Abstract
The myelodysplastic syndromes (MDS) are clonal hematopoietic stem cell diseases characterized by cytopenia(s) due to ineffective hematopoiesis accompanied by dysplasia in one or more myeloid cell lines and an increased risk of development of acute leukemia. A correct diagnosis and classification of MDS requires integration of morphology with clinical data and ancillary studies including cytogenetics and next-generation sequencing to detect submicroscopic pathogenic variants. Assessment of morphologic dysplasia relies on review of adequately stained peripheral blood smear, bone core biopsy, and bone marrow aspirate smears. In addition, the blast count is predictive of progression to acute leukemia and should be obtained from a careful assessment of 200 cells in the peripheral blood and 500 cells on the bone marrow aspirate. The chapter summarizes morphologic dysplasia for each of the lineages in the context of the diagnostic criteria for the WHO-defined MDS categories (see Table 10.1 and reference [1]). It is now recognized that cytopenia is invariably implicit in the diagnosis of MDS and the clinical behavior is influenced by the number of dysplastic lineages and the blast count [2]. The WHO revision therefore proposes to change the nomenclature to eliminate the use of refractory anemia and refractory cytopenia and replace it with “myelodysplastic syndrome” with further subclassification relying on the dysplastic lineages and the blast count (Tables 10.1 and 10.2) (Figs. 10.1, 10.2, 10.3, 10.4, 10.5, 10.6, 10.7, 10.8, 10.9, 10.10, 10.11, 10.12, 10.13, 10.14, 10.15, 10.16, 10.17, 10.18, 10.19, 10.20, 10.21, 10.22, 10.23, 10.24, 10.25, 10.26, 10.27, 10.28, 10.29, 10.30, 10.31, 10.32, 10.33, 10.34, 10.35, 10.36, 10.37, 10.38, 10.39, and 10.40).
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
The myelodysplastic syndromes (MDS) are clonal hematopoietic stem cell diseases characterized by cytopenia(s) due to ineffective hematopoiesis accompanied by dysplasia in one or more myeloid cell lines and an increased risk of development of acute leukemia. A correct diagnosis and classification of MDS requires integration of morphology with clinical data and ancillary studies including cytogenetics and next-generation sequencing to detect submicroscopic pathogenic variants. Assessment of morphologic dysplasia relies on review of adequately stained peripheral blood smear, bone core biopsy, and bone marrow aspirate smears. In addition, the blast count is predictive of progression to acute leukemia and should be obtained from a careful assessment of 200 cells in the peripheral blood and 500 cells on the bone marrow aspirate. The chapter summarizes morphologic dysplasia for each of the lineages in the context of the diagnostic criteria for the WHO-defined MDS categories (see Table 10.1 and reference [1]). It is now recognized that cytopenia is invariably implicit in the diagnosis of MDS and the clinical behavior is influenced by the number of dysplastic lineages and the blast count [2]. The WHO revision therefore proposes to change the nomenclature to eliminate the use of refractory anemia and refractory cytopenia and replace it with “myelodysplastic syndrome” with further subclassification relying on the dysplastic lineages and the blast count (Table 10.1 (Figs. 10.1, 10.2, 10.3, 10.4, 10.5, 10.6, 10.7, 10.8, 10.9, 10.10, 10.11, 10.12, 10.13, 10.14, 10.15, 10.16, 10.17, 10.18, 10.19, 10.20, 10.21, 10.22, 10.23, 10.24, 10.25, 10.26, 10.27, 10.28, 10.29, 10.30, 10.31, 10.32, 10.33, 10.34, 10.35, 10.36, 10.37, 10.38, 10.39, and 10.40).
