Abstract
Vestibular schwannoma (VS) is a benign tumor which develops in the internal auditory canal and the cerebellopontine angle, potentially diminishing hearing or balance. Most VS tumors arise from one of two vestibular branches: the superior or inferior vestibular nerve. Determining the specific nerve of origin could improve patient management in terms of preoperative counseling, treatment selection, and surgical decision-making and planning. The aim of this study was to introduce a preoperative testing protocol with high accuracy to determine the nerve branch of origin. The nerve of origin was predicted on the basis of preoperative vestibular evoked myogenic potentials (VEMPs), caloric stimulation test, and pure tone audiometry on 26 recipients. The acquired data were entered into a statistic scoring system developed to allocate the tumor origin. Finally, the nerve of origin was definitively determined intraoperatively. Receiver operating characteristic (ROC) curves analysis of preoperative testing data showed the possibility of predicting the branch of origin. In particular, ROC curve of combined VEMPs absence, nystagmus detectable at caloric stimulation, and PTA < 75 dB HL allowed to obtain high accuracy for inferior vestibular nerve implant of the tumor (area under the curve-AUC = 0.8788, p = 0.012). In 24 of 26 cases, the preoperatively predicted tumor origin was the same as the origin determined during surgery. Preoperative audiological and vestibular evaluation can predict the vestibular tumor branch of origin with high accuracy. Despite the necessity of larger prospective cohort studies, these findings may change preoperative approach, possible functional aspects, and counseling with the patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Vestibular schwannoma (VS) is a benign tumor arising from Schwann cells in the vestibular nerve. The vestibular nerve has two divisions in the internal auditory canal (IAC): the superior vestibular nerve (SVN) and the inferior vestibular nerve (IVN). The earliest symptoms in VS patients are auditory, such as hearing loss and tinnitus. VS primarily originates from one of the divisions of vestibular nerve, and hearing outcome might be affected by the origin of the tumor. Therefore, distinguishing the nerve of tumor origin in patients with VS is very important, mainly for the intraoperative strategy of microsurgical removal of small sized VS.
MRI with gadolinium is the gold standard for the vestibular schwannoma diagnosis. Still, it can be useful but it is not diriment in order to predict the branch of origin [2]. Caloric tests are used to estimate the function of the SVN, which innervates the horizontal semicircular canal and is responsible for the caloric response. Vestibular-evoked myogenic potential (VEMP) tests reflect the sacculocollic reflex and are used to evaluate IVN function. If the results of these two tests correlate with the nerve of tumor origin, they will be useful to preoperatively predict the odds of hearing preservation [7, 11].
For this study, we obtained the preoperative results of VEMP tests and caloric stimulation test. Furthermore, we also evaluated the correlations of those with the intraoperative findings regarding the nerve of tumor origin and hearing level in VS patients. We evaluated the efficacy of determining the branch of tumor origin of VS via these tests and looked for a relationship between the nerve of tumor origin and intraoperatory findings.
Methods
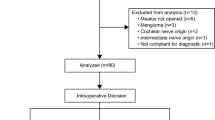
Patient population
This study included 26 patients with unilateral VS (Table 1) who underwent surgical removal of the tumor. Each patient received a caloric test, VEMP test, Auditory Brain Response, and hearing level test before the operation. Only the patients for whom the nerve of tumor origin could be unequivocally identified during surgery were included in the analysis. Mean tumor maximal diameter was 2.95 cm (range 1.8–4.5 cm). Hearing preservation was not attempted in any case: the preoperative hearing class was AAO-HNS C or D in all patients enrolled. All participants gave written informed consents concerning surgery. Authors routinely perform this kind of preoperative evaluation so ethics committee approval was not required.HyporeflexiaHyporeflexia
Magnetic resonance imaging
A 3.0-T superconducting magnet with a standard head coil was used for the head magnetic resonance imaging examinations. Preoperative imaging (MRI) did not allow to predict the possible position of facial nerve.
