Abstract
Kidney aging is under the influence of different factors including genetic factors, gender, ethnicity, and comorbidities, and normal aging process has an important role in daily clinical practice. In short, the physiological process of kidney aging includes reduced weight and preserved kidney volume, increased number of sclerotic glomeruli, increased size of remaining glomeruli, loss of afferent and peripheral arterioles and redistribution of blood into the medulla, decreased glomerular filtration, increased permeability of the glomerular basal membrane, tubular atrophy and interstitial fibrosis, reduced concentration and dilution ability of the kidney, and increased kidney sensitivity to toxic ischemic damage. The above-noted changes in the kidneys need to be known for establishing diagnosis of potential kidney disease/failure by adequate measurements of glomerular filtration, in order to adapt the therapy and to prevent numerous metabolic disturbances for which the kidney is responsible. Although age-related alterations are different to those induced by diseases, sometimes the two processes cannot be easily distinguished.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Kidney aging
- Sclerotic glomeruli
- GFR decline
- eGFR measurement
- Tubular atrophy
- Interstitial fibrosis
- Concentration ability
- Dilution ability
A complex process involves all organs along the time, which is reflected in structural and functional changes that delineate the process of “organ aging.” The basis of this process are numerous, known and less known mechanisms that vary not only by age but also by genetic factors, gender, ethnicity, and comorbidities. Although the aging process is controlled by signaling pathways very similar to disease processes, age-related alterations are different to those induced by diseases. Sometimes, these two processes cannot be easily distinguished, and this diagnostic problem is much more common in older than in younger patients.
Interest in the aging kidney has gained significance from the time when the limit for the diagnosis of chronic kidney disease (CKD) was established. Namely, the threshold for defining CKD based on estimated glomerular filtration rate (eGFR) was value less than 60 ml/min/1.73 m2. Accepted limit led to the diagnosis of a large number of elderly with CKD. Although this limit is not necessarily true for a group of elderly, a reduced kidney function along with a normal aging process has an important role in daily clinical practice to drug dosing, kidney donor selection, and the definition of the risk of acute kidney damage due to a reduced renal reserve. Therefore, most of the papers were related to renal function and determination of glomerular filtration rate (GFR) in the elderly.
Changes in the kidneys during the aging process can be detected by the imaging procedure (IP) [1,2,3,4,5], kidney biopsy [6,7,8], and by functional testing [9, 10] (Table 1.1).
The first molecular biology of aging at the cellular level was proposed by Dr. Harman who suggested oxidative stress and free radicals as a major cause of aging [9]. Additionally, accumulation of pro-fibrogenic mediators, mitochondrial damage, and loss of telomeres correlate with the process of kidney aging [11]. The process of kidney aging involves Klotho gene which is expressed in the distal convoluted tubules. Downregulation of Klotho gene increases the susceptibility to oxidative stress via stimulation of IGF-1 pathway [12]. Increased oxidative stress acts at the three levels [12, 13]:
-
1.
Activate angiotensin II pathway and transcription of transforming growth factor B1 (TGF-B1),
-
2.
Leads to shortening of telomeres via inhibition of telomerase.
-
3.
Activate rapamycin target (TOR) leading to accumulation of malignant mitochondria in cells.
Structural Changes
The first findings of changes in the kidney structure as part of the aging process are based on postmortem studies. It has been established that aging increases the number of sclerotic glomeruli and the frequency of changes in tubules and blood vessels [14]. Precious data was obtained in the era of transplantation by analysis of kidney from healthy donors from six decades. The advantage of these analyses over autopsy was that structural changes in the kidneys obtained by pre-implantation biopsy could be compared with a clinical finding, results in urine and blood (including functional tests) and finding on the computed tomography (CT) angiogram. For a better understanding, changes in the kidneys during aging can be classified into micro- and macroanatomical changes.
