Abstract
The goals of this chapter are to provide an introduction into the variety of animal models available for studying traumatic brain injury (TBI) and to provide a concise systematic review of the general materials and methods involved in each model. Materials and methods were obtained from a literature search of relevant peer-reviewed articles. Strengths and weaknesses of each animal choice were presented to include relative cost, anatomical and physiological features, and mechanism of injury desired. Further, a variety of homologous, isomorphic/induced, and predictive animal models were defined, described, and compared with respect to their relative ease of use, characteristics, range, adjustability (e.g., amplitude, duration, mass/size, velocity, and pressure), and rough order of magnitude cost. Just as the primary mechanism of action of TBI is limitless, so are the animal models available to study TBI. With such a wide variety of available animals, types of injury models, along with the research needs, there exists no single “gold standard” model of TBI rendering cross-comparison of data extremely difficult. Therefore, this chapter reflects a representative sampling of the TBI animal models available and is not an exhaustive comparison of every possible model and associated parameters. Throughout this chapter, special considerations for animal choice and TBI animal model classification are discussed. Criteria central to choosing appropriate animal models of TBI include ethics, funding, complexity (ease of use, safety, and controlled access requirements), type of model, model characteristics, and range of control (scope).
Access provided by CONRICYT – Journals CONACYT. Download protocol PDF
Similar content being viewed by others
Key words
- Traumatic brain injury TBI
- Animal models
- Homologous
- Predictive
- Static dynamic
- Isomorphic/induced
- Direct indirect
- Penetrating
- Non-penetrating
1 Introduction
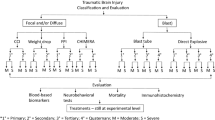
The use and application of in vivo animal models to human traumatic brain injury (TBI) research is widespread and very diverse. With numerous models available, researchers must consider their aims when choosing appropriate animal models. In general, animal models are categorized as homologous , isomorphic/induced [1], or predictive [2]. Homologous animal models mimic all aspects of a condition from causes to symptoms and treatment enabling biophysical, cellular/molecular, and behavioral assessments. Isomorphic or induced animal models share the same cellular/molecular mechanisms , symptoms and treatments but the cause is inflicted with laboratory equipment versus the actual cause in humans thus limiting biophysical assessments. These are the most common animal models used in TBI research. Predictive animal models only replicate the effect of a treatment or a single aspect of a multifaceted condition. This method is commonly used for screening and validating localized aspects of a condition when researchers do not know the underlying cause(s).
Animal models of TBI are further classified according to the mechanism and characteristics of injury desired. Moshang [3] compared diffuse and mechanical TBI while Cernak [4] further divided mechanical TBI models into static and dynamic TBI. Static TBI is defined as a localized and crushing injury via physical manipulation of tissue such as pinching a nerve with forceps [5] and allows for direct correlation of specific nerve damage to a particular neuropsychological outcome . While the amplitude and duration are predetermined and considered constant in static crushing injuries, acceleration and velocity are not considered as contributing factors to static injuries [4]. Alternatively, a dynamic TBI model may inflict contra coup damage to the brain due to transfer of forces, a ricochet/rebound effect of the brain within the skull, and/or stretching of tissue, including nerves and blood vessels as well as decreased blood flow due to inflammation [6]. Such dynamic TBI models are adjustable in amplitude, duration, velocity, and acceleration that may impact the entire body versus only a single nerve or tissue. Dynamic TBI models can be considered as either direct, or indirect . All models utilize anesthesia to minimize animal suffering during the injury and hence it is not considered as an advantage or limitation to any of the models.
With such a wide variety of available animals, types of models, mechanisms , and characteristics of injury, no single “gold standard” model of TBI exists. Therefore, comparing data across studies is very difficult. Criteria central to choosing appropriate animal models of TBI include: anatomy, physiology, cost, complexity (ease of use, safety, and controlled access requirements), type of model, model characteristics, and range of control (scope). This chapter aims to elaborate on these central criteria.
2 Materials
2.1 Animal Selection and Preparation
Anatomical and physiological features are critical to consider with respect to the aims of the research. The most common candidates for TBI animal models are rodents and porcine animals. Rodents and porcine animals are commonly used in TBI research; however, the larger animals are more expensive than smaller animals. Less common candidates for TBI animal models are nonhuman primates, canine, feline, chinchilla, and ferret. Not only is the initial cost of the animal important, but also ongoing animal care and complex assays which are necessary to inflict, support, and sustain the research.
Anatomically, the mechanism of injury should provide accurate and precise results scalable to the organism chosen. Consider hitting a small rodent with the same force as a football player—survival would be in jeopardy. The elasticity, porosity and thickness of the skull are significant issues to consider animal models seeking to replicate child abuse and/or TBI among the elderly. Additionally, a strong framework of physics is necessary to adequately quantify and validate a model’s amplitude, duration, velocity, and acceleration for consistency. These parameters should be correlated with the severity and symptomology of the injury inflicted—the more severe the impact, the more severe the symptoms. The Lab Animal Buyer’s Guide [7] provides detailed and current information on hundreds of laboratory animal suppliers and associated products such as biohazard equipment, euthanasia products, restraint equipment, and monitoring supplies.
Physiological features such as proteomics need to be considered if the intent of the research is to identify protein effects. If a particular organism does not have homologous biochemistry to humans then an isomorphic or induced model is not appropriate as primary and secondary injury cascades might differ [8]. Alternatively, if a biomechanical study aims to investigate the biophysics of the injury, then the molecular makeup of the organism is not necessarily a significant factor to consider as compared to the specific mechanical insult. For example, a military helmet manufacturer may be interested in the rebound and pressure changes within the skull as a result of blast overpressure, but may not be interested in the secondary molecular cascades that result from such an insult.
2.1.1 Rodents
Rats and mice are used extensively in TBI testing. The specific species used will depend on the aims of the research. For instance, a species should be chosen that does not float if the intent is to conduct water navigation studies. The two primary advantages of using rodents are cost and versatility (e.g., the ability to use in a wide variety of models to include ability to position the animal at the mouth of a shock tube such that they can be enveloped by blast, as a human would be in a free-field exposed to blast. The primary disadvantage is that the rat and mouse brain differs substantially in size and structure from a human brain. Without scaling laws to account for these differences, testing these species may be challenged in yielding relevant load thresholds to an adult human. However, if scaling laws between a rodent and human can be accurately identified, then the significant volume of historical data on rats and mice would be of greater value to the TBI research community. Furthermore, many knockout mice exist and abundant behavioral assessments are available for use with rodents which make them a more appealing choice for many scientists.
Anatomically, rodents are lissencephalic and have very large olfactory bulbs but small cerebral cortex that is arranged differently than the human cortex; therefore, the location of TBI must be considered and controlled. However, only small organisms (less than or equal to approximately 280 g) are able to fit in most high resolution magnetic resonance imaging (MRI) devices. Physiologically, rodents show striking similarities to humans lending to their common use in biomedical research. However, care must be taken to maintain vital signs as close to normal as possible. Average animal vitals are shown in Table 1.
Alternatives to rats and mice still within the rodent species include guinea pigs. Guinea pigs have more gyra than a rat brain. Both rodents and guinea pigs are relatively inexpensive to test and manage, thus enabling evaluation of a large number of subjects in a relatively short time. The relatively inexpensive cost of rodents and guinea pigs also enable the determination of optimum methods prior to application on more expensive animals.
