Abstract
The myelodysplastic syndromes (MDS) are a heterogeneous group of acquired clonal bone marrow disorders characterized by varying degrees of morphological and functional cellular abnormalities involving one or more cell lines. MDS is characterized by impaired, ineffective, proliferation and maturation of hematopoietic progenitor cells resulting in symptomatic anemia, leukopenia, or thrombocytopenia. The clinical course is variable, ranging from a chronic, stable, mildly symptomatic disorder to a disease that compromises the patients quality of life rapidly progresses to acute myeloid leukemia (AML). Infections and/or bleeding are the most frequent causes of morbidity and mortality in patients with MDS. MDS shares many clinical, cytogenetic, and laboratory features with other hematologic disorders including aplastic anemia, the myeloproliferative neoplasms and the acute leukemias. The World Health Organization (WHO) classification of MDS continues to evolve, incorporating clinical, cytogenetic, and molecular studies in an attempt to define MDS and separate it from the myeloproliferative neoplasms, hypoproliferative disorders and the acute leukemias. Finally, secondary causes of bone marrow failure and certain hereditary syndromes can masquerade as MDS. The WHO updated and modified the diagnosis and classification of MDS in 2016. The new classification is controversial and attempts to incorporate new mutational studies while continuing to support the role of morphology in the diagnosis and classification of MDS. Patients with MDS may present with clinical and laboratory features suggestive of reactive, autoimmune or other malignant stem cell disorders. In many instances, the diagnosis of MDS is based on the exclusion of other disorders associated with dysplasia and ineffective hematopoiesis. This chapter discusses the pathogenesis, clinical manifestations, classification, prognostic variables, and specific treatments for MDS.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
The myelodysplastic syndromes (MDS) are a heterogeneous group of clonal stem cell disorders characterized by impaired, and/or ineffective, proliferation and maturation of hematopoietic progenitor cells resulting in symptomatic anemia, leukopenia, or thrombocytopenia. The clinical course is very variable, ranging from a chronic, stable, mildly symptomatic disorder to a malignancy that rapidly progresses to AML. Morphological and functional cellular abnormalities involving one or more cell lines are common resulting in infections and/or bleeding. The complications from MDS and its treatment remain the major cause of morbidity and mortality. MDS shares many clinical, cytogenetic, and laboratory features with aplastic anemia, hypoplastic anemias, the myeloproliferative neoplasms, and the acute leukemias. The updated WHO classification attempts to define the diagnosis of MDS and separate it from the myeloproliferative neoplasms, reactive and secondary causes of hypoproliferative disorders and the acute leukemias. Patients with MDS may present with clinical and laboratory features suggestive of a reactive, autoimmune or other malignant stem cell disorder. Therefore, in many instances, the diagnosis of MDS is based on the exclusion of other disorders associated with dysplasia and impaired or ineffective hematopoiesis.
MDS is a progressive clonal disorder and the diagnostic studies and the initial evaluations are similar to those used to define other neoplastic and non-neoplastic stem cell disorders. However, the clinical course, prognosis, and treatment approach for a patient with a MDS is different from the other neoplastic stem cell disorders. The bone marrow and peripheral blood abnormalities in MDS can be subtle and require the cooperative efforts of pathologists, cytogeneticists, and clinicians to diagnosis, classify and define prognosis. MDS is one of most common hematologic malignancies in older populations and treatments remain controversial and limited for many patients. Treatments for many patients should be individualized and tailored to the MDS subtype, patient’s age, comorbidities, and other prognostic variables.
Myelodysplasia , derived from the Greek and meaning morphological abnormality of the bone marrow, is not a new disease but it has only recently been assigned as a separate category in the classification of malignant hematopoietic disorders based on specific diagnostic criteria. The initial reports identified elderly patients with progressive cytopenias, morphologically abnormal cells, and a propensity to progress to an acute leukemia. Terms such as smoldering leukemia, or preleukemia were used to describe this condition, reflecting that patients with MDS did not meet the usual criteria of acute leukemia but presented with a syndrome which included a hypercellular bone marrow with increased blast forms and dysplastic changes in one or more cell lines. In MDS, as in the myeloproliferative neoplasms and acute leukemias an oncogenic transforming event occurs at the level of the myeloid or pluripotential stem cell. Cytogenetic studies were first to identify the genetic alterations in MDS and are important in establishing the diagnosis and prognosis in MDS. More recently numerous specific gene mutations have been identified in MDS associated genes that may define prognosis and impact treatment. While many patients with MDS have features suggestive of an early, smoldering leukemia, and rapidly evolve into one of the myeloid leukemias, most patients do not evolve into AML but die as a result of the MDS or its treatment [1, 2]. MDS therefore should not be considered as a preleukemic disorder, but as a separate neoplastic disease of the hematopoietic pluripotential stem cells that is characterized by a progressive clonal proliferation of abnormal precursors that demonstrate both impaired maturation and ineffective proliferation. The separation of MDS from AML, myeloproliferative neoplasms, aplastic anemia, and reactive disorders continues to be problematic, which is reflected in the evolving and at times inconsistent classification systems, prognostic models, and treatment options. A proposed revised 2016 WHO classification refines the morphologic interpretation and assessment of cytopenias addresses, and applies new diagnostic terminology for MDS. The WHO classification still relies mainly on the degree of dysplasia and the percent of blasts for disease classification and specific cytopenias now have only a minor impact on the MDS classification [3, 4]. Moreover the morphologic dysplasia may not correlate with the lineage specific cytopenias. Therefore the WHO has removed terms such a refractory anemia or refractory cytopenia and replaced it with the suffix Myelodysplastic Syndrome followed by the specific abnormality. The WHO also attempted to define and incorporate identified gene mutations associated with MDS and address the controversy and limitations of incorporating distinct mutations in the new proposed classification criteria. The WHO noted that that identification of dysplasia is subjective and may vary even among experienced hematopathologists [3]. Therefore when the dysplasia is subtle or limited to a single lineage it is important to consider other possible reactive and non-neoplastic causes of the dysplasia prior to making the diagnosis of MDS.
Pathogenesis and Etiology
MDS is one of the most common hematologic malignancies in western countries with an overall incidence of 3.5–12.6/100,000/year. The median age of MDS patients in western countries is 73 years, at the time of diagnosis, and the incidence increases with age. In individuals over the age of 70 years the incidence is between 15–50/100,000/year and is increasing with the aging population [5, 6]. However, the overall incidence of MDS is likely much higher due to difficulties in reporting, diagnosis, and classification [4]. The incidence of MDS is higher in men than women with the exception of the del (5q), which has a marked female predominance. In Asian countries, notably Japan and China, the median age of patients with MDS is between 40–50 years, some two decades earlier than in western countries [5, 7, 8]. The reason for the differences in the epidemiology of MDS in Japan and China is unclear but may, in part, reflect the variability and limitations of population-based databases. However, the role of environmental factors, industrial solvents and agricultural chemicals, and smoking may contribute to the observed 20-year differences in the epidemiology of MDS [9, 10].
Environmental agents have been implicated in the etiology of MDS. In case-controlled studies, there is an association between MDS and cigarette smoking, exposure to benzene, petroleum products, organic solvents, fertilizers, pesticides, and herbicides [10]. The associated between smoking and MDS may reflect that cigarette smoke contains benzene and other suspected carcinogens [9]. The MDS risk is related to the intensity and duration of smoking and may persist for up to 15 years after cessation of smoking [9, 10]. Ionizing radiation exposure is associated with a significant increase risk for the development of MDS. In the Nagasaki atomic bomb survivors risk for developing MDS was greater in individuals exposed at a younger age and occurred 40–60 years after exposure. In contrast to the reported radiation induced leukemia in Nagasaki which occurred 10–15 years after the exposure. The long latency may reflect the proposed multistep pathogenesis model for the development of MDS with age related changes and genetic instability associated with the prior radiation exposure [11]. In epidemiologic studies there was a linear radiation dose response for the development of MDS in Nagasaki atomic bomb survivors 40–60 years after exposure.
MDS is characterized by dysplastic, ineffective hematopoiesis. The bone marrow is typically hypercellular for the patient’s age with peripheral cytopenias and an increase in hematopoietic precursors in the bone marrow and/or peripheral blood. The clonal origin of MDS has been confirmed by isozyme analysis of glucose 6 phosphate dehydrogenase (G6PD) in heterozygous females and more recently by molecular analysis of other loci such as the androgen receptor gene [8, 12]. Cytogenetic analysis has demonstrated recurrent genetic alterations that are prognostically important and next generation high throughput gene sequencing has defined a number of mutated genes in MDS [12] (Table 23.1). The appearance of clonal gene mutations arise in hematopoietic stem cells and appear to be early events that are associated with clonal dominance. Specific gene mutations and the cytogenetic abnormalities can be demonstrated before the detections of morphological dysplasia or the clinical findings of MDS [13, 14]. The initial cytogenetic and somatic gene mutations are part of a multistep process that predisposes the pluripotential stem cell to secondary genetic events and the development of MDS [14]. Epigenetic alterations in one or more oncogenes including in the aberrant expression of specific tumor promotor, tumor suppressor, and transcription factor genes are associated with the progression of MDS [15, 16]. The diagnostic and prognostic role of specific gene mutations and aberrant methylation of epigenetic regulators, however, is still unclear. MDS progression is characterized by a progressive increase in chromosomal instability that leads to the development of aberrant clones and the emergence of complex karyotypes. Telomeres , noncoding repeated sequences at the ends of chromosomes, that function to stabilize chromosomes and prevent chromosomal breaks and aberrations critical in the maintaining normal hematopoiesis and are postulated to play a role in the progressive chromosomal instability in MDS [17]. Each somatic cell division is associated with loss of telomere length and the cumulative effects of telomere shortening leads to cell senescence. The shortening of telomeres is noted in patients with progressive, advanced MDS, with multiple complex karyotypic abnormalities. The genetic instability associated with shortening of telomeres may contribute, in part, to the leukemic transformation in some patients with MDS [17, 18]. Moreover, the alteration of telomere dynamics in hematopoietic stem cells may precede the clinical development of MDS [19]. However, the majority of patients that develop MDS are greater than 70 years old and loss of telomere length and function is part of the normal aging process [19].
The hematopoietic microenvironment may also play a role in the pathophysiology of MDS [20]. MDS is characterized by ineffective hematopoiesis and the increased susceptibility of hematopoietic progenitors to apoptosis. The bone marrow stroma responds to signals from the hematopoietic cells and is abnormal in some patients with MDS. Abnormalities of the bone marrow microenvironment and the hematopoietic stem cell niche may affect and promote apoptosis and telomere shortening in clonal hematopoietic cells [21]. The overexpression of TNF-a produced by MDS mononuclear cells can inhibit the growth of residual normal hematopoiesis and lead to increased cell death of normal precursors, and a growth advantage for the abnormal MDS precursors. The bone marrow in MDS patients has increased apoptotic cells which is most marked in the less proliferative, better prognosis, low risk subtypes of MDS.
Genetic, environmental, and exposure factors have been associated with an increased risk for the development of MDS [22]. Inherited constitutional genetic defects have been associated with up to 30% of children with MDS and related myeloproliferative disorders. Children with Shwachman–Diamond syndrome, Fanconi anemia, dyskeratosis congenital, and neurofibromatosis type 1 have constitutional genetic defects that are associated with the increased risk for the development of both MDS and AML [25, 26].
Mutations of specific genes mediating DNA repair appear to predispose to the acquisition of secondary cytogenetic abnormalities that can lead to the development of MDS [23]. Somatic mutations occur in the majority of patients and may be associated with specific clinical features. Specific point mutations were associated with the clinical phenotype, specific cytopenias, disease progression, and overall survival. Genes encoding runt-related transcription factor 1 (RUNX1), tumor protein p53 (TP53), and neuroblastoma RAS viral oncogene homologue (NRAS) are associated with thrombocytopenia and an increased percent of bone marrow blast forms [23, 24]. Point mutations resulting in the activation of the specific genes (TP53, EZH2, ETV6, RUNX1, and ASXL1) are independent markers of poor prognosis and may, in part, explain the clinical heterogeneity of MDS. The TET family of genes maps to chromosome 4q24 and modulate hypomethylation by catalyzing an intermediate of DNA methylation that block the formation of silencing proteins to methylated DNA [13]. Mutations of the TET2 gene are found in a number of myeloid neoplasms including AML, MPNs, and MDS. In MDS TET2 mutation is the most frequent gene mutation occurring 20–30% of patients. Mutations of TET2 associated with loss of function may result in increased methylation and silencing of genes that are normally expressed. However, the prognostic impact of TET2 mutations on survival in MDS is unclear. The TET2 mutation is associated with a number of additional gene mutations and therefore may be one of the initial mutational events MDS. Recurrent mutations of epigenetic regulators, genes encoding the splicing machinery, spliceosomal components, and transcription factors are not unique to MDS and are found in a number of other myeloid neoplasms and occur across a spectrum of cytogenetic subgroups. It is controversial if these gene mutations are the primary events in MDS and are diagnostic and prognostic markers that are independent of other abnormalities [23, 24]. The frequency of the recurrent somatic mutations in MDS patients increases with progression of the disease and the subsequent development of secondary cytogenetic events and AML [25]. However, the etiological role of each of the somatic point mutations in the development of and progression of MDS is controversial and it is unclear if these mutations just reflect the genetic instability of the abnormal clone and its propensity to develop random genetic mutations [26, 27]. Moreover, similar somatic mutations have been noted in older normal individuals without evidence of MDS [27,28,29]. Somatic mutations resulting in clonal hematopoietic cells are detected in greater than 10% of persons older than 70 years of age and the incidence of somatic mutations increases with age. These MDS associated acquired clonal mutations occur in hematopoietic cells of healthy older persons with normal blood counts and without evidence of dysplasia [29]. The presence of somatic mutations may confer an increased risk in the individual for the subsequent development of a hematological malignancy and are associated with an all cause-increased mortality [30–32]. The term “Clonal Hematopoiesis of Indeterminate Potential “(CHIP) is used describe these acquired clonal somatic mutations which are associated with hematologic malignancies in apparently healthy older individuals without any clinical features of a MDS or any myeloid malignancy. The natural history of individuals with CHIP is unclear and these persons should not be considered to have a malignancy. The revised 2016 WHO classifications addresses the controversy associated with somatic mutations and notes that the presence clonal somatic mutation alone, without other clinical manifestations of MDS, is not sufficient to make the diagnosis of MDS. While CHIP may represent a pre - malignant myeloid conditions, similar to monoclonal gammopathy of undetermined significance (MGUS) and multiple myeloma, the natural history of individuals with CHIP is not clearly defined. Testing for somatic mutations in healthy individuals should not part of routine clinical practice.