Microanatomical Changes
These changes involve three basic components of the kidney: glomeruli, tubules, and vasculature. Changes in glomeruli during the aging process can be characterized as senile glomerulosclerosis with the glomeruli being replaced by fibrous tissue. Simultaneously with the increase in the number of sclerotic glomeruli, the remaining functional glomeruli can be increased. With time, they show progressive folding and thickening of glomerular basal membrane, increasing the volume of the mesangial matrix due to the imbalance between formation and decomposition and finally glomerular tuft collapse: globally sclerotic glomeruli (GSG) [15, 16]. Glomerulosclerosis is a non-specific process, can be due to several factors including ischemia and changes in the light microscope reminiscent of ischemic changes. Prevalence of GSG begins about 30 years of life (25%) and reaches as much as 82% in the eighth decade of life [17]. The number of glomeruli per area of cortex (glomerular density) inversely correlates with glomerular size. Glomerular density is lower in biopsies where less than 10% of glomeruli are sclerotic suggesting that the nephron hypertrophy with age can be detected in regions without significant nephrosclerosis. If the number of sclerotic glomeruli is more than 10%, the density increases due to a large number of small, sclerotic glomeruli and atrophic tubules in the region of significant nephrosclerosis. The described changes lead to discrepancies between weight and size of the kidney in old age. Although the renal weight decreases from 400 g (in the fourth decade) to 300 g (in the ninth decade), the volume of the kidney determined by computerized tomography is not necessarily changed.
Mesangial cells and endothelial cells have been shown to increase in number until the age of 50 years and number progressively decline thereafter. The ratio of the number of mesangial cells to enlarged glomerular volume is therefore initially maintained. Podocytes do not increase in number, and there are some reports that their number decreases over time along with the decreased capacity for their regeneration and repair. Also, podocytes can undergo hypertrophy together with glomerulus hypertrophy. Such changes affect kidney glomerular filtration rate and albumin permeability [18, 19].
Tubulointerstitial changes during the aging process include infarction, scarring, and fibrosis. Fibrosis is an active process that begins with interstitial inflammation and activation of fibroblasts as well as increased expression of adhesive proteins osteopontin and intercellular adhesion molecules 1. Additionally, accumulated collagen contributes to tubulointerstitial changes. Experimental model showed increased collagen deposits and increased expression of genes for fibronectin and TGF-B [20]. In distal tubules, the number of diverticula increases, which can eventually be transformed into simple cysts. Namely, it is well known that the number of simple cysts increases with the aging process [21]. Changes in tubular morphology have also been observed including a decrease in tubule volume and length and increased tubular atrophy [22]. The previously described changes in glomeruli, together with tubulointerstitial changes and changes in blood vessels, constitute the basis of nephrosclerosis. Its prevalence among living donors is 2.7% in the young and up to 73% in the oldest living donors [17].
Blood vessels of the kidney are most usually atheromatous and, if present, can lead to renovascular hypertension, ischemic nephropathy, and/or intrarenal atheroembolic events with consequent chronic renal failure [23]. Pre-arteriolar subendothelial accumulation of hyaline and collagen deposits lead to intimal thickening which can compromise blood vessel lumen and lead to sclerosis of the glomeruli, most often in the area of the kidney cortex. This so-called vascular aging of the kidneys results in the formation of aglomerular circulation in the juxtamedullary glomeruli, which is the communication between the afferent and the efferent arterioles and the redistribution of blood into the medulla [24]. At the same time, intima of small arteries is thickened due to the proliferation of elastic tissue and atrophy of the media. The arcuate arteries become more angulated, and the interlobular arteries become more tortuous and spiral [25, 26]. Data support that there are changes in vascular responsiveness and autoregulation. While vasoconstrictive response to angiotensin was not altered with aging, vasodilatatory response to acetylcholine or to acute sodium load was impaired with aging [27].
