Abstract
Congenital hypoventilation syndromes are a rare group of disorders that may be primary, e.g., congenital central hypoventilation syndrome (CCHS), or secondary, e.g., due to brainstem abnormalities in Arnold-Chiari malformation. CCHS is a rare, lifelong condition of primary hypoventilation that was first described systematically in 1970 by Mellins et al. In 2003, it was discovered that mutations in the PHOX2B gene on chromosome 4p12 were responsible for this syndrome. This gene also plays a role in neural crest cell migration, and many patients present with symptoms of autonomic dysfunction in addition to symptoms of hypoventilation. The spectrum of hypoventilation is varied, and although most patients present in the neonatal period, late-onset cases have been reported. The exact incidence is unknown, but a prevalence rate of 1 in 200,000 live births has been reported in France. Although, the absolute number of children with CCHS is not large, care of these patients requires significant resources including skilled caregivers and sophisticated equipment. However, the outcome for these children is generally good provided appropriate ventilatory support and monitoring are used.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Pathophysiology
Genetics
In 2003, it was discovered that CCHS is caused by a defect in the PHOX2B homeobox gene and that inheritance is autosomal dominant [1, 2]. PHOX2B maps to chromosome 4p12 and encodes for a transcription factor that plays a role in the regulation of neural crest cell migration and development of the autonomic nervous system [1, 2]. The transcription factor consists of 314 amino acids with two short and stable polyalanine repeats of nine and 20 residues, respectively. Approximately 90 % of PHOX2B mutations in CCHS involve expansion of the 20-residue polyalanine region, adding 4–13 copies [3]. These polyalanine repeat expansion mutations (PARMs) produce genotypes of 20/24 to 20/33, whereas the normal genotype is 20/20. The remaining 10 % of PHOX2B mutations in CCHS are nonpolyalanine repeat mutations (NPARMs) and include missense, nonsense, and frameshift mutations.
To date, there have been some associations made between the PHOX2B genotype and CCHS phenotype. Typically, a higher number of repeats are associated with a greater severity of the respiratory phenotype [3, 4]. Specifically, individuals with genotypes from 20/27 to 20/33 usually require ventilatory support during both wakefulness and sleep, while those with the 20/25 genotype usually require only nocturnal ventilation [3, 5, 6]. Later-onset cases with milder hypoventilation have been documented with 20/24 or 20/25 genotypes and likely represent cases of variable penetrance of these mutations [5–7]. Most mutations occur de novo in CCHS, but 5–10 % are inherited from a mosaic typically unaffected parent [7].
Effect of Sleep State
Central alveolar hypoventilation is diagnosed when the arterial partial pressure of carbon dioxide (PCO2) is >45 mmHg during wakefulness, due to decreased central ventilatory drive. This cutoff cannot be applied during sleep however, as PCO2 levels are typically higher in this state. The regulation of arterial blood gases during sleep in healthy humans is maintained primarily by central chemoreceptors which respond to changes in the PCO2 by detecting the pH of cerebrospinal fluid and peripheral chemoreceptors which respond to decreased arterial partial pressure of oxygen (PO2) and increased PCO2. During wakefulness, additional behavioral and arousal-related influences on breathing (from reticular activating system, forebrain, and mechanoreceptor afferents) also affect ventilatory control. In many situations, these non-chemoreceptive inputs to breathing result in relatively well-controlled arterial blood gases in patients with CCHS while awake and not engaged in vigorous exercise. This may explain why some patients with CCHS who breathe sufficiently during wakefulness (e.g., those with genotypes 20/24, 20/25, and some 20/26) only require ventilatory support during sleep.
Huang et al. studied nine children with CCHS during spontaneous breathing in both rapid eye movement (REM) and non-REM (NREM) sleep and demonstrated more severe hypoventilation during NREM periods, with greater decreases in minute ventilation [8]. It has been proposed that an intrinsic REM-related ventilatory drive could explain these findings, as shown by increased firing of single neuron recordings of medullary respiratory cells during REM compared to NREM sleep in healthy animals [9]. In addition, it is known that there are tonic excitatory inputs to the respiratory system during both REM and wakefulness that decline during NREM sleep. However, although patients with CCHS have better ventilation during REM than NREM sleep, they still have significant hypoventilation during REM sleep and thus require mechanical ventilation during all sleep stages including REM.
Mechanoreception
Additional proposed non-chemoreceptive inputs to breathing in patients with CCHS include mechanoreceptor pathways. Studies have confirmed that in children with CCHS, both passive motion during wakefulness and active exercise improve ventilation [10, 11]. In a study of treadmill exercise testing in five children with CCHS, exercise-induced hyperpnoea occurred [11]. CCHS subjects increased minute ventilation primarily by increasing respiratory rate, in association with increasing limb pacing frequency on the treadmill. Gozal et al. demonstrated that passive motion of the lower extremities during NREM sleep in six patients with CCHS resulted in increased respiratory frequency and decreased end-tidal CO2 levels [12]. These findings suggest that CCHS patients may be at higher risk for hypoventilation when they are physically still. One study of five patients with CCHS also demonstrated that they increased ventilation with mental activities such as reading, solving arithmetic problems, or playing video games [13].
A study of seven patients with CCHS during wakefulness demonstrated upward shift of EEG signals just before inspiration (pre-inspiratory potential) suggestive of supplementary motor area activation [14]. These potentials were present in a variety of conditions including resting breathing, exposure to CO2, and inspiratory mechanical constraints. In the control group, however, these pre-inspiratory potentials were generally absent except for during mechanical constraint. These findings indicate the existence of cortical mechanisms compensating for deficient generation of automatic breathing in CCHS.
