Abstract
Vestibular schwannomas (VS) mainly arise from either the superior (SVN) or the inferior vestibular nerve (IVN). Preoperative vestibular testing in patients affected by VS can be useful to predict which one of the vestibular nerves the tumor arises from. The relevance of identifying the nerve of origin lies in its prognostic factor for hearing preservation after surgery, with tumors arising from the (SVN) having a much higher hearing preservation rate. Diverse studies in the literature have tested the correlation between abnormal vestibular testing results and the nerve of origin of VSs; the techniques experimented in such context are posturography, vestibular evoked myogenic potentials (VEMPs), caloric test (always in combination with VEMPs), and video head impulse test (vHIT). vHIT has yielded promising results, with a positive predictive value ranging from 89.5 to 100%, so that the pattern of semicircular canal dysfunction on vHIT has been proposed to have a localizing value to identify the nerve of origin in VSs.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Vestibular schwannoma/vestibular nerve
- Vestibular schwannoma/vestibular testing
- Vestibular schwannoma/posturography
- Vestibular schwannoma/VEMPs
- Vestibular schwannoma/head impulse test
Vestibular schwannomas (VS) mainly arise from either the superior vestibular nerve (SVN) or inferior vestibular nerve (IVN). The SVN innervates the lateral semicircular canal (LSC) and anterior semicircular canal (ASC), utricle, and part of the saccule. On the other hand, the IVN innervates the posterior semicircular canal (PSC) as well as most of the saccule. On this basis, preoperative vestibular testing in patients affected by VS can be useful to predict which one of the vestibular nerves the tumor arises from. The relevance of identifying the nerve of origin in VS lies in its prognostic factor for hearing preservation after surgery [1,2,3,4,5], with tumors arising from the SVN having a 61–80% of hearing preservation rate, compared to 16–43% for an IVN origin [1, 4, 5] in cases when hearing preservation is attempted.
Diverse studies in the literature have tested the correlation between asymmetric or pathological vestibular testing results and the nerve of origin of VSs, with subsequent controversial conclusions. The techniques that have been experimented in such context are posturography, vestibular evoked myogenic potentials (VEMPs), caloric test (always in combination with VEMPs), and video head impulse test (vHIT).
1 Posturography
Computerized dynamic platform posturography (CDPP) is a sensory organization test that consists of six conditions (i.e., the steps of the examination) of increasing difficulty in separate 20 s trials; a balance score ranging from 0% (worst) to 100% (best) is assigned for each condition. Conditions 5 and 6 assess the vestibular component of the balance system separately by eliminating, through sway-referencing, information from vision and somatosensation, respectively. During condition 5, the patient stands on the mobile, sway-referenced platform with their eyes closed. During condition 6, the patient stands with their eyes open on a mobile, sway-referenced platform with a sway-referenced visual surround. Condition 5 score (C5S) and condition 6 score (C6S) are the respective arithmetic means (in %) of the scores recorded during three repetitions of each condition. Results below the fifth percentiles of age-matched normal individuals are rated as pathologic [1].
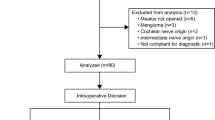
Gouveris et al. [6] performed a retrospective study to test whether CDPP findings could preoperatively predict the nerve of origin of VSs. Seventy-five consecutive VS patients were evaluated; C5S, C6S, vestibular ratio (VER), and mean overall balance score (MOBS) were calculated for each patient. The nerve of VS origin was identified intraoperatively. Although lower median values for C5S and C6S were observed in patients with SVN compared with IVN tumors, none of the four scores showed any significant difference between the SVN and IVN groups of VS patients [6].