Macroanatomical Changes
These changes include modifications in kidney volume, presence of cysts and tumors, often benign. There are many controversies about the kidney volume in the elderly and they come from different measurement methods (CT scan, ultrasound, histology). Also, kidney volume is an unspecific finding since it does not reflect true changes in kidney disease. Earlier data obtained from ultrasound examinations of over 600 volunteers showed that the volume of the kidney correlates with the younger age, weight, heights, and total body surface area [28]. Subsequent data obtained by an examination of individuals without kidney disease showed that the thickness of the kidney parenchyma decreased by 10% with each decade of age [29], data confirmed by the more recent study [30]. More precious data are obtained from the potential kidney donors of a wide range of age. It has been shown that the volume of the kidney is stable up to 50 years of age when it begins to decline [5]. Namely, for up to 50 years, the decrease in cortical volume is compensated by an increase in the volume of the medulla which maintains the dimension of the kidney. After 50 years, the volume of the medulla decreases in women and remains stable in men. Reduction of the cortical volume is the result of an increasing number of globally sclerotic glomeruli (GSG) with atrophy of corresponding tubules (nephrosclerosis). Hypertrophy of non-sclerotic glomeruli and tubules helps to maintain the volume of kidney parenchyma. However, after 50 years, this hypertrophy cannot compensate for the loss of volume due to nephrosclerosis [5, 31].
It has already been noted that changes in the tubules in the form of diverticula can predispose to renal cysts that become more frequent and larger with older age [2]. These cortical and medullar cysts correlate with larger body size, male gender, hypertension, and proteinuria. Parapelvic cysts and angiomyolipomas are also more frequent in older age. Since parapelvic cysts are of lymphatic origin, they are not associated with hypertension and albuminuria [32].
Other structural changes in kidney related to aging include cortical scars, parenchymal calcifications, fibromuscular dysplasia, and kidney artery atherosclerosis with the prevalence of 25% for patients between 65 and 75 years as compared with 0.4% for those younger than 30 years [3].
Functional Changes
Glomerular Functional Changes
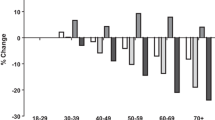
Since the early 1950s, it has been known that the urea clearance and GFR decrease with aging process [33, 34]. At present, it is not possible to establish single-nephron GFR, and therefore, there can be considerable heterogeneity of single-nephron GFR between subjects with the same GFR. The GFR remains constant until the fourth decade when it is reduced by an average of 46% from that in young people until the age of 90 [34]. It is worth mentioning that there is reduction in mean creatinine clearance despite no difference in serum creatinine and this can be explained by the so-called senile sarcopenia and by reduced protein intake. At the same time, functional reserve of the kidney (increase of basal GFR by 20% after amino acid load) is decreased in healthy elderly persons and reach its maximum of 50% for 60 min which is less and slower than in younger persons (80% for period of 30 min) [35, 36]. The decline in GFR is associated with a decrease in the effective renal plasma flow (ERPF), from 600 ml/min/1.73 m2 at youth to 300 ml/min/1.73 m2 in 80 years old healthy persons. This is followed by an increase in the filtration fraction as the EFRF was disproportionately lower than the GFR [37].
The GFR decline during the aging process can be calculated by Keller’s equation that shows eGFR in aged with no signs of kidney weakness [38]:
Additionally, BIS equation (based on serum creatinine or cystatin C) is currently considered the reliable equations for estimating GFR in the elderly [39, 40]:
The causes of decreased glomerular filtration were debated, and it was postulated that reduced GFR was probably associated with existing nephrosclerosis in old age. However, in multivariable models (adjusting for age and gender), biopsy-revealed nephrosclerosis was associated with urinary albumin excretion, nocturnal blood pressure and hypertension but not with GFR [17]. In living donor biopsy series, GFR declined with age independently of nephrosclerosis raising the question of the other pathological changes in the kidney and extrarenal factors contributing to the decline in GFR [41]. The opinion that cortical atrophy and GFR fall under the same mechanism(s) is not always justified given that the GFR decrease is possible regardless of the reduction in cortical volume [5].