2.1.2 Porcine (and Ovine) Animals
Porcine specimens have been commonly used for TBI testing over the last decade [9–12]. The porcine model provides a larger animal to facilitate scaling to the human brain based upon the gyrencephalic macrostructure and overall size of the brain. This allows thresholds of injury in porcine brain to be more readily translatable to human injury thresholds than rodent. Pigs can be acquired with a similar body mass to humans and although the frontal and midbrain skull are generally thicker in pigs than in humans [13] porcine and human parietal skull thicknesses are similar. In a CT study of 180-lb female pigs, the average thickness was 9.7 ± 1.7 mm while for humans, the average thickness is 7.2 ± 1.7 mm for females and 6.6 ± 1.3 mm for males [13]. Increased anatomical complexity of the pig brain allows for more sophisticated assessments of regional differences in injury. The distribution of many neurotransmitter uptake sites in pigs corresponds very closely to that in the brain of humans [14]. Overall, pigs are very similar to humans in general physiology (similar homeostatic mechanisms , similar shock response). The primary disadvantage to porcine research is the expense of managing large, hoofed species for animal testing.
2.1.3 Nonhuman Primates
Non-human primates are the most biofidelic surrogates available. The regional and vascular anatomies as well as cervical range are more similar to humans than lower order gyrencephalic animals. Furthermore, non-human primates can accommodate high order neurobehavioral testing, allowing for improved clinical correlation between behavioral deficit and observed tissue or physiological injury. However, despite the advantages of the nonhuman primates, research with these models is not common because it is typically much more expensive. Often, these models will not be approved by institutional animal care and use committees secondary to considerations related to pain and suffering of this high-order animal.
2.1.4 Canines, Felines, Chinchillas, and Ferrets
Canine and feline subjects have some structural similarities, and though they are large enough to perform detailed brain imaging, they present skull thickness and mass scaling challenges. Physiologically, their brains are organized differently than those of humans, thus further complicating translation [15]. However, as companion animals, the use of canine and feline species is accompanied by more significant animal usage concerns [16]. Chinchillas and ferrets present many of the same advantages and issues as do rats, but there is a paucity of historical data on their use in TBI experimentation. Ferrets have similar brain anatomy in that they are gyrencephalic [17], thus enabling determination of scaling factors from brain geometry and structure.
2.2 Animal Preparation
All animals should be anesthetized with a pre-approved agent prior to surgery and maintained under anesthesia throughout the procedure. In addition to anesthetics, each static and direct dynamic animal model has commonly used materials. The materials listed below are typically necessary for every model, regardless of the nature of the model or the type of animal used. Materials that are unique to each model are listed within subsequent sections.
-
1.
Laboratory scale proportional to animal.
-
2.
Electric hair shaver.
-
3.
Autoclave.
-
4.
10 % Ethanol and/or dry sanitizer.
-
5.
Povidone iodine.
-
6.
70 % Isopropyl alcohol.
-
7.
Scalpel.
-
8.
Hemostats.
-
9.
Forceps.
-
10.
Retractors.
-
11.
Sterile saline.
-
12.
Sterile cotton-tipped applicators.
-
13.
Sterile gauze.
-
14.
Trephine or some other microdrill and drill-bit.
-
15.
Suture monofilament and suture proportional to animal.
2.3 Static TBI Materials
The first main category of TBI is static. The key differentiators of static from dynamic TBI are the lack of movement and the confinement of the primary mechanism of injury to a specific, defined region of the brain. Compression is the primary static model used in animal research.
2.3.1 Compression Materials
-
1.
Clock to time duration of compression.
-
2.
Iridectomy scissors.
-
3.
Marker (e.g., powdered carbon).
2.4 Direct Dynamic TBI Materials
The second main category of TBI is direct dynamic (here forward referred to as direct). Direct TBI models may or may not impact and/or penetrate the skull and/or cortex of the animal. Direct impact TBI is the typical injury, the layman assumes as the sole mechanism of TBI. Although there are many impact-driven mechanisms of TBI, other models do exist. Impact TBI models mimic mechanisms ranging from penetrating head injury due to automobile accidents and military relevant mechanisms (ballistics) to sports and elderly related concussions. These direct-impact models may or may not penetrate the skull and may or may not involve constraining the animal while enduring the injury.
2.4.1 Penetrating Constrained (Percussion) Direct Brain Deformation
Penetrating constrained (percussion) direct brain deformation is a type of dynamic penetrating injury whereby the organism is constrained while the injury is inflicted. There are many specific models that fall within this category; however, most do not generate long-term TBI signs and symptoms. Instead, many of these models offer localized anatomical evaluations.
2.4.1.1 2.4.1.1 Fluid Percussion Injury (FPI) Materials
-
1.
Stereotaxic frame.
-
2.
FPI device consisting of a Plexiglas cylindrical reservoir restricted at the distal end by a rubber-covered Plexiglas piston and with the proximal end having a built-in transducer housing as well as a central injury screw or luer-loc needle hub fixed to the animal’s skull.
-
3.
Pressure transducer.
-
4.
Oscilloscope.
2.4.1.2 2.4.1.2 Controlled Cortical Impact (CCI) Materials
-
1.
Stereotaxic frame.
-
2.
CCI device.
-
3.
Dental cement, or bone wax (optional).
2.4.1.3 2.4.1.3 Vacuum/ Suction (Suction Ablation) Materials
-
1.
Stereotaxic frame.
-
2.
Fine glass Pasteur pipet.
-
3.
Measurable, controlled vacuum.
-
4.
Dental cement, or bone wax (optional).
2.4.1.4 2.4.1.4 Zymosan Materials
-
1.
Stereotaxic frame with injector and syringe.
-
2.
Hand-held drill.
-
3.
Zymosan.
2.4.1.5 2.4.1.5 Cryolesion Materials
-
1.
Stereotaxic frame.
-
2.
Metal cylinder (typically copper) proportional to animal size.
-
3.
Liquid nitrogen.
-
4.
Clock to time duration of cryolesion.
2.4.1.6 2.4.1.6 Stab Materials
-
1.
Stereotaxic frame.
-
2.
Guide cannula.
-
3.
22 G Needle.
-
4.
Dental cement, or bone wax.
-
5.
Razor blade.
-
6.
Clock to time duration of stab.
2.4.1.7 2.4.1.7 Epidural Mass Lesion (EML) Materials
-
1.
Stereotaxic frame.
-
2.
Latex surgical balloon with mitered valve.
-
3.
Penetrating ballistic brain injury (PBBI) probe or customized needle.
-
4.
Latex balloon with mitred valve.
-
5.
Variable pressure waveform generator.
-
6.
Dental cement, or bone wax.
-
7.
Clock to time duration of inflation and deflation.
2.4.1.8 2.4.1.8 HVM Materials
-
1.
Stereotaxic frame (if constrained).
-
2.
Ballistics (proportional to animal).
-
3.
Firearm.
-
4.
High-speed video.
2.4.1.9 2.4.1.9 Penetrating Ballistic Brain Injury (PBBI) Materials
-
1.
Stereotaxic frame.
-
2.
Latex surgical balloon with mitered valve.
-
3.
PBBI probe or customized needle.
-
4.
Latex balloon with mitred valve.
-
5.
Variable pressure waveform generator.
-
6.
Dental cement, or bone wax.
-
7.
Clock to time duration of inflation and deflation.
2.4.2 Direct Dynamic Non-penetrating TBI
Similar to direct dynamic penetrating brain deformation TBI models, direct dynamic non-penetrating TBI can be either constrained or not. However, non-penetrating TBI models alleviate the concern of additional damage by craniotomy.
Non-impact models that initiate movement of the brain within the skull without displacing the head laterally are also categorized as direct dynamic non-penetrating TBI. Safety concerns are significantly less pronounced in non-impact models. Rapid rotation is such a model which causes the characteristic diffuse axonal injury not replicable in non-rotational models. The nonhuman primate model [18, 19] delivers a single rotation of variable degree and acceleration. Porcine animal models are used in a similar device controlled pneumatically via a snout clamp [20]. Although this model accurately replicates the diffuse axonal injury most characteristic of human TBI, the use of large animals is more expensive and requires more technical equipment. A similar model for small animals is not currently available.