Peripheral blood smear from a 67-year-old gentleman with a diagnosis of refractory anemia (now classified as MDS with single lineage dysplasia [MDS-SLD]) showing dimorphic red blood cells including some macrocytic ovalocytes. The neutrophil in the field has appropriate nuclear lobation and cytoplasmic granularity. Blasts were not seen in the peripheral blood. The patient presented with anemia of 9 g/dL and normal white cell count and platelet count, normal B12 and folic acid levels. A diagnosis of MDS-SLD can be made with cytopenia of two lineages as long as dysplasia is restricted to a single lineage. Patients presenting with pancytopenia tend to have a different clinical outcome and are classified as myelodysplastic syndrome, unclassifiable (see Fig. 10.40)
Bone marrow biopsy shows a hypercellular bone marrow with increased erythroid precursors. There is no increase in bone marrow blasts, and progressively maturing granulopoiesis is present along with normal megakaryocytes (bottom of the field). Other patients can have normocellular and, less commonly, hypocellular bone marrows
Bone marrow aspirate from a 71-year-old woman with a diagnosis of MDS-SLD shows more pronounced erythroid dysplasia. Nuclear budding, multinuclearity, and nuclear hyperlobation can be seen in addition to megaloblastoid erythroid maturation. Granulocytic dysplasia is equivocal and manifests as occasional neutrophils with nuclear hypolobation and nuclear excrescences. Less than 10% of the neutrophils were affected. The vast majority of the cases with a diagnosis of MDS-SLD will be cases with anemia and bone marrow dyserythropoiesis [3]. Isolated granulocytic dysplasia and isolated megakaryocyte dysplasia are uncommon and warrant meticulous exclusion of autoimmune phenomenon, exposure to drugs, and infectious etiologies that might result in secondary suppression of these lineages as well as morphologic changes mimicking dysplasia
Peripheral blood smear from a patient with a history of kidney transplant on valacyclovir and tacrolimus showing red cell macrocytosis and numerous hypolobated neutrophils in the peripheral blood. The case highlights the fact that the presence of morphologic dysplasia alone is not sufficient to establish a diagnosis of MDS and was secondary to the medications in this case
Bone marrow aspirate smear from a 42-year-old female patient who presented with pancytopenia. Bone marrow aspirate showed cytoplasmic vacuoles in precursors of all lineages. There was no increase in bone marrow blasts. A karyotype analysis revealed a normal female karyotype. Additional history obtained was notable for bariatric surgery performed 2 years prior to her current presentation. Because of the history and bone marrow morphology notable for vacuolated cytoplasm of both erythroid and myeloid lineage, copper deficiency (an MDS mimic) was suspected and laboratory studies showed a copper level of less than 20 mcg/dL. In addition to bariatric surgery, copper deficiency can result from parenteral or tube feedings without copper supplementation, protein-losing enteropathies and excessive zinc intake (causes intestinal trapping of copper), zinc-containing denture adhesive, and nutritional supplements [4]
Peripheral blood smear from a patient with myelodysplastic syndrome with single lineage dysplasia and ring sideroblasts (MDS-RSSLD) previously known as refractory anemia with ring sideroblasts (RARS) . The red cells are macrocytic, and basophilic stippling noted in the red cells is a consequence of abnormal ribosomal maturation and retention in anucleate red cells
Prussian blue stain of the bone marrow aspirate of MDS-RSSLD shows numerous ring sideroblasts. Ring sideroblasts are defined as red cell precursors with 5 or more granules encircling one-third or more of the nucleus. Historically, the diagnosis of refractory anemia with ring sideroblasts (RARS) was rendered in patients with peripheral blood anemia and dysplasia restricted to the erythroid lineage if 15% or more of the erythroid precursors were demonstrated to be ring sideroblasts. Recent data [5] has indicated a strong correlation between the presence of bone marrow ring sideroblasts and mutation in the spliceosome gene SF3B1 . The upcoming revision of the WHO classification therefore allows for making the diagnosis with as few as 5% ring sideroblasts if an SF3B1 mutation is present. In keeping with the revised nomenclature that eliminates the use of refractory anemia, the proposed new classification of RARS is MDS-RSSLD