Vestibular-evoked myogenic potential testing
cVEMP are short latency electromyogenic responses that are recorded from contracted sternocleidomastoid (SCM) muscle in response to very loud transient stimuli. These are thought to reflect momentary inhibition of the contraction of SCM due to loud sounds and are mediated by sacculocollic pathway [12]. The outcome measures of cVEMP, i.e., the latency of P1 and N1 waves, amplitude of P1–N1 complex, and inter-aural amplitude ratio (IAR), are thought to reflect the functioning of saccule and/or inferior branch of vestibular nerve although presently the test cannot differentially diagnose between lesions of these two sites. As the inferior vestibular nerve is involved in neural lesions such as vestibular schwannoma, cVEMP can be a useful tool in the test battery. Furthermore, the proposed pathway of cVEMP involves neural impulses from the inferior vestibular nerve reaching the inferior vestibular nucleus in the brainstem. The descending arc is supposedly via the medial vestibulospinal tracts (MVST) that supply the spinal accessory nerve to the effector muscle SCM [12]. Thus, lesions or tumors of the lower brainstem can affect the cVEMP pathway either in its ascending path (inferior vestibular nerve) or descending path (MVST).
Caloric tests
Caloric tests were performed by standard bithermal irrigation of the external auditory meatus using air at 24 °C and 50 °C for 20 s. The test can conduct to three possible options: areflectic response (no nystagmus), hyporeflectic (paresis), or standard (symmetric nystagmus). Canal paresis (CP) was calculated using the maximal slow-phase eye velocity of caloric nystagmus. CP values > 12% were defined as abnormally decreased on the affected side [1]. Authors considered to distinguish a group with hyporeflective response from another with areflective one.
Hearing level
The hearing level of the patients was detected preoperatively and pure tones averaging (PTA) were calculated.
Statistical analysis
Data were collected and analyzed by means of MedCalc and STATA statistical softwares. In order to determine the accuracy of preoperative test results to determine the branch of origin, authors selected receiver operating characteristic (ROC) curves analysis. A ROC curve is a graphical plot used to show the diagnostic ability of binary classifiers. A ROC curve is constructed by plotting the true positive rate (TPR-y axis) against the false positive rate (FPR-x axis). The higher is the AUC (area under the curve) value obtained, the higher is the accuracy of the preoperative test to identify the branch of origin. In consideration of the dicotomic variable (presence/absence) for VEMPs and caloric stimulation Ny, the identification of a criterion of > 75 dB Hl for PTA ROC curve for inferior branch origin (the nearest branch to the cochlear one) was retained to include in the statistical analysis ROC curves of, respectively, the VEMPS absence (Fig. 1), detectable Ny at caloric stimulation (Fig. 2), and pure tone averaging (PTA) (Fig. 3) for detection of inferior branch origin. Furthermore, it was calculated the interactive dot diagram for PTA (Fig. 4) and the combined ROC curve with VEMPs absence, detectable Ny at caloric stimulation, and PTA values accuracy for the detection of he the inferior branch origin (Fig. 5). Statistical analysis data summary is reported in Table 2.
Results
Preoperative testing data analysis showed the possibility to predict the branch of origin of the lesion. ROC curve of the variable VEMPs absence for the detection of the inferior branch origin showed an area under the curve (AUC) of 0.855 (p < 0.0001), indicating a high accuracy (Fig. 1). Both the detection of nystagmus at caloric stimulation (Fig. 2) and PTA (Fig. 3) ROC curves indicated a slight accuracy for inferior branch origin of the tumor, with AUC values of, respectively, 0.709 (p = 0.0194) and 0.603 (p = 0.3999). A PTA > 75 dB Hl, despite the not significant p value obtained, was obtained as criterion of accuracy for vestibular inferior branch involvement (Fig. 4). Moreover, the ROC curve of combined VEMPs absence, Ny detectable at caloric stimulation, and PTA > 75 dB Hl allowed to obtain high accuracy for inferior vestibular nerve implant of the tumor, with statistical significance (area under the curve-AUC = 0.8788, p = 0.012), as shown in Fig. 5.
Neurosurgeons were blinded to the presumed branch of origin prior to surgery. The branch of tumor origin was identified in all patients by neurosurgeons. In 2 patients on 26, it was not possible to correctly identify preoperatively the branch of origin.
Discussion
Authors investigated whether audiologic and vestibular tests can predict the branch of origin of VS. Caloric stimulation is effective on the horizontal semicircular canal and SVN function. VEMPs are related to the posterior semicircular canal, innervated by IVN. The combination of both tests allow to discriminate between superior and inferior nerve branch function [6]. VEMPs test could be really useful for the diagnosis of VS and it should be assumed that it is the most robust diagnostic method in order to differentiate between superior and inferior vestibular branches.
