Abstract
Myelodysplastic syndrome (MDS) is clonal hematopoietic stem cell disorders characterized by presence of cytopenia(s), dysplasia in ≥1 hematopoietic cell lineage, ineffective hematopoiesis, and an increased risk of progression to acute myeloid leukemia (AML) [1]. The diagnosis of MDS rests on the clinical features, presence of cytopenia in one or more myeloid lineages, morphological evidence of dysplasia, increased blasts in bone marrow and relevant cytogenetic abnormalities and molecular mutations. World Health organization (WHO) 2017 revised classification uses a combination of morphology, genetic features, and immunophenotype to assign a disease category to a case [2].
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
Myelodysplastic syndrome (MDS) is clonal hematopoietic stem cell disorders characterized by presence of cytopenia(s), dysplasia in ≥1 hematopoietic cell lineage, ineffective hematopoiesis, and an increased risk of progression to acute myeloid leukemia (AML) [1]. The diagnosis of MDS rests on the clinical features, presence of cytopenia in one or more myeloid lineages, morphological evidence of dysplasia, increased blasts in bone marrow and relevant cytogenetic abnormalities and molecular mutations. World Health organization (WHO) 2017 revised classification uses a combination of morphology, genetic features, and immunophenotype to assign a disease category to a case [2].
Anemia is the commonest feature, presents as easy fatigability, feeling of tiredness, malaise and may require blood transfusions. Severe neutropenia may present with increased infections, and moderate to severe thrombocytopenia may cause bleeding in the form of petechiae, and ecchymosis. Patients may present with a single or a combination of cytopenias [3].
2 Nomenclature
Since the French-American-British classification proposed in 1982 [4], cases of MDS were referred to as refractory anemia and refractory cytopenia. The same was retained through the two previous WHO classifications [5, 6]. However, this terminology of “refractory anemia” and “refractory cytopenia” has been replaced by MDS in recent classification. The entities are further defined on the basis of presence of single lineage/multilineage dysplasia, blast counts, ring sideroblasts (RS) into subdivisions of MDS. A comparative of WHO 2008 and 2017 classified cases is given in Table 9.1.
3 Cutoffs in MDS
The evaluation of a patient of MDS requires well-stained cellular peripheral blood (PB) and bone marrow aspirate (BMA) smears. WHO has recommended the use of May Grunwald Giemsa and Wright-Giemsa stained smears for optimal assessment of granularity [5].
3.1 Cutoffs for Cytopenias
The WHO 2017 classification retains the prior cutoffs for cytopenias, a hemoglobin of <10 g/dL, absolute neutrophils count (ANC) of ≤1.8 × 109/L, and platelet count of 100 × 109/L [7]. However, it has been recognized that some patients may have persistent cytopenias at values higher than the recommended thresholds [8, 9]. The WHO 2017 classification provides lower thresholds for such cases when characteristic morphological abnormalities or cytogenetic abnormalities are present and hemoglobin <13 g/dL in men and <12 g/dL in women or platelet count is <150 × 109/L [2]. In addition, all cases of MDS should have an absolute monocyte count of <1 × 109/L [2, 5, 6]. A platelet count of >450 × 109/L may be present in patients of MDS with del(5q) abnormality or cases associated with t(3,3)(q21.3;q26.2) or inv(3) (q21.3;q26.2) and does not warrant a classification to myelodysplastic syndrome/myeloproliferative neoplasm (MDS/MPN) [2].
3.2 Cutoffs for Dysplasia and Blasts
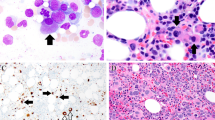
The second hallmark of MDS is the morphological evidence of dysplasia in ≥1 myeloid cell line. The WHO 2017 classification has retained a cutoff of ≥10% dysplasia in either erythroid, myeloid, or megakaryocytic lineage. It, however, recognizes the fact that some normal individuals may harbor dysplasia in >10% cells [2]. Parmentier et al. [10] showed that >10% dysmyelopoiesis could be seen in 45% marrows of normal stem cell donors, 26% have bi-lineage, and 7% have tri-lineage dysplasia. In contrast to the age-related increase in MDS, it was seen that young donors were more likely to have dysplasia in myeloid and megakaryocytic lineage [10]. Certain abnormalities like pseudo Pelger–Huet abnormality and megakaryocytic abnormalities (karyorrhexis, multinuclearity, nuclear fragmentation, and micromegakaryocytes) are more specific for MDS [11, 12]. Reproducibility of dysplasia, however, tends to be poor even when experienced hematopathologists examine the slides [13]. Moreover, cases with subtle dysplasia limited to one lineage require a stringent exclusion of reactive mimics of MDS [10].
Myeloblasts constitute <20% of all nucleated cells. Peripheral blood and bone marrow blast percentages decide the categorization of MDS into individual subdivisions [2]. Morphological features of dysplasia are described in Table 9.2.
3.3 Cutoffs for Ring Sideroblasts
Cases of MDS may show the presence of ring sideroblasts (RS) defined as >5 granules encircling >1/3rd of the nuclear membrane [14]. The earlier WHO 2008 classification warranted ≥15% RS to be considered as significant [6] but the WHO 2017 classification incorporates the genetic data for SF3B1 mutations [2]. In cases where RS are present but are 5–15%, the presence of SF3B1 mutations should be ideally assessed and if present, they are adequate to classify a case as MDS-single lineage dysplasia with RS or MDS-multilineage dysplasia with RS [2, 15, 16]. This is the only mutation that impacts the classification of MDS as it has been strongly found to be associated with this subcategory of MDS [17,18,19]. The RS threshold has been lowered as cases with SF3B1 mutations may present with as low as 1% RS [19]. However, if the SF3B1 mutation testing cannot be performed, a threshold of ≥15% should be adhered to [2].