MDS patients have defects in a number of signal transduction pathways that appear to be related to the evolving ineffective hematopoiesis and epigenetic changes [33, 34]. These acquired abnormalities may contribute to the further dysregulation of progenitor cell cycle kinetics, response to cytokines, and the maintenance of DNA integrity, which results in progressive genetic instability. Abnormal regulation of microRNAs (miRNA) which function as epigenetic regulators of gene expression may play a role in the pathogenesis of MDS and alterations in miRNAs may be independent markers of prognosis [24].
MDS is associated with a number of immunoregulatory abnormalities including the development of autoantibodies and monoclonal gammopathies [35]. In subsets of patients with MDS, autoreactive T-cell clones are present that inhibit autologous erythroid and granulocytic colony growth. T-cell-mediated suppression of bone marrow growth and maturation is an important development of aplastic anemia and the hypoplastic variant of MDS [35, 36]. The incidence of MDS is increased in patients with autoimmune disorders and autoimmune disorders are more common in patients with MDS. The presence of autoimmune disorders is associated with a better overall survival and less frequent transformation to AML, The immunoregulatory abnormalities may also explain the response to immunosuppressive therapy in selected patients with MDS.
There are defined genetic predisposing factors in some MDS patients that relate to naturally occurring complex DNA polymorphisms in genes that mediate DNA repair and the metabolism of environmental carcinogens [37, 38]. In selected genetically predisposed individuals, MDS may arise as a result of cumulative environmental exposures and studies have linked the development of MDS and the nonfunction 609 C.T polymorphic allele of the NAD(P)Quinone oxidoreductase (NQO1) gene [40, 41]. These genes appear to play a critical role in detoxifying benzene and its metabolites. This association is controversial, but may explain the increased incidence of MDS in some patients exposed to organic solvents and benzene-containing compounds [39]. Similar controversial, but provocative results have been reported in the glutathione S-transferase (GST) genes that mediate the metabolism of cytotoxic and genotoxic agents [40].
A prior exposure to chemotherapy, especially alkylating agents and purine analogues is associated with an increased risk of MDS and AML (Table 23.2). The WHO identifies therapy-related MDS (t-MDS) as a separate category. Therapy related MDS represents approximately 10–20% of MDSs and MDS/MPNs [41]. The risk is, in part, related to the dose and duration of the cytotoxic therapy and generally occurs 3–7 years after the exposure. Patients who received combination radiation therapy and chemotherapy are at greater risk for the development of t-MDS [42]. Total body irradiation, administered as part of the preparative regimen for an autologous stem cell transplantation, is associated with an increased risk for MDS, and the combination of high-dose alkylator therapy and total body irradiation was associated with a 10–15% risk of t-MDS and secondary AML [41]. The MDS that occurs after chemotherapy, has a very poor prognosis [42]. Therapy-related MDS, is associated with deletions of chromosomes 5 and/or 7 and complex karyotypes. In contrast to the cytogenetic findings in AML, balanced cytogenetic abnormalities including translocations and inversions are rare in MDS. The cytogenetic abnormalities in MDS are important independent prognostic risk factors for overall survival and risk of the development of AML (Table 23.3). However, in the majority of patients with MDS there is no history of exposure to known mutagens, cytotoxic agents, or environmental agents and therefore the etiology of the syndrome remains idiopathic or unknown.
Diagnosis and Classification
The diagnosis and classification of MDS, similar to other myeloid malignancies, is evolving and incorporates new cytogenetic and molecular findings. The updated 2016 WHO classification attempts to addresses the heterogeneity of MDS and separates MDS from reactive processes and other malignant stem cell disorders. The revised classification refines the morphologic interpretations and addresses the influence of new genetic information in MDS diagnosis, classification and prognosis. The FAB (French–American–British) group was the first to define morphological criteria in the blood and bone marrow for the diagnosis and classification of MDS and was based only on morphology, and the percentage of blast forms in the blood and bone marrow. This classification system, although generally adopted at the time, was clinically and biologically inconsistent [43]. The separation of MDS from AML and other clonal disorders was based on an arbitrary number of blast forms. Moreover, many patients with MDS had clinical and laboratory features of AML, aplastic anemia, and myeloproliferative neoplasms which were not addressed in the FAB classification [44]. The FAB criteria also did not address the clinically important cytogenetic changes in MDS and were too variable to accurately predict prognosis, survival, or transformation to AML. The FAB classification remained as a widely accepted classification system for diagnosis of MDS for two decades. The FAB group defined five categories, of MDS based on morphologic dysplasia, cytochemical stains for iron to detect ring sideroblasts, and the percent of blast forms in the bone marrow and peripheral blood and included refractory anemia (RA), or refractory cytopenia, refractory anemia with ringed sideroblasts (RARS), refractory anemia with excess blasts (RAEB), chronic myelomonocytic leukemia (CMML), and refractory anemia with excess blasts in transformation (RAEB-T). The World Health Organization (WHO), in collaboration with the Society for Hematopathology and the European Association of Hematopathology in 2001, proposed a revision of the FAB morphological approach to the classification of MDS [45]. The WHO classification was updated in 2008 and most recently in 2016 [3, 46] (Table 23.4). The revised WHO classification attempts to combine clinical, morphologic, immunophenotypic, genetic and molecular features to define clinically and prognostically important subtypes. The current WHO classification is generally accepted and is incorporated in prognostic and treatment models of MDS.
The WHO classification included requirements for the type of specimens to be obtained, the assessment of blasts, assessment of blast lineage, and cytogenetic or mutational studies. The assessment of blasts in the peripheral blood (PB) and bone marrow (BM) should be obtained prior to any definitive therapy. Cytogenetic analysis and flow cytometry should be obtained, with additional material saved for later molecular genetic studies as needed [12]. The WHO lowered the threshold for percent of blasts to diagnose AML from 30% (FAB) to 20%. The percent of blasts should be derived from a 200-cell differential count of the peripheral blood smear and a 500-cell differential count of all nucleated bone marrow cells. The 2016 revised WHO classification changed the diagnostic criteria for myeloid neoplasms with erythroid dominance, defined as erythroid precursors ≥50% of all bone marrow cells. In the new classification the percent of blasts is based not on non-erythroid nucleated cells but on all nucleated bone marrow cells. This new criteria will result in cases previously diagnosed as the erythroid/myeloid subtype of acute erythroid leukemia to now being classified as MDS with excess blasts.
The FAB and the subsequent WHO classifications defined MDS as a clonal stem cell disorder characterized by ineffective, dysplastic hematopoiesis, with dysplasia in one or more hematopoietic cell lines and the dysplasia should be noted in >10% of cells in either the bone marrow or the blood. The WHO noted that morphological dysplasia is not specific or diagnostic of MDS and noted the difficulty in separating MDS from other disorders associated with cytopenias and dysplasia. The 2016 WHO classification recognized that dysplasia in excess of 10% may occur in some normal individuals and in other non-malignant hematologic disorders. The hematopathologist’s identification of dysplasia is also variable and not always reproducible even by expert panels [47]. The WHO classifications like the original FAB classification is based on the degree of dysplasia and percent of blast forms in the blood and bone marrow. The WHO classification noted that the cell line demonstrating the most prominent dysplasia may not correlate with the cytopenia of the most affected lineage. The 2016 WHO classification therefore changed the descriptive terms such as refractory anemia and applied the new terminology Myelodysplastic syndrome followed by the “appropriate modifiers”; single or multilineage dysplasia, ring sideroblast, excess blast or the del(5q) cytogenetic abnormality (Table 23.4). There are, however, some of he morphological abnormalities that are more characteristic of MDS and are useful in confirming the diagnosis. The neutrophil and megakaryocytic dysplastic changes are the most specific and characteristic of MDS [3, 46, 48]. In the myeloid/neutrophilic dysmyelopoiesis the presence in the peripheral blood of the acquired, pseudo, Pelger–Huët anomaly is a frequent and useful characteristic finding in the MDS. This acquired abnormality resembles the inherited Pelger–Huët anomaly , therefore the designation of pseudo, and is characterized by mature neutrophils that are hypolobated with a single lobe or two joined by a thin band of chromatin [49]. Abnormal granulopoiesis is usually evident on the peripheral smear and includes hypersegmented neutrophils, with decreased or absent cytoplasmic granules The presence of dysmegakaryopoiesis including the presence of micromegakaryocytes in the bone marrow is also very suggestive of MDS rather than a reactive process [3, 45]. The finding of micromegakaryocytes and megakaryocytes that are the size of a myeloblast with one or two abnormal small nuclei in the bone marrow is one of the most characteristic, diagnostic and recognizable morphological features in MDS.
A majority of patients with MDS are asymptomatic at presentation and are usually diagnosed when they present with an unexplained macrocytic anemia (MCV > 102) with a absolute low reticulocyte count. Anemia is the most common presenting abnormality and patients may complain of the insidious onset fatigue and progressive dyspnea on exertion. Bone pain and weight loss are uncommon. While patients may be neutropenic and have dysplastic and impaired neutrophil function, infections are unusual at presentation. The physical examination is notable for the lack of adenopathy, cutaneous lesions, prominent splenomegaly, or hepatomegaly. The diagnosis of MDS relies largely on the morphological findings in the peripheral blood and the bone marrow (Table 23.5). MDS must be differentiated from other disorders that present with abnormalities of one or more cell line including aplastic anemia, myeloproliferative neoplasms, nutritional deficiencies, and autoimmune disorders (Table 23.6). AML in elderly patients may also present with progressive pancytopenia with rare circulating blast forms [56]. The differentiation of AML with dysplasia from MDS can be difficult. Patients with acute erythroleukemia may have prominent dysplastic erythroid precursors and may initially be diagnosed with one of the MDSs. Patients with hypoplastic AML can also be confused with one of the MDS subtypes. In prospective trials of MDS up to 15% of the patients with hypoplastic MDS were later reclassified as having AML [48, 50].
The finding of a clonal cytogenetic abnormality characteristic of MDS is important in establishing the diagnosis, assessing prognosis and differentiating it from other disorders [3]. The WHO defined specific cytogenetic abnormalities, even in the absence of diagnostic morphologic dysplasia, that where sufficient to make a diagnosis of MDS (Table 23.6). In these cases the cytogenetic abnormality must be demonstrated by conventional karyotyping and not by in fluorescence in situ hybridization (FISH) or sequencing technologies. FISH analysis has facilitated an accurate cytogenetic diagnostics and compliments karyotyping. FISH can be performed on the non-dividing cells and therefore can be performed on PB cells. FISH studies may be helpful in identifying specific rearrangements not recognized by banding studies alone. FISH also provides a convenient and sensitive method for monitoring patients with a specific cytogenetic abnormality. The WHO also defined some common MDS associated cytogenetic abnormalities as not sufficiently specific to diagnosis MDS in the absence of diagnostic morphologic findings. The presence of cytogenetic abnormalities +8, −Y, and del (20q) while frequently observed in patients with MDS was noted not to be diagnostic of MDS. In the updated 2016 WHO classification del(5q) remains the only cytogenetic or molecular genetic abnormality that defines a specific MDS subtype.
The patient’s clinical findings and history are helpful in guiding the pathological evaluation. An analysis of the bone marrow is essential for the diagnosis of MDS. The bone marrow is typically hypercellular for the patient’s age, confirming the ineffective hematopoiesis, and shows dysplastic features in one or several cell lines. A number of other disorders can present with finding similar to MDS (Table 23.7). A history of the patient receiving chemotherapy and or radiotherapy is important. Questions about environmental and occupational exposures should be noted, including the patient’s smoking history. An occupation history is important because excess cases of MDS have been reported in agriculcultural and industrial workers.
Clonal cytogenetic abnormalities are found in 38–78% of patients with de novo MDS and greater than 80% of t-MDS patients [50]. Cytogenetics are critical in evaluating disease progression and prognosis. All of the currently used prognostic scoring system acknowledge the importance of specific cytogenetics abnormalities to define prognosis and plan therapy. In addition, the acquisition of new cytogenetic abnormalities is generally associated with progression of the disease and a poor prognosis. Although anemia is the most common presenting laboratory feature in patients with MDS, approximately 50% of patients will demonstrate an abnormality of more than one cell line [51]. The WHO thresholds for defining cytopenias remain the same in the new 2016 classification: hemoglobin <10 g/dL, platelets <100 × 109/L and a absolute neutrophil count of <1.8 × 109/L. Patients may be at risk for bacterial infection generally due to qualitative abnormalities of neutrophil function and platelet functional abnormalities are associated with increased risk for bleeding even with an adequate platelet count. Iron studies may demonstrate increased iron stores even in patients who have not received red cell transfusions. The use of flow cytometry to determine the percent of blasts, assessment of CD34+ cells, is not recommended by WHO criteria as a substitute for the visual inspection of the bone marrow, unless the aspirate was of poor quality. The percent of CD34+ cells generally correlates with morphologic examination of routine bone marrow aspirate and peripheral blood smear; however, the WHO noted that not all leukemic blasts express CD34 and hemodilution and processing artifacts can yield misleading results. Multiparameter flow cytometry was recommended to determine the blast lineage and to determine aberrant antigen expression. However, it remains unclear if these changes are specific for the diagnosis of MDS as they occur in other myeloid neoplasms [51].
Immunophenotyping combined with cytogenetics and morphology help in the diagnosis and assessing the possible evolution of MDS to AML [52]. An increase in the percentage of CD34+ cells or CD117+ positive cells may help in documenting the progression to AML in a low-grade MDSs. The WHO, however, while noting that aberrant antigen expression patterns are common in MDS did not consider the phenotypic abnormalities sufficient, in the absence of conclusive morphologic and/or cytogenetic abnormalities, for the diagnosis of MDS. The finding of three or more phenotypic abnormalities involving one or more of the myeloid lineages should be considering suggestive, but not diagnostic of MDS. Patients whose cells demonstrate aberrant immunophenotypic markers should be followed for morphologic features sufficient to diagnose MDS. The use of additional studies including FISH analysis and gene mutational analysis should be performed as clinically indicated. The myelodysplastic/myeloproliferative neoplasm (MDS/MPN) group is an overlap disorder reflecting that some patients have features of both MDS and MPN and patients present with a clinical picture that demonstrates both increased proliferation and dysplastic and ineffective maturation. The classification of MDS/MPN reflects difficulty-separating MDS from other myeloid neoplasms.