In this study, caloric stimulation and VEMPs results allowed to predict the tumor branch of origin. In patients with revealable nystagmus at caloric stimulation and no VEMPs thebranch of origin was IVN. In those cases with VEMPs presence and no caloric stimulation responses the branch of origin was SVN. Therefore, VEMPs and caloric stimulation results can aid the neurosurgeon to better approach the dissection by means of previously know the hypothetic branch of origin of the tumor. Still, these findings alone cannot have sufficient accuracy to predict the origin of the tumor and in some cases VEMPs are absent also in superior branch involvement. Chen et al. [3] also reported that in patients with a normal caloric response and no VEMP, the tumor had originated from the IVN. Tsutsumi et al. [14] reported that the complete disappearance of VEMPs was observed only in patients with tumors arising from the IVN. In patients with vestibular neuroma, VEMP could be used as an indicator of IVN involvement [9, 16].
The nerve of origin in 24 patients on 26 was correctly identified with preoperative tests. These numbers were in agreement with previous reports [4, 5, 13, 15]. Moreover, our findings show that the combination of absence of VEMPS, detectable Ny at caloric stimulation, and PTA > 75 dB HL conducts to a higher accuracy in terms of prediction of inferior branch involvement, despite the the number of patients in this study is very small and needs confirmation with higher sample numbers. This information did not have an impact on the surgical approach, but the knowledge of the vestibular nerve of origin could be useful for the intraoperative strategy of microsurgical removal of VS, especially in patients with small tumors. In particular, cutting the capsule and starting the intracapsular debulking of tumor in correspondence of the nerve of origin allow to maintain intact the arachnoidal lane for the following capsule elevation and dissection from brainstem and for facial nerve and, in selected cases, for hearing preservation. This is particularly important in small VS with socially helpful preoperative hearing in order to preserve in the best way the cochlear nerve, but also in larger VS, starting dissection from the vestibular branch of origin allows a better control of the arachnoid lane surrounding the facial nerve.
Recipients with tumor origin on the IVN usually show bad hearing results [7]. During IVN dissection, cochlear nerve can be directly damaged or its blood supply can be involved mainly due to the close anathomical position [10, 17]. In both, patients with with VEMPs absence and revealable responses at caloric stimulation, and those with revealable VEMPs and no nystagmus at caloric stimulation, it was possible to predict the VS branch of origin. Prolonged VEMP latencies may be caused not only by tumor compression to the brain stem or vestibular spinal tract, but also by tumor compression isolated to the IVN [8]. Moreover, caloric test interpretation between areflectic and hyporeflective responses is not so obvious in most cases. It should be then pointed out the possibility of border cases where the combination of these tests could not clarify if the tumor grows from the superior or inferior vestibular branch. Still, VEMP tests are considered to be a clinical test of the IVN, whereas caloric testing is a clinical evaluation of the superior vestibular system. In combination with caloric response testing, VEMP responses have facilitated separate examinations of the inferior and SVN functions [6]. And pure tone audiometry enhances information concerning these diagnostic tasks.
In conclusion, this study indicates that the results of VEMPS, caloric tests, and pure tone audiometry values in patients with VS could be used to identify the nerve origin of the tumor. The combined analysis of these three tests can predict the nerve of tumor origin and disclose the residual function of the IVN.
The audiologic cochleovestibular tests are short and inexpensive; therefore, it would be practical to make this part of the routine examination for patients with VS, as they are also important for predicting hearing preservation.
Conclusion
Audiological and vestibular evaluation with auditory threshold PTA, VEMPs, and caloric stimulation can predict the vestibular tumor branch of origin with high accuracy. Of course, further studies with larger population, prospective cohort case control, and double blinded are needed in order to confirm these findings. Still, the high accuracy found for audiological and vestibular combined preoperative tests in terms of branch of origin identification should open new perspectives concerning not only surgical aspects, but of course also patient preoperative counseling.
Data availability
Not applicable.
Code availability
Not applicable.