Clonal cytogenetic abnormalities are present in ~50% of all patients of MDS [2, 6, 20, 21]. The incidence is higher in patients with therapy-related MDS at ~80% [21]. Del(5q) is the commonest abnormality seen in MDS with an incidence of ~10–15%. On one extreme, it is associated with good prognosis and a good response to lenalidomide therapy [22, 23] and at the other extreme, it is enriched in therapy-related MDS and is associated with a short overall survival and high risk of progression to acute myeloid leukemia [24,25,26]. Hence, for the diagnosis of MDS with isolated del(5q), it is important that all therapy-related MDS be classified first and the strict diagnostic criteria of the entity are then adhered to. Del(5q) is associated with a distinct clinical syndrome with presence of macrocytosis, normal or high platelet count, and presence of hypolobated or monolobated megakaryocytes on the BM examination [2, 6]. Trisomy 8, del(20q), and loss of chromosome Y are seen in 10%, 5–8%, and ~5% cases of MDS but are not sufficient to warrant a diagnosis of MDS as they are not specific to MDS [2]. The list of cytogenetic abnormalities which can lead to a classification of MDS in MDS-U is presented in Table 9.3 [2]. These abnormalities should be demonstrated only by conventional karyotype and not by FISH or sequencing [2]. Loss of 17p is associated strongly with TP53 mutations and manifests morphologically as pseudo Pelger–Huet anomaly and vacuolation in neutrophils [2].
3.4 Exclusion Criteria
A diagnosis of MDS should not be made if the assessment is made during an acute infection. Vitamin B12/folate, copper deficiencies should be excluded. Patients exposed to heavy metals such as arsenic, lead, and zinc may also show marked dysplasia [2, 5, 6]. Copper deficiency causes cytopenias with cytoplasmic vacuolization in the erythroid precursors and presence of RS [27,28,29]. Copper deficiency may be precipitated by zinc excess and should be considered in patients receiving supplemental zinc [30]. In addition, tuberculosis [31] and autoimmune diseases [32] may also be associated with myelodysplasia on morphology and they should be excluded if other suggestive features are present. Mycophenolate mofetil, tacrolimus, and ganciclovir may cause pseudo Pelger–Huet abnormality [33, 34], and isoniazid in absence of pyridoxine may cause ring sideroblasts [35]. Patients should not be evaluated within a short period of chemotherapeutic agents or granulocyte colony stimulating factor (G-CSF) therapy [2, 5, 6]. Other clinical mimics of MDS are paroxysmal nocturnal hemoglobinuria (PNH), large granular lymphocytic leukemia, and hairy cell leukemia [2].
4 Diagnostic Criteria for WHO 2017 Classification of MDS [2]
5 Evaluation of a Case of MDS
Evaluation of a patient suspected as MDS requires a peripheral blood sample for a complete blood count, reticulocyte count, and smear evaluation. A 200 cell differential on well-stained PB smears and 500 cell myelogram on BM smears is mandatory [2]. Blood smears should be prepared within 2 h of sample collection and in cases of very low counts, buffy coat smears may be used for differential counts on the peripheral smear [2].
A bone marrow examination procedure should always include an aspiration and bone marrow biopsy (BMBx), and additional samples should be collected in heparin and EDTA to send for karyotyping, fluorescence-in-situ hybridization (FISH), and for molecular workup [2]. Additional stains may be required on BMA smears to identify erythroid dysplasia. These include Perl’s stain to look for RS and Per-iodic acid Schiff stain (PAS) to identify dysplastic erythroid cells [2]. Normally erythroid cells are negative for PAS but dysplastic erythroid cells may show diffuse cytoplasmic positivity or diffuse granular positivity or block positivity [12]. BMBx is extremely important in MDS presenting with marrow fibrosis for evaluation of megakaryocytic dysplasia and blast counts in borderline cases using immunohistochemistry (IHC) for CD34 and CD117. IHC for CD61 or CD42b may be applied to identify micromegakaryocytes and megakaryocytic dysplasia [36]. Though WHO has not made immunophenotyping mandatory, it should also be considered in the evaluation of MDS as it can give objective clues in difficult cases, especially the low-grade MDS cases with blasts <5% and RS <15% [37,38,39,40]. The evaluation for PNH clone should be done in low-grade MDS cases [41].
6 Other Changes in WHO Classification, 2017
-
1.
Reclassification of acute erythroleukemia to MDS
With the proposal of the updates in WHO 2008 classification in 2016 [16] and finally with the release of the WHO 2017 revised edition [2], a major change in the acute leukemia classification that affects MDS directly is the abolishment of the acute erythroid/myeloid leukemia (AML-M6a). This entity was originally defined by French-American-British classification [42] but was accepted by the WHO in 2001 [5] and retained in 2008 [6]. The criteria of definition were: (a) Bone marrow containing ≥50% erythroid cells of the total nucleated cells; (b) Myeloblasts ≤20% of all nucleated cells; (c) Myeloblasts ≥20% of all non-erythroid cells. The WHO 2017 classification [2] has done away with the “non-erythroid blast count” altogether. Therefore, most cases that were classified in pre-2016 era as AML-M6a would now fall into the category of MDS with excess blasts.