Clinical Presentation
CCHS is characterized by the clinical presentation of alveolar hypoventilation with insensitivity to hypoxemia and hypercapnia, most pronounced during sleep. Infants with CCHS typically present in the newborn period with intermittent episodes of cyanosis or apnea, and most require mechanical ventilation immediately after birth. As their oxygen saturation falls and their carbon dioxide level rises, affected infants demonstrate no increase in respiratory rate or effort and usually do not arouse or appear distressed [15]. During sleep, infants will appear to have regular but shallow respirations with reduced chest wall movement, interspersed with periods of central apnea. Occasionally, infants may present in the first few months of life with acute life-threatening events or even frank respiratory arrest.
In many infants during the first few months of life, hypoventilation may be evident during both wakefulness and sleep. However, these patients may eventually breathe adequately while awake, probably reflecting the development of sleep-wake regulation or maturation of the respiratory and central nervous systems rather than an improvement in their CCHS [16]. Some affected patients may continue to display symptoms of hypoventilation during quiet activities while awake and may require daytime ventilatory support.
Symptoms of hypoventilation are more pronounced in times of illness or stress because patients with CCHS are unable to demonstrate respiratory responses to increased ventilatory demands. Thus, when faced with gas exchange abnormalities (e.g., during a respiratory tract infection), children with CCHS do not manifest signs of respiratory distress such as tachypnea, retractions, or nasal flaring. In some cases patients with CCHS can present late with symptoms of end-organ damage, such as cor pulmonale, seizures, developmental delay, or failure to thrive, from chronic, unrecognized hypoxemia and hypercarbia. In one survey of almost 200 children with CCHS, developmental delays, including motor, speech, and learning disabilities, were reported in 45 % [17].
Rarely, patients with CCHS survive into adulthood before presenting with symptoms of hypoventilation that are triggered by a minor respiratory tract infection or general anesthesia. Other potential presenting symptoms of adult cases include epileptic seizures, cognitive disabilities, and sleep apnea or in rare occasions after a child is diagnosed with CCHS [1]. In such late-onset cases, there is frequently a history of ventilatory disturbances in infancy that resolved spontaneously, e.g., breath-holding spells, and patients often have cognitive impairment [18].
Autonomic Dysfunction
Patients with CCHS often manifest symptoms of autonomic nervous system dysregulation including temperature instability, excessive sweating, decreased perception of discomfort and anxiety, and swallowing dysfunction. Periods of autonomic crises with and without elevated urinary catecholamines have also been described [19]. Although baseline heart rate does not differ from controls, the relative increase above the mean heart rate at rest with exercise is attenuated, and heart rate variability is decreased [20–22]. Cardiac arrhythmias, including sinus bradycardia and transient asystole up to 6.5 s, have also been reported [20]. One study of 39 patients with CCHS reported that among three children who had R-R intervals greater than 3 s and did not receive a cardiac pacemaker, two died suddenly [23]. Additionally, blood pressure in patients with CCHS is lower during wakefulness and higher during sleep compared to controls, indicating attenuation of the normal sleep-related blood pressure decrement [22]. Goldberg et al. documented ophthalmologic disorders in 27 of 37 children with CCHS, most of whom had miotic pupils that reacted poorly to light [24].
Abnormalities of neural crest origin, also known as neurocristopathies, may be present in patients with CCHS. Hirschsprung’s disease is present in approximately 16 % of cases of CCHS [17]. This is often severe, with 50 % of cases having total colonic aganglionosis, compared to the general population with Hirschsprung’s disease in whom 80 % have short segment forms [25]. Children with CCHS who receive mechanical ventilation for 24 h a day are more likely to have Hirschsprung’s disease [17].
Case reports of tumors of neural crest origin, including mediastinal or abdominal neuroblastoma or ganglioneuromas, have been documented in association with CCHS [25–27]. Approximately 5 % of patients with CCHS will have neural crest tumors although tumor-related deaths are uncommon [17, 28]. The tumors can present at variable ages with neuroblastoma typically presenting before age two years and ganglioneuromas presenting later as incidental findings [28]. Tumors of neural crest origin occur more frequently in patients with NPARMS, specifically missense or frameshift homozygous mutations of the PHOX2B gene [29, 30]. Among patients with PARMs, only subjects with the 20/29 and 20/33 genotypes have been identified with neural crest tumors (ganglioneuromas and ganglioneuroblastomas) to date [7].
Late-Onset Central Hypoventilation Syndrome with Hypothalamic Dysfunction
Late-onset central hypoventilation syndrome with hypothalamic dysfunction (LO-CHS ) has been reported in previously well children who present after infancy [31]. This syndrome was first described in 1965 and is distinct from CCHS [32]. Both CCHS and LO-CHS can be associated with diseases of neural crest origin; however, features of hypothalamic dysfunction are not seen in CCHS [31]. Features of hypothalamic function reported in LO-CHS include hyperphagia, hypersomnolence, thermal dysregulation, emotional lability, and endocrinopathies. The diagnostic term “rapid onset obesity with hypothalamic dysfunction, hypoventilation, and autonomic dysregulation (ROHHAD) ” has also been used [33]. Clinical presentation can be varied with additional reported symptoms of thermal dysregulation, pain hyposensitivity, behavioral disorders, strabismus, pupillary anomalies, and tumors of neural crest origin [34]. A recent study of 23 children with this syndrome demonstrated negative PHOX2B gene sequencing in all cases [33]. Thus, this clinical presentation represents a syndrome clinically distinct from CCHS.