Finally, about three decades ago, Lindeman et al. described that about one-third of 254 healthy individuals had an increase in creatinine clearance with aging. Apart from possible imprecision of calculation of the slope of GFR over time, it is possible that transient comorbidities that are associated with aging such as obesity, diabetes, and subclinical cardiovascular disease may lead to transient hyperfiltration and preserved or even increased GFR [42].
Tubulointerstitial Functional Changes
Tubular-interstitial changes related to aging include changes in water, sodium, potassium, urea, creatinine, and divalent cation handling. These are usually interpreted as three “nephrogeriatric giants,” which means frequent structural and physiological renal changes in the elderly, which influence the course of the disease and the therapeutic strategies in the elderly [23]:
-
Tubular dysfunction
-
Medullary hypotonicity
-
Tubular frailty
Tubular dysfunction includes changes in water and electrolyte handling which, unrecognized, can cause serious problems in the elderly, particularly in special clinical conditions. Compared to younger persons, reabsorption of sodium in proximal tubules is not different in elderly but it is reduced in the thick ascending loop of Henle (Table 1.2). Therefore, the amount of urinary loss of sodium is increased and the free water clearance is reduced. These changes lead to reduced osmolality of the interstitium and reduced ability of the medulla to concentrate urine. Sodium urinary loss is also potentiated by reduced plasma renin and aldosterone levels. According to some reports, serum and urinary natriuretic peptides are elevated which in turn may increase natriuresis [43]. Elderly individuals also seem to have more sodium excretion at the night suggesting an impaired circadian variation. Knowing about these specificities in sodium handling is very important to avoid hyponatremia and hypovolemia and to adjust fluid intake and therapy in the aged.
There are several reasons for the change in potassium handling in the aged. Apart from reduced muscle mass and low potassium diet [44], the elderly have significantly lower renal excretion of potassium compared with the young. Impaired potassium secretion is directly associated with disorders in sodium reabsorption and tubular atrophy and interstitial scarring. Additionally, hyporeninemic hypoaldosteronism and suppression of water and sodium delivery into the distal nephron are associated with potassium secretion disorders in the aging kidney [45]. An increase in H+K+ATPasa pump at collecting tubules leads to increased potassium reabsorption [46].
Magnesium excretion is increased in the scenario of volume overload lowering its serum level. Hypomagnesemia in the elderly may also be explained by decreased intake and poor intestinal absorption that lead to hypomagnesemia. Since in healthy old people sodium reabsorption is reduced in the thick ascending loop of Henle and magnesium reabsorption occurs chiefly at this tubular segment, it has been hypothesized that a urinary magnesium loss could explain this increased Mg excretion [47]. There is no data on altered calcium handling in the elderly with normal renal function, adequate diet, and sunlight exposure.
Experimental data revealed that distal urea reabsorption is decreased in old rats due to the reduction of urea channels (UT1) in the collecting tubules. Urea excretion contributes to osmotic diuresis and together with medullary hypotonicity makes the elderly prone to dehydration [48]. With regard to creatinine, there are data on decreased tubular secretion and even tubular reabsorption in dehydrated elderly [49].
During the aging process, no physiological changes were observed in the level of serum vitamin D, parathormone, or erythropoietin. Therefore, hyperphosphatemia, hyper- and hypocalcemia, and anemia cannot be explained by the process of aging, and one should look for other possible causes.
Elderly people are capable of secreting an acid load and maintain normal serum bicarbonate level and urine pH on a 70 g protein diet [50]. However, following an acid load, senescent kidneys do not increase acid excretion and lower urinary pH to the degree that younger kidneys do. Also, the maximal value of ammonia and titratable acid excretion were reached in 6–8 hours as compared to 4 hours in the young. Therefore, elderly have difficulties to cope acidosis particularly in acute setting [47].