In contrast to Fig. 10.9, this bone marrow aspirate shows a dysplastic unilobated megakaryocyte in addition to megaloblastoid erythroid precursors. A Prussian blue stain showed numerous ring sideroblasts and next-generation sequencing (NGS) was notable for an SF3B1 mutation. In the absence of increased bone marrow blasts, the presence of SF3B1 mutation is associated with a favorable outcome even in patients with multilineage dysplasia [6]. The 2016 revision of the WHO classification allows for recognition of patients with multilineage dysplasia and ring sideroblasts or SF3B1 mutation as a distinct subtype designated MDS with multilineage dysplasia and ring sideroblasts (MDS-RSMLD)
MDS-RSMLD with megaloblastoid erythroid maturation and granulocytic dysplasia manifest as nuclear hypolobation and hypogranular cytoplasm in 20% of the neutrophil precursors and neutrophils. Blasts were less than 5% of the cells in the bone marrow. A Prussian blue stain showed ring sideroblasts and NGS showed SF3B1 mutation
MDS with multilineage dysplasia (MDS-MLD) is associated with variable cytopenias. In this example, all three lineages are affected. No blasts were appreciated in the peripheral blood. The neutrophil shown is dysplastic and shows hypolobated nucleus with abnormally condensed chromatin and hypogranular cytoplasm
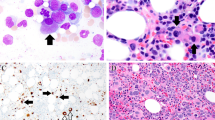
MDS-MLD with hypercellular bone marrow indicative of ineffective hematopoiesis, which is a common underlying feature of all MDS. The biopsy is notable for megaloblastoid erythroid maturation and unilobated megakaryocytes. While granulocytic maturation is left shifted, blasts account for less than 5% of the marrow cellularity
The bone marrow aspirate smear shows dysplastic megakaryocytes that are small in size and have a single-lobed nucleus. Other megakaryocytes are larger and shows widely separated nuclear lobes. In addition, there is megaloblastoid erythroid maturation with nuclei notable for budding and bilobation consistent with dysplasia in two lineages and a diagnosis of MDS-MLD previously referred to as refractory cytopenia with multilineage dysplasia (RCMD)
MDS-MLD affecting granulocytic and megakaryocyte lineage. Neutrophil dysplasia is represented by nuclear hypolobation and cytoplasmic granularity. Megakaryocyte dysplasia is represented by abnormally separated nuclear lobes. Erythropoiesis is overall reduced and blasts were less than 5%. No ring sideroblasts were appreciated and the karyotype was notable for i(17q) resulting in deletion of the short arm of chromosome 17 with consequent loss of TP53 gene
The bone marrow aspirate smear is from a 71-year-old gentleman who presented with anemia and thrombocytopenia and 2% blasts in the peripheral blood. The bone marrow aspirate shows marked granulocytic dysplasia represented by unilobated and hypolobated neutrophils with cytoplasmic hypogranularity and 6% blasts in the bone marrow consistent with a diagnosis of MDS with excess blasts-1 (MDS-EB1) previously referred to as refractory anemia with excess blasts (RAEB)
The bone marrow aspirate smear is notable for presence of dysplastic megakaryocytes, dysplastic neutrophils, and 12% blasts consistent with a diagnosis of MDS-EB2. The karyotype was notable for -5 and del(20q). The clinical course was notable for progression to acute myeloid leukemia 3 months after initial diagnosis
In about 15% of patients with MDS, significant fibrosis can be seen in the bone marrow [7]. The bone core biopsy shown here is notable for streaming of cells and dilated sinuses suggestive of underlying fibrosis. Clearly dysplastic megakaryocytes are appreciated close to the boney trabeculum
CD34 immunostaining in a patient with MDS and increased bone marrow fibrosis. Most cases of MDS with fibrosis are associated with increased blasts. However, the bone marrow aspirate smears are inadequate for an accurate differential, and the demonstration of increased bone marrow blasts relies on immunohistochemistry
CD61 immunostaining used to highlight small dysplastic megakaryocytes in a bone core biopsy in a patient with MDS and increased bone marrow fibrosis. These dysplastic megakaryocytes can be numerous in patients with increased bone marrow fibrosis and somewhat masked by numerous granulocytic precursors particularly when micromegakaryocytes are present
MDS-EB with ring sideroblasts and SF3B1 mutation as exemplified by this case with multilineage dysplasia and increased blasts is not associated with the favorable outcome noted in patients with SF3B1 mutation but no increase in bone marrow blasts. Therefore, irrespective of SF3B1 mutation, the diagnosis for these cases remains MDS with excess blasts
The bone marrow aspirate shows increased blasts (6% of the marrow cellularity) along with increased erythroid precursors that account for 80% of the marrow cellularity. This would have resulted in enumeration of the blasts as a fraction of non-erythroid cells and a diagnosis of acute myeloid leukemia of the erythroid/myeloid type per the 2008 WHO classification. However, the clinical behavior and genetic profile of these cases are more closely aligned to MDS than AML [8]. Therefore the 2016 revision of the WHO classification recommends enumeration of the blast count from all nucleated cells in the bone marrow. The appropriate diagnosis for this bone marrow aspirate would therefore be MDS-EB1