The prognostic similarity of AML-M6a and MDS has been shown by two series from MD Anderson Cancer center [43] and Grupo Español de Síndromes Mielodisplásicos (GESMD) [44] published in the same issue of Modern Pathology in 2016. In the former series, 77 AML-M6a cases were compared to 279 de novo MDS-refractory anemia with excess blasts cases. Patients of AML-M6a treated with intensive AML chemotherapy did not perform better than patients treated with lower intensity therapy or only supportive care. In addition, on multivariate analysis, very high R-IPSS and high R-IPSS were independent risk factors for short overall survival while a diagnosis of AML-M6a was not a risk factor [43]. In the second series, AML-M6a patients were compared to erythroid predominant refractory anemia with excess blasts 1 and 2 (RAEB1 and RAEB2) patients separately and there was no prognostic difference between them. Only high-risk karyotype as defined by R-IPSS and IPSS was associated with prognosis. Even patients of AML-M6a diagnosed at a low blast percentage of 5–10% on the all nucleated cell count were prognostically similar to AML-M6a patients with higher blast counts in all nucleated cells [44]. These studies demonstrate the actual applicability of the WHO 2017 classification and prove that acute erythroleukemia is an extension of MDS and the cases are better classified in MDS.
The reasons considered by the Clinical Advisory Committee for this change were that in cases with extremely high number of erythroid cells, the complicated calculation would sometimes lead to a classification of a case with ≤5% blasts as AML-M6a. Secondly, the cytogenetic and mutational profile of cases classified as AML-M6a is more similar to MDS than de novo AML, such as the presence of p53 mutations and rare presence of NPM1 and FLT3 mutations. Thirdly, it was seen that diagnosis of a case as erythroleukemia did not always predict clinically aggressive disease course. In addition, it is very well recognized that a slight change in percentage of erythroid cells from <50 to ≥50% can alter the diagnosis and may result from many variables including nutritional deficiency, erythropoietin supplementation, or inter-/intra-observer variation. There are problems pertaining to poor reproducibility and lack of consistency [15, 45,46,47,48]. Therefore, the entity of erythroleukemia/AML-M6a has been abolished by WHO 2017 classification [2]. This change in classification means that cases with 70% erythroid cells, 12% myeloblasts and >20% non-erythroid blasts will now be classified as MDS-EB2 and not as AML-M6a. The entity of pure erythroid leukemia (PEL) will however continue to be a part of the AML classification. To classify a case as PEL, there should be ≥80% erythroblasts and ≥30% pro-erythroblasts [2]. An approach to the cases with ≥50% erythroblasts in the bone marrow is being presented in Fig. 9.2.
-
2.
Identification of myeloid neoplasms with germline mutations
This category has been incorporated by WHO 2017 to address the familial cases of MDS and AML [2]. MDS/AML associated with inherited marrow failure syndromes like Fanconi anemia, dyskeratosis congenita, etc. had been recognized since long but now other disorders with an inherited predisposition to MDS and AML have been identified [2]. Of these, common ones are MDS/AML with RUNX1 mutations, ETV6 mutations, ANKRD26 and DDX41 mutations [2]. The reported neoplasms associated with DDX41 mutations include MDS-MLD, MDS-EB, and MDS with isolated del(5q), and they appear to have a long latency [49]. Cases with RUNX1 mutations have monoallelic germline RUNX1 mutations and have a bleeding tendency out of proportion to the platelet counts [50]. The median patient age is lower at 33 years and they exhibit the phenomenon of anticipation with the disease manifesting at an earlier age in the subsequent generations [51, 52]. The other myeloid neoplasms with germline predisposition may have ANKRD26 or ETV6 mutations [2]. Of the cases associated with organ dysfunction, germline GATA2 mutations are very interesting as they can present with 4 syndromes—MonoMAC syndrome, Emberger syndrome with a predisposition to MDS, familial MDS/AML, and dendritic cell, monocyte, B- and NK-lymphoid (DCML) deficiency with vulnerability to viral infections [53, 54]. The patients may present with MDS at a median age of 29 years, and MDS may be the first manifestation of the disease [55]. GATA2 mutations have been found in 5% cases of RCC and were associated with monosomy 7 or trisomy 8. If all childhood MDS cases are considered, GATA2 mutations are seen in ~15% of advanced and ~7% of all MDS cases. Bone marrow features in such cases include marrow hypocellularity, multilineage dysplasia with dysmegakaryopoiesis and reticulin fibrosis [56]. A clue to detection is an almost complete absence of monocytes, B cells, and NK cells on flow cytometry [53, 54, 57].
These disorders should be considered in individuals presenting with MDS/acute leukemia if they have either (a) a personal history of multiple cancers or (b) pre-existent thrombocytopenia, bleeding tendency or macrocytosis or (c) a first/second-degree relative with a hematological malignancy or (d) first/second-degree relative with a solid tumor consistent with germ line predisposition such as sarcoma, early-onset breast cancer at <50 years of age or brain tumors or (e) abnormal nails or skin pigmentation, oral leukoplakia, idiopathic pulmonary fibrosis, unexplained liver disease, lymphoedema, atypical infections, immune deficiencies, congenital limb anomalies, or short stature either in the patient or a first/second-degree relative or (f) failure of mobilization of a related donor using standard protocol or if such a donor is being considered and the patient meets any of the criteria from a to e [2, 58].
Recognition of these disorders is important for the treatment, family counseling, and anticipating other issues that might arise later in the course of the disease.