Medullary Hypotonicity
Elderly individuals are not capable to dilute or concentrate urine as well as younger ones and they are more prone to water disorders and volume depletion. The ability to generate free water depends on several factors including sufficient GFR, functional intact distal diluting site, and suppression of antidiuretic hormone to avoid water reabsorption in the collecting duct. According to experimental data from aged rats, there is downregulation of V2 receptors in renal tubules and also lower abundance of aquaporins 2 and 3 [51]. Knowing the changes in kidney function with aging (defect in sodium reabsorption, reduced distal urea reabsorption), the maximal urinary concentration capacity decreases by 30 mOsm/kg per decade after the age of 30. Decreased effect of antidiuretic hormone and water reabsorption capability may cause severe dehydration in elderly who have increased threshold for the thirst [52].
At the same time, there is a decrease in capacity to dilute urine in the aged; maximum free water clearance is reduced from 12.2 to 5.9 ml/min, and minimum urine concentration is 90 mOsm/kg in the elderly as compared with 50 mOsm/kg in the young [43].
Tubular Frailty
Renal tubular cells are more vulnerable to ischemic and toxic injury and also they recover more slowly from acute tubular necrosis [23]. Consequently, aged are predisposed for developing acute kidney injury and chronic kidney disease [53].
Age-Related Changes and Definition of Chronic Kidney Disease
According to the Kidney Disease Improving Global Outcomes (KDIGO) guidelines [54], CKD is present if the patient has a GFR <60 ml/min/1.73 m2 that persists for 3 months even in the absence of the finding of kidney damage (increased albuminuria). The most commonly used formulas for the calculation of glomerular filtration rate are based on serum creatinine: The Modification of Diet in Renal Disease (MDRD) study equation and Chronic Kidney Disease Epidemiology (CKD-EPI) equation. However, both formulas underestimate measured GFR in healthy adults since they have higher muscle mass as compared to CKD patients.
Namely, in healthy patients with an eGFR between 45 and 59 ml/min/1.73 m2 CKD-EPI equation underestimate GFR by 16% and the MDRD study equation by 25% [55]. Age-related decline in GFR and underestimation of GFR in healthy older patients are the reasons for overdiagnosis of CKD in the elderly. Therefore, KDIGO 2012 guidelines suggest eGFR measurement based on serum cystatin C, particularly in those with eGFR 45–59 ml/min/1.73 m2 (according to creatinine-based formulas) and without albuminuria. Still, precaution is needed in case of obesity, inflammation, and atherosclerosis [56].
The importance of determining glomerular filtration in the old ones is reflected in the prediction of the outcome, i.e., the prognosis of the elderly. It has been confirmed that an increase in cardiovascular mortality in individuals over 65 years starts when eGFR is less than 45 ml/min/1.73 m2 [57]. By analyzing 46 cohorts with more than 2 million individuals, CKD Prognosis Consortium concluded that eGFR less than 60 ml/min/1.73 m2 is a threshold for CKD in all age groups [58]. However, elderly individuals with eGFR of 45–59 ml/min/1.73 m2 rather have a reduced kidney reserve than CKD.
Another contribution to more adequate presumptive diagnosis of CKD in the elderly is the HUGE formula based on hematocrit, urea, and gender [59]:
Values less than zero exclude CKD while values equal or higher than zero point to CKD. Although this equation has sensitivity of 92.8%, specificity of 93.2%, and positive predictive value of 95.8%, it is screening method that has to be confirmed by appropriate medical evaluation. However, a prospective study recently conducted in the population of Buenos Aires (Argentina) documented a lower performance of the HUGE formula for detecting CKD, even in the elderly population (sensitivity, 40.0%), also verifying that the performance of the HUGE formula improved when combined with the calculated GFR (MDRD-4) and urinary sediment (sensitivity, 95.8%) [60].
Conclusion
Knowledge about which are the renal aging changes is crucial to differentiate renal aging from chronic kidney disease and understand the trend to the internal milieu alterations and kidney disorders in the elderly.