Borgmann et al. [1] combined posturography and caloric electronystagmography (ENG); caloric testing was done by standard bithermal irrigation of the vestibular organ, using water at 30 and 44 °C, to stimulate the LSC and thus yield a functional depiction of SVN functional state. Eye movements were recorded by ENG, and the maximal slow-phase eye velocity was used to calculate canal paresis. A percentage of left-right difference ≥25% was defined as pathologic. Eighty-nine patients with VS originating from the IVN and 22 patients with VS from the SVN were included. Pathologic results in preoperative caloric ENG (p < 0.0001) and CDPP (p = 0.025) were significantly more frequent in subjects with SVN than with IVN VSs. In addition, hearing preservation rate was significantly higher in patients with tumors from the SVN than from the IVN (p = 0.011) [1].
2 VEMPs and Caloric Test
VEMPs’ apparatus arrangement may differ according to the protocols used; however, a surface electrode is always placed on the upper half of the sternocleidomastoid muscle ipsilateral to the stimulated ear along with a reference electrode on the upper sternum and a ground electrode on the nasion [4, 7]. The patients are then instructed to rotate their heads toward the non-stimulated ear side. During recording, electromyographic activities are monitored on a display to maintain muscle activity at a constant level. Clicks and bursts (of different duration and intensity according to the chosen protocol) are presented through a headphone at a determinate stimulation rate. After response averaging, the amplitude of the first positive-negative peak—i.e., p13-n23—is analyzed, and the percentage of response asymmetry between the two sides is calculated, if present. The responses of VEMPs are regarded as abnormal when the responses on the affected side are absent or decreased compared with those of the unaffected side [4, 7].
VEMPs and caloric test can be regarded as complementary vestibular tests. In fact, they allow for IVN and SVN individual examination, respectively. VEMPs are designed to elicit the vestibulocollic reflex, thus stimulating ASC and PSC, the latter of which is innervated by IVN. On the other hand, the injection of either cold [4, 7, Ushio] or hot [1] water into the external auditory meatus evokes the vestibulo-ocular reflex (VOR) (recorded by ENG), thus stimulating the LSC, innervated by SVN.
Tsutsumi et al. [8] performed a retrospective study to determine whether the nerve of origin of VSs could be predicted using VEMPs alone. Twenty-eight patients undergoing surgical resection were included in the analysis. Complete disappearance of VEMPs was observed only in patients with tumors arising from IVN; therefore the authors concluded that prediction of the nerve of origin was possible only in certain restricted cases [8].
Ushio et al. [9] described a series of 109 consecutive patients diagnosed as having unilateral VS; each of them underwent both VEMPs and caloric test evaluation before surgery. The nerve of origin of the tumor was identified in 63 of the 109 patients. The percentage of patients showing abnormal responses in each test was not different between 37 patients with SVN VSs and 26 patients with IVN VSs: abnormal caloric responses were seen in 86.5% (32/37) of patients with superior VS and in 80.8% (21/26) of patients with inferior VS (p = 0.54), and abnormal VEMPs responses were shown in 77.4% (24/31) of patients with superior VS and in 66.7% (12/18) of patients with inferior VS (p = 0.41) [9].
Suzuki et al. [7] reported results similar to those of the study by Ushio et al. In their 130-patient series, abnormal caloric and VEMPs response rates in patients with tumors arising from the SVN were not significantly different from those in patients with tumors of the IVN (χ2 = 0.618 for caloric test responses, SVN vs. IVN tumor; χ2 = 0.715 for VEMPs responses, SVN vs. IVN tumors) [7].
In the prospective study by Chen et al. [10], eight patients with a cerebellopontine angle (CPA) tumor underwent caloric test and VEMPs examination. Four of the eight patients received surgical intervention, which included three cases of VS and one epidermoid cyst. Follow-up study was performed 1 year after the surgery. During the surgery, the patients with neither caloric response nor VEMPs had a tumor that involved both SVN and IVN. On the contrary, in the one patient with a normal caloric response and absent VEMPs, the tumor originated from IVN. In the follow-up caloric test and VEMPs examination, only one patient with an epidermoid cyst had a complete recovery in both tests, whereas the other three VS patients with absent VEMPs were unchanged. In spite of the limited number of cases, the authors concluded that before surgery, VEMPs test could be used to predict the nerve of origin and to formulate the best surgical approach. After surgery, VEMPs test could be used to define the nature of the tumor (compressing or infiltrating the nerve) and disclose the residual function of the IVN [10].