7 Determining Prognosis in MDS
Prognosis in MDS was determined using various prognostic scoring systems. The most used was International Prognostic Scoring System (IPSS) that was derived from cases classified according to FAB classification and included patients of CMML. It could be applied only to patients at first presentation and included categories of number of cytopenias, blast percentage, and karyotype [7]. After the WHO 2001 classification, a new prognostic scoring system called WHO classification-based prognostic scoring system (WPSS) that incorporated WHO classification subtype, karyotype and transfusion requirement was validated in 2005 [59].
In 2012, Greenberg et al. analyzed over 7000 cases of MDS to derive a better prognostic system that could differentiate five different prognostic categories. The cytogenetic risk groups were expanded from three to five categories. Taking cytogenetics, BM blast percentage, hemoglobin, neutrophil count and platelet counts, Revised International Prognostic Scoring System (R-IPSS) was devised and is given in Table 9.5 [8]. These risk categories correlate both with better survival and also predict evolution to AML. R-IPSS has shown a very good correlation with WPSS in a large study [60]. The WHO 2017 revised classification has not lowered the blast threshold to ≤2% for low-risk MDS as the reproducibility would be low [2, 15, 16].
Additional scoring system for low-grade MDS was proposed by M.D. Anderson cancer center as M.D. Anderson Lower-Risk MDS Prognostic Scoring System (MDA-LR). This system incorporates BM blast percentage, cytogenetics, hemoglobin, platelet count, and patient age [61].
8 Flow Cytometry in MDS
Flow cytometry in MDS has been studied extensively. The aberrant maturational patterns on granulocytes are abnormal CD11b-CD16, abnormal CD13-CD16, abnormal CD11b-CD13 patterns while on monocytes, CD11b-HLADR pattern is most frequently abnormal. A reduction in normally expressed antigen like CD10 on granulocytes and CD33 on monocytes is also considered as an abnormality [62, 63]. The second set of abnormalities pertains to aberrant antigen expression like CD7, CD2, CD56, and CD5 on either granulocyte, monocytes, or myeloblasts [39, 63]. A different approach was utilized by Ogata et al. who limited the study to myeloblasts and B-cell progenitors in low-grade MDS patients. Their study explored percentage of CD34 positive myeloblasts, percentage of CD34 positive B-cell progenitors in all CD34 positive cells, lymphocyte/myeloblast CD45 mean fluorescent intensity, and granulocyte/lymphocyte SSC peak channel ratio to come to the Ogata score. A score of ≥2 is associated with MDS [37]. This Ogata mini-panel has a high positive predictive value and specificity for MDS at ~90% but the sensitivity and negative predictive value is relatively lower at ~70% to identify low-grade MDS and differentiate them from non-clonal cytopenias [38].
Flow cytometry has been applied extensively to MDS but is still not considered mandatory in a patient’s evaluation as there is a lack of standardization in the panels used. An attempt to bring about this standardization was taken up by European leukemia Net with the first guideline in 2012 [64] and the most recent in 2014 [65]. These guidelines require ≥3 abnormalities in the set of markers affecting granulocytic or monocytic maturation and also the Ogata parameters. Flow cytometry findings if studied should always be reported as a part of an integrated report incorporating morphology and cytogenetic data [65].
9 Genetic Landscape of MDS
Over the last 5 years, there has been a massive surge in publications pertaining to mutations in MDS using next generation sequencing (NGS) [17,18,19, 34, 66,67,68,69,70,71]. The mutations described affect the epigenetic regulation and spliceosome machinery, and others affect the cohesin complex while some are the mutations of the transcription factors [66, 67]. Using NGS, mutations have been discovered in ~90% of all MDS cases. The epigenetic pathway comprises of two main subdivisions—the CpG islands and hypermethylation and the histone modification. The methylation pathway is controlled by the methyltransferase DNMT3A and DNA hydroxymethylation genes TET2, IDH1, and IDH2. Histone pathway comprises genes EZH2, ASXL1, and UTX. The transcription factor mutations affect RUNX1, ETV6, GATA2, and PHF6. Kinase signaling mutations affect KRAS, NRAS, JAK2, and CBL. Cohesin complex mutations occur in STAG2, SMC3, and RAD1 genes [66,67,68]. Mutations in the epigenetic regulators occur in ~45% of all cases of MDS while spliceosome pathway is affected in ~50% of all cases of MDS. About 25% patients exhibit mutations both in the spliceosome machinery and in the epigenetic pathway [69]. TP53 is affected in ~5% cases and is consistently associated with a poor prognosis [69]. TP53 mutations are also associated with complex karyotype, monosomies, and abnormalities of chromosome 7 [70]. Patients of MDS with isolated del(5q) may also harbor p53 mutations at diagnosis and such patients show a higher rate of progression in lenalidomide therapy. Even subclonal TP53 mutations impact prognosis and in the setting of del(5q), even IHC has been used to pick up TP53 mutations using a cutoff of ≥2% positive cells. This cutoff correlated with TP53 mutations detected by NGS could predict evolution to AML and was associated with lower overall survival [34]. Therefore, testing for TP53 in patients with del(5q), a low or intermediate-1 IPSS score has been recommended by European Leukemia Net guidelines in 2013 as these patients may not perform well on lenalidomide therapy [72].