References
Al-Said J, Brumback MA, Moghazi S, Baugarten DA, O’Neill WC. Reduced renal function in patients with simple renal cysts. Kidney Int. 2004;65(6):2303–8.
Rule AD, Sasiwimonphan K, Lieske JC, Keddis MT, Torres VE, Vrtiska TJ. Characteristics of renal cystic and solid lesions based on contrast-enhanced computed tomography of potential kidney donors. Am J Kidney Dis. 2012;59(6):611–8.
Lorenz EC, Vrtiska TJ, Lieske JC, et al. Prevalence of renal artery and kidney abnormalities by computed tomography among healthy adults. Clin J Am Soc Nephrol. 2010;5(3):431–8.
Duan X, Rule AD, Elsherbiny H, et al. Automated assessment of renal cortical surface roughness from computerized tomography images and its association with age. Acad Radiol. 2014;21(11):1441–5.
Wang X, Vrtiska TJ, Avula RT, et al. Age, kidney function, and risk factor associate differently with cortical and medullary volumes of the kidney. Kidney Int. 2014;85(3):677–85.
Kubo M, Kiyohara Y, Kato I, et al. Risk factors for renal glomerular and vascular changes in an autopsy –based population survey: the Hisayama study. Kidney Int. 2003;63(4):1508–15.
Baert L, Steg A. Is the diverticulum of the distal and collecting tubules a preliminary stage of the simple cist in the adult? J Urol. 1977;118(5):707–10.
Elsherbiny HE, Alexander MP, Kremers WK, et al. Nephron hypertrophy and glomerulosclerosis and their association with kidney function and risk factors among living kidney donors. Clin J Am Soc Nephrol. 2014;9(11):1892–902.
Harman D. Aging: a theory based on free radical and radiation chemistry. J Gerontol. 1956;11(3):298–300.
Dai DF, Chiao YA, Marcinek DJ, Szeto HH, Rabinovitch PS. Mitochondrial oxidative stress in aging and health span. Longev Healthspan. 2014;3:6.
Perico N, Remuzzi G, Benigni A. Aging and the kidney. Curr Opin Nephrol Hypertens. 2011;20:312–27.
Yang H, Fogo A. Cell senescence in the aging kidney. J Am Soc Nephrol. 2010;21:1436–9.
Zhou X, Saxena R, Liu Z, et al. Renal senescence in 2008: progress and challenges. Int Urol Nephrol. 2008;40:823–39.
Darmady EM, Offer J, Woodhouse MA. The parameters of the ageing kidney. J Pathol. 1973;109(3):195–207.
Martin JE, Sheaff MT. Renal ageing. J Pathol. 2007;211(2):198–205.
Hoy WE, Douglas-Denton RN, Highson MD, Cass A, Johnson K, Bertram JF. A stereological study of glomerular number and volume: preliminary findings in a multiracial study of kidneys at autopsy. Kidney Int Suppl. 2003;63(83):S31–7.
Rule AD, Amer H, Cornell LD, et al. The association between age and nephrosclerosis on renal biopsy among healthy adults. Ann Intern Med. 2010;152(9):561–7.
Huber TB, Edelstein CL, Hartleben B, et al. Emerging role of autophagy in kidney function, diseases and aging. Autophagy. 2012;8(7):1009–31.
Wiggins JE. Aging in the glomerulus. J Gerontol A Biol Sci Med Sci. 2012;67(12):1358–64.
Gagliano N, Arioso B, Santanbrogio B, et al. Age-dependent expression of fibrosis-related genes and collagen deposition in rat kidney cortex. J Gerontol A Biol Sci Med Sci. 2000;55(8):365–72.
Lauks SP Jr, McClachlan MS. Aging and simple cysts of the kidney. Br J Radiol. 1981;54(637):12–4.
Lindeman RD, Goldman R. Anatomic and physiologic age changes in the kidney. Exp Gerontol. 1986;21(4–5):379–406.
Musso CG. Geriatric nephrology and the “nephrogeriatric giants”. Int Urol Nephrol. 2002;34:255–6.