Patients with MDS/MPN usually present with a leukocytosis and hepatosplenomegaly. The MDS/MPN category includes four defined entities: chronic myelomonocytic leukemia (CMML), atypical chronic myelogenous leukemia (a CML-Philadelphia chromosome negative), juvenile myelomonocytic leukemia (JMML), and a more heterogenous group of unclassifiable MDS/MPN (U-MDS/MPN). The criteria for MDS/MPN with ring sideroblasts and thrombocytosis, MDS/MPN-RS-T, (previously known as RARS-T) is better defined and includes thrombocytosis, ≥450 × 109/L associated with anemia, erythroid dysplasia, with ring sideroblasts in ≥15% of erythroid precursors. Megakaryocytes with features of a chronic myeloproliferative neoplasm that are hyperlobulated and atypical and are increased in number with large or giant forms with lobated staghorn like nuclei and occur in lose clusters or found adjacent to the endosteum or within sinusoids and important pathologic finding [52]. The spliceosome gene mutation SF3B1, associated with ring sideroblast, is frequently present in cases of MDS/MPN-RS-T but the subtype still requires ≥15% ring sideroblasts. The JAK 2 V617F mutation has been noted in some of the cases of MPN/MDS but the proliferative potential of most cases appear to be related to aberration in the RAS/MAPK or other signaling pathways and the JAK 2 mutation is not the primary oncogenic event to explain the MPN [42, 66]. The prognosis of patients with MDS/MPN-RS-T is better than most of the MDS/MPN disorders. The transformation to AML is uncommon and unlike the MPN there does not appear to be an increase risk of thrombotic or bleeding complications associated with the elevated platelet count. The treatment options for this subtype are not clear and additional studies are needed to further define the clinical course. In addition to the JAK 2 mutation some patients demonstrate the MPL mutation and both mutations appear to correlate with the elevated platelet count. In general the MDS/MPN disorders have a variable clinical course but are generally associated with poorer prognosis than their myeloproliferative neoplastic counterpart and an increased incidence of leukemic transformation. In MDS/MPNs the karyotype is usually normal or demonstrates a typical MDS cytogenetic abnormality. Gene mutations are common in the MDS/MPNs and can be helpful in assessing difficult cases with a normal karyotype. The 2016 WHO classification, however, noted that gene mutations even of the most commonly mutated genes, SRSF2, TET2, ETV6 and ASXL1 is not sufficient proof of a neoplastic disorder because gene mutations occurs in healthy older persons with undetermined significance. While some of these mutations are prognostically important and define aggressive disease, and have been incorporated into new prognostic scoring systems they should not be the sole determinant of a neoplastic disorder [53].
The diagnosis of myelodysplastic/myeloproliferative neoplasm unclassifiable (MDS/MPN-U) includes patients with features of both myelodysplasia and myeloproliferation who cannot be assigned to a more specific category. Patients must meet the criteria of one of the categories of MDS and demonstrate prominent myeloproliferative features without a prior MPN or MDS. The WHO emphasizes that the diagnosis of MDS/MPN-U should not be made in patients who have recently recovered from cytotoxic chemotherapy or have received recent growth factor therapy. A follow-up evaluation in these patients is essential to demonstrate that the changes in the PB and BM are independent of recent treatments or recovery from chemotherapy. The features that distinguish this subgroup include an elevated platelet count or WBC without evidence of BCR–ABL1 or rearrangement of PDGFRA, PDGFRB or FGFR1, del 5q, t (3; 3), or inv3. In most patients, the karyotype is normal and no abnormal mutational studies are noted but the JAK2 V617F mutation may be present [54].
MDS with Fibrosis and Hypocellular MDS
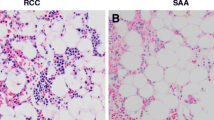
The WHO classifications did not define a number of MDS subtypes that are generally recognized as clinically distinct . The categories MDS with marrow fibrosis and hypocellularity MDS are distinct disorders but the WHO noted that because they lack a consensus on the precise definition or the importance of these findings as distinct entities they on not included in the current classification. A subset of patients with MDS present with a hypocellular bone marrow (less than 15% cellularity on bone marrow biopsy) and minimal dysplasia. Hypocellular MDS must be differentiated from aplastic anemia and hypocellular AML [55]. Hypocellular MDS and aplastic anemia may also be pathophysiologically related [54]. The similarity of both disorders is suggested by their response to immunosuppressive therapy. Hypocellular MDS may represent an intermediate stage in the evolution of aplastic anemia. However, hypocellular MDS in contrast to aplastic anemia tends to occur in older patients, with a more gradual onset and dysplasia involving more than one cell line. In contrast to aplastic anemia dysplastic megakaryocytes are more prominent in hypocellular MDS. Megaloblastic red cell precursors, pancytopenia, and the presence of a paroxysmal nocturnal hemoglobinuria clone (PNH)—occur in both hypoplastic MDS and aplastic anemia and are therefore not helpful diagnostic features A characteristic MDS cytogenetic abnormality sometimes helps to define hypocellular MDS but similar findings may also be present in aplastic anemia [48]. Patients with a PNH clone and hypocellular MDS respond better to immunosuppression.
MDS with fibrosis (MDS-F) can be difficult to differentiate from primary myelofibrosis (PMF), acute megakaryocytic leukemia or acute panmyelosis [55]. The bone marrow is usually not aspiratable (dry tap) and the morphological findings of dysplasia may be difficult to identify on the bone marrow biopsy. Splenomegaly and leukoerythroblastosis on peripheral smear are unusual in MDS-F and when present suggest the diagnosis of PMF. Staining the marrow biopsy and circulating blast forms with megakaryocytic lineage- specific antigens can identify abnormal megakaryoblasts [55]. The finding of diffuse fibrosis in MDS is associated with a poor prognosis and greater than 2+-reticulum fibrosis, as defined by the European consensus system, is an independent negative prognostic marker [52]. The diagnostic challenges that such cases present are discussed by the WHO with a recommendation that hematopathologists should specifically comment upon the hypocellularity or extensive fibrosis in interpretative reports. The WHO classification, however, does not recognize hypocellular MDS and MDS-F as distinct entities as the sub-classification of these cases can be problematic and there is no accepted agreement on the diagnostic features associated with these two disorders. Immunohistochemical stains for CD34 on the biopsy may demonstrate excess blasts and may help in identifying these patients. Bone marrow fibrosis is associated with a higher red cell transfusion requirement, multilineage dysplasia, pancytopenia, and a poor prognosis. The 2008 and 2016 WHO classification attempts to address these issues, about when to call a disorder a separate diagnostic entity, and raises the question of when sufficient clinical characteristics or morphologic findings are distinctive enough to warrant a separate diagnostic category.
The recognition and enumeration of blast cells is of critical importance for the diagnosis of AML, MDS and defining the subtypes of MDS and requires a differential blast count on 500 cells on the aspirate to be 20% or more for a diagnosis of AML (either de-novo or evolved from a prior MDS). If a concomitant non-myeloid neoplasm (i.e., plasma cells) is present those cells should be excluded from the count used to evaluate the percent of blast forms. If an aspirate is not available a touch preparation of the biopsy may yield valuable cytologic information, but differential counts from touch preparations may not be representative and should be confirmed on the bone marrow biopsy. The definition of a blast cell can be difficult in MDS. The WHO did not specifically define the definition of a blast, but noted that blasts can be granular or agranular [54]. Myeloblasts are defined by a high nuclear/cytoplasmic ratio, visible nucleoli and usually fine nuclear chromatin. Nuclear shape can be a variable with basophilic granule, or Auer rods, aggregates of lysozymes, may be noted but no Golgi zone is detected. Granular blast cells must be distinguished from promyelocytes and the principal distinguishing characteristic of the normal promyelocyte is the presence of a visible Golgi zone [54]. Dysplastic promyelocytes have the recognizable features of promyelocytes including round, oval or an indented nucleus that is often eccentric with decreased granules or irregular distributed granules and a poorly developed Golgi zone. Determining the overall percentage of blasts in the context of marked erythroid hyperplasia can be problematic. In the updated 2016 WHO classification the percent of blasts is based on all nucleated cells not just the non-erythroid cells. This new criteria will results in most cases previously diagnosed as the erythroid/myeloid subtype of acute erythroid leukemia in the 2008 WHO criteria now being classified as MDS with excess blasts. In the updated 2016 WHO classification the cytogenetic abnormalities that are MDS defining remain unchanged. While acknowledging the prognostic importance of genetic abnormalities in MDS, in the 2016 WHO criteria only the del(5q) cytogenetic or molecular genetic abnormality defines a specific MDS subtype even if an there is an additional cytogenetic abnormality [3].
The 2016 WHO criteria noted the association between ring sideroblasts and an SF3B1 mutation. The SF3B1 mutation appears to be a early initiating event in the development of MDS and manifests a distinct gene expression profile and correlates with a favorable and indolent course [56]. Patients with MDS carrying the SF3B1 mutation have a more homogeneous phenotype characterized by isolated erythroid dysplasia and the presence of ring sideroblasts. Moreover, the actual percent of cells with ring sideroblast does not affect the prognosis.
The 2008 WHO classification redefined a number of new subgroups [57, 58]. Three categories of refractory cytopenia with unilineage dysplasia (RCUD) are defined: Refractory anemia (RA), refractory neutropenia (RN) and refractory thrombocytopenia (RT). These subgroups do not have an increase in blasts and involve a single lineage. In the 2016 WHO classification these subgroups are part of MDS with Single lineage Dysplasia (MDS-SLD). Other causes of dysplasia need to be addressed and excluded before the diagnosis of single lineage MDS is established (Table 23.7). The expansion of the erythroid component can occur in non-neoplastic disorders, including hemolytic anemia, iron deficiency, and B12 or folate deficiency. Erythropoietin administration may also lead to a marked expansion of the erythroid precursors. Simultaneous or chronologically close administration of erythropoietin and granulocyte growth factors may lead to erythroid hyperplasia with an increase in pronormoblasts and myeloblasts. Therefore, the pathologist must have knowledge of the patient’s clinical history, including the administration of recent chemotherapy or growth factors when evaluating the bone marrow. Other causes of erythroid dysplasia include alcohol abuse (vacuolated erythroid precursors and ring sideroblasts), anti-tuberculosis medications and chloramphenicol. Isolated unilineage dyspoiesis should raise suspicion for secondary causes, including disorders not associated with prescription medications as seen in zinc over consumption leading to copper deficiency. Zinc competes with copper for its carrier, ceruloplasmin. Primary copper deficiency can present with pancytopenia with marked vacuolation of erythroid and myeloid precursors, megaloblastoid changes in red cell precursors and ring sideroblasts [59, 60] (Table 23.6). The 2016 WHO classification notes that the prognostic importance of genetic finding in MDS and the expanding knowledge of the clinical importance of recurring mutations in MDS but notes that the finding of one or more somatic mutation is not considered diagnostic of MDS even in a patient with unexplained cytopenias where these mutation may be frequently found [3].
In patients with MDS who lack the appropriate finding of any defined MDS category diagnosed with subtype, MDS, unclassifiable (MDS-U) . MDS-U has no specific morphological features but includes MDS with the presence of 1% blast forms in the peripheral blood and <5% blasts in the bone marrow. An occasional blast can be found in healthy individuals and to avoid over interpreting the rare blast form the WHO notes that blasts must be noted in the peripheral blood on two or more successive evaluations to confirm the diagnosis of MDS-U. In addition the diagnosis of MDS - U can be made in cases with 1% or fewer blasts in in the blood and <5% blasts in the bone marrow with unequivocal dysplasia in <10% of one or more myeloid lineages but have a diagnostic cytogenetic abnormality. MDS-U is a very heterogenous subtype and patients have a variable clinical course and should be reclassified if they develop findings characteristic of a specific MDS subtype. The MDS-U subtype may represent the early phase of one or more specific MDS subtypes but with nonspecific morphological features of MDS.
Idiopathic Cytopenia(s) of Undetermined Significance and Idiopathic Dysplasia of Uncertain Significance
Patients who present with cytopenias but lack the diagnostic criteria of MDS, but in whom the diagnosis of MDS is suspected, are classified with the diagnosis “Idiopathic Cytopenia(s) of Undetermined Significance” (ICUS) [61]. The criteria for this group of disorders reflects the diagnostic uncertainty in these patients. A key distinction of ICUS from other potential precursor conditions such as MGUS, monoclonal B-cell lymphocytosis (MBL) and T cell clonality of undetermined is that an ICUS designation does not necessarily imply a clonal disorder. Limited data are available about the frequency or natural history of ICUS and reflects that some patients present with persistent cytopenia but lack the diagnostic features of MDS. The term idiopathic dysplasia of uncertain significance (IDUS) was proposed to describe a group of patients with dysplasia but no or only mild cytopenias [61]. In contrast to ICUS, patients with IDUS demonstrate dysplasia in >10% of cells in one or more lineage with or without a MDS-related karyotype but without persistent cytopenias. ICUS and IDUS have very variable courses and it is unclear if all the patients will ultimately develop a defined subtype of MDS or another myeloid neoplastic disorder. Moreover, it is unclear if these disorders are mutually exclusive or if the classification of a potentially premalignant disorders will provide meaningful prognostic or diagnostic information for patients in whom no cause for the cytopenia is found. The proposed term Clonal Cytopenia of Undetermined Significance (CCUS) has been proposed for cases with somatic mutations, or a non-diagnostic chromosomal abnormality, defining a clonal population in the bone marrow, but without dysplasia and one or more cytopenia in the blood (Table 23.8) [62].
MDS Subtypes
MDS with Ring Sideroblasts (MDS-RS)
MDS with ring sideroblasts (MDS-RS) is characterized by anemia, erythroid dysplasia and >15% ring sideroblasts of bone marrow erythroid precursors. There is generally no or minimal dysplasia in the non-erythroid precursors. Myeloblasts comprise <5% of the nucleated BM cells and are not present in the PB. In the 2016 WHO criteria MDS-RS is associated with recurrent mutations of the spliceosome gene SF3B1. The classification of MDS-RS was changed to include MDS cases with ring sideroblasts and multilineage dysplasia. This change reflected the link between ring sideroblasts and an SF3B1 mutations. In the 2016 classification if the SF3B1 mutation is identified then the diagnosis of MDS—RS can be made even if the ring sideroblast comprise only 5% of nucleated erythroid cells. If the SF3B1 mutation is lacking then ≥15% ring sideroblasts of nucleated erythroid cells is still required. MDS-RS subtype is divided into two groups; a group with single lineage dysplasia (MDS-RS-SLD), previously classified as refractory anemia with ring sideroblasts, and second group with multilineage dysplasia (MDS-RS-MLD), previously classified as refractory cytopenia with multilineage dysplasia. Patients with MDS—RS who lack the SF3B1 mutation have a more heterogenous phenotype, a high prevalence of TP53 mutations and less favorable prognosis. The SF3B1 mutation is early event in the development of MDS and may be an important therapeutic target in MDS-RS [58]. MDS-RS constitutes approximately 10% of cases of MDS. A majority of patients present with a moderate normochromic or macrocytic anemia. The PB frequently reveals dimorphic red cells due to a small population of microcytic and hypochromic red cells. Basophilic stippling and Pappenheimer bodies may be noted in red cells. Dysplasia is present in <10% of neutrophils and platelets. The bone marrow is usually hypercellular for the patient’s age and demonstrates erythroid hyperplasia. The iron stain, Prussian blue staining, reveals ring sideroblasts that surround at least a third of the nuclear circumference. Iron stores are generally increased even in the absence of red cell transfusions. The number of CD 34+ cells is normal and most patients do not demonstrate a cytogenetic abnormality. Ring sideroblasts may be seen in a number of other, non- MDS-related disorders including lead poisoning, drugs including isoniazid which inhibits delta aminolevulinic acid (ALA) dehydratase activity and block hemoglobin formation resulting in ring sideroblast formation [45]. A number of acquired and hereditary conditions are associated with ring sideroblast formation and should be excluded before a diagnosis of MDS-RS is established. In RARS the ring sideroblasts and increased iron stores reflect abnormal iron metabolism in the erythroid lineage resulting from the ineffective erythropoiesis. The overall prognosis for patients with MDS-RS is 69–108 months and less than 2% of cases transform into AML. Progressive anemia requiring transfusion support is frequent and in select patients iron chelation therapy should be considered early in the clinical course to prevent iron overload and end organ failure. However, the overall beneficial effects of early iron chelation has not been demonstrated to improve survival in prospective randomized studies and therefore remains controversial [63].