Patients with 3 or more than 3 driver mutations have a lower leukemia-free survival than patients with 0–2 mutations. This impact on leukemia-free survival is regardless of whether the mutation is subclonal or clonal [66]. Mutations affecting TP53, ASXL1, RUNX1, ETV6, and EZH2 have a negative impact on overall survival even in very low risk, low-risk, and intermediate R-IPSS risk categories [70]. A few papers have explored the impact of these mutations with response to hypomethylating agents. The most data exists for TET2 mutations as a predictor of better response to hypomethylating agent therapy [71, 73, 74]. In one series, patients who were TET2+/ASXL1 negative were shown to have the best chance of responding to hypomethylating agents [71]. These mutations also affect overall survival in patients who undergo stem cell transplantation. In a series of ~87 patients who underwent stem cell transplantation, ~46% patients had mutations in TP53, TET2 and DNMT3A mutations, and the overall survival in these patients was ~19% compared to ~59% in patients who lacked these mutations. Among these mutations, TP53 had the worst impact on overall survival [68]. In contrast, SF3B1 mutations are associated with good overall survival and fewer cytopenias [17,18,19]. These mutations are strongly associated with RS, and SF3B1 mutations are the only ones that have been incorporated in WHO 2017 classification to classify a patient as MDS-RS-SLD and MDS-RS-MLD in presence of 5–<15% RS [2]. In addition, these are also a target for small molecule inhibitors like luspatercept that are in trial and have shown an excellent response if a patient shows the SF3B1 mutation [75].
Since these mutations have also been described in normal individuals without MDS [Clonal hematopoiesis of indeterminate potential (CHIP)] [76,77,78,79], the presence of these alone is not sufficient to classify a patient as MDS. This is also applicable to patients who have unexplained cytopenias and do not meet the diagnostic criteria for MDS [2, 80]. With the advent of NGS, three large series of patients were found to have age-related clonal hematopoiesis designated as CHIP [76,77,78]. This was found to be associated with all-cause mortality but all patients do not progress to MDS or AML.
Idiopathic cytopenia of undetermined significance (ICUS): The term ICUS was proposed for those patients in whom a diagnosis of MDS could not be established but is possible. An individual case can be classified as ICUS if there are cytopenias including hemoglobin of <11 g/dL, ANC of <1.5 × 109/L, and platelet count of <150 × 109/L that persist for a minimum of 6 months, do not meet diagnostic criteria for MDS and cannot be explained by any other possible causes. The patient requires extensive evaluation to establish this diagnosis. There is a subset of ICUS patients who can be shown to have clonal hematopoiesis if genetic mutations can be demonstrated [80]. These cases can be called as clonal cytopenia of undetermined significance (CCUS) [81]. It is understandable that with the wide application of newer tools like flow cytometry and application of NGS, many cases of ICUS would move to categories of MDS and CCUS. Based on the presence of cytopenias, clonality, BM blast percentage, and dysplasia, the spectrum of these disorders and MDS is given in Table 9.6.
10 Conclusions
The WHO 2017 classification has revamped MDS and each entity is being described as MDS with rather than “refractory anemia” or “refractory cytopenia”. There have been important changes specially pertaining to MDS-RS-SLD, and there has been a re-recognition of the entity of MDS-RS-MLD which derives from the earlier RCMD-RS in WHO 2001 classification. This has been possible due to incorporation of SF3B1 mutations for identification of these categories if there are 5–<15% RS. Another important change has been inclusion of one additional chromosomal anomaly in del(5q) as long as it is not −7 or del(7q). Minor changes are that PB blasts ~1% have to be documented on two separate occasions if considering a diagnosis of MDS-U. In addition, the entity of acute erythroleukemia has been abolished and most of these cases would now be classified as MDS. There is now a recognition that many myeloid neoplasms with germline mutations exist and that these have an important impact on patient outcome. Flow cytometry although not mandatory to the patient evaluation in MDS should be considered especially in patients with low-grade MDS lacking RS. There has been a massive surge in the genetic knowledge of MDS with the advent of NGS. This information has an impact on prognosis and possibly on response to hypomethylating agent therapy and may form a part of every patient’s evaluation if the cost of the testing reduces in the future. The advent of NGS has also led to the discovery of CHIP adding to the complexity associated around MDS.
References
Cazzola M, Malcovati L. Myelodysplastic syndromes—coping with ineffective hematopoiesis. N Engl J Med. 2005;352:536–8.
Swerdlow SH, Campo E, Harris NL, et al., editors. WHO classification of tumours of haematopoietic and lymphoid tissues. Revised 4th ed. Lyon: IARC; 2017.
Hamblin T. Clinical features of MDS. Leuk Res. 1992;16:89–93.
Bennett JM, Catovsky D, Daniel MT, et al. Proposals for the classification of the myelodysplastic syndromes. Br J Haematol. 1982;51:189–99.
Jaffe ES, Harris NL, Stein H, Vardiman JW, editors. World Health Organization classification of Tumours: pathology and genetics of tumours of haematopoietic and lymphoid tissues. Lyon: IARC; 2001.
Swerdlow SH, Campo E, Harris NL, et al., editors. WHO classification of tumours of haematopoietic and lymphoid tissues. Lyon: IARC; 2008.
Greenberg P, Cox C, Le Beau MM, et al. International scoring system for evaluating prognosis in myelodysplastic syndromes. Blood. 1997;89:2079–88.
Greenberg PL, Tuechler H, Schanz J, et al. Revised international prognostic scoring system for myelodysplastic syndromes. Blood. 2012;120:2454–65.