Evaluation and Diagnosis
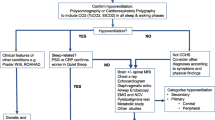
A diagnosis of CCHS should be considered in all children with evidence of hypoventilation without underlying cardiopulmonary, metabolic, neuromuscular, or brainstem dysfunction. Initial genetic testing should be performed with the PHOX2B screening test, which will identify the mutation in 95 % of CCHS cases [7]. If the screening test is negative but the patient’s phenotype supports the diagnosis of CCHS, a PHOX2B sequencing test may detect a subset of NPARMs [7]. Additionally, recent evidence indicates that further deletion/duplication analysis can identify another subset of patients affected (<1 %) [35]. Differential diagnoses for CCHS are wide and varied and should be ruled out while genetic testing for CCHS is pending (Table 17.1). Investigations to consider include chest radiograph, echocardiogram, and fluoroscopy of the diaphragm to identify any primary cardiopulmonary diseases or respiratory muscle weakness. Pulmonary function testing may be performed in cooperative older children. Infant pulmonary function testing, however, should be considered with caution due to the increased risk of hypoventilation with sedation. Intracranial lesions resulting in central hypoventilation can be identified by magnetic resonance imaging of the brain. Metabolic screening should be considered when clinical signs suggest inborn errors of metabolism.
Assessment of Hypoventilation
Children with a suspected diagnosis of CCHS should have comprehensive studies of respiratory physiology during wakefulness, REM, and NREM sleep to assess the degree of hypoventilation and the level of ventilatory support required. Testing should include all aspects of routine polysomnography including end-tidal/transcutaneous CO2 monitoring. Figure 17.1 shows different patterns on polysomnography that may be observed in children with CCHS [8, 36]. Ventilatory responses to hypoxia and hypercapnia during wakefulness and sleep can be measured to confirm the diagnosis and are usually flat [37]. This testing is performed primarily as a research tool but at times may be useful in establishing a diagnosis.
(a) Portions of a polysomnogram from an infant with congenital central hypoventilation syndrome. In the left panel, the infant is awake with normal oxyhemoglobin saturation but is hypoventilating slightly. At sleep onset (middle panel), end-tidal carbon dioxide levels begin to rise and oxyhemoglobin levels begin to drop. When placed on supplemental oxygen (right panel), the oxyhemoglobin levels normalize, but end-tidal carbon dioxide levels continue to rise (Marcus CL. 2001. Sleep-disordered breathing in children. American Journal of Respiratory and Critical Care Medicine. 164: 16–30. Official Journal of the American Thoracic Society. Reprinted with permission of the American Thoracic Society. Copyright © 2013 American Thoracic Society). (b) Polysomnogram epoch from an 8-year-old subject with CCHS during NREM sleep is shown. Following ventilator disconnection (arrow), the subject had an immediate 24-s central apnea, followed by an arousal. Cardiac oscillations are present on the airflow and PCO2 waveform channels. Y-axis parameters; time axis, clock time (in s) is shown, with the epoch number superimposed; C3-A2, C4-A1, O1-A2, and O2-A1 are EEG leads; LOC-A2 and ROCA1 are left and right electrooculograms, respectively; CHIN submental EMG signal, CHEST chest wall motion, ABDM abdominal wall motion, PNEUMFLO airflow measured with a pneumotachograph, PN pressure measured at the tracheostomy site, CAP end-tidal PCO2 waveform, ETCO 2 end-tidal PCO2 value, TCCO 2 transcutaneous PCO2, SAO 2 arterial oxygen saturation, PWF oximeter pulse waveform, LLEG left tibial EMG, RLEG right tibial EMG (Huang J et al. J Appl Physiol 2008. Am Physiol Soc, with permission)
The severity or chronicity of the central hypoventilation should be assessed by screening the patient for chronic respiratory acidosis and compensatory metabolic alkalosis (bicarbonate levels) and polycythemia (hemoglobin levels). Echocardiogram (ECG) and serum brain-type natriuretic peptide levels will determine if there is any evidence of pulmonary hypertension or cor pulmonale as a result of chronic hypoxemia.
Screening for Autonomic Dysfunction
Patients with CCHS and symptoms suggestive of autonomic dysfunction should be investigated appropriately. Barium enema or rectal biopsy should be performed for patients with constipation or abdominal distension to rule out Hirschsprung’s disease. Chest and abdominal imaging should be obtained early if there is any possibility of a neural crest tumor, particularly in patients with missense or frameshift mutations of the PHOX2B gene which correlate more frequently with this phenotype [29, 30].
Holter monitoring should be performed if there is clinical suspicion of cardiac arrhythmias, including bradycardias, that may necessitate pacemaker insertion. An ophthalmologic examination will identify any eye involvement and allow for early intervention to avoid interference with learning. Other measures of autonomic testing may be employed as clinically indicated, e.g. tilt testing to assess syncope [7].
Management
Goals of Care
The goal of treatment for CCHS is to ensure adequate oxygenation and ventilation during both wakefulness and sleep. This will improve long-term prognosis by reducing the risks of cor pulmonale and neurological insult from chronic hypoxemia.