MDS with Single Lineage Dysplasia and MDS with Multilineage Dysplasia
This group of disorders was previously know as Refractory anemia and refractory anemia with multilineage dysplasia in the 2008 WHO classification and is now classified as MDS-SLD and MDS-MLD. The difference between these subtypes reflects either a single or 2 or more lineages demonstrate dysplasia. These groups constitute approximately 30% of MDS cases and are characterized by one or more cytopenias and dysplastic changes in one two or more of the myeloid lineages. Blasts are rare, <1%, in the PB and <5% in the BM. Auer rods are not present in either the PB or BM. The anemia is usually macrocytic or normocytic with prominent granulocytic dysplasia including hypo granularity, nuclear shape abnormalities including hypo-lobation, acquired pseudo Pelger-Huet anomaly, and abnormal nuclear clumping. The bone marrow is usually hypercellular for age of the patient with <5% blasts. Erythroid precursors may demonstrate cytoplasmic vacuoles and marked nuclear irregularity including internuclear bridging and nuclear budding. The BM may have variable number of ring sideroblasts but less than 15%. The previously described WHO category of refractory cytopenias with multilineage dysplasia with ring sideroblasts has been omitted and incorporated in MDS-RS-MLD. Megakaryocytic dysplasia includes hypolobated and non-lobated nuclei, multinucleated and micromegakaryocyte, megakaryocytes with non-lobated or bi-lobed nuclei. Clonal cytogenetic abnormalities are present in up to 50% of patients and are important in defining the prognosis. The prognosis is related to the degree of cytopenias and cytogenetic abnormalities.
MDS with Excess Blasts 1(MDS-EB1 and MDS-EB2)
MDS-EB1 and EB2 comprises 40% of cases of MDS and is divided into MDS-EB1 and MDS-EB2 on the basis of the number of blasts and the presence or absence of Auer rods. EB 1 is defined by 5–9% blasts in the BM or 2–4% blasts in the PB and no Auer rods and EB2 is defined by 10–19% blasts in the BM or 5–19% blasts in the PB. The presence of Auer rods confirms the diagnosis of EB2 irrespective of the percent of blast forms. Most patients present with symptoms of BM failure including anemia, bleeding or neutropenia. The PB generally shows dysplastic changes in all three-cell lines and is typically hypercellular for age of the patient. Erythroid precursors may be increased with megaloblastoid changes and ring sideroblasts. The excess blasts define these subtypes. Dysmegakaryopoiesis is a frequent finding including micromegakaryocytes and abnormal megakaryocytic clustering. Blasts may form abnormal aggregates or clusters that are located away from trabeculare and vascular structures, a histologic finding previously referred to an abnormal localization of immature precursors (ALIP) . Immunohistochemical staining for CD34 may help in identifying blast forms. Clonal cytogenetic abnormalities are observed in 30–50% of cases including +8, -5, del(5q),−7, del(7q), del (20q) and complex karyotypes. Fibrosis may be present and results in a dry tap. The presence of fibrosis should be noted and the finding of extensive fibrosis is an independent negative prognostic marker in MDS [3]. MDS-EB1 and 2 frequently progress to AML, 25% and 33% respectively for MDS-EB1 and MDS-EB2 respectively. The median survival is approximately 16 months for MDS-EB1 and 9 months for MDS-EB2. The survival is dependent on the number of blast forms. Cases with >5% blasts and a complex karyotype have a median survival of ≤3 months similar to AML with myelodysplastic changes.
Myelodysplastic Syndrome with Isolated del (5q)
Heterozygous, interstitial deletions of the long arm of chromosome 5 (5q) are the most common cytogenetic abnormality in patients with MDS. Del 5q is associated with a consistent clinical phenotype previously known as the 5q- syndrome in a subset of patients. Abnormalities in chromosome 5 occur in approximately 25% of MDS patients, but the incidence of the originally described 5q- syndrome is much less frequent [63]. The 5q- syndrome was originally described in patients with a macrocytic anemia, dyserythropoiesis and erythroid hypoplasia in the bone marrow and a normal to elevated platelet count, hypolobated megakaryocytes and an intestinal deletion involving the long arm of chromosome 5. In addition the 5q- syndrome in characterized by the absence of circulating myeloblast and therapeutic sensitivity to treatment with lenalidomide. The deletion of 5q in MDS does not necessarily equate to the clinical 5q- syndrome. Both the original 5q- syndrome and del (5q) MDS respond to lenalidomide and the revised WHO changed its definitions to this cytogenetically defined subset from 5q- syndrome to MDS with abnormality del(5q) [64, 65]. The deletion occur on a single chromosome resulting in a heterozygous (haploinsufficient) with the unaffected chromosome 5 contains the normal allele of all the genes contained in deleted segment. None of the genes on the nondeleted chromosome 5q are mutated or undergo homozygous inactivation in MDS patients. The recurrent haploinsufficiency for critical genes within the common deleted regions (CDR) on chromosome 5q is the basis for the unique pathological phenotype that results in the MDS subtypes del (5q). Haploinsufficiency of the RPS 14 gene on the long arm of chromosome 5 (5q) leads to activation of the P53 pathways and the development of the characteristic macrocytic anemia. The CDR on chromosome 5 and the breakpoints and size of the deletions in the original 5q- syndrome patients and the del (5q) patients with advanced MDS and AML are variable. The CDR of the 5q–syndrome the interstitial deletion occurs in a 1.5 MB region at 5q32–33. The region contains genes for the ribosomal protein RPS14 and three micro RNAs mrR-143, miR-145, and mir-146. The non-allelic deletion of the RPS14 gene encodes for a component of the 40 s ribosome and is critical for the development of the macrocytic anemia. In contrast, patients with del (5q), and additional chromosomal abnormalities and excess blast have a different clinical course and response to treatment [85]. Patients with a deletion of 5q- and AML have large interstitial deletions that overlap the CDR of the 5q-syndrome and low risk del (5q) However, in high risk MDS and AML the deleted region was in a more distal CDR in the 5q32–33 region. Lenalidomide selectively inhibits the Del (5q) clone and results in RPS 14 inactivation of the p53 pathway. Lenalidomide exerts unique karyotype specific activity in Del (5q) MDS but does not eradicate the Del (5q) stem cell population in all patients. The inactivation RPS14 leads to defective erythropoiesis and increased apoptosis in erythroid progenitors. Moreover, in the congenital disorder Diamond- Blackfan anemia the down regulation of an another ribosomal gene (RPS19) is critical in the development of the erythroid hypoplasia and chronic anemia [65]. The down regulation of RPS14 may not be the sole genetic event underlying the del 5q- syndrome and alteration of other genes in the commonly deleted segment in 5q- may be required. The tumor suppressor SPARC (Secreted Protein Acidic and Rich in Cysteine) gene is located in the del 5q31 region. SPARC has tumor suppressor, antiproliferative, and anti angiogenesis properties and may also be important in this syndrome [64]. The loss of additional genes that code for these and other factors appear to contribute to the development of this syndrome and its unique response to the immune modulatory drug, lenalidomide. MDS with isolated del 5q syndrome is frequently associated with morphological features of MDS-SLD. Thrombocytosis and anemia is occasionally seen and when present is suggestive of the del 5q chromosomal abnormality. The bone marrow aspirate and biopsy are typically hypercellular for the patient’s age with erythroid hypoplasia and dysplastic erythropoiesis. Ring sideroblasts may be present but <15% of erythroblasts. A del(5q) subtype should be suspected in patients who present with a refractory macrocytic anemia, with a normal or mildly low leukocyte counts, and thrombocytosis (a platelet count >400 × 109/L). In contrast to the other MDS subtypes, where the mononuclear megakaryocytes are smaller (micromegakaryocytes), in the MDS with del 5q the megakaryocytes are bilobed or non-lobulated but of normal size (mono lobulated). The MDS with del 5q has a marked female predominance (70%), and rarely transforms to AML. A majority of patients have progressive anemia and become red cell transfusion dependent and rarely respond to growth factors including erythropoietin. Lenalidomide is the treatment of choice and results in transfusion independence in over two thirds of cases with durable clinical and cytogenetics responses [42].
Clinical and Laboratory Features of MDS
Blood and Bone Marrow Findings
Red Cells/Anemia
Macrocytosis or a macrocytic anemia with a low reticulocyte count is common in MDS and reflects the ineffective erythropoiesis. Impaired red cell maturation has been associated with acquired abnormalities of globin chain synthesis, and red cell enzymes. PNH has been described in the setting of MDS, and these patients have many of the typical diagnostic features of PNH including a defect in the synthesis of the glycosylphosphatidylinositol (GPI)-linked surface protein, but lack the ongoing red cell hemolysis and thrombotic complications associated with PNH. Cases may have abnormalities in the size and shape of red cells including basophilic stippling (red cell inclusions composed of ribonucleoprotein and mitochondrial remnants), Pappenheimer bodies (basophilic iron-containing granules peripherally located in red cells), macro-ovalocytes, teardrop forms, and nucleated red cells. The bone marrow may reveal multinuclear fragments, inter-nuclear bridging, and nuclear cytoplasm asynchrony.
Neutrophils
Qualitative abnormalities of neutrophil function are a common feature of MDS and may explain the increased risk for bacterial infections. Morphological abnormalities include hypo-granular and hyposegmented neutrophils, which are associated with a negative peroxidase reaction and decreased myeloperoxidase activity. The neutrophils are hyposegmented and may be confused with band forms. Nuclear fragmentation and nuclear-cytoplasmic asynchrony in early myeloid precursors may be a prominent feature in the bone marrow. Dysplastic myeloid precursors can be difficult to distinguish from blast forms and therefore a pathologist experienced in the interpretation of MDS should review the bone marrow.
Platelets
Thrombocytopenia and abnormal platelet function occur in MDS. Thrombocytopenia is an adverse prognostic feature independent of other prognostic factors [65,66,68]. While thrombocytopenia is associated with poor performance status and other unfavorable prognostic variable bleeding complications are underreported. Thrombocytopenia (<100 × 109/L) has been reported in 66% of patients and was associated with a 24% incidence of deaths from hemorrhage. Impaired platelet function may also explain the increased risk of bleeding in patients with MDS. Spontaneous bruising and bleeding after surgery or mild trauma occurs in MDS patients with a normal or slightly depressed platelet counts. Dysplastic platelets and abnormal megakaryocytes are important diagnostic features and help in distinguishing MDS from other disorders. Giant platelets, and agranular (grey platelets) and megakaryocytic fragments in the peripheral blood film are important diagnostic features of MDS.
Bone Marrow Findings
A bone marrow aspirate and biopsy is essential for the making diagnosis of a MDS and to define the MDS subtype. Abnormal distribution of cells is often present; erythroid islands may be absent or very large. Granulocytic precursors may be clustered centrally rather than their normal paratrabecular distribution. Micromegakaryocyte, mononuclear megakaryocytes, and hyperlobulated megakaryocytes are important diagnostic features of MDS and are reliable morphological findings of dysplasia. In the bone marrow the megakaryocytes may be clustered or adjacent to the bony trabecula. The del 5q syndrome has mononuclear megakaryocytes that are of normal size but with a single eccentrically placed round non-lobulated nucleus [3]. Megaloblastic changes (nuclear cytoplasm asynchrony) can be seen in the myeloid and erythroid precursors. Dysgranulopoiesis and dyserythropoiesis are more readily noted in the bone marrow aspirate smear and not the biopsy. The bone marrow smear is necessary to identify ring sideroblasts that may not be apparent on the biopsy sample. Immunohistochemistry may be a useful supplement to histology. Small mononuclear megakaryocytes can be confused with myeloid precursors. A biopsy is necessary to access the degree of reticulin fibrosis and overall bone marrow cellularity. Immunophenotyping using flow cytometry on the bone marrow and/or peripheral blood may be helpful in the diagnosis and defining prognosis and response to treatment. However, while controversial there are currently no accepted standards for the diagnosis of MDS by flow cytometry.
The finding of aberrant immunophenotyping of myeloid blasts is helpful in corroborating the diagnosis of MDS, but is not diagnostic of MDS. The aberrant expression of the lymphoid antigen CD7 on myeloid blasts is a common phenotypic abnormality and correlates with a poor prognosis [42]. Increase and/or clustering of blasts favors MDS. Immunostaining for CD34 on core biopsy is very helpful to estimate blast numbers and possible clustering. In the absence of reliable aspirate smear, CD34 immunostaining on core biopsy and/or clot section can be used for estimating percentage of blasts. The use of flow cytometry on both the PB and BM is the focus of many studies and should be part of the initial evaluation of MDS [42].
Clinical and Prognostic Features
The initial evaluation of all patients with MDS should be performed before planning treatment and should include a detailed history of prior exposures to chemotherapy, radiation therapy or toxic exposures. The cellularity should be noted from the bone marrow biopsy. The percent of blasts and the iron stain and the presence of ring sideroblasts should be performed on the bone marrow aspirate. Iron studies including a ferritin and transferrin saturation should be obtained prior to starting growth factors and on patients who are receiving red cell transfusions. A serum erythropoietin should be determined in patients with symptomatic anemia. In patients who are candidates for an allogeneic hematopoietic stem cell transplant HLA typing should be performed on the patient and their siblings.