Verburgh E, Achten R, Louw VJ, et al. A new disease categorization of low-grade myelodysplastic syndromes based on the expression of cytopenia and dysplasia in one versus more than one lineage improves on the WHO classification. Leukemia. 2007;21:668–77.
Parmentier S, Schetelig J, Lorenz K, Kramer M, Ireland R, Schuler U, et al. Assessment of dysplastic hematopoiesis: lessons from healthy bone marrow donors. Haematologica. 2012;97(5):723–30.
Bain BJ, Clark DM, Wilkins B. Bone marrow pathology. 4th ed. Hoboken, NJ: Wiley-Blackwell; 2010.
Bain BJ. Leukaemia diagnosis. 4th ed. Hoboken, NJ: Wiley-Blackwell; 2010.
Ramos F, Fernandez-Ferrero S, Suarez D, Barbon M, Rodriguez JA, Gil S, et al. Myelodysplastic syndrome: a search for minima diagnostic criteria. Leuk Res. 1999;23(3):283–90.
Mufti GJ, Bennett JM, Goasguen J, Bain BJ, Baumann I, Brunning R, et al. Diagnosis and classification of myelodysplastic syndrome International Working Group on Morphology of myelodysplastic syndrome (IWGM-MDS) consensus proposals for the definition and enumeration of myeloblast and ring sideroblasts. Haematologica. 2008;93:1712–7.
Arber DA, Hasserjian RP. Reclassifying myelodysplastic syndromes: what’s where in the new who and why. Hematol Am Soc Hematol Educ Prog. 2015;2015:294–8.
Arber DA, Orazi A, Hasserjian R, et al. The 2016 revision to the World Health Organization classification of myeloid neoplasms and acute leukemia. Blood. 2016;127:2391–405.
Papaemmanuil E, Cazzola M, Boultwood J, et al. Somatic SF3B1 mutation in myelodysplasia with ring sideroblasts. N Engl J Med. 2011;365(15):1384–95.
Visconte V, Makishima H, Jankowska A, et al. SF3B1, a splicing factor is frequently mutated in refractory anemia with ring sideroblasts. Leukemia. 2012 Mar;26:542–5.
Malcovati L, Karimi M, Papaemmanuil E, et al. SF3B1 mutation identifies a distinct subset of myelodysplastic syndrome with ring sideroblasts. Blood. 2015;126(2):233–41.
Pozdnyakova O, Miron PM, Tang G, et al. Cytogenetic abnormalities in a series of 1,029 patients with primary myelodysplastic syndromes: a report from the US with a focus on some undefined single chromosomal abnormalities. Cancer. 2008;113:3331–40.
Haase D, Germing U, Schanz J, Pfeilstocker M, Nosslinger T, Hildebrandt B, et al. New insights into the prognostic impact of the karyotype in MDS and correlation with subtypes: evidence from a core dataset of 2124 patients. Blood. 2007;110:4385–95.
Fenaux P, Giagounidis A, Selleslag D, et al. A randomized phase 3 study of lenalidomide versus placebo in RBC transfusion-dependent patients with low-/intermediate-1-risk myelodysplastic syndromes with del5q. Blood. 2011;118:3765–76.
List A, Dewald G, Bennett J, et al. Lenalidomide in the myelodysplastic syndrome with chromosome 5q deletion. N Engl J Med. 2006;355:1456–65.
Christiansen DH, Andersen MK, Pedersen-Bjergaard J. Mutations with loss of heterozygosity of p53 are common in therapy-related myelodysplasia and acute myeloid leukemia after exposure to alkylating agents and significantly associated with deletion or loss of 5q, a complex karyotype, and a poor prognosis. J Clin Oncol. 2001;19:1405–13.
Jädersten M, Saft L, Pellagatti A, et al. Clonal heterogeneity in the 5q-syndrome: p53 expressing progenitors prevail during lenalidomide treatment and expand at disease progression. Haematologica. 2009;94:1762–6.
Möllgård L, Saft L, Treppendahl MB, et al. Clinical effect of increasing doses of lenalidomide in high-risk myelodysplastic syndrome and acute myeloid leukemia with chromosome 5 abnormalities. Haematologica. 2011;96:963–71.
Gregg XT, Reddy V, Prchal JT. Copper deiciency masquerading as myelodysplastic syndrome. Blood. 2002;100:1493–5.
Fong T, Vij R, Vijayan A, et al. Copper deficiency: an important consideration in the differential diagnosis of myelodysplastic syndrome. Haematologica. 2007;92:1429–30.
Halfdanarson TR, Kumar N, Li CY, et al. Hematological manifestations of copper deficiency: a retrospective review. Eur J Haematol. 2008;80:523–31.
Monte SW, Sara AM, Michael LM, et al. Zinc-induced copper deficiency: a report of three cases initially recognized on bone marrow examination. Am J Clin Pathol. 2005;123:125–31.
Kar R, Rao S, Saxena R. Myelodysplastic syndromes: classification and prognostic scoring systems and their applicability in Indian scenario-experience from a tertiary care center. Hematology. 2009;14:145–9.
Braun T, Fenaux P. Myelodysplastic syndromes (MDS) and autoimmune disorders (AD): cause or consequence? Best Pract Res Clin Haematol. 2013;26:327–36.
Endi W, Elizabeth B, Imran S, et al. Pseudo–Pelger-Huët anomaly induced by medications: a clinicopathologic study in comparison with myelodysplastic syndrome–related Pseudo–Pelger-Huët anomaly. Am J Clin Pathol. 2011;135:291–303.