2.4.2.1 2.4.2.1 Concussion Materials
-
1.
CCI device.
-
2.
Plate or cone to affix to skull.
-
3.
Cushion customized to allow predetermined movements during and after impact.
2.4.2.2 2.4.2.2 Unconstrained Impact Acceleration Materials
-
1.
Plate or cone to affix to skull.
-
2.
Cushion customized to allow predetermined movements during and after impact.
-
3.
Weight drop device and weight.
2.4.2.3 2.4.2.3 Weight Drop Materials
-
1.
Plate or cone to affix to skull.
-
2.
Dental cement if investigating a penetrating injury.
-
3.
Weight drop device and weight.
2.5 Indirect Dynamic TBI
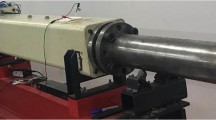
The second main category of dynamic TBI is indirect. Blast TBI is the newest addition to the animal models of TBI and is the main type of indirect TBI. Instead of direct impact, blast TBI uses compressed air, live explosives, or an LISW to reproduce overpressure injuries. Original blast TBI models exposed entire organisms to over- and under-pressure. The most commonly used species for evaluating blast exposure are rodents and pigs. Scientists quickly identified multiple traumas to other organs besides the brain—mainly lung damage. With new body armor available to protect the body, the model was modified to only blast the head. Several companies have developed compressed air driven shock tubes that deliver an adjustable pressure over variable durations, distances, and angles to rodents. Many aspects of shock tubes are adjustable. For example, a pressure-sensitive membrane ruptures at specific pressures and releases a rapid overpressure. The type and thickness of the membrane, tube-length, and initial pressure determine the peak pressure. The diameter of the exit can be altered to change the duration of the overpressure. Typical peak overpressure ranges from 154 to 340 kPa [Standard atmospheric pressure is 101 kPa (1 atm)] but can be increased to over 10 kPa. To further complicate the blast TBI model, the organism can be located on or off axis (directly in line, or offset from the blast center) and at varying distances from the blast tube exit. Multiple expensive pressure sensors with associated software are necessary to monitor the resulting pressure. As the membrane ruptures, a loud noise is generated reaching (120–160 Db depending on the dimensions of the shock tube ) similar to a gunshot sound. Typically, military personnel are limited to a maximum peak of 140 dB [21]. Therefore, shams must include exposure to anesthesia and sound only with no blast to account for potential effects due to high Db exposure and researchers must wear hearing protection. Alternatively, no incisions are made as in the direct models of TBI thus eliminating unrelated damage and allowing for biomechanical evaluations in addition to cellular, molecular, and behavioral assessments.
The use of live explosives complicates every aspect of experimentation from execution to evaluation by introducing changes in thermal load and gas byproducts of the explosion, not to mention potential fragmentation. An additional challenge faced with live explosives is reducing the scale of blast exposure for small organisms. Existing software, such as Conventional Weapons software and Bowen Curves to determine survivability at various standoff distances, are geared toward calculating acceptable impulse (mechanical energy), peak overpressure, and charge size for humans. Safety precautions include clearance for handling explosives, adequate standoff from the explosive site, and ensuring the area is clear prior to returning to the explosion site, to name a few.
2.5.1 Pneumatic Blast Materials
-
1.
Compressed air or other gas.
-
2.
Previously characterized shock tube and associated accessories to include hearing protection.
-
3.
Pressure transducers.
-
4.
Video camera.
2.5.2 Live Blast Materials
-
1.
Explosive charge.
-
2.
Previously characterized blast tube and associated accessories to include hearing protection.
-
3.
Pressure transducers.
-
4.
Video camera.
2.5.3 Laser-Induced Shock Wave (LISW) Blast Materials
-
1.
Laser source (neodymium: yttrium-aluminum-garnet [Nd:YAG] laser at 1064 μm wavelength for underwater microexplosion LISW [22], or Q-switched ruby laser at 694 μm [23] or Q-switched Nd:YAG laser at 532 nm [24] wavelength for elastic targeting LISW).
-
2.
Previously characterized truncated ellipsoidal reflector (proportional to the size craniotomy) for underwater microexplosion.
-
3.
1–400 μg Silver azide for underwater microexplosion LISW [22] or 1.0 mm polyethylene terephthalate (PET) and 0.5 mm black rubber for elastic targeting LISW [23, 24].
-
4.
0.6 mm diameter quartz optical fiber (diameter dependent on animal chosen and craniotomy size) for underwater microexplosion LISW [22].
-
5.
Physiological saline (volume, concentration, and temperature dependent on animal chosen) for underwater microexplosion [22] or ultrasound gel for elastic targeting LISW [23, 24].
-
6.
Polyvinylidene fluoride (PVDF) needle hydrophone (laser fluence sensor to monitor pressure available from Precision Acoustics Ltd, Onda Corp, or Müller Instruments).
3 Methods
3.1 Systematic Review Procedures
To collect data for this systematic review, literature searches were conducted for animal choice and unique methodologies utilized in relevant peer-reviewed TBI research articles published in or after 1980 (see Fig. 1). PubMed, ISI Web of Knowledge, and Google Scholar were searched for the name of each model. A representative sampling of 50 peer-reviewed articles with comprehensive methods in animals were systemmatically reviewed for models where hundreds of articles were available. Twenty-five compression, 50 CCI, 50 FPI, 12 suction/ablation, 25 zymosan, 29 cryolesion, 16 stab, 8 EML, 3 HVM, 33 PBBI, 50 concussion, 8 impact acceleration, 5 weight drop, 50 pneumatic blast, and 6 live blast brain injury articles were reviewed. The general animal choice and methodologies utilized for each respective model were combined to compare and contrast the approaches used in various animal models of TBI. Considerations for choosing each animal model were identified and factored into the systematic review. Using the parameters of each approach, each animal model was classified with respect to a commonly accepted hierarchy of TBI [4]. To determine the relative ease of use of each model, the volume and complexity of the materials and methods used for each general approach were compared to include safety precautions. The results of the systematic review were summarized, analyzed, and integrated into a summary table (see Table 2).
Systematic review flow chart. The search strategy for this systematic review of animal models of traumatic brain injury entailed screening three major literature databases, excluding duplicates and publications with incomplete methods, and sampling representative publications when the search resulted in hundreds of publications with like models. The search strategy resulted in 373 publications included in the qualitative methods review
3.2 Animal Adaptation/Preparation
For all protocols detailed in this chapter, it is important to note the following:
-
1.
All animal procedures should be performed with the approval of the local Institution’s Animal Care and Ethics Committee and in accordance with the National Institutes of Health guidelines, with measures taken to minimize pain and discomfort. Animals must be handled according to the approved protocol at the research institution as well as the funding agency, if applicable.
-
2.
Similar to behavioral studies, after the arrival of the rats at the animal facility, the rats should acclimate to the new environment for 1 week.
-
3.
Procedures should be executed at the same time each day based on physiological rhythms unless the dependent variable is the time of day.
-
4.
Animals should be housed under temperature-controlled conditions on an animal-appropriate light and dark cycle and diet (e.g., 12-h reverse light and dark cycle, while fed mouse chow and water ad libitum for rodents).
-
5.
All procedures should be accomplished while wearing a mask, gown, and sterile gloves.
-
6.
Before conducting any procedures, the animals to be tested should be moved into the vicinity of the testing area to allow them to adapt to the new environment for 20–30 min in their cages before starting the procedure. Note: Only the animal undergoing the procedure should be in the procedure room at any given time to avoid undue stress.
-
7.
The user should become familiar with the procedure and set up the protocols ahead of time to avoid mistakes during the procedure.
-
8.
All surfaces of the surgical tools and devices must be autoclaved (if possible) and cleaned with 10 % ethanol solution or sterilized with an instant dry sterilizer before any procedure.
-
9.