The WHO classification system attempts to offer general prognostic guidance for each subtype but additional information is usually needed to assign prognosis and plan therapy. In an effort to determine prognosis a number of prognostic scoring systems have been developed including the International Prognostic Scoring System (IPSS), the MD Anderson Prognostic Scoring System (MDAPSS), World Health Organization –based Prognostic Scoring System (WPSS) and others models have been developed to define the prognosis and guide therapy [69, 70]. The widely used and generally accepted International Prognostic Scoring System (IPSS) developed in 1997 and recently revised, IPSS-R, addresses clinical features not included in the WHO classification and attempts to define prognosis and leukemic progression. The IPSS-R included 5 cytogenetic subsets reflecting the importance of new prognostically important cytogenetic groupings (Table 23.9). The scoring system assigns a point score for each the following variables: the number of bone marrow blast forms, karyotypic abnormalities, and number of cell lines affected (cytopenias) (Table 23.10). The combined score determines the overall risk category: very low (risk score ≤ 1.50), Low (risk score > 1.5–3.0), Intermediate (risk score > 3–4.5), High (risk score > 4.5–6) and very high (risk score > 6). The IPSS-R risk category and score correlates with the overall survival and probability of transformation to AML (Table 23.9).
The other prognostic scoring systems include similar parameters but the IPSS-R scoring system continues to be widely used for stratification of patients enrolled in clinical trials [69, 70]. However, the IPPS-R system has a number of important limitations. The IPPS-R system is based in part on the FAB classification of MDS and includes MDS patients with 30% blasts. The threshold for AML in the WHO classification is 20% blasts which is not reflected in the IPSS–R blast scoring system. The IPSS also does not completely address the severity of the cytopenias or the need for transfusion support and does not take into account other prognostic variables. The IPSS-R acknowledged the prognostic importance of additional variable but did not assign a point score to these factors including LDH, serum ferritin, β2-microglobulin, marrow fibrosis, patient’s age, performance status and comorbidities. Other prognostic factors including disease duration or prior treatments are not part of the IPSS-R. The IPPS and IPSS-R was intended to assign prognosis at the time of diagnosis and therefore is a static score that was not intended to change with time or treatments. The IPSS–R also includes a number of uncommon cytogenetic subsets does not address the expanding role of molecular genetic studies in MDS.
MDS is often broadly separated, for treatment decisions, into low risk and high-risk disease based on overall survival and risk of AML transformation. The lower risk subtypes include MDS with single lineage dysplasia, MDS with Multilineage dysplasia, MDS with ring sideroblasts, MDS with isolated del(5q). The IPSS-R low risk categories include the very low, low and intermediate risk categories. These groups are associated with a general survival of >3 years and a low risk for transformation to AML and generally correspond to a IPPS-R score of <3.5. In contrast the higher risk MDSs groups include MDS-EB 1 and 2 and IPSS-R groups high and very high and are associated with a greater risk for transformation to AML [70].
Treatment
The treatment
of a patient with MDS should be individualized based on the patient’s age, subtype, IPSS-R risk category, performance status, cytogenetics and co-morbid medical problems. The majority of patients with MDS are elderly and tolerate intensive chemotherapy poorly. Moreover, standard therapies do not result in a cure and their impact on survival for most patients is unclear. Therefore any potential benefits of treatment must be weighed against the side effects and the patient’s overall prognosis. The alleviation of disease-related complications and improved quality of life are important goals for most patients. The most appropriate care for many patients still remains supportive care. Although there are a number of therapeutic options available for MDS patients, none, other than an allogeneic stem cell transplantation, offers the potential for cure. The therapeutic options for patients with MDS include the use of hematopoietic growth and trophic factors, immunosuppressive agents, low-intensity cytoreductive chemotherapy including the hypomethylating agents, and intensive chemotherapy. While advances in the diagnosis and risk stratification has refined the prognosis for patients and defined gene mutations that are potential targets in MDS, no new drugs s have been approved for the treatment of MDS in over a decade.
Guidelines for evaluating the response to treatment in patients with MDS have been updated and incorporated into the criteria by the International Working Group (IWG) [71]. These guidelines attempted to define standard, criteria for complete and partial responses to treatment. Moreover, the response criteria emphasized that the goals of treatment of MDS is to alter the natural history of the disease and alleviate the disease-related complications and improve the quality of life. Stable disease or minimal responses are difficult to interpret and make comparisons between trials difficult. In addition, the response rate in some Phase II trials did not translate into prolongation of survival, time to treatment failure, or improvement in the quality of life. The IWG criteria are a useful standard to use for comparing results across therapeutic trials and are now widely used for defining response to treatment.
Supportive Therapy
In many patients the diagnosis of MDS may require a period of observation and reevaluation. The WHO appropriately noted that in some patients reevaluating the peripheral blood and bone marrow after 3–6 months period was essential to exclude other causes of the dysplasia. In patients with indolent disease or who are asymptomatic, elderly, and frail or have co-morbidities, supportive therapy including transfusions represents a widely accepted standard of care. Patients should be followed for a change in their clinical pattern i.e., increase in red cell transfusion, declining platelet count, circulating blast forms, splenomegaly or decline in performance status. Red cell and platelet transfusions are administered for the symptomatic treatment of the anemia and thrombocytopenia. There is no one single hemoglobin cut off at which RBC transfusion should be offered to all patients but the use of transfusion support is increasing over the years in an effort to maintain a higher hemoglobin/hematocrit. Platelet transfusions are generally given when the platelet count is <10,000 × 109/L but should be adjusted on the basis of individual risk factors and bleeding history. Thrombocytopenia is common in MDS and bleeding complications are exacerbated by impaired platelet function [68]. Platelet dysfunction is common and patients may bleed even with an adequate platelet count. Therefore, platelet support may be required prior to surgery and procedures to prevent excess bleeding. Patients with a platelet count of ≤20,000 × 109/L are at higher risk for bleeding. Disease modifying agents such a lenalidomide and hypomethylating agents are associated with thrombocytopenia. The repeated use of platelet transfusions is associated with allo immunization and transfusion reactions. Danazol an attenuated synthetic androgen with immune modulating activity may be effect in some thrombocytopenic patients with MDS [72]. Thrombopoietin receptor agonist (TPO) are being tested in clinical trials as single agents in low-risk MDS patients and in combination therapy with disease modifying agents (lenalidomide) in high risk MDS. Romiplostim a Fc- peptide fusion protein with no sequence homology with endogenous TPO has been evaluated in low /intermediate risk MDS patients with thrombocytopenia [73, 74]. Romiplostim reduced overall bleeding events but the trial was stopped because of concerns regarding leukemic transformation. Eltrombopag and oral nonpeptide, noncompetitive TPO receptor agonist which is indicated for the treatment of ITP was evaluated in a phase 2 randomized trial in low/intermediate risk MDS patients, Eltrombopag increased the platelet count in a limited number of patients without a increase in leukemic risk. It was unclear in the limited studies that either TPO improved survival. The TPOs are not approved at this time for treatment of thrombocytopenia in MDS patients.
Neutropenia and impaired neutrophil function are also common in MDS patients. The use of prophylactic antibiotics, however, is not warranted for most patients. Neutropenia without a history of recurrent infection is not a justification for the initiation of therapy. Granulocyte colony stimulating factor or granulocyte macrophage colony stimulating factors can transiently increase the neutrophil and blast count in many patient with MDS. However, the clinical benefit of these growth factors is unclear. The use of G-CSF did decrease the incidence of serious infections but did not favorably impact survival in a prospective controlled trial. The use of these cytokines did increase the white blood count and the number of circulating blasts but did not appear to accelerate the progression to acute leukemia. Although in selected patients with active, serious infections there may be a role for the use of these cytokines in the MDS patient with neutropenia in combination with antibiotics, at present there is no evidence to support the general use of either G-CSF or GM-CSF [74].
Patients may require multiple transfusions over many years and the potential for iron overload should be addressed early in a patient’s course. Each unit of RBC contains 200–250 mg of iron and iron overload from transfusions occurs when a patient has received 25 units of packed red cells [74,75,76,77,79]. The benefits of chelation therapy (ICT) in MDS remains controversial. Patients with transfusion dependent low risk MDS may benefit from the early introduction of iron chelation and chelation may reduce the effects of iron overload on cardiac and possibly prevent end organ damage due to tissue iron overload [77]. Iron chelation may also reduce the risk of infections and improve survival after allogeneic hematopoietic stem cell transplantation and may delay the leukemic progression and improve hematopoiesis [78]. Some observations suggest that cytopenias in iron-overloaded patients with MDS could be mitigated by ICT, possibly by a decrease in reactive oxygen species-mediated damage to hematopoietic cells [79]. In addition hematologic improvement was seen in some patients who received deferasirox including a normalization of labile plasma iron [79]. The use of ICT may suppress ineffective erythropoiesis by reducing iron and/or oxidative stress and modulating proliferation and differentiation. However, the risk of iron overload in transfusion dependent MDS patients is unclear. Iron toxicity in MDS patients may not only depend on tissue iron accumulation but also the extent of non-transferrin bound iron. Prospective studies evaluating the clinical benefit of iron chelation in MDS patients ongoing [77]. Iron chelation is a slow process and therefore it is important to view chelation as a preventive supportive measure. The use of deferoxamine is impractical for most patients with MDS. Deferoxamine has a short half-life and requires a prolonged parental, either subcutaneous or intravenous, infusion that is administered over 8–12 h. The rapid infusion of deferoxamine following a red cell transfusion has limited benefit and does not result effective chelation. The oral iron chelator deferasirox (Exjade, Jadenu) is administered daily and is effective in reducing the serum ferritin [79]. Deferasirox can cause reversible renal insufficiency and GI disturbances, including gastrointestinal bleeding. In a number of studies Deferasirox was poorly tolerated in MDS patients with serious renal and gastrointestinal side effects [76]. A number of guidelines on the use of chelation therapy in MDS have been reviewed and a consensus statement published recommending the use of oral chelation therapy in transfusion dependent patients with low risk MDS. Iron overload may contribute to increased morbidity and mortality in low risk MDS patients. However other studies did not demonstrate a direct correlation of the serum ferritin, numbers of transfusions and overall survival. The benefits of prolonged oral chelation therapy is low risk MDS patients remains controversial and in general the benefits should be weighed against the potential risks and its effect on quality of life. The beneficial effects of iron chelation therapy on organ function and survival in transfusion dependent MDS patients is currently lacking. But, in low risk transfusion dependent patients with a ferritin of >1000 mg/dL or patients considered eligible for an allogeneic stem cell transplant ICT should be considered and renal and hepatic function closely monitored.
Erythropoiesis Stimulating Agents (ESAs)
Recombinant hematopoietic growth factors have been used with varying degrees of success to treat the cytopenias in MDS. Recombinant human erythropoietin (rHuEPO, EPO and darbepoetin), granulocyte-colony-stimulating factor (G-CSF), and granulocyte-macrophage colony stimulating factor (GM-CSF) have a role in managing the anemia and neutropenia in selected patients with MDS. ESAs have been studied extensively and approximately 30% of anemic patients with MDS will respond to treatment [75]. The reported response rates in low risk MDS varies between 30 and 82% depending on patient selection and response criteria [80]. The best responses to erythropoiesis stimulating agents (ESA) are observed in patients with an endogenous erythropoietin level of <500 U, a transfusion requirement of less than two units of red cells a months and low risk MDS with <5% myeloblasts [81]. ESAs decrease red cell transfusion requirements and improved the quality of life (QOL). Higher doses of EPO appear to enhance the erythroid responses. The combination of EPO plus G-CSF appears to be synergistic and may optimize the response to EPO. The duration of response was 11–24 months and EPO with or without G-CSF did not increase the incidence of AML transformation. ESAs did improve the QOL but treatment did not impact on overall survival. The ESAs have been associated with an increased mortality, possible promotion of tumor growth in solid tumors and thromboembolic events in non-MDS patients. No increase in treatment related either cardiovascular or thrombotic events occurred in patients who received either EPO alone or combination cytokines EPO with G-CSF as compared to a control population. The FDA recently cited safety concerns from data in clinical studies with ESAs administered to patients with solid tumors [81]. In patients with various solid tumors the use of ESAs was associated with a shortened survival, and/or increased risk of tumor progression or recurrence as well as a increased risk for thrombotic events in patients with renal disease (http://www.fdagov/Drugs/DrugSafety/). MDS patients did not have a increase in disease progression or thrombotic complications associated with ESAs [80]. A predictive model for treatment with EPO and G-CSF demonstrated that patients with an EPO level of <500 mU/mL, and a pretreatment transfusion requirement of less than 2 units/month responded best to ESAs [81]. Best responses were noted in IPSS lower risk patients. Responses can take 8 or more weeks with most patients responding by 12 weeks and the recommended starting for the recombinant human erythropoietin alpha (rEPO) doses are 40–60,000 units administered once or twice a weekly, and increasing the dose up to 300,000 U/week depending on the response. The longer acting form, Darbepoetin , is administered starting at 50–300 mcg/weekly or every other week. Darpoetin administered every 2–3 weeks at a dose of 500 mcg is also effective. Adequate iron stores should be documented prior to starting EPO treatment and during therapy as the failure to respond or loss of response may be a manifestation of depleted iron stores. Low doses of G-CSF (1 μg/kg) with EPO can be added to patients who fail to respond and appeared to augment the response in selected patients [80]. The mechanism of the response to high doses of EPO is unclear but the growth factors may modulate apoptosis in MDS progenitors and enhance erythropoiesis. Moreover, the response to ESAs may define a more favorable group of MDS patients and in a Phase III trial MDS patients who responded to EPO had a longer overall survival versus those who did not respond [80].
Thrombocytopenia is an independent adverse prognostic factor for survival in MDS. Bleeding complications resulting from thrombocytopenia and MDS associated platelet dysfunction are major causes of morbidity and mortality in MDS. Treatments to increase the platelet count are limited. Danazol is an attenuated, synthetic androgen that has been used in the treatment of immune-mediated thrombocytopenia (ITP) . Danazol may increase the platelet count in low-risk MDS patients who are thrombocytopenic [72]. The mechanism of action is unclear, but may reflect that some patients with MDS have immune-mediated thrombocytopenia that responds to the immunoregulatory effects of danazol. Danazol, 200 mg po tid, is generally well tolerated and associated with an increase in platelets in 10–46% of treated patients. The duration of response is variable, 2–26+ months, and maintained only while the drug is administered. Patients with platelet counts greater than 15 × 109/L appear to respond best, and the impact on survival or disease progression is unknown. Two thrombopoietin receptor agonists (TPO), eltrombopag and romiplostim, are currently available to treat patient with refractory ITP. Both agents are active in patients with ITP by increasing platelet production. However, safety concerns remain including the risk of marrow fibrosis and leukemic transformation [68]. A transient increase in blasts forms has been noted in patients treated with TPO. Eltrombopag is currently being studied in higher risk MDS patients. Ongoing studies are evaluating the role of these agents in the treatment of the thrombocytopenic patient with MDS. These early trials of TPOs suggest that they are well tolerated in MDS patients and increased the platelet count and decreased the need for platelet transfusions and clinical bleeding events. But their effect on survival and disease progression is unclear.