Ventilation
The natural history of CCHS is that ventilatory responses to hypoxemia and hypercarbia do not improve over time. All newly diagnosed infants and children will require some form of assisted ventilation in the home setting. The proportion of all patients with CCHS who require ventilatory support during both wakefulness and sleep varies from 6 to 33 % in different study populations [16, 21]. Oxygen administration alone will improve oxygen saturation (SpO2) levels but will not prevent hypoventilation and the ensuing complications. Respiratory stimulants including theophylline, dexamphetamine, and clomipramine have not been shown to improve ventilatory drive in this patient population [38, 39]. Objective measurements of adequate ventilation, including pulse oximetry levels, should be monitored in the home. Ventilators are adjusted to maintain CO2 levels ideally between 30 and 40 mmHg and SpO2 ≥ 95 % [7]. Maintaining low-normal CO2 levels ensures that patients with CCHS have some ventilatory reserve when challenged during their daily activities, e.g., exercise, and when ill with intercurrent infections. Ventilator settings should be adjusted regularly during polysomnography or hospital admission, particularly in young children who are growing rapidly or patients who are symptomatic. Establishing optimal ventilator settings will help prevent neurocognitive dysfunction and avoid the development of atelectasis.
A variety of modalities of home ventilation are available to the patient with CCHS including portable positive pressure ventilation via tracheostomy, noninvasive ventilation (NIV) via nasal mask, diaphragmatic pacing, and, rarely, negative pressure ventilation. The advantages and disadvantages of each modality should be discussed with the family prior to decision-making (Table 17.2). Factors that determine the choice of technique include efficacy, practicality, psychosocial acceptance, complications, and cost. Ideally, the choice of ventilation should provide optimal technology to meet the patient’s lifestyle needs.
Transition of a patient with CCHS to a home portable ventilator should be established in the hospital under the supervision of an expert medical team. Discharge planning should include arrangements for the home ventilator, a backup ventilator, and home nursing support. In addition, a pulse oximeter and end-tidal CO2 monitor in the home allow for objective measurements of any clinical deterioration or change in ventilatory requirements.
During early infancy and childhood, patients with CCHS typically require more ventilatory support than older children and adults. This is because younger infants typically sleep for longer periods, are more prone to infections, and overall have more immature respiratory systems, which contribute to more instability in ventilation. It should be highlighted, however, that although there may be some maturation of the respiratory system, the patient never develops ventilatory responses and cannot be weaned from nocturnal ventilatory support. In a study of 196 patients with CCHS, two-thirds were able to adequately maintain ventilatory homeostasis during waking hours by age 12 months, while another quarter of the children were older than one year before they achieved such an ability [17]. This study also revealed a reduced need for intervention by medical professionals with age [17]. A greater healthcare burden was present among the 24-h ventilator-dependent patients; however, the need for hospitalization decreased with age in all patients [17].
The weaning of daytime assisted ventilation is best accomplished by sprint weaning where the child is removed from the ventilator for short periods of time during wakefulness [15]. The child with CCHS may not exhibit any signs of respiratory distress and so must be carefully monitored noninvasively during sprints to prevent hypoxemia or hypercapnia. The duration and frequency of sprints may be increased as tolerated, but progress will be hampered if performed too rapidly or without meticulous supervision.
Positive Pressure Ventilation via Tracheostomy
Positive pressure ventilation (PPV ) via tracheostomy is the commonest mode of ventilation used, particularly in infants and younger children. Many physicians agree that it is the safest form of ventilation to ensure adequate ventilation and oxygenation during the first years of life while the respiratory and central nervous systems are maturing [7]. While beneficial in older children, use of NIV is avoided in younger infants because of potential problems including difficulty with mask fitting, difficulty with triggering/cycling NIV ventilators, and the propensity of infants to take frequent naps. Older patients with tracheostomies may opt for decannulation and transition to NIV. Home positive pressure ventilators are portable and can be battery operated, improving mobility for the patient. Uncuffed tracheostomy tubes are typically used to permit a leak large enough to use a Passy-Muir valve, which encourages speech development, and to avoid subglottic stenosis. Pressure plateau ventilation or pressure control modes can be used to accommodate leak, compensate for tubing compliance, and ensure sufficient lung inflation.
While PPV via tracheostomy is generally a safe technique, there are a number of longer-term complications associated with it, including delayed speech and language development, colonization and infection of the lower respiratory tract, and tracheal granulation and stenosis [40]. There is also the low (≤6 %) but definite risk of tracheostomy-related death from cannula obstruction or accidental decannulation [41]. Due to the risk of complications, these patients will require caregivers available at all times that are trained to change and manage tracheostomies. This can further increase financial and social burdens on the patients and their families.
Despite the disadvantages, an epidemiological survey involving 196 patients with CCHS from 19 countries reported that more than 60 % of patients with CCHS were ventilated via tracheostomy [17]. In this study, the transition to NIV typically occurred between the ages of 6 and 11 years. A recent Japanese study of 37 patients with CCHS reported a similar proportion of 57 % ventilated by tracheostomy [42].
Noninvasive Bi-level Positive Airway Pressure
This is a mode of NIV via nasal mask or nasal prongs that does not require tracheostomy. These machines provide variable continuous flow via a blower (fan) and have a fixed leak that prevents CO2 retention and can compensate for leaks around the mask. When used in the timed/pressure control mode, they guarantee breath delivery in children with CCHS who cannot generate adequate large spontaneous breaths to trigger the ventilator [7]. NIV is not, however, suitable in isolation for patients requiring 24-h ventilation because it can interfere with daytime activity. Prolonged daily use of NIV can cause significant facial skin breakdown, nasal deformity, and injury to the eyes. Midfacial hypoplasia and dental malocclusion may occur in younger patients [43, 44]. One report of the use of NIV in two infants reported the development of class 3 dental malocclusion in both patients, after about 2 years, necessitating addition of negative pressure ventilation to reduce the duration of mask ventilation [45]. Presumably, midfacial hypoplasia is due to the chronic pressure exerted by the headgear and face mask unit against the malleable nasal, zygomatic, and maxillary areas in young patients and appears to be less of an issue with modern interfaces [44]. The severity of these complications can be reduced by alternating between nasal masks and nasal pillows, using customized masks, and avoiding tight-fitting interfaces [46]. Villa et al. described successful correction of midface hypoplasia with an orthodontic device in a 7-year-old child with CCHS who had been ventilated with a nasal mask from the age of 9 months [44].