All animals should be anesthetized with a pre-approved agent prior to surgery and maintained under anesthesia throughout the procedure.
-
10.
Weigh the animal immediately prior to administering anesthesia to ensure appropriate dosing.
-
11.
To maintain the most sterile conditions possible, the skin at the site of surgery should be shaved. Note: This does not apply to indirect blast models where no surgery is involved.
-
12.
Clean the skin using sterile cotton tipped applicators and povidone iodine.
-
13.
Consider application of ophthalmic ointment to the eyes using sterile cotton tipped applicators to avoid dryness if the procedure is expected to last for longer durations.
-
14.
Place the animal on a sterile stainless steel plate with a preheated homeothermic blanket system underneath.
-
15.
Secure all animal limbs taking care to position the hind limbs symmetrically.
-
16.
Cover the surgical field with a sterile drape.
-
17.
Once the procedure is completed, the animal should be returned to animal-appropriate, temperature controlled recovery housing until they wake from anesthesia, and not directly to their original housing. Note the time the animal was under anesthesia and any deviations from normal physiological parameters (see Notes 1 – 5 ).
-
18.
Return animal to the appropriate housing facility. Note the time until recovery (see Notes 6 and 7 ).
-
19.
CAUTION: All sharps and tools used for animal studies should be handled as biosafety level-2 waste, collected in special containers and disposed of only after being autoclaved or inactivated with bleach or other disinfectant while wearing protective gloves and a lab coat.
3.3 Compression
3.3.1 Compression Procedures
-
1.
Place the animal in a stereotaxic frame secured by ear bars and an incisor bar.
-
2.
Carefully expose the skull and perform a craniotomy using a trephine drill or some other minidrill at predetermined stereotaxic coordinates. The length of the incision and diameter of the craniotomy are dependent on the animal chosen, the complexity of accessing the tissue to crush, and the experience of the surgeon.
-
3.
Using forceps, iridectomy scissors, and retractors, gently expose the tissue to be crushed. For a negative control, equivalent tissue should be exposed, but not crushed.
-
4.
Place the nerve on the bottom jaw of a hemostatic forceps proportional to the tissue to be crushed (e.g., super-fine if a single, specific nerve). Note the alignment of the tissue and forceps before crushing to ensure consistency between trials and to avoid displacing the tissue beyond the forceps as a result of the crush.
-
5.
Crush the tissue for the predetermined amount of time by securing the forceps to a predetermined setting (e.g., once for 20 s at three clicks). Do not shift the forceps when the tissue is being crushed to avoid unintended consequences.
-
6.
If crushing the tissue multiple times, mark the specific area with a sterile indicator for reference. Powdered carbon is one way to mark the crush site [25] between crush injuries, but care must be taken to avoid marking beyond the injury site. Bauder [25] recommends opening sterile forceps in powdered carbon, gently close but do not click the forceps while still in the carbon, and wipe the carbon on the outside of the forceps off using sterile gauze before marking the area.
-
7.
After crushing the tissue, carefully return the retracted tissue and suture the skin back in place.
3.3.2 Compression Precautions
Safety concerns include the use of a scalpel for the scalp resection, use of a drill for the craniotomy, use of iridectomy scissors to expose the tissue to be crushed, and sutures for closing the scalp after the injury.
3.4 Fluid Percussion Injury
FPI is a highly characterized and widely accepted model for use in numerous organisms (refer to Table 2 for a comparison of all models with corresponding criteria) that falls within the penetrating constrained (percussion) direct brain deformation category. FPI is inflicted as a metal pendulum is released and strikes a piston which drives injection of a small volume of sterile saline into the cranial cavity of the animal through the plastic luer-loc needle hub. In other words, FPI entails a craniotomy and direct saline application to intact dura via the use of a plastic cap and a Plexiglass cylinder. The hammer (pendulum) is controlled electrically and the voltage correlates to the pressure delivered. The location of the craniotomy can be changed; however, with potential consequences. Specifically, a lateral craniotomy (at least 3.5 mm lateral to the sagittal suture) leads to contralateral cortical damage with impact [26]—both focal (such as hemorrhage) and diffuse similar to most human TBI. However, noting the specific location of the craniotomy allows for consistency. Lateral fluid percussion (LFP) allows for a direct unilateral injury with very little to no subsequent contralateral rebound and/or brainstem injury. Central fluid percussion (CFP) impacts both cortices and subsequently shifts the brainstem which results in increased mortality thus limiting the dose–response [8, 27]. Each injury model induces similar signs and symptoms as in humans which allows for study of pathology, physiology, and pharmacology. However, the use of fluid is less mechanically controllable because of its diffusivity. If the fluid evaporates, gas bubbles accumulate, and/or the plastic cap degrades then the fluid may escape, the gas may change the delivered pressure, or the plastic cap may expand differently, thus creating inconsistencies between injuries. To increase the longevity of the model, the various o-rings must be lubricated and inspected.
One notable case of the use of FPI is in modeling epilepsy after severe TBI similar to the case of Henry Gustav Molaison (HM). After receiving a TBI from a supposed bicycle accident, HM suffered ongoing seizures—post-traumatic epilepsy (PTE). To alleviate the seizures, HM’s medial temporal lobes were extracted. Severe FPI (greater than 3 atm fluid pressure) initiates such seizures in hippocampal structures [28, 29]. Unfortunately, the onset of the seizures is often 7–12 months post-FPI.
3.4.1 FPI Procedures
-
1.
Place the animal in a stereotaxic frame secured by ear bars and an incisor bar.
-
2.
Carefully expose the skull and perform a craniotomy using a trephine drill or some other minidrill at predetermined stereotaxic coordinates.
-
3.
Carefully secure a sterile luer-loc needle hub over the exposed dura with either skull screws or cyanoacrylate glue.
-
4.
Once secure, fill the luer-loc needle hub with saline and cap until ready to perform the FPI.
-
5.
Prior to preparing the animal for the FPI, ensure the injury settings are appropriate (e.g., pulse duration).
-
6.
At a predetermined time after the preparation of the animal luer-loc needle hub, re-anesthetize the animal and then fill the luer-loc needle hub with saline to ensure consistent pulse and avoid air bubbles. Connect the hub to the FPI device.
-
7.
Deliver the impact while measuring the amplitude of the resulting pressure pulse using a pressure transducer and wave form with an oscilloscope.
-
8.
Remove the animal from the FPI device and cap the hub.
3.4.2 FPI Precautions
Safety concerns include the use of a scalpel for the scalp resection, use of a drill for the craniotomy, use of a syringe to remove gases in fluid cylinder, use of electricity to power the hammer, and sutures for closing the scalp after the injury.
3.5 Controlled Cortical Impact (CCI)
Controlled cortical impact, or rigid percussion model, also falls within the penetrating constrained (percussion) direct brain deformation category. CCI is the attempt to solve the limitations of the FPI model while maintaining consistency with clinical signs and symptoms. Both models utilize a stereotaxic device to constrain the animal (rat or mouse in most cases) and ensure a repeatable alignment with the impact device. Instead of fluid, the CCI is delivered to the intact dura via an adjustable pneumatic- or weight-drop-driven piston (impactor) of variable diameter, thus providing a more localized injury. The impactor is mounted to an adjustable ruled crossbar that can be rotated to regulate it at different angles. In addition to the adjustable diameter and depth, the velocity and dwell time of the impactor are adjustable. Depth and velocity of impact correlate to pathological severity of the injury. Evidence to support a correlation between dwell time and severity of injury is not apparent. Although this model alleviates the controllability limitation of the FPI impact, the CCI model still requires a craniotomy which causes additional damage to the surrounding cortex area.
3.5.1 Controlled Cortical Impact Procedures
-
1.
Prior to preparing the animal for the CCI, ensure that the injury settings are appropriate (e.g., depth, velocity, and duration).