He et al. [4] conducted as well a prospective study and enrolled 106 VS patients, who received both caloric test and VEMPs examination before the surgical procedure and during follow-up. During the operation, the nerve of origin (SVN or IVN) was identified by the surgeon; proper identification of the nerve of origin was feasible in 68 patients. The tumors arose from the SVN in 26 patients and from the IVN in 42 patients. The results of the caloric tests and VEMPs tests were significantly different in tumors originating from SVN and IVN. The combination of abnormal VEMPs and normal caloric test response yielded a positive predictive value (PPV) as high as 21.4% of tumor originating from IVN; on the other hand, the combination of normal VEMPs and abnormal caloric tests yielded a PPV as high as 50% of tumor originating from SVN. The authors concluded that caloric and VEMPs tests might help to identify whether VSs originate from the SVN or IVN and that such tests could also be used to evaluate the residual function of the nerves after surgery [4].
3 Video Head Impulse Test
The vHIT is a noninvasive test that allows quantitative evaluation of the gain of VOR as well as the identification of covert (occurring while the head is still moving) and overt (occurring once the head movement is finished) saccades on LSCs, ASCs, and PSCs. The procedure consists in the analysis of eye movement (with a video-oculography camera) during head movement, detected and quantified by a dedicated sensor. The patient is asked to fix his gaze at a target 1 m away; then, the examiner rotates the patient’s head randomly 15°–20° on the horizontal plane, thus allowing for the evaluation of both LSCs. The vertical semicircular canals are evaluated with a 45° head rotation to the right (left ASC and right PSC) and to the left (right ASC and left PSC), each followed by an anterior and then a posterior impulse. Twenty stimuli for every semicircular canal are performed to assure a sustained response. The evaluated parameters are gain of VOR (relationship between the velocity of head and eye movements) of every canal, expressed as percentage to evaluate the functional deficit of the affected ear, and the presence of overt and covert saccades. Gain of VOR is categorized as normal or abnormal according to age-dependent normative values. Refixation saccades (both covert and overt) are a physiological phenomenon used by the central vestibular pathways to compensate for the low gain of VOR—thus, they are a sign of a deficit in VOR efficiency [11]. As vHIT analyzes each of the semicircular canals singularly, the detected alterations may be interpreted as indirect signs of pathological compression or infiltration of the corresponding vestibular nerve.
Rahne et al. [12] conducted a study to introduce a novel scoring system that was designed to determine the nerve of origin of VSs, based on vHIT and cervical/ocular VEMPs. The rationale in collecting results of both the functional tests was to gain data as complete as possible about the functional state of both SVN and IVN. In fact, vHIT analyzes the semicircular canals but not the utricle or the saccule. Instead, cervical VEMPs correlate with saccular function and IVN activity as well as ocular VEMPs correlate with utricular function and SVN activity. The parameters included in the scoring system were abnormal gain of VOR and presence of saccades for each of the semicircular canals, abnormal cervical VEMPs, and abnormal ocular VEMPs. The preoperatively acquired data were entered into the scoring system, and the nerve of tumor origin was eventually determined intraoperatively. The scoring system was applied to five consecutive patients undergoing surgical VS treatment. In one case, no determination was possible—this was the largest tumor of the cohort, Koos Grade IV. In all the other cases, the preoperatively predicted tumor origin corresponded to the surgical finding, so that the experimented scoring system yielded a PPV of 100% [12].