Immunosuppressive Therapy
Patients with MDS can present with a number of immune-mediating pancytopenias that potentially respond to immunosuppressive therapy [82]. Some patients with low risk and hypocellular MDS responded to immunosuppressive regimens used for the treatment of aplastic anemia. Selected patients with hypocellular or normal cellular bone marrows responded to the administration of anti-thymocyte globulin (ATG), cyclosporine A(CSA) and steroids [83]. Antithymocyte globulin (ATG) either rabbit or hoarse derived, administered at doses similar to those used in the treatment of aplastic anemia resulted in improvement of one or more cytopenia in 30–50% of selected patients [83]. Trilineage responses were observed in some patients and the median duration of response was 10+ months. Responses were more frequent with hypocellular MDS but were even noted in patients with normocellular bone marrows. Improvements were seen in patients with low-, intermediate-, and high-risk IPSS scores. Age, 60< years, HLA- DR15 positivity, low risk disease, shorter duration of transfusion dependency, and trisomy 8 cytogenetic abnormality correlated with the response to treatment [84]. The responses did not correlate with the loss of a previously noted cytogenetic abnormality, suggesting that the treatment was not affecting the MDS clone. A majority of the patients attained a partial response and treatment did not restore normal hematopoiesis. The mechanism of action is not clear but in vitro studies suggest that the response may be mediated by a loss of cytotoxic T-lymphocyte activity which correlated with changes in the T-cell receptor profiles [84]. The response to ATG appears greatest in low-risk patients. In some patients who initially responded to ATG and then relapsed, retreatment was effective. Toxicity of ATG therapy included fevers, infusion related side effects, and infections. Age was the most important predictor of response with patients >60 years of age having a poorer outcome and increased complications associated with immunosuppressive therapy. These studies suggested that older patients with MDS may have a decreased marrow reserve associated with a diminished response to immune-suppression. CSA, alone may also be effective in hypocellular MDS patients. The combination of CSA and ATG may enhance the response in selected patients. In addition the use of alemtuzumab, an antibody against CD52, has been used in selected patients. The reported studies of ATG and CSA treated a highly selected subset of patients that represent a minority of patients with MDS. Most of the responding patients presented with hypocellular marrows (<15% cellularity) with minimal dysplasia. The responses of MDS patients to immunosuppressive therapy reflect the heterogeneity of the disorder and the relationship between the immune system, marrow suppression and MDS remains controversial. In addition it is unclear if the use of ATG with or with CSA impacted overall survival. In at least one Phase 3 trial comparing ATG + CSA versus best supportive care found no difference in overall survival or transformation to AML in the ATG + CSA arm. The use of immunosuppressive therapy to modulate the abnormal clone represents a controversial but a potential treatment that needs to be further evaluated to define the optimal group of patients who are candidates for immunosuppression.
Lenalidomide
Lenalidomide is a second generation 4-amino-gluteramide analog of thalidomide. Lenalidomide has multiple modes of action including pro-apoptotic cytokine generation, T cell stimulation or inhibition, antiangiogenesis, altering cell adhesions to bone marrow stroma, direct antiproliferative activity and the inhibition of a pro-inflammatory cytokines [85]. Lenalidomide was active in patients with del (5q) by selectively inhibiting the del(5q) clone. Lenalidomide in a phase II trial was administered at 10 mg/day for a 28 cycle or 21/28 days cycle in transfusion dependent patients with del(5q) abnormality 67% of patients became transfusion independent and 45% obtained a complete cytogenetic; complete and partial responses occurred in 84% of patients with del (5q) [63]. The finding of additional cytogenetic abnormalities, with the exception of −7/del(7q), did not significantly affect the response to lenalidomide. All patients who had a cytogenetic response became transfusion independent which was associated with improvement in overall survival. Patients who did not response to lenalidomide had higher rate of progression to AML. The median duration of response was 2.2 years (range 0.1–4.4 years) and approximately 30% of patients remain transfusion independent after 3 years [63]. Most of the responding patients developed pancytopenia and the myelosuppression served as a surrogate marker of clonal suppression of the del(5q) clone and predictive of the response to lenalidomide. Greater than 70% of patients with the del(5q) developed thrombocytopenia within the first 4–8 weeks of treatment and the development of thrombocytopenia was significantly correlated with a favorable response and the development of transfusion independence and a cytogenetic response [63]. A platelet decline in the first 8 weeks of treatment correlated with the response to treatment and likely reflected a direct specific cytotoxic effect of lenalidomide on the MDS clone. Most patients needed dose reductions due to myelosuppression and/or thrombocytopenia and in phase III trial comparing 5 daily and 10 mg on days 1–21 on a 28-day cycle versus placebo, the 10 mg dose was superior. Long term follow up in patients treated with lenalidomide demonstrated a prolonged duration of response, with durable transfusion independence, cytogenetic responses and extended survival with improvement in quality of life [63]. In low risk, transfusion dependent MDS patient without the del (5q) cytogenetic abnormality the response rate to lenalidomide was much less and the mechanism of action appears to be very different. The overall response rate in this non del(5q) group was 33% but only 17% became transfusion independent. A majority of the responses were characterized as a decrease in RBC transfusions as compared to the baseline transfusion requirement. There were minimal or no changes in the bone marrow morphology and documented histological and cytogenetic responses were rare. Myelosuppression, grade 3/4, neutropenia and thrombocytopenia occurred only in 20–25% of patients. Moreover, the development of cytopenias including thrombocytopenia and neutropenia on lenalidomide for patients without the del(5q) was not associated with a response to treatment. The response duration of lenalidomide in the non-del (5q) patients ranged from 3 to 85 weeks with a median of 41 weeks. The median time to response was short at 4.8 weeks and response after 16 weeks of treatment were rare and alternate treatment was recommended for patients who fail to respond after 4 months of lenalidomide. Higher responses correlated with a baseline platelet count of >150 × 109/L and shorter duration of MDS. Lenalidomide mechanism of action in MDS is clearly karyotype dependent. In del(5q) patient’s lenalidomide appears to have a direct cytotoxic effect on the dysplastic clone resulting in eradication of the malignant clone. In contrast in the lower risk transfusion dependent MDs patient without the del(5q) lenalidomide effects appear to be mediated indirectly perhaps by effecting the bone marrow microenvironment or cytokine modulation.
Low-Dose Chemotherapy
Potential Differentiating Agents
Cytarabine administered at low doses (low dose Ara-C: Lo DAC) has been the most extensively used chemotherapy for elderly patients with high-risk, symptomatic MDS [86]. Cytarabine is administered daily by either continuous infusion or bolus subcutaneous injections at doses of 10–20/mg/m2 for 14–21 days. At low dose cytarabine may induce differentiation but most likely works by a direct cytotoxicity [86]. In a prospective controlled trial patients higher risk MDS patients had the highest response rates, 20–35% (complete remission partial response [CR] + PR). The median duration of response for all subtypes was 8–15 months, with a range of 6–24 months. The response to Lo DAC correlated with its cytoreductive effect on the bone marrow. In a Phase III trial treatment with low-dose cytarabine was not superior to supportive care with regards to overall survival or leukemic transformation [86]. The role of low-dose cytarabine in the treatment of patients with high-risk MDS is controversial. In high-risk patients it remains a widely used treatment that may be effective in inducing transient responses in a subset of patients with progressive disease who are not candidates for alternative treatments. Low doses of chemotherapy may have a supportive role in selected patients with MDS. A number of trials have addressed the use of low doses of oral chemotherapy that was well tolerated and administered over a prolonged period. Low-dose oral etoposide (VP-16) and hydroxyurea were effective in controlling symptoms in some patients [87]. The use of steroids alleviated some of the cytokine-mediated symptoms associated with MDS/MPN and produced transient hematological improvements. Low-dose melphalan (2 mg/day until response or progression) in high-risk, frail patients with MDS was well tolerated and responses were noted in both hypercellular and hypocellular MDS [88]. The overall response rate to a prolonged course of low-dose melphalan in Phase II studies was approximately 40%. The duration of the responses to low-dose melphalan is unclear and additional studies are needed to determine its role in treating high risk MDS.
Histone acetylation facilitates active gene transcription and highly regulated by histone deacylases (HDACs) and histone acetyltransferases (HATs) . HDAC inhibition may restore normal acetylations of histone proteins and promote cell cycle arrest and induce apoptosis in malignant cells. Normal differentiation and cell death programs are influenced by histone modification. HDAC expression is frequently deregulated in high risk MDS and AML and is therefore a potential therapeutic target. A number of HDAC inhibitors have been developed including Valproic acid, Entinostat, Belinostat, Panobinostat, Romidepsin, Vorinostat and others in various stages of development. HDAC inhibitors have multiple potential mechanism of action leading to their pleiotropic activity and use in various disorders. The response rate for single agent HDACs is low and therefore they are combined with other agents including the DNA methyltransferase inhibitors including decitabine and azacitidine [88]. The potential synergism between demethylation and histone deacetylase inhibition made the use of combination therapy the focus of a number of ongoing trials.
DNA Methyltransferase Inhibitors
The DNA hypomethylating agents, 5-azacytidine (Azacitidine—Vidaza) and 2,5-deoxycytidine (Decitabine—Dacogen) are both analogs and the pyrimidine nucleoside cytidine. Both drugs inhibit DNA methyltransferase, reduce DNA methylation, and may induce re-expression of key tumor suppressor genes in MDS [89]. They are incorporated into the DNA of cells and result in hypomethylation of critical residues, cytosine prior to guanine sequences, (CpG) in the promoter regions in the DNA. At low doses they are believed to induce hypomethylation through depletion of cellular DNA methyltransferases and at higher doses both agents are cytotoxic by incorporation into RNA and/or DNA. The use of low doses in MDS is based on the principle that hypomethylation of DNA leads to reactivation of tumor suppressor genes expression which is passed down through subsequent generation of MDS cells.
The effect of azacitidine was evaluated in a randomized phase III trial. Azacitidine-treated patients showed a better overall response compared to those treated with supportive care only (60% versus 5%) and a longer time to progression to AML or death, but no overall survival advantage. A confirmatory international phase III trial evaluating the effects on long-term outcome with azacitidine versus conventional care (i.e., physician choice of low-dose cytarabine, standard chemotherapy, or best supportive care). Azacitidine was administered subcutaneously (75 g/m2/day) for seven consecutive days every 28 days for patients with high risk MDS. Azacitidine treatment was associated with a significantly median overall survival 24.4 months compared to 15 months in the conventional care arm [89]. Most patients in the conventional treatment arm received low dose cytarabine. The 2 year survival was 50.8% in azacitidine as compared with 26.2% in the control, conventional treatment arm. This was the first randomized study to demonstrate a survival advantage for treatment with a hypomethylating agent. While some patients had a complete clinical response while receiving Azacitidine the durations of the complete response were short and not maintained when treatment was stopped. Myelosuppression was frequently observed in patients receiving Azacitidine and its role as a differentiating agent or de repressor of tumor suppressor genes in MDS was unclear. Responses were associated and improved quality of life in some patients. But in other trials the impact of treatment on survival was unclear. An oral formulation of 5-azacitidine is being studied in patients with low risk—intermediate risk MDS.
Decitabine (DAC) is a more potent inhibitor of DNA methyltransferase than azacitidine and is associated with greater myelosuppression. Decitabine has been effective in patients with high-risk MDS and may prolong the time to transformation to AML. The schedule of decitabine administration suggests that both the duration, dose and number of doses are important. Decitabine is given intravenously at various doses and dose schedules. The Phase I, II, and early Phase III trials DAC was administered the dose was 15 mg/m2 over 3–4 h every 8 h for 3 days. The overall response rate in MDS was 49 and 64% in high-risk patients. The actuarial median survival time was 15 months and myelosuppression was common. In a randomized dose finding study, DAC was administered at 20 mg/m2 IV over 1 h daily for 5 days; while not the FDA approved dosing, it is the standard of care at many institutions [89]. The CR rate in a dose finding trial was 39% and an overall response rate of 70%. The CR rate of 34% versus 9% when decitabine was given at a higher dose with fewer and less frequent cycles. Different dosing schedule have been associated with less myelosuppression and similar efficacy. Decitabine administered weekly, or 3 days a week was associated with a 60% trilineage response with minimal hematologic toxicity [90].
Phase III randomized studies however, did not demonstrate a survival benefit with DAC in a very high risk patient population. Azacitidine and decitabine generally require 3–6 treatment cycles to obtain an optimal therapeutic response, suggesting that the mechanism of action is more than just cytoreduction. For high-risk MDS, the hypomethylating agents either azacitidine and decitabine continue to be the treatments of choice [88]. MDS patients with monosomy 7(del 7) either alone or with other complex cytogenetic abnormalities may be particularly sensitive to treatment with DNMT inhibitors. High cytogenetic responses rates have been reported with both azacitidine and decitabine in retrospective analysis and both agents appear to alter the natural course of MDS and may be of benefit for selected patients. However, additional studies are needed to define the duration of therapy, dosing and their role as single agents or in combination for high risk patients with MDS. Some trials have shown a correlation between expression of methylated genes and clinical response but this finding remains controversial. Early trials using a combination of azacitidine and lenalidomide have reported acceptable toxicity and encouraging activity albeit in limited number of selected patients. In patients with low risk disease who have failed growth factors and/or lenalidomide the use of one of low dose azacitine or decitabine is associated with decrease in transfusion requirement with acceptable toxicity.
Intensive Chemotherapy
Combination, intensive cytoreductive induction chemotherapy regimens result in meaningful toxicity and modes responses in patients with high risk MDS. The complete remission rate with intensive AML regimens is 40–60% with a 20–30% induction related mortality [88]. High risk cytogenetics, advanced age, and performance status are associated with poor response to intensive chemotherapy. In a retrospective study evaluating 510 patients with high risk MDS who received intensive chemotherapy the induction related mortality was 17% and 5 year survival probability 8% [37]. However in selected younger patients who present with poor prognosis MDS and who may proceed to an allogeneic transplant are potential candidates for intensive combination chemotherapy. Newly diagnosed patients with high risk MDS without a prior history of MDS appear to respond to standard AML induction chemotherapy in a similar fashion to de novo AML. However, patients who present with an antecedent or evolving MDS generally respond poorly to intensive AML-type induction chemotherapy [88]. The complete remission rate is 13–40% with an incidence of toxic deaths during therapy of 1–53%. Moreover, the role of post induction chemotherapy is unclear in patients with MDS who respond to treatment. In selected younger patients with MDS intensive chemotherapy including an anthracycline and cytarabine has resulted in complete remission rates of 20–60% but with a relapse rate of 90%. The remission durations are typically 6–12 months with only rare instances of prolonged disease-free survival. The poor response of MDS patients to intensive induction chemotherapy reflects the biological differences between de novo AML that occurs in younger patients and MDS. Moreover, in patients who have poor risk cytogenetics and prior MDS treatment or a longer time to progression responded poorly to induction chemotherapy with a median overall survival of less than 4 months. Moreover a CR may not impact overall survival in patients with MDS and therefore may not be the best end point for evaluating studies. The use of AML intensive induction regimens should be reserved selected younger patients with high risk disease as a bridge to an allogeneic stem cell transplant or as part of a investigational trial.