-
2.
Place the animal in a stereotaxic frame secured by ear bars and an incisor bar.
-
3.
Carefully expose the skull and perform a craniotomy using a trephine drill or some other minidrill at predetermined stereotaxic coordinates. Note: It is helpful to align the impactor with the craniotomy site prior to removal of the bone.
-
4.
Deliver the CCI to the intact dura with a predetermined penetration depth, velocity, and duration.
-
5.
Consider replacing the bone from the craniotomy and sealing with either dental cement, or bone wax.
-
6.
Close the scalp incision with sutures following the injury.
3.5.2 CCI Precautions
Safety concerns include the use of a scalpel for the scalp resection, use of a drill for the craniotomy, use of high velocity blunt objects, and sutures for closing the scalp after the injury.
3.6 Vacuum/Suction
Vacuum pulse and/or mechanical suction are another type of direct dynamic penetrating brain deformation which creates a focal cortical injury, without neither hemorrhage nor diffuse injury, by inserting a suction force to the intact dura via a plastic plunger of variable diameter. The main benefit is the reduction of neurochemical cascades due to reduced hemorrhaging. Disadvantages include the lack of an increase in intracranial pressure (ICP) which is characteristic of most TBI and the vacuum may need application for a longer duration than most TBI would sustain [30]. Such a model may be applicable to brain injury due to asphyxia and/or brain deformation without blood vessel damage. For instance, many infants are reported to sustain brain injury during birth. The use of medical forceps and vacuum extraction increase the occurrence of infant brain injury, both focal and diffuse.
3.6.1 Vacuum/Suction Procedures
-
1.
Prior to preparing the animal for vacuum/suction injury, ensure the vacuum is set appropriately (e.g., 200–250 mm of mercury).
-
2.
Place the animal in a stereotaxic frame secured by ear bars and incisor bar.
-
3.
Carefully expose the skull and perform a craniotomy using a trephine drill or some other minidrill at predetermined stereotaxic coordinates.
-
4.
Deflect the dura and remove the cortex underlying the craniotomy site with gentle suction through a fine glass Pasteur pipet. Suction should be continued until a predetermined depth.
-
5.
Consider replacing the bone from the craniotomy and sealing with dental cement, or bone wax.
-
6.
Close the scalp incision with sutures following the injury.
3.6.2 Vacuum/Suction Precautions
Safety concerns include the use of a scalpel for scalp resection, use of a drill for the craniotomy, and sutures for closing the scalp after the injury.
3.7 Zymosan
Other direct dynamic penetrating brain deformation models attempt to bypass the primary injury mechanism in order to model aspects of the secondary injury such as glial scarring and inflammation. Fitch [31] modeled such scarring with a zymosan (macrophage activator) solution delivered to the corpus callosum. Such a model creates cavitation without biophysical components typical of TBI. Not many studies appear to use this technique. One potential application of this model is the in vivo research regarding the glial scarring process and enabling axons to regrow beyond the barrier created by the scar.
3.7.1 Zymosan Procedures
-
1.
Prior to preparing the animal for zymosan injection, ensure the zymosan solution is prepared and loaded in the needle for injection to avoid delays in the procedure.
-
2.
Place the animal in a stereotaxic frame secured by ear bars and incisor bar.
-
3.
Carefully expose the skull and perform a craniotomy at predetermined stereotaxic coordinates by thinning the skull over the area to be injected. The area of thinned skull should be approximately 1 mm by 1 mm per injection site using a hand-held drill. Stop when the bone is very thin and the blood vessels in the dura become clearly visible. Note: Do not drill through the bone to avoid unintended injury to the surface of the brain parenchyma. Keep both the skull and exposed dura moist with saline.
-
4.
Carefully perforate the thinned area of skull with a small needle (e.g., 27 G).
-
5.
Carefully flip up and remove the thinned bone with fine-tipped forceps.
-
6.
Align the craniotomy site with the tip of the stereotaxic injector.
-
7.
Lower the injector tip until it touches the exposed dura. If necessary, cut a small incision in the dura with a 27-G needle held at a flat angle to avoid unanticipated injury.
-
8.
After penetrating the dura, slowly lower the injector tip to the predetermined z coordinate.
-
9.
Slowly and consistently apply pressure to the injector syringe to inject the predetermined volume of zymosan solution.
-
10.
To avoid backflow of the zymosan solution, wait for 2–3 min before withdrawing the injector.
-
11.
Clean the injection site with moist cotton swabs.
-
12.
Consider replacing the bone from the craniotomy and sealing with dental cement, or bone wax.
-
13.
Close the scalp incision with sutures following the injury.
3.7.2 Zymosan Precautions
Safety concerns include use of a scalpel for scalp resection, use of a drill for the craniotomy, use of a syringe to deliver the solution, and sutures for closing the scalp after the injury.
3.8 Cryolesion
Focal cortical cryolesion is a direct dynamic model of TBI which causes a focal penetrating brain deformation using extreme cold [31]. To avoid the spread of injected liquid nitrogen in the freezing process, a pre-cooled probe chilled in liquid nitrogen is applied to the brain. This model is usually used when the primary mechanism of the brain injury is not the primary aim of the study. Instead cryolesion is used to induce local histopathological damage consistent with TBI. This particular model of TBI is effective in very small organisms (infants) where the other TBI models available may not otherwise allow for survival.
3.8.1 Cryolesion Procedures
-
1.
Place the animal in a stereotaxic frame secured by ear bars and incisor bar.
-
2.
Carefully expose the skull and perform a craniotomy using a trephine drill or some other minidrill at predetermined stereotaxic coordinates.
-
3.
Precool a metal cylinder in liquid nitrogen.
-
4.
Stereotactically apply the precooled metal cylinder to the predetermined region of the brain for a predetermined amount of time. Care should be taken to avoid unanticipated injury due to too much pressure applied to the precooled cylinder. If the duration of cryolesion is long, the cylinder should be filled with liquid nitrogen to ensure it remains cold for the entire duration of the injury.
-
5.
Consider replacing the bone from the craniotomy and sealing with dental cement, or bone wax.
-
6.
Close the scalp incision with sutures following the injury.
3.8.2 Cryolesion Precautions
Safety concerns include use of a scalpel for scalp resection, use of a drill for the craniotomy, use of liquid nitrogen may cause burns, and sutures for closing the scalp after the injury.
3.9 Stab Wounds
Stab wounds are easily modeled in many organisms, most popularly in the rodent [32]. The cortical stab injury (CSI) model is homologous to stab TBI in humans, but is seldom used due to the relatively low incidence of stab TBI [The main cause of TBI (non-military) is automobile accident]. Some studies may opt to skip the craniotomy, thus reproducing the effect of stabbing through the skull. The main use of this model appears to be in emergency medicine where careful removal of the blade to reduce hemorrhage is considered paramount for acute TBI management.
3.9.1 Stab Procedures
-
1.
Place the animal in a stereotaxic frame secured by ear bars and incisor bar.
-
2.
Carefully expose the skull and perform a craniotomy using a trephine drill or some other minidrill at predetermined stereotaxic coordinates.
-
3.
Implant and cement a guide cannula at predetermined stereotaxic coordinates using a 22 G needle.
-
4.
At a predetermined time after implantation of the guide cannula, re-anesthetize the animal and thin the skull bone located at the appropriate distance from the guide cannula with a hand-held drill and stereotactically insert a sterilized razor blade to a predetermined depth. Remove the blade after a predetermined amount of time.
-
5.
Remove the guide cannula.
-
6.
Consider replacing the bone from the craniotomy and sealing with dental cement, or bone wax.
-
7.
Close the scalp incision with sutures following the injury.
3.9.2 Stab Precautions
Safety concerns include the use of a scalpel for scalp resection, use of a drill for the craniotomy, use of high-velocity sharp objects, and sutures for closing the scalp after the injury.