Taegtmeyer AB, Halil O, Bell AD, et al. Neutrophil dysplasia (acquired pseudo-pelger anomaly) caused by ganciclovir. Transplantation. 2005;80:127–30.
Sharp RA, Lowe JG, Johnston RN. Anti-tuberculous drugs and sideroblastic anaemia. Br J Clin Pract. 1990;44:706–7.
Valent P, Orazzi A, Büschner G, et al. Standards and impact of hematopathology in myelodysplastic syndromes (MDS). Oncotarget. 2010;1:483–96.
Ogata K, Della Porta MG, Malcovati L, Picone C, Yokose N, Matsuda A, et al. Diagnostic utility of flow cytometry in low-grade myelodysplastic syndromes: a prospective validation study. Haematologica. 2009;94:1066–74.
Della Porta MG, Picone C, Pascutto C, Malcovati L, Tamura H, Handa H, et al. Multicenter validation of a reproducible flow cytometric score for the diagnosis of low-grade myelodysplastic syndromes: results of a European LeukemiaNET study. Haematologica. 2012;97:1209–17.
Kern W, Haferlach C, Schnittger S, Haferlach T. Clinical utility of multiparameter flow cytometry in the diagnosis of 1013 patients with suspected myelodysplastic syndrome: correlation to cytomorphology, cytogenetics, and clinical data. Cancer. 2010;116:4549–63.
Kern W, Bacher U, Haferlach C, et al. Multiparameter flow cytometry provides independent prognostic information in patients with suspected myelodysplasti syndromes: a study on 804 patients. Cytometry B Clin Cytom. 2015;88:154–64.
Wang SA, Pozdnyakova O, Jorgensen JL, et al. Detection of paroxysmal nocturnal hemoglobinuria clones in patients with myelodysplastic syndromes and related bone marrow diseases, with emphasis on diagnostic pitfalls and caveats. Haematologica. 2009;94:29–37.
Bennett JM, Catovsky D, Daniel MT, et al. Proposals for the classification of the acute leukemias. French-American-british (FAB) co-operative group. Br J Haematol. 1976;33:451–8.
Wang SA, Patel KP, Pozdnyakova O, et al. Acute erythroid leukemia with <20% bone marrow blasts is clinically and biologically similar to myelodysplastic syndrome with excess blasts. Mod Pathol. 2016;29:1221–31.
Calvo X, Arenillas L, Luno E, et al. Erythroleukemia shares biological features and outcome with myelodysplastic syndromes with excess blasts: a rationale for its inclusion into future classifications of myelodysplastic syndromes. Mod Pathol. 2016;29:1541–51.
Santos FP, Faderl S, Garcia-Manero G, et al. Adult acute erythroleukemia: an analysis of 91 patients treated at a single institution. Leukemia. 2009;23(12):2275–80.
Bacher U, Haferlach C, Alpermann T, Kern W, Schnittger S, Haferlach T. Comparison of genetic and clinical aspects in patients with acute myeloid leukemia and myelodysplastic syndromes all with more than 50% of bone marrow erythropoietic cells. Haematologica. 2011;96(9):1284–92.
Hasserjian RP, Zuo Z, Garcia C, et al. Acute erythroid leukemia: a reassessment using criteria refined in the 2008 WHO classification. Blood. 2010;115(10):1985–92.
Bacher U, Haferlach C, Alpermann T, et al. Comparison of genetic and clinical aspects in patients with acute myeloid leukemia and myelodysplastic syndromes all with more than 50% of bone marrow erythropoietic cells. Haematologica. 2011;96:1284–92.
Polprasert C, Schulze I, Sekeres MA, et al. Inherited and somatic defects in DDX41 in myeloid neoplasms. Cancer Cell. 2015;27:658–70.
Owen C, Barnett M, Fitzgibbon J. Familial myelodysplasia and acute myeloid leukaemia—a review. Br J Haematol. 2015;140:123–32.
Nickels EM, Soodalter J, Churpek JE, et al. Recognizing familial myeloid leukemia in adults. Ther Adv Hematol. 2013;4:254–69.
West AH, Godley LA, Churpek JE. Familial myelodysplastic syndrome/acute leukemia syndromes: a review and utility for translational investigations. Ann N Y Acad Sci. 2014;1310:111–8.
Collin M, Dickinson R, Bigley V. Haematopoietic and immune defects associated with GATA2 mutation. Br J Haematol. 2015;169:173–87.
Hsu AP, McReynolds L, Holland SM. GATA2 deficiency. Curr Opin Allergy Clin Immunol. 2015;15:104–9.
Micol JB, Abdel-Wahab O. Collaborating constitutive and somatic genetic events in myeloid malignancies: ASXL 1 mutations in patients with germline GATA2 mutations. Haematologica. 2014;99:201–3.
Wlodarski MW, Hirabayashi S, Pastor V, et al. Prevalence, clinical characteristics, and prognosis of GATA2-related myelodysplastic syndromes in children and adolescents. Blood. 2016;127:1387–97.
Calvo KR, Vinh DC, Marie I, et al. Myelodysplasia in autosomal dominant and sporadic monocytopenia immunodeficiency syndrome: diagnostic features and clinical implications. Haematologica. 2011;96:221–5.
Churpek JE, Lorenz R, Nedumgottil S, et al. Proposal for the clinical detection and management of patients and their family members with familial myelodysplastic syndrome/acute leukemia predisposition syndromes. Leuk Lymphoma. 2013;54:28–35.