Other potential problems encountered with use of NIV in children with CCHS include gastric overdistension resulting in gastroesophageal reflux. In addition, incorrect positioning of the nasal interface or oral leakage during sleep could cause pressure losses and reduce the effectiveness of NIV [47].
Another frequent challenge to the successful use of NIV is poor patient adherence to treatment. One study reported that adherence to NIV in children and adolescents with obstructive sleep apnea was related primarily to family and demographic factors rather than severity of apnea, pressure levels, or psychosocial functioning [48]. Important supportive mechanisms to promote NIV adherence include education of both parents and patients along with anticipatory guidance for common problems, side effects, and device troubleshooting [49]. Another intervention to promote NIV adherence is to ensure positive first experiences for patients with NIV, including during in-laboratory or in-hospital treatment trials [49].
The first successful case of NIV use for CCHS was reported in 1987 in a 6-year-old child who had previously received mechanical ventilation [50]. A 2004 survey of 196 patients with CCHS (age range 0.4–38 years, mean 10.2 years) reported that 55 (28.1 %) were using NIV alone [17].
Some patients have been successfully transitioned from PPV via tracheostomy to NIV support upon reaching school age when the clinical course is more stable and the child is able to accept mask ventilation and cooperate fully. Limitations to transition include the availability of suitable and comfortable nasal interfaces for the child. In cases where there is pressure loss because of open mouth breathing, the concomitant use of chin straps or full face masks can permit adequate ventilation. One must also consider that, when transitioning to NIV from PPV via tracheostomy, there will be the added load of upper airway resistance to overcome, which may necessitate higher ventilator settings. Evaluation of the upper airway for possible tonsillectomy and adenoidectomy may be indicated in patients requiring high settings. NIV generally does not provide pressures as high as those provided by invasive ventilators, and children may require intubation and greater levels of ventilatory support during acute respiratory illnesses.
Patients with CCHS may have life-threatening events if not adequately ventilated during sleep; thus, documentation of the adequacy of NIV settings is essential before chronic NIV treatment can be safely initiated [51]. As with PPV, optimal NIV settings should be determined and titrated periodically in the sleep laboratory. The American Academy of Sleep Medicine published guidelines for sleep center adjustment of NIV in patients with stable chronic alveolar hypoventilation syndromes including those with central respiratory control disturbances [51]. The underlying concept is that a successful NIV titration is one in which there is an optimized trade-off between increasing pressure to yield efficacy in supporting ventilation and decreasing pressure to minimize emergence of pressure-related side effects [51].
One recent case report described a 16-year-old female with CCHS who was successfully transitioned to a new modality of NIV, average volume-assured pressure support (AVAPS), that automatically adjusts the pressure support level in order to provide a consistent tidal volume [52]. AVAPS has been recently introduced as a new additional mode for bi-level pressure ventilation that automatically adjusts the pressure support level to provide a consistent tidal volume. Studies on its physiologic and clinical effects are few and more are needed [53, 54].
Negative Pressure Ventilation
Negative pressure ventilation (NPV ) causes inspiration by generating a negative inspiratory pressure around the chest and abdomen. The popularity of NPV, however, has been limited by the risk of obstructive sleep apnea because of lack of synchrony between vocal fold opening and thoracic inspiratory efforts. In one report, additional mask CPAP was used successfully in cases of upper airway obstruction during NPV [55].
Negative pressure ventilators are bulky and not portable, and some necessitate that the patient remains in the supine position. In addition, the chest shells or wraps currently available can cause discomfort, skin breakdown, and leaks that make their use unacceptable in many cases. NPV has been used rarely since the advent of PPV and NIV. It may be an acceptable alternative for those requiring ventilation during sleep if other modes of ventilation are unsuitable. In rare cases, it has permitted decannulation in patients with CCHS.
Diaphragmatic Pacing
This mode of ventilation involves electrical stimulation of the phrenic nerve that results in diaphragmatic contraction. In 1972, Glenn et al. first demonstrated that electrical stimulation of the phrenic nerves resulted in rhythmic contraction of the diaphragm (pacing) and could provide full-time, long-term ventilatory support for an adult patient with acquired central hypoventilation [56]. In 1978, Hunt et al. reported the first three cases of diaphragmatic pacing in infants with CCHS [57].
Typically, pacing during the day and PPV by mask or tracheostomy at night affords more daytime mobility for active children who require ventilation 24 h per day. This can both improve quality of life and optimize neurodevelopmental progress. Pacing has not been used for 24 h a day because of a theoretical concern of damage to the phrenic nerves. Patients with CCHS who may best benefit from diaphragm pacing include those with no or mild intrinsic lung disease with preserved phrenic nerve-diaphragm axis integrity and presence of a tracheostomy at least during the initiation of pacing [58].