3.10 Epidural Mass Lesions (EML)
Epidural mass lesions (EML) are produced with variable inflation and reperfusion of a latex balloon typically inserted epidurally [33]. Such a model mimics the physical effects of hemorrhage and inflammation without the primary mechanism of injury or secondary neurochemical cascades associated with inflammation (e.g., cytokines). A specific application of this model is in bicycle crashes that result in middle meningeal artery transection. A famous case for potential EML application is in the death of Liam Neeson’s wife, Natasha Richardson, who likely suffered from “walk and die” syndrome [walk and die” syndrome is typically due to delayed epidural bleeding] due to a skiing accident in March of 2009.
3.10.1 EML Procedures
-
1.
Place the animal in a stereotaxic frame secured by ear bars and incisor bar.
-
2.
Carefully expose the skull and perform a craniotomy using a trephine drill or some other minidrill at predetermined stereotaxic coordinates.
-
3.
Stereotactically inject an uninflated latex balloon with a mitered valve using a microcatheter assembly. Do NOT penetrate the dura.
-
4.
Carefully expand the latex balloon to a predetermined pressure in a predetermined amount of time, using air or water supplied via a variable pressure waveform generator.
-
5.
Carefully deflate the latex balloon at a predetermined rate. Typically, the rate for inflation of the balloon is slower and the duration of maintaining the inflation longer when investigating EML than it is for PBBI.
-
6.
Immediately retract the probe with the latex balloon.
-
7.
Consider replacing the bone from the craniotomy and sealing with either dental cement or bone wax.
-
8.
Close the scalp incision with sutures following the injury.
3.10.2 EML Precautions
Safety concerns include the use of a scalpel for scalp resection, use of a drill for the craniotomy and sutures for closing the scalp after the injury.
3.11 High-Velocity Missile (HVM)
High-velocity missile (HVM) models are also referred to as craniocerebral missile injuries (CMI) and use actual ballistics fired into the skull at varying distances, while the animal is either constrained or unconstrained. This model often utilizes larger organisms such as cats [34, 35] and sheep [36] to mimic the anatomical alterations due to large military weapons. The HVM model can vary in caliber of the firearm used, distance (range) of fire, and direction of impact (entrance and exit). Anterior to posterior paths cause unilateral damage whereas transverse impacts cause bilateral damage. Unfortunately, the size of the animals must be large due to the large size of the ballistics and resulting cavitation. Resulting hemorrhage may limit subsequent molecular monitoring with increased mortality.
3.11.1 HVM Procedures
-
1.
Place the animal in a stereotaxic frame secured by ear bars and incisor bar (if constrained).
-
2.
Stereotactically discharge a firearm at predetermined stereotaxic coordinates.
-
3.
Consider replacing any bone displaced by the ballistic and sealing with dental cement, or bone wax.
-
4.
Close the scalp incision with sutures following the injury.
3.11.2 HVM Precautions
Safety concerns include the use of a controlled weapon and sutures for closing the scalp after the injury. It is necessary to perform any experiments involving ballistics in a controlled range approved for animal use.
3.12 Penetrating Ballistic-Like Brain Injury (PBBI)
Penetrating ballistic-like brain injury (PBBI) [3] is the attempt to solve the limitations of the HVM models by using inflatable stereotaxic implant probes versus actual ballistics. The probe is smaller, but proportional to the ballistics used in HVM models to allow for use in rodents. The inflatable bladder is adjustable in time and percent. For example, 12 % inflation creates a larger cavity than 5 % inflation. Some researchers opt to leave the skull intact thus replicating the effect of the ballistics penetrating the skull on the injury site. A recent application of both the HVM and PBBI models is in understanding the case of Gabrielle Giffords, a Democratic congresswoman who was shot in the head by Jared Laughner. Medical examiners and investigators can apply HVM and PBBI research to aid in diagnosing the specific path of the ballistics, type of ballistics, and resulting pathology.
3.13 PBBI Procedures
-
1.
Place the animal in a stereotaxic frame secured by ear bars and incisor bar.
-
2.
Carefully expose the skull and perform a craniotomy using a trephine drill or some other minidrill at predetermined stereotaxic coordinates.
-
3.
Stereotactically inject an uninflated latex balloon with a mitered valve using a microcatheter assembly.
-
4.
Carefully expand the latex balloon to a predetermined pressure in a predetermined amount of time using air or water supplied via a variable pressure waveform generator.
-
5.
Carefully deflate the latex balloon at a predetermined rate. Typically, the rate for inflation of the balloon is faster and the duration of maintaining the inflation shorter when investigating PBBI than it is for EML.
-
6.
Immediately retract the probe with latex balloon.
-
7.
Consider replacing the bone from the craniotomy and sealing with dental cement, or bone wax.
-
8.
Close the scalp incision with sutures following the injury.
3.14 PBBI Precautions
Safety concerns include the use of a scalpel for scalp resection, use of a drill for the craniotomy, use of high-velocity blunt or sharp objects, and sutures for closing the scalp after the injury.
3.15 Concussion
Controlled concussion is similar to CCI without a craniotomy. Since the impact is to the skull, the injury is not as well localized and often results in subsequent brainstem damage. Many models fail to correlate impact with severity [6, 37].
3.15.1 Concussion Procedures
-
1.
Prior to preparing the animal for the impact, ensure the settings are appropriate (e.g., dwell time, duration, and velocity).
-
2.
Leave the animal unconstrained with its head on the customized cushion.
-
3.
Carefully expose the skull and secure the plate or cone to the predetermined location on the skull.
-
4.
Deliver the impact(s) to the intact skull via the plate or cone.
-
5.
Close the scalp incision with sutures following the injury.
3.15.2 Concussion Precautions
Safety concerns include the use of a scalpel for scalp resection, use of high-velocity blunt objects, and sutures for closing the scalp after the injury.
3.16 Unconstrained Impact Acceleration
Unconstrained primate and ovine impact acceleration models use a piston impactor of variable weight to inflict head motion similar to that of constrained controlled concussion. The rapid acceleration and deceleration of the head allow for biophysical evaluation of the injury, but are less controllable since the head is free to move rotationally and laterally. This head movement creates the characteristic diffuse axonal injury but is difficult to reproduce unless the animal is at least partially restrained. When partially restrained (pseudo-constrained), at the neck, thus only allowing head movement, the animals head can only move in one dimension. Application of this model lies primarily in transportation-related acceleration and deceleration injuries.
3.16.1 Unconstrained Impact Acceleration Procedures
-
1.
Prior to preparing the animal for the impact, ensure that the settings are appropriate (e.g., weight and height of drop).
-
2.
Leave the animal unconstrained with its head on the customized cushion. Typically, unconstrained impact acceleration delivers an impact more laterally, whereas the weight drop impact is typically more along the midline.
-
3.
Carefully expose the skull and secure the plate or cone to the predetermined location on the skull.
-
4.
Deliver the weight drop to the intact skull, or dura if penetrating, with a predetermined weight from a predetermined height.
-
5.
Consider replacing the bone from the craniotomy and sealing with dental cement, or bone wax if investigating a penetrating injury.
-
6.
Close the scalp incision with sutures following the injury.
3.16.2 Unconstrained Impact Acceleration Precautions
Safety concerns include the use of a scalpel for scalp resection and sutures for closing the scalp after the injury.
3.17 Weight Drop
Marmarou’s weight drop model [38] is an example of a pseudo-constrained acceleration model. In this case, a variable weight is dropped from a variable height through a Plexiglas tube to impact with the skull of an animal placed on a foam pad. The tube must be slightly larger than the weight which allows for uncontrolled lateral movement of the weight prior to impact. Some argue that additional variability is due to the weight rebounding after the initial drop thus creating a double injury/impact [4]. However, this rebounding effect can be countered with a barrier that restricts the second impact—or bounce. This model is comparable to the controlled concussion in application, but is less controllable.