Stem Cell Transplantation
Autologous and allogeneic stem cell transplantation has been used in patients with MDS or MDS-AML. The role of autologous transplantation remains very controversial. The 3-year disease-free survival in a selected group of patients ranges from 14 to 58% in single arm or single institution studies [90]. All patients were transplanted in first remission and adequate number of stem cells were harvested. The 2-year survival in selected patients reported to the EBMT for patients in first complete remission was 39%, with a disease-free survival of 34% and a relapse rate of 64% [90]. In patients over the age of 40 years the disease-free survival was 25%. Patients younger than 40 years of age, and in first complete remission, responded better. The transplant-related mortality was high: 39% and 17% for patients over and younger than the age of 40 years, respectively. The relapse rate is higher than in patients with AML. Larger prospective studies are needed to define the potential role, if any, of an autologous stem cell transplantation for patients with MDS. However it is possible, in selected patients, to harvest polyclonal and karyotypically normal progenitors from the peripheral blood in younger patients with MDS following intensive induction chemotherapy [90].
Allogeneic stem cell transplantation represents the only potential curative therapy for patients with MDS and should be considered for patients who have an HLA compatible donor. While there are no prospective randomized trials that have compared outcomes of HSCT versus no HSCT for patients with MDS who have eligible donors it is accepted as the standard of care and generally recommended for selected low risk and all clinical eligible high risk patients with MDS [91]. However, patients with MDS have an increased incidence of transplant-related mortality as compared to patients with AML undergoing similar HSCTs [91]. The non relapse morbidity and mortality in MDS patients is high and not solely explained by the older age of the patient population [91]. Younger patients with MDS also appear to have an increased incidence of transplant-related complications. Patients with advanced disease and unfavorable cytogenetics have a higher probability of relapse and lower overall survival. The outcome is better for patients with a lower risk IPSS-R score, who are less transfusion dependent and a good performance status. Moreover, the standard risk factors that predict overall survival in MDS appear to affect the post-transplant outcome [92]. Performance status, comorbidities and fragility scores predicted overall survival [93]. Age was not the most important factor relating to transplant related morbidity and mortality [93]. The timing of the transplant for most patients remains controversial [94]. The factors that determine the overall survival and rates of relapse of an allogenic stem cell transplant include the percent of blasts, transfusion dependence, serum ferritin, comorbidities and pre transplant genetic profiles. The IPSS-R does not consider the prognostic variables associated with transplant related complications or survival but the IPSS-R score correlates with the HSCT outcome. In the IPSS-R scoring system the very high risk MDS patients had a only 10–14 months survival from the time of diagnosis and derived limited benefit from standard treatments [95]. Patients with high risk MDS should therefore be referred early in their course for consideration of an hematopoietic allogeneic stem cell transplant (HSCT) [90]. The role of HSCT in low risk MDS, while a accepted standard of care is controversial [91]. Patients with (very) low and intermediated risk IPSS-R scores with good performance status and poor, high risk features should be considered for an allogeneic hematopoietic stem cell transplant. Low risk patients with poor risk cytogenectics, life threatening cytopenias and a transfusion requirement of ≥ units a month for 6 months should be considered for early referral to a transplant center. While the percent of bone marrow blasts did not significantly effect the overall survival cytoreductive therapy prior to HSCT is recommended for patients with ≥ bone marrow myeloblasts [96]. Patients with low risk disease have a better transplant related outcome than patients with more advanced disease [96]. However, treatment related complications is a major cause of morbidity and mortality after a HSCT transplant and must be considered in advising younger patients with low risk disease. Moreover older patients with multiple co-morbidities, very poor risk cytogenetic and mutational studies should not be offered a HSCT due to the very low chance of a successful HSCT. The patients pretransplant genetic profile and mutational findings are important predictors for overall survival and should be included in a decision to recommend a HSCT. TP 53, RAS and JAK 2 mutations were associated with a signigficantly shorter overall survival following a HSCT. Mutational studies are important predictors of overall response and should be obtained on all patients prior to performing a HSCT [96]. The use of reduced intensity regimens have decreased the early transplant related mortality and are generally recommended for patients with co morbid conditions or older age. The reduced intensity regimens are associated with a decrease in non relapse mortality but a higher risk of relapse. The reduced intensity transplant depend on the immune effects mediated by the donor derived cells and graft versus disease effect. Reduced intensity transplants, however, have not impacted the overall incidence of acute and chronic GVHD which remains the major cause of morbidity and mortality in older patients. Chronic GVHD remains a serious and life long complication of HSCTs. Studies have documented the decrease in quality of life in older patients with chronic GVHD [97]. Chronic GVHD is associated with an increase in cardiovascular disease, metabolic syndrome, diabetes, cognitive decline, fatigue, sexual dysfunction and endocrine abnormalities. However, for the younger patient with a good performance status and a suitable HLA matched donor an allogeneic stem cell transplant should be considered as it represents the only potential curative therapy and should be considered earlier in high risk patients. Determining the optimal timing of the HSCT remains a controversial issue and is the subject of a number of ongoing clinical trials [97, 98].
Future Directions and Evolving Role of Molecular Genetics
Advances in treatment will parallel our understanding of the molecular and immunological events involved in development and progression of MDS. Molecular genetic technolology may help in defining the prognosis of patients with MDS [99]. In AML the use of mutational analysis has helped define the prognosis of patients with favorable or normal cytogenetics [100]. Going forward molecular genetics, including DNA array technology and whole genome sequencing (WGS) studies are likely to play a significant role in defining more biologically based prognostic scoring system. The current MDS prognosis scoring systems stratify untreated patients at the time of diagnosis. The scoring systems do not account for changes in the prognostically important covariables over time. Currently used scoring models predict outcome at diagnosis but do not predict overall survival and transformation over time. The need for a biologically based model of MDS that can reflect the heterogenous course of high and low risk patients is needed to better define therapy and evaluate long term trials. A recent large study of patients with MDS undergoing stem-cell transplantation and evaluating the association of mutations with transplantation outcomes identified subgroups of patients with prognostic and therapeutic (conditioning regimen) implications. So for example TP53 mutations in patients with MDS were associated with sorter survival and shorter time to relapse and so was presence of RAS pathway and JAK2 mutations. Knowing mutational status of these key genes along with other biological parameters will help in clinical decision making [101] (Table 23.10).
Aberrations in gene mutations are still poorly characterized in MDS. The most common point mutations in MDS are still not specific for MDS but are associated with secondary, prognostically important mutations. In addition, most cases of MDS are genetically heterogenous with a dominant clone and many subclones and based on whole genome sequencing studies (WGS) no single gene is exclusively mutated in the funding clone [102]. The combined use of flow cytometry, mutational analysis and DNA arrays may identify the most appropriate therapy for patients with MDS. A recent Genomic classification of AML defined specific genomic categories that are biologically and prognostically important [99, 100]. Hopefully a similar classification system can be developed from the large MDS data bases. Incorporating molecular genetic studies into diagnostic and prognostic models for MDS with help in defining the role of newer agents with precise targets. A biologically based system will help evaluate studies of combination with immune based treatments for different subsets of patients. While it is till unclear how somatic mutations will be applied in cases of MDS. MDS associated genes, however not specific, appear to be relevant clinical markers for the diagnosis and prognosis but have yet to be incorporated in prognostic scoring systems. More dynamic scoring systems are needed to define biologically important subtype. A molecular diagnostic system will facilitate comparing the results of different trials and assessing treatments to specific subtypes. Newer prognostic models that incorporate molecular genetic studies are being developed and validated. The use of molecular genetic studies in a predictive model may provide for a more dynamic scoring system that evolves over the patient’s course and may help in the developing targeted therapy and the timing of HSCTs [103].
Summary
The myelodysplastic syndromes are a heterogeneous group of disorders with a variable clinical course. The incidence of MDS is increasing with the aging population and now represents the most common hematologic malignancy in patients older than 60 years. A majority of MDS patients present with lower-risk MDS and do not progress to AML and die of infections or bleeding related to their MDS. The WHO classification system remains controversial but is currently accepted at the standard criteria for defining MDS and attempts to separate MDS from reactive disorders other clonal disorders. Defining and differentiating MDS from other clonal or reactive process is critical many disorders can result in dysplasia and cytopenias. Clonal cytogenetic abnormalities are helpful in establishing a diagnosis of MDS, particularly when morphologic findings are subtle. Multilineage dyspoiesis favors MDS; however, prominent dysplasia can be seen associated with chemotherapy, immunosuppressive medications, and nutritional deficiencies. The diagnosis and management of patients with MDS require the close cooperation of clinician, cytogenetist and pathologist. The application of newer molecular studies may aide in the diagnosis and planning therapy.
MDS diagnosis and classification is currently in a transitional phase from reliance almost entirely on cell morphology supplemented by cytochemistry and G-banded karyotyping, towards a new model in which molecular and perhaps immunophenotypic findings will be fully incorporated. The revised 2016 WHO MDS classification represents the new standard for the diagnosis of MDS and reflects the complexity and heterogeneity of MDS. The trend towards greater classification complexity seems likely as additional molecular and cytogenetic lesions in MDS are characterized and incorporated into the diagnosis and prognosis. It is hoped that with additional information unifying themes will emerge that will help in defining prognosis and address new therapies.
References
Santini V, Alessandrino PE, Angelucci E, et al. Clinical management of myelodysplastic syndromes: update of SIE, SIES, and GITMO practice guidelines. Leuk Res. 2010;34(12):1–13.
Dayyani F, Conley A, Strom SS, et al. Cause of death in patients with lower risk myelodysplastic syndrome. Cancer. 2010;116:2174–80.
Aber DA, Orazi A, Hasserijian R, et al. The 2016 revision to the World Health Organization classification of myeloid neoplasms and acute leukemia. Blood. 2016;127(20):2391–405.
Williamson PJ, Kruger AR, Reynolds PJ, Hamblin TJ, Oscier DG. Establishing the incidence of myelodysplastic syndrome. Br J Haematol. 2008;87:743–51.
Rollison DE, Howlader N, Smith MT, et al. Epidemiology of myelodysplastic syndromes and chronic myeloproliferative disorders in the United States, 2001–2004, using data from the NAACCR and SEER programs. Blood. 2008;112:45.
Nicolas B, Feller A, Rovo A, et al. Trends of classification, incidence, mortality and survival of MDS patients in Switzerland between 2001 and 2012. Cancer Epidemiology.2017;46:82–92.
Paydas S. Young age MDS: differences between western and eastern countries. Leuk Res. 2006;30:36–4.
Strom SS, Velez-Bravo V, Estey E. Epidemiology of myelodysplastic syndromes. Semin Hematol. 2008;45:8–13.
Du Y, Fryzek J, Sekeres MA, Taioli E. Smoking and alcohol intake as risk factors for myelodysplastic syndromes (MDS). Leuk Res. 2010;34:1–8.
Nisse C, Lorthois C, Dorp V, et al. Exposure to occupational and environmental factors in myelodysplastic syndromes. Preliminary results of a case control study. Leukemia. 1995;9:693.
Iwanaga M, Wan-Ling H, Soda M, et al. Risk of myelodysplastic syndromes in people exposed to ionizing radiation: a retrospective cohort study of Nagasaki atomic bomb survivors. J Clin Oncol. 2012;29:428–34.
Weimar IS, Bourhis J-H, de Gast GC, et al. Clonality in myelodysplastic syndromes. Leuk Lymphoma. 1994;13:215.
Busque L, Zhu J, Dehart D, et al. An expression based clonality assay at the human androgen receptor locus (HUMARA) on chromosome X. Nucleic Acids Res. 1994;2:697.
Ades LIR, Fanaux P. Myelodysplastic syndromes. Lancet. 2014;383:2239–52.
Chakraborty S, Sun C-L, Francisco L, et al. Accelerated telomere shortening precedes the development of therapy-related myelodysplasia or acute myelogenous leukemia after autologous transplantation for lymphoma. J Clin Onc. 2009;27:791.
Ohyashiki JH, Sasida G, Tauchi T, Ohyashiki K. Telomeres and telomerase in hematologic neoplasms. Oncogene. 2002;21:680.
Brummendorf TH, Balbanov S. Telomere length dynamics in normal hematopoiesis and in disease states characterized by increased stem cell turnover. Leukemia. 2006;20:1706.
Lange K, Vang Nielsen K, Hahn A, et al. Telomere shortening and chromosome instability in myelodysplastic syndromes. Genes Chromosomes Cancer. 2010;49:260.
Bejar R, Levine R, Ebert BL. Unraveling the molecular pathophysiology of myelodysplastic syndromes. J Clin Oncol. 2011;29:507–15.
Cogle RC, Saki N, Khodadi E, et al. Bone arrow niche in myelodysplastic syndromes. Leuk Res. 2015;39:1020–7.
Marcids AM, Ramakrishnan A, Deeg HJ. Myeloid malignancies and the microenvironment: some recent studies in patients with MDS. Curr Cancer Ther Rev. 2009;5(4):310.
Paul B, Reid MM, Davidson EV, et al. Familial myelodysplasia: progressive disease associated with emergence of monosomy 7. Br J Haematol. 1987;65:321.
Bejar R, Stevenson K, Abdel-Wahab O, et al. Clinical effect of point mutations in myelodysplastic syndromes. N Engl J Med. 2011;364:2496–506.
Zou Z, Calin GA, de Paula HM, et al. Circulating microRNAs let −7a and miR-16 predict progression—free survival and overall survival in patients with myelodysplastic syndome. Blood. 2011;118:413–5.
Steensma DP, List AF. Genetic testing in the myelodysplastic syndromes: molecular insights into hematologic diversity. Mayo Clin Proc. 2005;80:681–98.
Bejar R. Myelodysplastic syndrome diagnosis: what is the role of molecular testing? Curr Hematol Malig Rep. 2015;10(3):282–91.
Busque L, Patel JP, Figueroa ME, et al. Recurrent somatic TETS mutations in normal elderly individual with clonal hematopoiesis. Nat Genet. 2012;44:1179–81.
Welch JS, Ley TJ, Lin DC, et al. The origine and evolution of mutations in acute myeloid leukemia. Cell. 2012;150:264–74.
Jaiswal S, Fontanillas P, Flannick J, et al. Age related clonal hematopoiesis associated with adverse outcomes. NEJM. 2014;371:2488–98.
Steensma DP. Cytopenias + mutations-dysplasia=what? Blood. 2015;126(21):2349–51.
