. 2017;47:1751. [Epub ahead of print].
Dishop MK, Kuruvilla S. Primary and metastatic lung tumors in the pediatric population: a review and 25-year experience at a large children’s hospital. Arch Pathol Lab Med. 2008;132:1079–103.
Yu DC, Grabowski MJ, Kozakewich HP, et al. Primary lung tumors in children and adolescents: a 90-year experience. J Pediatr Surg. 2010;45:1090–5.
Brenner D, Elliston C, Hall E, Berdon W. Estimated risks of radiation-induced fatal cancer from pediatric CT. Am J Roentgenol. 2001;176:289–6.
MacMahon H, Naidich DP, Goo JM, et al. Guidelines for management of incidental pulmonary nodules detected on CT images: from the Fleischner Society 2017. Radiology. 2017;284:228–43.
Schneebaum N, et al. Use and yield of chest computed tomography in the diagnostic evaluation of pediatric lung disease. Pediatrics. 2009;124:472–9.
Acknowledgment
Dedicated to Robert Zwerdling, MD
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Carraway, T., Coates, A.C., Grimes, C.K. (2020). Pulmonary Incidentaloma. In: Cleveland, R., Lee, E. (eds) Imaging in Pediatric Pulmonology. Springer, Cham. https://doi.org/10.1007/978-3-030-23979-4_22
Download citation
DOI: https://doi.org/10.1007/978-3-030-23979-4_22
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-23978-7
Online ISBN: 978-3-030-23979-4
eBook Packages: MedicineMedicine (R0)