Cernak’s model [39] attempts to solve the limitations of the Marmarou model [38, 40] by using a pneumatic driven steel impactor that is laser guided to a steel disc cemented to the animal’s skull. The pneumatic driven impactor is similar to the CCI and is controllable in velocity, dwell time and depth. The force is monitored via software, ensuring accurate correlation of injury severity and delivered impact while still replicating clinical signs and symptoms.
3.17.1 Weight Drop Procedures
-
1.
Prior to preparing the animal for the weight drop, ensure that the settings are appropriate (e.g., weight and height of drop).
-
2.
Place the animal in a stereotaxic frame secured by ear bars and incisor bar, or leave unconstrained.
-
3.
Carefully expose the skull and secure the plate or cone to the predetermined location on the skull. If investigating a penetrating injury, perform a craniotomy using a trephine drill or some other minidrill at predetermined stereotaxic coordinates. Note: It is helpful to align the impactor with the craniotomy site prior to removal of the bone.
-
4.
Deliver the weight drop to the intact skull, or dura if penetrating, with a predetermined weight from a predetermined height.
-
5.
Consider replacing the bone from the craniotomy and sealing with dental cement, or bone wax if investigating a penetrating injury.
-
6.
Close the scalp incision with sutures following the injury.
3.17.2 Weight Drop Precautions
Safety concerns include the use of a scalpel for scalp resection, use of high-velocity blunt objects, and sutures for closing the scalp after the injury. In addition to the safety concerns of the Marmarou’s model, safety concerns of Cernak’s model include use of a laser which may cause eye damage.
3.18 PneumaticBlast
3.18.1 Pneumatic Blast Procedures
-
1.
Prepare the shock tube to the predetermined shockwave and overpressure parameters (see Note 8 ).
-
2.
Place the animal within or at a predetermined distance from the shock tube opening. Consider placing the animal at 20–40° lateral to the shock tube axis to avoid unanticipated effects due to the exhaust gasses, or blast wind.
-
3.
Consider constraining the head laterally and inferiorly to prevent head rotational acceleration-induced injury.
-
4.
Consider placing a metal cylinder around the body to limit shockwave overpressure exposure of the torso.
-
5.
Deliver the shockwave.
3.18.2 Pneumatic Blast Precautions
Safety concerns include the use of high pressure air and cut metal membranes which result in sharps. Besides the blast overpressure, the pneumatic blast causes a loud noise capable of disrupting hearing in unprotected ears.
3.19 Live Blast
3.19.1 Live Blast Procedures
-
1.
Prepare the blast tube either with the predetermined explosive charge parameters, or in an explosive range (see Note 8 ).
-
2.
Place the animal within or at a predetermined distance from the blast tube opening, or explosive charge. Consider placing the animal at 20–40° lateral to the blast tube axis to avoid unanticipated effects due to the exhaust gasses, or blast wind.
-
3.
Consider constraining the head and neck to prevent head rotational acceleration-induced injury.
-
4.
Consider placing a metal cylinder around the body in order to limit shockwave overpressure exposure of the torso.
-
5.
Detonate the explosive charge.
3.19.2 Live Blast Precautions
-
1.
Safety concerns include use of live explosives. Besides the blast overpressure, the live blast causes a loud noise capable of disrupting hearing in unprotected ears.
3.20 LISW Blast
3.20.1 LISW Blast Procedures
-
1.
Prepare the laser according to the manufacturer’s instructions and using the predetermined parameters (wavelength, pulse width) based on the animal and specific aims of your study.
-
2.
Place the animal in a stereotaxic frame secured by ear bars and incisor bar unless the LISW is being inflicting to the ear in which case the animal will need to be secured manually or with a custom restraint.
-
3.
Carefully expose the skull and perform a craniotomy using a trephine drill or some other minidrill at predetermined stereotaxic coordinates (if necessary based on the location of the LISW).
-
4.
For underwater microexplosion LISW [22], fill the truncated ellipsoidal reflector with physiological saline and gently secure against the brain tissue within the craniotomy with the scalp. Care should be taken to avoid unanticipated injury due to too much pressure applied to the truncated ellipsoidal reflector. Deliver the predetermined LISW (single, or multiple pulses).
-
5.
For elastic targeted LISW [23, 24], gently place the black rubber against the brain tissue within the craniotomy. On top of the black rubber, smear a thin layer of ultrasound gel. On top of the ultrasound gel, place the PET. Care should be taken to avoid unanticipated injury due to too much pressure applied to the elastic laser target. Deliver the predetermined LISW (single, or multiple pulses).
-
6.
Gently remove the underwater microexplosion apparatus, or the elastic target. Consider replacing the bone from the craniotomy and sealing with dental cement, or bone wax.
-
7.
Close the scalp incision with sutures following the injury.
3.20.2 LISW Blast Precautions
Safety concerns include use of a scalpel for scalp resection, use of laser which may cause eye damage, and sutures for closing the scalp after the injury.
3.21 Conclusion
Ultimately, no single “gold standard” model of TBI exists and there is overwhelming overlap among the existing models. With the abundance of animal models of TBI and the incomplete characterization of each model, data comparison is complicated between models. Therefore, the use of multiple models and animals as well as common data elements is encouraged, to expedite characterization and to validate results. Although there are a number of limitations to each animal and each model, the use of multiple models and multiple animals in combination provides an opportunity to explore mass and skull thickness among other scaling effects. Each stakeholder is seeking answers to different questions that require different approaches. No one model suffices to fully characterize every type of human TBI possible. Moreover, ethics are driving computerized models to replace animal models. Thus, one day we may rely on a virtual human to conduct our research rather than animal models.
4 Notes
-
1.
The lighting in the room is an important factor to consider while conducting all procedures to avoid shadowing and allow for illumination of the subject.
-
2.
Sterile techniques before, during, and after each procedure are critical to avoiding secondary effects of infection which can interfere with the interpretation of results.
-
3.
Use of pulse oximetry is essential to maintaining a controlled experiment involving animal models. A specific range of physiological parameters needs to be set and adhered to based upon the animal chosen. Should the specific physiological range be exceeded, the animal should be omitted from the study and the rationale should be formally documented.
-
4.
It is advisable to use the same surgeon throughout a study to maintain consistency. Should a study involve administration of a treatment protocol while surgeries are still occurring, a second researcher should be involved to allow the surgeon to continue uninterrupted. The second researcher should also remain the same, for consistency in treatment administration.
-
5.
Consideration to physiological rhythms must be factored into planning procedures to ensure that observed effects are due to the procedures and not due to naturally occurring biological rhythms.
-
6.
Animals should not be returned to the same cage with other animals if treating with strategies that can either transfer between animals or be tampered with by other animals.
-
7.
Animals should be returned to recovery housing before being returned to original housing especially if sharing a cage with other animals to avoid startling any cage mates. Consideration should be given to isolating animals for the entire testing period to avoid acute changes to stress and anxiety-like behavior .
-
8.
Aerodynamics and blast tubes characteristics must be fully delineated prior to application to any animal studies. Video-recording is highly recommended.
References
Ds S (1997) Biological Aspects of Disease. CRC Press, Netherlands
Pinel JPJ (2011) Biopsychology, 8th edn. Allyn & Bacon, Boston
Moshang E, L. G. (2002) A model of penetrating traumatic brain injury using air inflation technique. (Army, U. S. ed., U.S. Army Medical Research and Materiel Command, Ft Detrick, MD.
Cernak I (2005) Animal models of head trauma. NeuroRx 2:410–422
David S, Aguayo AJ (1985) Axonal regeneration after crush injury of rat central nervous system fibres innervating peripheral nerve grafts. Journal of neurocytology 14:1–12
Salzman SK, Faden AI (1994) The Neurobiology of central nervous system trauma. Oxford University Press, New York
Lab Animal's Buyer Guide. LabAnimal.