Takazakura E, Sawabu N, Handa A, et al. Intrarenal vascular changes with age and disease. Kidney Int. 1972;2:224–30.
Silva FG. The ageing kidney: a review – part I. Int Urol Nephrol. 2005;37:185–205.
Silva FG. The ageing kidney: a review – part II. Int Urol Nephrol. 2005;37:419–32.
Hollenberg NK, Adams DF, Solomon HS, et al. Senescence and the renal vasculature in normal man. Circ Res. 1974;34:309–16.
Emamiam SA, Nielsen MB, Pedersen JF, Ytte L. Kidney dimensions at sonography: correlation with age, sex, and habitus in 665 adult volunteers. AJR Am J Roenthenol. 1993;160(1):83–6.
Gourtsoyiannis N, Prassopoulos P, Cavouras D, Pantelidis N. The thickness of the renal parenchyma decreases with age: a CT study of 360 patients. AJR Am J Roentgenol. 1990;155(3):541–4.
Glodny B, Unterholzner V, Taferner B, et al. Normal kidney size and its influencing factors – a 64-slice MDCT study of 1040 asymptomatic patients. BMC Urol. 2009;9:19.
McLachlan M, Wasserman P. Changes in sizes and distensibility of the aging kidney. Br J Radiol. 1981;54(642):488–91.
Schwarz A, Lenz T, Klaen R, Offermann G, Fiedler U, Nussberger J. Hygroma renale: pararenal lymphatic cysts associated with renin-dependent hypertension (page kidney). Case report on bilateral cysts and successful therapy by marsupialization. J Urol. 1993;150(3):953–7.
Smith HW. The kidney: the structure and function in health and disease. New York: Oxford University Press; 1951.
Davies DF, Shock NW. Age changes in glomerular filtration rate, effective renal plasma flow, and tubular excretory capacity in adult males. J Clin Invest. 1950;29(5):496–507.
Musso CG. Renal reserve test: its methodology and significance. Saudi J Kidney Dis Transpl. 2011;22(5):990–3.
Musso CG, Reynaldi J, Martinez B, Pierángelo A, Vilas M, Algranati L. Renal reserve in the oldest old. Int Urol Nephrol. 2011;43(1):253–6.
Alvarez Gregori J, Musso C, Macias Núñez JF. Renal ageing. In: Sastre J, Pamolona R, Ramón J, editors. Medical biogerontology. Madrid: Ergon; 2009. p. 111–23.
Keller F. Kidney function and age. Nephrol Dial Transplant. 1987;2(5):382.
Swedish Council on Health Technology Assessment. Methods to estimate and measure renal function (glomerular filtration rate): a systematic review, SBU Yellow Report No. 214. Stockholm: Swedish Council on Health Technology Assessment (SBU); 2011.
Musso CG, Álvarez-Gregori J, Jauregui J, MacíasNúñez JF. Glomerular filtration rate equations: a comprehensive review. Int Urol Nephrol. 2016;48(7):1105–10.
Rule AD, Cornell LD, Poggio ED. Senile nephrosclerosis-does it explain the decline in glomerular filtration rate with aging? Nephron Physiol. 2011;119(Suppl):6–11.
Eriksen BO, Lochen ML, Arntzen KA, et al. Subclinical cardiovascular disease is associated with high glomerular filtration rate in the nondiabetic general population. Kidney Int. 2014;86(1):146–53.
Musso CG, Macías-Núñez JF. Dysfunction of the thick loop of Henle and senescence: from molecular biology to clinical geriatrics. Int Urol Nephrol. 2011;43(1):249–52.
Lye M. Distribution of body potassium in healthy elderly subjects. Gerontologie. 1981;27:286–92.
Phelps KR, Lieberman RL, Oh MS, et al. Pathophysiology of the syndrome of hyporeninemic hypoaldosteronism. Metabolism. 1980;29:186–99.