Diaphragmatic pacing requires surgical implantation of bilateral phrenic nerve electrodes, in the intrathoracic or intracervical segments of the nerve. The cervical approach in the lower neck is a less desirable site for placement because the phrenic nerve forms a complex of rootlets that only unite in the thorax. Thus, the cervical approach may only capture 75 % of the fibers in the neck [59]. Bilateral receivers are implanted subcutaneously that transmit radio frequency signals from a battery-operated external pulse generator to the phrenic nerve electrodes. The patient also wears an energy transfer coil on the skin over the receiver. When a signal arrives from the external pulse generator, it is converted via the subcutaneous receivers to an electrical current that stimulates the phrenic nerve (Fig. 17.2). Settings on the external generator include respiratory rate and electrical voltage and are adjusted to give enough tidal volume to allow for adequate oxygenation and ventilation.
(a) Diaphragmatic pacing device showing the external pulse generator and energy transfer coils. (Reprinted from Paediatric Respiratory Reviews, 2011 Dec; 12 (4):253–63. Healy F, Marcus CL. Congenital central hypoventilation syndrome in children, pages 253–63, Copyright 2011, with permission from Elsevier). (b) Patient with congenital central hypoventilation syndrome post tracheal decannulation who uses nocturnal diaphragmatic pacing. Here she is wearing the energy transfer coils of her diaphragmatic pacer and holding the external pulse generator during setup for a titration polysomnogram (Reprinted from Paediatric Respiratory Reviews, 2011 Dec; 12 (4):253–63. Healy F, Marcus CL. Congenital central hypoventilation syndrome in children, pages 253–63, Copyright 2011, with permission from Elsevier)
The goal with diaphragm pacing is to minimize the electrical stimulation while providing optimal ventilation and oxygenation. Pacing is typically initiated 4–6 weeks after surgical implantation to allow tissue reaction around the electrodes to stabilize [15]. Training of the muscle fibers is necessary to sustain pacing for the required 12–16 h per day, and a period of 3–4 months is usually required to attain full pacing [15]. In patients with CCHS who also have cardiac pacemakers, it is important to minimize the potential for electromagnetic interference by ensuring that the cardiac pacemaker is bipolar [7].
Potential complications of pacing include equipment failure, infection (e.g., empyema), and late injury due to fibrosis or tension on the phrenic nerve [60]. In one study of 33 infants and children using diaphragmatic pacing, receiver failure was the most common cause of internal component failure [61]. However, the receiver can be replaced without thoracotomy because it is located in a subcutaneous pocket. Longevity of equipment should improve as hardware becomes more refined over time. Flageole et al. reported their longest survivor to date was paced for 21 years [59]. This patient had successfully tolerated seven separate procedures for receiver or wire replacement.
Pacing at night may permit tracheal decannulation. However, in some decannulated patients, obstructive sleep apnea occurs because vocal fold opening does not occur with a paced inspiration (Fig. 17.3). In some cases this may be overcome by adjusting settings on the pacers to lengthen inspiratory time and/or decrease the force of inspiration. If the obstruction persists, then these patients may be better managed by NIV. Patients should be monitored by polysomnography to ensure that they do not have obstructive sleep apnea related to diaphragmatic pacing.
Thirty-second epoch from a titration polysomnogram image from the patient with congenital central hypoventilation syndrome in Fig. 17.2b who had previously been decannulated and was using nocturnal diaphragmatic pacing . During the study the patient experienced persistent partial upper airway obstruction while paced, with stridor, paradoxical breathing, and oxyhemoglobin desaturation. C3-A2, O1-A2, C4-A1, O2-A1 electroencephalogram channels, LOC-A2 and ROCA1 left and right electrooculograms, CHIN submental EMG, EKG electrocardiogram, NPAF nasal pressure airflow, CHEST thoracic movement, ABDM abdominal movement, CAP capnography, ETCO 2 end-tidal carbon dioxide level (torr), SAO 2 arterial oxygen saturation, PWF oximeter pulse waveform, TCCO 2 transcutaneous carbon dioxide level (torr), RLEG right tibial EMG, LLEG left tibial EMG (Reprinted from Paediatric Respiratory Reviews, 2011 Dec; 12 (4):253–63. Healy F, Marcus CL. Congenital central hypoventilation syndrome in children, pages 253–63, Copyright 2011, with permission from Elsevier)
All patients with CCHS who rely on diaphragm pacing should have an additional backup diaphragm pacer transmitter already set to their physiological requirements. An additional advantage of a second transmitter is that, for children who are paced during the day, the backup transmitter can be set to deliver optimal settings for exercise. This allows the child to use one transmitter during school and the other transmitter during a moderate level of age-appropriate activity (settings for each should be ascertained during physiologic assessments at a center with expertise in diaphragmatic pacing) [7].
Diaphragmatic pacers can work well, but patients must have access to teams with the necessary expertise in maintaining them. This includes staff with the ability to set the pacers with a digital oscilloscope and surface electromyogram recordings. In addition, the implantation of the internal components (receivers, connecting wires, and phrenic nerve electrodes) requires thoracic surgery and should only be implanted by experienced pediatric surgeons at a center with the appropriate expertise [7].
Ongoing Care and Monitoring
Screening for Medical Comorbidities Associated with CCHS
Children with CCHS require input by a wide variety of medical specialists due to the array of associated medical conditions including autonomic dysfunction and sequelae of ventilatory insufficiency and hypoxemia. Neurocognitive assessments should be considered as patients with CCHS have an increased risk of learning disabilities and developmental delay [62, 63]. Most children with CCHS have adequate growth and nutrition, but some may have swallowing incoordination requiring temporary gastrostomies [15].