Povlishock JT, Hayes RL, Michel ME, McIntosh TK (1994) Workshop on animal models of traumatic brain injury. J Neurotrauma 11:723–732
Kilbaugh TJ, Lvova M, Karlsson M, Zhang Z, Leipzig J, Wallace DC, Margulies SS (2015) Peripheral Blood Mitochondrial DNA as a Biomarker of Cerebral Mitochondrial Dysfunction following Traumatic Brain Injury in a Porcine Model. PLoS One 10, e0130927
Sillesen M, Rasmussen LS, Jin G, Jepsen CH, Imam A, Hwabejire JO, Halaweish I, DeMoya M, Velmahos G, Johansson PI, Alam HB (2014) Assessment of coagulopathy, endothelial injury, and inflammation after traumatic brain injury and hemorrhage in a porcine model. J Trauma Acute Care Surg 76:12–19, discussion 19-20
Hwabejire JO, Jin G, Imam AM, Duggan M, Sillesen M, Deperalta D, Jepsen CH, Lu J, Li Y, deMoya MA, Alam HB (2013) Pharmacologic modulation of cerebral metabolic derangement and excitotoxicity in a porcine model of traumatic brain injury and hemorrhagic shock. Surgery 154:234–243
Glass TF, Fabian MJ, Schweitzer JB, Weinberg JA, Proctor KG (2001) The impact of hypercarbia on the evolution of brain injury in a porcine model of traumatic brain injury and systemic hemorrhage. J Neurotrauma 18:57–71
Ross AH, Jantz RL, McCormick WF (1998) Cranial thickness in American females and males. Journal of forensic sciences 43:267–272
Smith DF, Jensen PN, Gee AD, Hansen SB, Danielsen E, Andersen F, Saiz PA, Gjedde A (1997) PET neuroimaging with [11C]venlafaxine: serotonin uptake inhibition, biodistribution and binding in living pig brain. European neuropsychopharmacology : the journal of the European College of Neuropsychopharmacology 7:195–200
Roberts T, McGreevy P, Valenzuela M (2010) Human induced rotation and reorganization of the brain of domestic dogs. PLoS One 5, e11946
Russow LM, Theran P (2003) Ethical issues concerning animal research outside the laboratory. ILAR J 44:187–190
McSherry GM (1984) Mapping of cortical histogenesis in the ferret. J Embryol Exp Morphol 81:239–252
Gennarelli TA, Adams JH, Graham DI (1981) Acceleration induced head injury in the monkey. I. The model, its mechanical and physiological correlates. Acta Neuropathol Suppl 7:23–25
Adams JH, Graham DI, Gennarelli TA (1981) Acceleration induced head injury in the monkey. II. Neuropathology. Acta Neuropathol Suppl 7:26–28
Smith DH, Chen XH, Xu BN, McIntosh TK, Gennarelli TA, Meaney DF (1997) Characterization of diffuse axonal pathology and selective hippocampal damage following inertial brain trauma in the pig. J Neuropathol Exp Neurol 56:822–834
USAM Command (1997) Noise limits for military materiels. USAM Command, Redstone Arsenal, AL
Nakagawa A, Fujimura M, Kato K, Okuyama H, Hashimoto T, Takayama K, Tominaga T (2008) Shock wave-induced brain injury in rat: novel traumatic brain injury animal model. Acta Neurochir Suppl 102:421–424
Kurioka T, Matsunobu T, Niwa K, Tamura A, Kawauchi S, Satoh Y, Sato S, Shiotani A (2014) Characteristics of laser-induced shock wave injury to the inner ear of rats. J Biomed Opt 19:125001
Sato S, Kawauchi S, Okuda W, Nishidate I, Nawashiro H, Tsumatori G (2014) Real-time optical diagnosis of the rat brain exposed to a laser-induced shock wave: observation of spreading depolarization, vasoconstriction and hypoxemia-oligemia. PLoS One 9, e82891
Bauder AR, Ferguson TA (2012) Reproducible mouse sciatic nerve crush and subsequent assessment of regeneration by whole mount muscle analysis. J Vis Exp 60:pii 3606
Vink R, Mullins PG, Temple MD, Bao W, Faden AI (2001) Small shifts in craniotomy position in the lateral fluid percussion injury model are associated with differential lesion development. J Neurotrauma 18:839–847
Gennarelli TA (1994) Animate models of human head injury. J Neurotrauma 11:357–368
D'Ambrosio R, Fender JS, Fairbanks JP, Simon EA, Born DE, Doyle DL, Miller JW (2005) Progression from frontal-parietal to mesial-temporal epilepsy after fluid percussion injury in the rat. Brain 128:174–188
Kharatishvili I, Nissinen JP, McIntosh TK, Pitkanen A (2006) A model of posttraumatic epilepsy induced by lateral fluid-percussion brain injury in rats. Neuroscience 140:685–697
Mathew P, Bullock R, Graham DI, Maxwell WL, Teasdale GM, McCulloch J (1996) A new experimental model of contusion in the rat. Histopathological analysis and temporal patterns of cerebral blood flow disturbances. J Neurosurg 85:860–870
Fitch MT, Doller C, Combs CK, Landreth GE, Silver J (1999) Cellular and molecular mechanisms of glial scarring and progressive cavitation: in vivo and in vitro analysis of inflammation-induced secondary injury after CNS trauma. J Neurosci 19:8182–8198
Ghirnikar RS, Lee YL, He TR, Eng LF (1996) Chemokine expression in rat stab wound brain injury. J Neurosci Res 46:727–733
Burger R, Bendszus M, Vince GH, Roosen K, Marmarou A (2002) A new reproducible model of an epidural mass lesion in rodents. Part I: characterization by neurophysiological monitoring, magnetic resonance imaging, and histopathological analysis. J Neurosurg 97: 1410–1418
Carey ME (1995) Experimental missile wounding of the brain. Neurosurg Clin N Am 6:629–642
Carey ME, Sarna GS, Farrell JB (1990) Brain edema following an experimental missile wound to the brain. J Neurotrauma 7: 13–20
Finnie JW (1993) Pathology of experimental traumatic craniocerebral missile injury. J Comp Pathol 108:93–101
Lighthall JW, Dixon CE, Anderson TE (1989) Experimental models of brain injury. J Neurotrauma 6:83–97
Marmarou A, Foda MA, van den Brink W, Campbell J, Kita H, Demetriadou K (1994) A new model of diffuse brain injury in rats. Part I: pathophysiology and biomechanics. J Neurosurg 80:291–300
Cernak I, Vink R, Zapple DN, Cruz MI, Ahmed F, Chang T, Fricke ST, Faden AI (2004) The pathobiology of moderate diffuse traumatic brain injury as identified using a new experimental model of injury in rats. Neurobiol Dis 17:29–43
Foda MA, Marmarou A (1994) A new model of diffuse brain injury in rats. Part II: morphological characterization. J Neurosurg 80: 301–313
Disclaimer
The material presented in this chapter does not necessarily represent the views or opinions of Booz Allen Hamilton.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer Science+Business Media New York
About this protocol
Cite this protocol
Phipps, H.W. (2016). Systematic Review of Traumatic Brain Injury Animal Models. In: Kobeissy, F., Dixon, C., Hayes, R., Mondello, S. (eds) Injury Models of the Central Nervous System. Methods in Molecular Biology, vol 1462. Humana Press, New York, NY. https://doi.org/10.1007/978-1-4939-3816-2_5
Download citation
DOI: https://doi.org/10.1007/978-1-4939-3816-2_5
Published:
Publisher Name: Humana Press, New York, NY
Print ISBN: 978-1-4939-3814-8
Online ISBN: 978-1-4939-3816-2
eBook Packages: Springer Protocols