Musso CG, Miguel RD, Algranati L, Farias Edos R. Renal potassium excretion: comparison between chronic renal disease patients and old people. Int Urol Nephrol. 2005;37(1):167–70.
Musso CG, Juarez R, Vilas M, Navarro M, Rivera H, Jauregui R. Renal calcium, phosphorus, magnesium and uric acid handling: comparison between stage III chronic kidney disease patients and healthy oldest old. Int Urol Nephrol. 2012;44(5):1559–62.
Musso CG, Alvarez Gregori J, Jauregui JR, Macías Núñez JF. Creatinine, urea, uric acid, water and electrolytes renal handling in the healthy oldest old. World J Nephrol. 2012;1(5):123–6.
Musso CG, Michelángelo H, Vilas M, Reynaldi J, Martinez B, Algranati L, Macías Núñez JF. Creatinine reabsorption by the aged kidney. Int Urol Nephrol. 2009;41(3):727–31.
Wagner EA, Falciglia GA, Amlal H, et al. Short-term exposure to high-protein diet differentially affect glomerular filtration rate but not acid-base balance in older compared to younger adults. J Am Diet Assoc. 2007;107:1404–8.
Preisser L, Teillet L, Aliotti S, et al. Downregulation of aquaporin-2 and -3 in aging kidney is independent of V(2) vasopressin receptor. Am J Phyiol Renal Physiol. 2000;279:F144–52.
Musso CG, Macías Núñez JF. Renal handling of water and electrolytes in the old and old-old healthy aged. In: Núñez M, Cameron S, Oreopoulos D, editors. Renal ageing: health and disease. New York: Springer; 2008. p. 141–54.
Musso CG, Liakopoulos V, Ioannidis I, Eleftheriadis T, Stefanidis I. Acute renal failure in the elderly: particular characteristics. Int Urol Nephrol. 2006;38(3–4):787–93.
Stevens PE, Levin A. Evaluation and management of chronic kidney disease: synopsis of the kidney disease improving global outcomes 2012 clinical practise guideline. Ann Intern Med. 2013;158(11):825–30.
Murata K, Bauman NA, Saenger AK, Larson TS, Rule AD, Lieske JC. Relative performance of the MDRD and CKD-EPI equations for estimating glomerular filtration rate among patients with varied clinical presentations. Clin J Am Soc Nephrol. 2011;6(8):1863–972.
Rule AD, Glassock RJ. GFR estimating equations: getting closer to the truth? Clin J Am Soc Nephrol. 2013;8(8):1414–20.
Stengel B, Metzger M, Froissart M, et al. Epidemiology and prognostic significance of chronic kidney disease in the elderly –the Three-City prospective cohort study. Nephrol Dial Transplant. 2011;26(10):3286–95.
Hallan SI, Matsushita K, Sang Y, et al. Age and association of kidney measures with mortality and end-stage renal disease. JAMA. 2012;308(22):2349–60.
Robles NR, Felix FJ, Lozano L, Miranda I, Fernandez-Berges D, Macías JF. The H.U.G.E. formula (Hematocrit, Urea, Sex) for screening chronic kidney disease (CKD) in an age-stratified general population. J Nutr Health Aging. 2015;19(6):688–92.
Musso CG, Maytin S, Conti P, Terrasa S, Primerano A, Reynaga A, Vilas M, Jauregui J. HUGE equation accuracy for screening chronic kidney disease: a prospective study. J Aging Res Clin Pract. 2017;6:158–62.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Dimkovic, N. (2019). Structural and Functional Renal Changes Secondary to Aging. In: Musso, C., Jauregui, J., Macías-Núñez, J., Covic, A. (eds) Clinical Nephrogeriatrics. Springer, Cham. https://doi.org/10.1007/978-3-030-18711-8_1
Download citation
DOI: https://doi.org/10.1007/978-3-030-18711-8_1
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-18710-1
Online ISBN: 978-3-030-18711-8
eBook Packages: MedicineMedicine (R0)