Genetic Counseling
Genetic counseling should be offered to the parents of children diagnosed with CCHS irrespective of whether a genetic mutation is identified or not. This will provide information on the nature, autosomal dominant inheritance pattern, and implications of this disorder to help them make informed medical and personal decisions. If a specific PHOX2B mutation is identified in their child, parents should be offered testing to determine their own risk for later-onset CCHS or mosaicism [28]. Risk to siblings and other family members will depend on the genotype status of the parents.
Home Care and Nursing Support
The majority of care for children with CCHS occurs in the home setting where parents can easily be overwhelmed by sophisticated medical equipment and coordination of appointments with multiple medical professionals. Children with CCHS are a particularly vulnerable group who require skilled care and monitoring, particularly at sleep onset when they could suffer severe hypoventilation or even complete respiratory arrest if ventilation is not adequately supported. Additionally, these children do not typically develop fever, tachypnea, or dyspnea in response to respiratory tract infections, even pneumonia, and thus careful assessment is necessary during illness [13, 64]. Caregivers need to be well educated about CCHS, and nursing support, if available, can be very helpful. One study reported that, of 196 families with a child with CCHS, 49.5 % had no nursing support at night [17]. Access to other skilled healthcare professionals including social workers, speech therapists, physical therapists, and special education teachers may be needed to optimize care.
Social Issues and Quality of Life
Most children with CCHS will have a good quality of life if diagnosed early and managed rigorously. There should be minimal restrictions on daytime activity; however, children with CCHS lack the appropriate ventilatory and autonomic responses to heavy or extended exercise [65]. If swimming, they should be carefully supervised regardless of the presence or absence of a tracheostomy (swimming is not recommended for those with tracheostomies) [7]. Children with CCHS do not derive discomfort from breath-holding and are therefore at heightened risk of drowning.
Normal risk-taking behavior during adolescence places CCHS patients in great danger. Sedative medications and central nervous system depressants such as alcohol or illicit drugs should be avoided as much as possible, as they worsen hypoventilation. Chen et al. reported three cases of young adults with CCHS who had severe adverse events related to alcohol use, including coma and death [66]. Parents and patients should be counseled about these specific risks prior to and throughout adolescence. Patients should wear MedicAlert bracelets to warn paramedical and medical staff in case of emergency.
In the majority of cases, CCHS does not cause significant levels of psychological distress in caregivers, who typically report good coping resources and high levels of motivation to provide care [17, 63]. Some studies do, however, report higher levels of marital discord [63].
Perioperative Care
Children with CCHS will require ventilatory support during sedation or general anesthesia. Anesthetic care for the child with CCHS can be challenging. To avoid the need for additional ventilation during wakefulness and prolonged hospitalization, anesthetic drugs with the shortest half-life should be chosen, e.g., remifentanil, nitrous oxide, and sevoflurane [67]. For other procedures, the use of regional anesthesia techniques may avoid the central effects of anesthetic drugs. Cardiovascular complications of CCHS including cor pulmonale and autonomic dysfunction may also impact perioperative care. Metabolic alkalosis should be prevented as this can further inhibit central respiratory drive. Drugs with negative chronotropic effects or direct effects on blood pressure should be avoided.
Pregnancy
Increasing numbers of patients with CCHS are now progressing to parenthood themselves [68, 69]. Although most current cases of CCHS represent de novo mutations in the PHOX2B gene, some cases are inherited in an autosomal dominant fashion. If both parent and children are affected, this creates greater challenges for the parent who must monitor the ventilatory needs of both themselves and their child. Prenatal testing by amniocentesis for PHOX2B allows for anticipated cases to be delivered in appropriate tertiary centers that can manage ventilation of both mother and child. Pregnant women with CCHS will require frequent physiological monitoring because they do not have the central respiratory drive to meet the increased respiratory load caused by the enlarging uterus [68]. Diaphragmatic pacing is poorly tolerated after Cesarian section due to the abdominal incision, and alternative means of ventilation will be required [68].
Long-Term Prognosis
Long-term follow-up of patients with CCHS and neurodevelopmental outcome reveal a broad range of results with a great deal of variability, usually correlating with the degree of severity of their CCHS [15]. Mortality rates ranging from 8 to 38 % have been documented in various CCHS patient cohorts [21, 42, 58, 63]. The main causes of death include cor pulmonale, pneumonia, and aspiration.
With an increasing awareness of the disease entity, patients will be recognized and treated earlier than in the past. Advancements in home ventilation and monitoring abilities as well as vigilant ongoing patient assessment and equipment maintenance by medical teams will further improve prognosis. As these children survive to adulthood, the development of transition programs with age-appropriate support will contribute to independent lifestyles, careers, and family lives for this complex population.
Future Directions
As the prognosis for patients with CCHS improves, there remains, however, the need to ensure that ventilatory requirements are addressed with ongoing research into new, more acceptable forms of artificial ventilation. The deficiencies in current methods of ventilation are most apparent in those children who require support 24 h a day. During varied levels of daytime activity and exercise, these patients may become hypercapnic and hypoxemic but cannot adequately compensate because of fixed artificial ventilatory support with either diaphragmatic pacers or a mechanical ventilator.
At present the only effective therapeutic option for patients diagnosed with CCHS is mechanical ventilation. One potential treatment was recently reported in two women with CCHS who demonstrated improved ventilatory responses to hypoxia and hypercapnia after taking the progestin contraceptive, desogestrel [70]. The exact mechanism of action of desogestrel remains unclear, but it has been postulated that it may stimulate or activate “alternative” central and/or peripheral chemosensitive neural circuits [70]. Further trials are warranted to determine the true potential of this treatment option.