The bone marrow aspirate smear illustrates an Auer rod in patient with megakaryocyte and erythroid dysplasia and bone marrow blast count of 3%. Irrespective of the peripheral blood or bone marrow blast count, the presence of Auer rods in the blasts tends to be associated with a more aggressive clinical course, and these cases are best classified as MDS-EB [9]
Bone marrow aspirate smear shows several small, unilobated megakaryocytes and no dysplasia in the maturing granulocytic cells. The karyotype was notable for a single cytogenetic abnormality of del(5q). The term 5q- syndrome has been used to designate cases with macrocytic anemia, normal or elevated platelet count, and BM erythroid hyperplasia. By definition, the peripheral blood blast count is less than 1% and the bone marrow blast count is less than 5%. Recent literature has demonstrated that single additional, low-risk cytogenetic abnormalities do not influence the clinical behavior of the disease, and therefore the diagnosis of MDS with isolated del(5q) can be made even in the presence of one additional cytogenetic abnormality provided it is not monosomy 7 [10]
Another example of bone marrow aspirate notable for megaloblastoid erythroid maturation and unilobated megakaryocyte. While rare neutrophils with hypogranular cytoplasm, as shown here, can be present, neutrophil dysplasia in more than 10% of the neutrophils or more than 5% bone marrow blasts precludes the diagnosis of MDS with isolated del(5q)
MDS presenting in childhood is extremely uncommon and the diagnosis should always lead to careful exclusion of inherited bone marrow failure syndrome. Unlike the adult population, low-grade MDS in the childhood group frequently presents with very hypocellular bone marrow and needs to be distinguished from aplastic anemia. The presence of clusters of erythroid precursors with megaloblastoid erythroid maturation and increased mitoses as shown in this image are supportive of a diagnosis of refractory cytopenia of childhood (RCC) and help distinguish the condition from aplastic anemia [11, 12]
The bone core biopsy with dysplastic megakaryocytes and increased blasts demonstrates another presentation of childhood MDS. In the context of increased bone marrow blasts, the presence of leukemia-defining cytogenetic abnormalities such as t(8;21) or inv(16) should be excluded. When present, these recurrent cytogenetic abnormalities allow the diagnosis of AML even with less than 20% bone marrow blasts
The bone marrow aspirate shows increased blasts along with dysplastic neutrophils . The karyotype was notable for monosomy 7. Abnormal karyotype is seen in 55% of children with MDS with excess blasts with monosomy 7 being the most common cytogenetic abnormality followed by trisomy 8 and trisomy 21 [13]
Contrary to the name, MDS unclassifiable (MDS-U) as a category is a designation used for three specific situations. The peripheral blood illustrates one such example of the presence of 1% blasts on two repeat peripheral blood smears in a patient with peripheral pancytopenia and bone marrow notable for 2% blasts accompanied by dysgranulopoiesis and dyserythropoiesis. These patients tend to have a clinical course somewhat more aggressive than that observed when peripheral blood blasts are less than 1% resulting in a diagnosis of MDS-U
More frequently, a diagnosis of MDS-U is made when, in the context of peripheral cytopenia(s), the bone marrow dysplasia is equivocal or affects less than 10% cells for a given lineage but is accompanied by an MDS-defining cytogenetic abnormality (see Table 10.2). This bone marrow aspirate showed occasional hypolobated neutrophils, 1% bone marrow blasts, and no erythroid or megakaryocyte dysplasia. The karyotype was notable for the presence of monosomy 13
The third category of MDS cases, in which diagnosis of MDS-U is preferred, is in the context of pancytopenia with unequivocal dysplasia in a single lineage in the bone marrow. The peripheral blood shown here is notable for pancytopenia with no circulating blasts. However, the bone marrow showed mostly hypolobated megakaryocytes but unremarkable neutrophils and erythroid precursors. The karyotype was notable for trisomy 8 and a normal chromosome 5
References
Arber DA, Orazi A, Hasserjian R, Thiele J, Borowitz MJ, Le Beau MM, et al. The 2016 revision to the World Health Organization classification of myeloid neoplasms and acute leukemia. Blood. 2016;127:2391–405.