Steensma DP, Bejar R, Jaiswai S, et al. Clonal hematopoiesis of indeterminate potential and its distinction from myelodysplastic syndromes. Blood. 2015;126:9–16.
Xie M, Lu C, Wang J, et al. Age-related mutations associated with clonal hematopoiesis with adverse outcomes. N Engl J Med. 2014;371(26):1472–8.
Naiswal S, Fontanillas P, Flannick J, et al. Clonal hematopoiesis and blood –cancer risk inferred from blood DNA sequence. N Engl J Med. 2014;371(26):2488–98.
Bejar R. Myelodysplastic syndromes diagnosis: what is the role of molecular testing. Cur Hematol Malig Rep. 2015;10:282–91.
Barrett AJ, Sloand E. Autoimmune mechanisms in the pathophysiology of myelodysplastic syndromes and their clinical relevance. Haematolog. 2009;94:449–51.
West RR, Stafford DA, White AD, et al. Cytogenetic abnormalities in the myelodysplastic syndromes and occupational or environmental exposure. Blood. 2000;95:2093.
Bollag G, Clapp DW, Shih S, et al. Loss of NFI results in activation of the RAS pathway and leads to aberrant growth in hematopoietic cells. Nat Genet. 1996;12:144.
Rothman N, Smith MT, Hayes RB, et al. Benzene poisoning, a risk factor for hematological malignancy, is associated with the NQOI 609 C.T mutation and rapid fractional excretion of chlorzoxazone. Cancer Res. 1997;57:2839–44.
Larson RA, Wang Y, Banarjee M, et al. Prevalence of the inactivating 609 C.T polymorphism in the NAD(P)Quinone oxidoreductase (NQO1) gene in patients with primary and therapy-related myeloid leukemias. Blood. 1999;94:803.
Wiernals JL, Pagnamenta A, Taylor GM, et al. A lack of functional NAD(P)Quinone ox reductase allele is selectively associated with pediatric leukemias that have MLL fusions. Cancer Res. 1999;59:4095–9.
Larson RA, Le Beau MM. Therapy related myeloid leukemia: a model for leukemogenesis in humans. Chem Biol Interact. 2005;153–154:187–95.
Zeidan AM, Linhares Y, Gore SD. Current therapy of myelodysplastic syndromes. Blood Rev. 2013;27:243–50.
Bennett JM, Catovsky D, Daniel MT, et al. Proposals for the classification of the myelodysplastic syndromes. Br J Haematol. 1982;51:189.
Verhoef GE, Pittaluga S, De Wolf-Peters C, et al. FAB classification of myelodysplastic syndromes: merits and controversies. Ann Hematol. 1995;71:3.
Vardiman JW, Thiele J, Arber DA, et al. The 2008 revision of the WHO classification of myeloid neoplasms and acute leukemia: rationale and important changes. Blood. 2009;114:947.
Swerdlow SH, Campo E, Harris NL, Jaffe ES, Pileri SA, Stein H, Thiele J, Vardiman JW, editors. WHO classification of tumours of haematopoietic and lymphoid tissues. Lyon: International Agency for Research on Cancer; 2008. p. 88–107.
Font P, Loscertales J, Benavente C, et al. Inter-observer variance with the diagnosis of myelodysplastic syndromes (MDS) following the 2008 WHO classification. Ann Hematol. 2013;92(1):19–24.
Valent P, Horney HP, Bennett JM, et al. Definitions and standards in the diagnosis and treatment of the myelodysplastic syndromes: consensus statements and report from a working conference. Leuk Res. 2007;31:727.
Cunningham JM, Patnail MM, Hammerschmidt DE, Vercellotti GM. Historical perspective and clinical implications of the Pelger-Huet cell. Am J Hematol. 2009;84:116.
Haase D, Germing U, Schanz J, et al. New insights into the prognostic impact of the karyotype in MDS and correlation with subtypes: evidence from a core dataset of 2124 patients. Blood. 2007;110:4385–95.
Mughal TI, Cross NC, Padron E, et al. An international MDS/MPN working Group’s perspective and recommendations on molecular pathogenesis, diagnosis and clinical characterization of myelodysplastic/myeloproliferative neoplasms. Haematologica. 2015;100(9):1117–30.
Foucar K. Myelodysplastic/myeloproliferative neoplasms. Am J Clin Pathol. 2009;132(2):282–92.
Kwork B, Hall JM, Witte JS, et al. MDS associated somatic mutations and clonal hematopoiesis are common in idiopathic cytopenias of indeterminant significance. Blood. 2015;126(21):2355–61.
Vardiman JW. The World Health Organization (WHO) classification of tumors of the hematopoietic and lymphoid tissue: an overview with emphasis on the myeloid neoplasm. Chem Biol Interact. 2010;184:16–23.
Della Porta MG, Malcovati L, Boveri E, et al. Clinical relevance of bone marrow fibrosis and CD34-positive cell clusters in primary myelodysplastic syndromes. J Clin Oncol. 2009;27:754.
MalcovatiL KM, Papaemmanuil E, et al. SF3B1 mutation identifies a distinct subset of myelodysplastic syndrome with ring sideroblasts. Blood. 2015;126:233–41.
Malcovati L, Karimi M, Papaemmanuil E, et al. SF3B1 mutation identifies a distinct subset of myelodysplastic syndrome with ring sideroblasts. Blood. 2015;126(2):233–1.
Apaemmanuil E, Cazzola M, Boultwood J, et al. Chronic myeloid disorders working group of the International Cancer Genone Consortium. Somatic SF3B1 mutation in myelodysplasia with ring sideroblasts. N Engl J Med. 2011;365(15):3376–82.
Gregg XT, Reddy V, Prchal J. Copper deficiency masquerading as myelodysplastic syndrome. Blood. 2002;100:1493–5.
Irving JA, Mattman A, Lockitcg G, Farrell K. Wadsworth. Element of caution: a case of reversible cytopenias associated with excessive zinc supplementation. CMAJ. 2003;169(2):129–31.
Valent P, Bain BJ, Bennett JM, et al. Idiopathic cytopenia of undetermined significance(ICUS) and idiopathic dysplasia of uncertain significance (IDUS) and their distinction from low risk MDS. Leuk Res. 2011;35:1016.
Kwok B, Hall JM, Witte JS, et al. MDS—associated somatic mutations and clonal hematopoiesis are common in idiopathic cytopenias of undetermined significance. Blood. 2015;126(21):2355–61.
Gaballa M, Basa E. Myelodysplastic syndromes with 5q deletion: pathophysiology and role of lenalidomide. Ann Hematol. 2014;93:723–33.
Komrokji RS, List AF. Short and long- term benefits of lenalidomide treatment in patients with lower-risk del (5q) myelodysplastic syndromes. Ann Oncol. 2016;27(1):62–8.
Komrokji RS, Padron E, Ebert BL, List AF. Deletion 5qMDS: molecular and therapeutic implications. Best Pract Res Clin Haematol. 2013;26:365–75.
Brierley CK, Steensma DP. Thrombopoiesis- stimulating agents and myelodysplastic syndromes. Br J Haematol. 2015;169:309–23.
Bussel JB. The new thrombopoietic agenda: impact on leukemias and MDS. Best Pract Res Clin Haematol. 2014;27:288–92.
Morrone WL, Kambhampati S, Will B, Steidl U, Verma A. Thrombocytopenia in MDS: epidemiology, mechanisms, clinical consequences and novel therapeutic strategies. Leuk. 2016;30:536–44.
Greenberg PL, Tuechier H, Schanz J, et al. Revised international prognostic scoring system for myelodysplastic syndromes. Blood. 2012;120:2454–65.
Zeidan AM, Sekeres MA, Garcia-Manero G, et al. Comparison of risk stratification tools in predicting outcomes of patients with higher—risk myelodysplastic syndromes treated with aza nucleosides. Leukemia. 2016;30(3):649–57.
Cheson BD, Greenberg PL, Bennett JM, et al. Clinical application and proposal for modification of the International Working Group (IWG) response criteria in myelodysplasia. Blood. 2006;108:419.
Chan G, DiVenuti MK. Danazol for the treatment of thrombocytopenia in patients with myelodysplastic syndromes. Am J Hemat. 2002;71:166–71.
Giagounidis A, Mufti GJ, Fenaux P, et al. Results of a randomized double blind study of romiplostim versus placebo in patients with low/intermediate −1-risk myelodysplastic syndrome and thrombocytopenia. Cancer. 2014;120:1838–46.
Negrin RS, Haeber DB, Nagler A, et al. Maintenance treatment of patients with myelodysplastic syndromes using recombinant human granulocyte colony—stimulating factor. Blood. 1990;76:36–43.
Steensma DP, Gattermann N. When is ion overload deleterious, and when and how should iron chelation therapy be administered in myelodysplastic syndromes. Best Pract Res Clin Haematol. 2013;26(4):431–44.
Pullark V. Objectives or iron chelation in myelodysplastic syndromes: more than meets the eye. Blood. 2009;114:5251–62.
Maurillo L, Breccia M, Voso MT, et al. Deferasirox chelation therapy in patients with transfusion—dependent MDS: a ‘real-world’ report from two Italian registries: Gruppo Romano Myelodysplasia and Registro Basilicata. Eur J Haematol. 2015;95(1):52–6.
Armand P, Kim HT, Cutler CS, et al. Prognostic impact of elevated pretransplant serum ferritin in patients undergoing myeloablative stem cell transplantation. Blood. 2007;114:5251–5.
Rachmilewitz E, Merkel D, Ghoti H, et al. Impovement of oxidative stress parameters in MDS patients with iron overload treated with deferasirox. Blood. 112:924–31.
Greenberg PL, Sun Z, Miller KB, et al. Treatment of myelodysplastic syndrome patients with erythropoietin with or without granulocyte colony stimulating factor: results of a prospective randomized phase 3 trial by the Eastern Cooperative Oncology Group (E1996). Blood. 2009;114:2393–400.
Steesnama DP. Myelodysplastic syndromes: diagnosis and treatment. Mayo Clin Proc. 2015;90(7):969–83.
Sloand EM, Wu CO, Greenberg P, et al. Factors affecting response and survival in patients with myelodysplasia treated with immunosuppression. J Clin Oncol. 2008;26:2505–11.
Calado RT. Immunologic aspects of hypoplastic myelodysplastic syndrome. Semin Oncol. 2011;38(5):667–72.
Passweg JR, Giagounidis AA, Simcock M, et al. Immunosuppressive therapy for patients with myelodysplastic syndrome: a prospective randomized multicenter phase III trial comparing antithymocyte globulin plus cyclosporine with best supportive care-SAKK 33/99. J Clin Oncol. 2011;29(3):303–9.
Fanaux P, Giagounidis A, Selleslag D, et al. A randomized phase 3 study of lenalidomide versus placebo in RBC transfusion dependent patients with low−/intermediate 1 risk myelodysplastic syndromes with del5q. Blood. 2011;118(14):3765–76.
Miller K, Kyungmann K, Morrison FS, et al. The evaluation of low dose cytarabine in the treatment of myelodysplastic syndromes: a phase III intergroup study. Ann Hematol. 1992;65:162–9.
Sekeres MA, Cutler C. How we treat higher–risk myelodysplastic syndromes. Blood. 2014;123(6):829–36.
Malcovati L, Hellstrom-Lindberg E, Bowen D, et al. Diagnosis and treatment of primary myelodysplastic syndromes in adults recommendations from the European leukemia net. Blood. 2013;122(17):2943–64.
Issa RF, Garcia-Manero G, Obrien S, et al. Superior outcome with hypomethylating therapy in patients with acute myeloid leukemia and high risk myelodysplastic syndrome and chromosome 5 and 7 abnormalities. Cancer. 2009;115:5746–51.
Majhail NS, Farnia SH, Carpenter PA, et al. Indications for autologous and allogeneic hematopoietic cell transplantation: guideline from the American Society for Blood Marrow Transplantation. Biol Blood Marrow Transplant. 2015;21(11):1863–9.
Michaelis LC, Hamadani DJ, Hari PN. Hematopoietic stem cell transplantation in older persons: respecting the heterogeneity of age. Exp Rev Hematol. 2014;7:321–4.
Garcia-Manero G, Jabbour E, Borthakur G, et al. Randomized open-label phase II study of decitabine in patients with low—or intermediate risk myelodysplastic syndromes. J Clin Oncol. 2013;31(20):2548–53.
Buckstein R, Wells RA, Zhu N, et al. Patient –related factors independently impact survival in patients with myelodysplastic syndrome: an MDS-CAN prospspective study. Br J Haematol. 2016;174:88–101.
Estey E. Acute myeloid leukemia and myelodysplastic syndromes in older patients. J Clin Oncol. 2007;25:1908–15.
Germing U, Kundgen A. Prognostic scoring systems in MDS. Leukemia Res. 2012;36:1463–9.
de Witte T, Bowen D, Robin M, et al. Allogeneic hematopoietic stem cell transplantation for MDS and CMML :recommendations from an international expert panel. Blood. 2017;129:1753–62.
Della Porta MG, Alessandrino EP, Bacigalupo A, et al. Predictive factors for he outcome of allogeneic transplantation in patients with MDS stratified according to the revised IPSS-R. Blood. 2014;123(15):2333–42.
El-Jawahri A, Pidala J, Inamoto Y, et al. Impact of age on quality of life, functional statusand survival with chronic graft versus host disease. Biol Blood Marrow Transplant. 2014;20(9):1341–8.
He R, Witkor AE, Durnick DK, et al. Bone marrow conventional karyotyping and fluorescence in situ hybridization. AM J Clin Path. 2016;146:86–94.
Papaemmauil E, Gerstung M, Bullinger L, et al. Genomic classification and prognosis in acute myeloid leukemia. N Engl J Med. 2016;374:2209–21.
Lindsley RC, Saber W, Mar BG, et al. Prognostic mutations in myelodysplastic syndrome after stem-cell transplantation. N Engl J Med. 2017;376:536–47.
Walter MJ, Shen D, Shao J, et al. Clonal diversity of recurrently mutated genes in myelodysplastic syndromes. Leukemia. 2013;27(6):1275–82. https://doi.org/10.1038/leu.2013.58.
Pfeilstocker M, Tuechler H, Sanz G, et al. Time dependent changes in mortality and transformation risk in MDS. Blood. 2016;128:902–10.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2018 Springer International Publishing AG, part of Springer Nature
About this chapter
Cite this chapter
Miller, K., Pilichowska, M. (2018). The Myelodysplastic Syndromes. In: Wiernik, P., Dutcher, J., Gertz, M. (eds) Neoplastic Diseases of the Blood. Springer, Cham. https://doi.org/10.1007/978-3-319-64263-5_23
Download citation
DOI: https://doi.org/10.1007/978-3-319-64263-5_23
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-64262-8
Online ISBN: 978-3-319-64263-5
eBook Packages: MedicineMedicine (R0)