Malcovati L, Germing U, Kuendgen A, et al. Time-dependent prognostic scoring system for predicting survival and leukemic evolution in myelodysplastic syndromes. J Clin Oncol. 2007;25:3503–10.
Della Porta MG, Tuechler H, Malcovati L, et al. Validation of WHO classification-based Prognostic Scoring System (WPSS) for myelodysplastic syndromes and comparison with the revised International Prognostic Scoring System (IPSS-R). A study of the International Working Group for Prognosis in Myelodysplasia (IWG-PM). Leukemia. 2015;29:1502–13.
Garcia-Manero G, Shan J, Faderl S, et al. A prognostic score for patients with lower risk myelodysplastic syndrome. Leukemia. 2008;22:538–43.
Bowen KL, Davis BH. Abnormal patterns of expression of CD16 (FcR-III) and CD11b (CRIII) antigens by developing neutrophils in the bone marrow of patients with myelodysplastic syndrome. Lab Hematol. 1997;3:292–8.
Stetler-Stevenson M, Arthur DC, Jabbour N, Xie XY, Molldrem J, Barrett AJ, et al. Diagnostic utility of flow cytometric immunophenotyping in myelodysplastic syndrome. Blood. 2001;98:979–87.
Westers TM, Ireland R, Kern W, Alhan C, Balleisen JS, Bettelheim P, et al. Standardization of flow cytometry in myelodysplastic syndromes: a report from an international consortium and the European LeukemiaNet Working Group. Leukemia. 2012;26(7):1730–41.
Porwit A, van de Loosdrecht AA, Bettelheim P, Brodersen LE, Burbury K, Cremers E, et al. Revisiting guidelines for integration of flow cytometry results in the WHO classification of myelodysplastic syndromes-proposal from the International/European LeukemiaNet Working Group for Flow Cytometry in MDS. Leukemia. 2014;28(9):1793–8.
Papaemmanuil E, Gerstung M, Malcovati L, et al. Clinical and biological implications of driver mutations in myelodysplastic syndromes. Blood. 2013;122:3616–27.
Haferlach T, Nagata Y, Grossmann V, et al. Landscape of genetic lesions in 944 patients with myelodysplastic syndromes. Leukemia. 2014;28:241–7.
Bejar R, Stevenson KE, Caughey B, et al. Somatic mutations predict poor outcome in patients with myelodysplastic syndrome after hematopoietic stem-cell transplantation. J Clin Oncol. 2014;32:2691–8.
Bejar R, Steensma DP. Recent developments in myelodysplastic syndromes. Blood. 2014;124:2793–803.
Bejar R, Stevenson K, Abdel-Wahab O, Galili N, Nilsson B, Garcia-Manero G, et al. Clinical effect of point mutations in myelodysplastic syndromes. N Engl J Med. 2011;364:2496–506.
Bejar R, et al. TET2 mutations predict response to hypomethylating agents in myelodysplastic syndrome patients. Blood. 2014;124:2705–12.
Malcovati L, Hellström-Lindberg E, Bowen D, et al. Diagnosis and treatment of primary myelodysplastic syndromes in adults: recommendations from the European LeukemiaNet. Blood. 2013;122:2943–64.
Itzykson R, Thepot S, Quesnel B, et al. Prognostic factors for response and overall survival in 282 patients with higher-risk myelodysplastic syndromes treated with azacitidine. Blood. 2011;117:403–11.
Traina F, Visconte V, Elson P, et al. Impact of molecular mutations on treatment response to DNMT inhibitors in myelodysplasia and related neoplasms. Leukemia. 2014;28:78–87.
Platzbecker U, Germing U, Götze KS, et al. Luspatercept for the treatment of anaemia in patients with lower-risk myelodysplastic syndromes (PACE-MDS): a multicentre, open-label phase 2 dose-finding study with long-term extension study. Lancet Oncol. 2017;18:1338–47.
Xie M, Lu C, Wang J, et al. Age-related mutations associated with clonal hematopoietic expansion and malignancies. Nat Med. 2014;20:1472–8.
Genovese G, Kahler AK, Handsaker RE, et al. Clonal hematopoiesis and blood-cancer risk inferred from blood DNA sequence. N Engl J Med. 2014;371(26):2477–87.
Jaiswal S, Fontanillas P, Flannick J, et al. Age-related clonal hematopoiesis associated with adverse outcomes. N Engl J Med. 2014;371(26):2488–98.
Kwok B, Hall JM, Witte JS, et al. MDS associated somatic mutations and clonal hematopoiesis are common in idiopathic cytopenias of undetermined significance. Blood. 2015;126(21):2355–61.
Valent P, Hprny H-P, Bennett JM, et al. Definitions and standards in the diagnosis and treatment of the myelodysplastic syndromes: consensus statements and report from a working conference. Leuk Res. 2007;31:727–36.
Steensma DP, Bejar R, Jaiswal S, et al. Clonal hematopoiesis of indeterminate potential and its distinction from myelodysplastic syndromes. Blood. 2015;126(1):9–16.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter
Dass, J., Kotwal, J. (2019). Myelodysplastic Syndrome: An Overview. In: Saxena, R., Pati, H. (eds) Hematopathology. Springer, Singapore. https://doi.org/10.1007/978-981-13-7713-6_9
Download citation
DOI: https://doi.org/10.1007/978-981-13-7713-6_9
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-13-7712-9
Online ISBN: 978-981-13-7713-6
eBook Packages: MedicineMedicine (R0)