References
Brackmann DE, Owens RM, Friedman RA, Hitselberger WE, De la Cruz A, House JW et al (2000) Prognostic factors for hearing preservation in vestibular schwannoma surgery. Am J Otol 21:417–424. https://doi.org/10.1016/S0196-0709(00)80054-X
Chen CW, Young YH, Tseng HM (2002) Preoperative versus postoperative role of vestibular-evoked myogenic potentials in cerebellopontine angle tumor. Laryngoscope 112:267–271. https://doi.org/10.1097/00005537-200202000-00013
Clemis JD, Ballad WJ, Baggot PJ, Lyon ST (1986) Relative frequency of inferior vestibular schwannoma. Arch Otolaryngol Head Neck Surg 112:190–194. https://doi.org/10.1001/archotol.1986.03780020070016
Cohen NL, Lewis WS, Ransohoff J (1993) Hearing preservation in cerebellopontine angle tumor surgery: the NYU experience 1974–1991. Am J Otol 14:423–433. https://doi.org/10.1097/00129492-199309000-00002
Dang L, Tu NC, Chan EY (2020) Current imaging tools for vestibular schwannoma. Curr Opin Otolaryngol Head Neck Surg 28(5):302–307. https://doi.org/10.1097/MOO.0000000000000647
Iwasaki S, Takai Y, Ito K, Murofushi T (2005) Abnormal vestibular evoked myogenic potentials in the presence of normal caloric responses. Otol Neurotol 26:1196–1199. https://doi.org/10.1097/01.mao.0000194890.44023.e6
Jacob A, Robinson LL Jr, Bortman JS, Yu L, Dodson EE, Welling DB (2007) Nerve of origin, tumor size, hearing preservation, and facial nerve outcomes in 359 vestibular schwannoma resections at a tertiary care academic center. Laryngoscope 117:2087–2092. https://doi.org/10.1097/MLG.0b013e3181453a07
Komatsuzaki A, Tsunoda A (2001) Nerve origin of the acoustic neuroma. J Laryngol Otol 115:376–379. https://doi.org/10.1258/0022215011907910
Moriyama T, Fukushima T, Asaoka K, Roche PH, Barrs DM, McElveen JT Jr (2002) Hearing preservation in acoustic neuroma surgery: importance of adhesion between the cochlear nerve and the tumor. J Neurosurg 97:337–340. https://doi.org/10.3171/jns.2002.97.2.0337
Murofushi T, Halmagyi GM, Yavor RA, Colebatch JG (1996) Absent vestibular evoked myogenic potentials in vestibular neurolabyrinthitis. An indicator of inferior vestibular nerve involvement? Arch Otolaryngol Head Neck Surg 122:845–848. https://doi.org/10.1001/archotol.1996.01890200035008
Murofushi T, Matsuzaki M, Mizuno M (1998) Vestibular evoked myogenic potentials in patients with acoustic neuromas. Arch Otolaryngol Head Neck Surg 124:509–512. https://doi.org/10.1001/archotol.124.5.509
Rachinger J, Rampp S, Prell J, Scheller C, Alfieri A, Strauss C (2011) Tumor origin and hearing preservation in vestibular schwannoma surgery. J Neurosurg 115:900–905. https://doi.org/10.3171/2011.7.JNS102092
Slattery WH 3rd, Brackmann DE, Hitselberger W (1997) Middle fossa approach for hearing preservation with acoustic neuromas. Am J Otol 18:596–601
Stockwell CW (1991) Vestibular function tests. In: Paparella MM, Shumrick DA, Gluckman JL, Meyerhoff WL (eds) Otolaryngology. W.B. Saunders Company, Philadelphia, p. 921–48 ò5
Suzuki M, Yamada C, Inoue R, Kashio A, Saito Y, Nakanishi W (2008) Analysis of vestibular testing in patients with vestibular schwannoma based on the nerve of origin, the localization, and the size of the tumor. Otol Neurotol 29:1029–1033. https://doi.org/10.1097/MAO.0b013e3181845854
Takeichi N, Sakamoto T, Fukuda S, Inuyama Y (2001) Vestibular evoked myogenic potential (VEMP) in patients with acoustic neuromas. Auris Nasus Larynx 28(Suppl):S39-41. https://doi.org/10.1016/S0385-8146(01)00075-X
Tsutsumi T, Tsunoda A, Noguchi Y, Komatsuzaki A (2000) Prediction of the nerves of origin of vestibular schwannomas with vestibular evoked myogenic potentials. Am J Otol 21:712–715
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by Francesca Cianfrone and Italo Cantore. The first draft of the manuscript was written by Francesca Cianfrone and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
Not applicable (routinary preoperative audiologic testings).
Consent for publication
Not applicable.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Cianfrone, F., Cantore, I., Roperto, R. et al. Preoperative vestibular evoked myogenic potentials (VEMPs), caloric test, and pure tone audiometry to identify the vestibular nerve branch of schwannoma origin: preliminary results in a series of 26 cases. Neurosurg Rev 45, 3231–3236 (2022). https://doi.org/10.1007/s10143-022-01834-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10143-022-01834-z