Costanzo et al. [11] preoperatively evaluated 31 VS patients with vHIT (gain of VOR, overt and covert saccades on each semicircular canal were reported); the nerve of origin was identified intraoperatively during surgical resection. Surgical identification of the nerve of origin was achieved in 29 of the 31 patients, both the remaining cases being Hannover-T4b lesions. Of the 19 surgically identified SVN schwannomas, vHIT showed a SVN dysfunction pattern in 17 cases and a normal response in 2 cases, giving a correct preoperative diagnosis rate—i.e., a PPV—of 89.5%. Of the ten IVN lesions, vHIT showed an IVN dysfunction pattern in nine cases and a normal test in one case, giving a correct preoperative diagnosis rate of 81.8%. Overall, vHIT lead to a correct identification of the nerve of origin in 100% of altered exams and in 26 (89.7%) of the 29 surgically identified cases. Therefore, the authors concluded that the pattern of semicircular canal dysfunction on vHIT has a localizing value to identify the nerve of origin in VSs [11].
References
Borgmann H, Lenarz T, Lenarz M. Preoperative prediction of vestibular schwannoma’s nerve of origin with posturography and electronystagmography. Acta Otolaryngol. 2011;131(5):498–503.
Brackmann DE, Owens RM, Friedman RA, Hitselberger WE, De la Cruz A, House JW, et al. Prognostic factors for hearing preservation in vestibular schwannoma surgery. Am J Otol. 2000;21(3):417–24.
Cohen NL, Lewis WS, Ransohoff J. Hearing preservation in cerebellopontine angle tumor surgery: the NYU experience 1974-1991. Am J Otol. 1993;14(5):423–33.
He YB, Yu CJ, Ji HM, Qu YM, Chen N. Significance of vestibular testing on distinguishing the nerve of origin for vestibular schwannoma and predicting the preservation of hearing. Chin Med J (Engl). 2016;129(7):799–803.
Jacob A, Robinson LL, Bortman JS, Yu L, Dodson EE, Welling DB. Nerve of origin, tumor size, hearing preservation, and facial nerve outcomes in 359 vestibular schwannoma resections at a tertiary care academic center. Laryngoscope. 2007;117(12):2087–92.
Gouveris H, Akkafa S, Lippold R, Mann W. Influence of nerve of origin and tumor size of vestibular schwannoma on dynamic posturography findings. Acta Otolaryngol. 2006;126(12):1281–5.
Suzuki M, Yamada C, Inoue R, Kashio A, Saito Y, Nakanishi W. Analysis of vestibular testing in patients with vestibular schwannoma based on the nerve of origin, the localization, and the size of the tumor. Otol Neurotol. 2008;29(7):1029–33.
Tsutsumi T, Tsunoda A, Noguchi Y, Komatsuzaki A. Prediction of the nerves of origin of vestibular schwannomas with vestibular evoked myogenic potentials. Am J Otol. 2000;21(5):712–5.
Ushio M, Iwasaki S, Chihara Y, Kawahara N, Morita A, Saito N, et al. Is the nerve origin of the vestibular schwannoma correlated with vestibular evoked myogenic potential, caloric test, and auditory brainstem response? Acta Otolaryngol. 2009;129(10):1095–100.
Chen CW, Young YH, Tseng HM. Preoperative versus postoperative role of vestibular-evoked myogenic potentials in cerebellopontine angle tumor. Laryngoscope. 2002;112(2):267–71.
Constanzo F, Sens P, Teixeira BC de A, Ramina R. Video head impulse test to preoperatively identify the nerve of origin of vestibular schwannomas. Oper Neurosurg. 2018. https://doi.org/10.1093/ons/opy103.
Rahne T, Plößl S, Plontke SK, Strauss C. Preoperative determination of nerve of origin in patients with vestibular schwannoma. German version. HNO. 2017;65(12):966–72.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Campione, A., Cacciotti, G., Roperto, R., Giacobbo Scavo, C., Mastronardi, L. (2019). Vestibular Testing to Predict the Nerve of Origin of Vestibular Schwannomas. In: Mastronardi, L., Fukushima, T., Campione, A. (eds) Advances in Vestibular Schwannoma Microneurosurgery. Springer, Cham. https://doi.org/10.1007/978-3-030-03167-1_19
Download citation
DOI: https://doi.org/10.1007/978-3-030-03167-1_19
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-03166-4
Online ISBN: 978-3-030-03167-1
eBook Packages: MedicineMedicine (R0)