Arber DA, Hasserjian RP. Reclassifying myelodysplastic syndromes: what’s where in the new WHO and why. Hematology Am Soc Hematol Educ Program. 2015;2015:294–8.
Germing U, Strupp C, Giagounidis A, Haas R, Gattermann N, Starke C, et al. Evaluation of dysplasia through detailed cytomorphology in 3156 patients from the Dusseldorf registry on myelodysplastic syndromes. Leuk Res. 2012;36:727–34.
Willis MS, Monaghan SA, Miller ML, McKenna RW, Perkins WD, Levinson BS, et al. Zinc-induced copper deficiency: a report of three cases initially recognized on bone marrow examination. Am J Clin Pathol. 2005;123:125–31.
Papaemmanuil E, Cazzola M, Boultwood J, Malcovati L, Vyas P, Bowen D, et al. Somatic SF3B1 mutation in myelodysplasia with ring sideroblasts. N Engl J Med. 2011;365:1384–95.
Malcovati L, Karimi M, Papaemmanuil E, Ambaglio I, Jädersten M, Jansson M, et al. SF3B1 mutation identifies a distinct subset of myelodysplastic syndrome with ring sideroblasts. Blood. 2015;126:233–41.
Vardiman JW. Hematopathological concepts and controversies in the diagnosis and classification of myelodysplastic syndromes. Hematology Am Soc Hematol Educ Program. 2006:199–204.
Grossmann V, Bacher U, Haferlach C, Schnittger S, Pötzinger F, Weissmann S, et al. Acute erythroid leukemia (AEL) can be separated into distinct prognostic subsets based on cytogenetic and molecular genetic characteristics. Leukemia. 2013;27:1940–3.
Willis MS, McKenna RW, Peterson LC, Coad JE, Kroft SH. Low blast count myeloid disorders with Auer rods: a clinicopathologic analysis of 9 cases. Am J Clin Pathol. 2005;124:191–8.
Germing U, Lauseker M, Hildebrandt B, Symeonidis A, Cermak J, Fenaux P, et al. Survival, prognostic factors and rates of leukemic transformation in 381 untreated patients with MDS and del(5q): a multicenter study. Leukemia. 2012;26:1286–92.
Baumann I, Führer M, Behrendt S, Campr V, Csomor J, Furlan I, et al. Morphological differentiation of severe aplastic anaemia from hypocellular refractory cytopenia of childhood: reproducibility of histopathological diagnostic criteria. Histopathology. 2012;61:10–7.
Niemeyer CM, Baumann I. Classification of childhood aplastic anemia and myelodysplastic syndrome. Hematology Am Soc Hematol Educ Program. 2011;2011:84–9.
Hasle H. Myelodysplastic and myeloproliferative disorders of childhood. Hematology Am Soc Hematol Educ Program. 2016;2016:598–604.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2018 Springer Science+Business Media, LLC
About this chapter
Cite this chapter
Gurbuxani, S. (2018). Myelodysplastic Syndrome. In: George, T., Arber, D. (eds) Atlas of Bone Marrow Pathology. Atlas of Anatomic Pathology. Springer, New York, NY. https://doi.org/10.1007/978-1-4939-7469-6_10
Download citation
DOI: https://doi.org/10.1007/978-1-4939-7469-6_10
Published:
Publisher Name: Springer, New York, NY
Print ISBN: 978-1-4939-7467-2
Online ISBN: 978-1-4939-7469-6
eBook Packages: MedicineMedicine (R0)