Since the discovery of the PHOX2B mutation, there has been increasing interest in the possibility of a genetic therapy for CCHS. The severity of the CCHS phenotype correlates with the length of polyalanine expansions, which ultimately lead to the formation of toxic intracytoplasmic aggregates and impaired PHOX2B-mediated transactivation [71]. A recent study by Zanni et al. identified two molecules, 17-AAG and curcumin, that were effective in vitro in counteracting these pathological effects [71]. The ultimate goal of such research is to identify medications that, if initiated in early infancy or even in utero, could modify disease progression and avoid the need for mechanical ventilation, permitting significant improvements in quality of life, morbidity, and mortality for these patients.
Continuing investigation of the genetic intricacies of this syndrome is needed, with ongoing attempts to correlate the genotype-phenotype relationship and improve patient care and prognosis. In addition, the presumed genetic etiology of patients with late-onset central hypoventilation and hypothalamic dysfunction remains to be determined. As with any complex illness, further research, including autopsy studies using new molecular technologies, will help to define the anatomical and physiological features of this syndrome.
References
Amiel J, Laudier B, Attie-Bitach T, Trang H, de Pontual L, Gener B, et al. Polyalanine expansion and frameshift mutations of the paired-like homeobox gene PHOX2B in congenital central hypoventilation syndrome. Nat Genet. 2003;33(4):459–61.
Weese-Mayer DE, Berry-Kravis EM, Zhou L, Maher BS, Silvestri JM, Curran ME, et al. Idiopathic congenital central hypoventilation syndrome: analysis of genes pertinent to early autonomic nervous system embryologic development and identification of mutations in PHOX2b. Am J Med Genet A. 2003;123A(3):267–78.
Antic NA, Malow BA, Lange N, McEvoy RD, Olson AL, Turkington P, et al. PHOX2B mutation-confirmed congenital central hypoventilation syndrome: presentation in adulthood. Am J Respir Crit Care Med. 2006;174(8):923–7.
Matera I, Bachetti T, Puppo F, Di Duca M, Morandi F, Casiraghi GM, et al. PHOX2B mutations and polyalanine expansions correlate with the severity of the respiratory phenotype and associated symptoms in both congenital and late onset Central Hypoventilation syndrome. J Med Genet. 2004;41(5):373–80.
Repetto GM, Corrales RJ, Abara SG, Zhou L, Berry-Kravis EM, Rand CM, et al. Later-onset congenital central hypoventilation syndrome due to a heterozygous 24-polyalanine repeat expansion mutation in the PHOX2B gene. Acta Paediatr. 2009;98(1):192–5.
Weese-Mayer DE, Berry-Kravis EM, Zhou L. Adult identified with congenital central hypoventilation syndrome—mutation in PHOX2b gene and late-onset CHS. Am J Respir Crit Care Med. 2005;171(1):88.
Weese-Mayer DE, Berry-Kravis EM, Ceccherini I, Keens TG, Loghmanee DA, Trang H. An official ATS clinical policy statement: congenital central hypoventilation syndrome: genetic basis, diagnosis, and management. Am J Respir Crit Care Med. 2010;181(6):626–44.
Huang J, Colrain IM, Panitch HB, Tapia IE, Schwartz MS, Samuel J, et al. Effect of sleep stage on breathing in children with central hypoventilation. J Appl Physiol. 2008;105(1):44–53.
Orem JM, Lovering AT, Vidruk EH. Excitation of medullary respiratory neurons in REM sleep. Sleep. 2005;28(7):801–7.
Gozal D, Marcus CL, Ward SL, Keens TG. Ventilatory responses to passive leg motion in children with congenital central hypoventilation syndrome. Am J Respir Crit Care Med. 1996;153(2):761–8.
Paton JY, Swaminathan S, Sargent CW, Hawksworth A, Keens TG. Ventilatory response to exercise in children with congenital central hypoventilation syndrome. Am Rev Respir Dis. 1993;147(5):1185–91.
Gozal D, Simakajornboon N. Passive motion of the extremities modifies alveolar ventilation during sleep in patients with congenital central hypoventilation syndrome. Am J Respir Crit Care Med. 2000;162(5):1747–51.
Shea SA, Andres LP, Paydarfar D, Banzett RB, Shannon DC. Effect of mental activity on breathing in congenital central hypoventilation syndrome. Respir Physiol. 1993;94(3):251–63.
Tremoureux L, Raux M, Hudson AL, Ranohavimparany A, Straus C, Similowski T. Does the supplementary motor area keep patients with Ondine’s curse syndrome breathing while awake? PLoS One. 2014;9(1), e84534.
Chen ML, Keens TG. Congenital central hypoventilation syndrome: not just another rare disorder. Paediatr Respir Rev. 2004;5(3):182–9.
Lesser DJ, Ward SL, Kun SS, Keens TG. Congenital hypoventilation syndromes. Semin Respir Crit Care Med. 2009;30(3):339–47.
Vanderlaan M, Holbrook CR, Wang M, Tuell A, Gozal D. Epidemiologic survey of 196 patients with congenital central hypoventilation syndrome. Pediatr Pulmonol. 2004;37(3):217–29.
Trochet D, de Pontual L, Straus C, Gozal D, Trang H, Landrieu P, et al. PHOX2B germline and somatic mutations in late-onset central hypoventilation syndrome. Am J Respir Crit Care Med. 2008;177(8):906–11.
Commare MC, Francois B, Estournet B, Barois A. Ondine’s curse: a discussion of five cases. Neuropediatrics. 1993;24(6):313–8.
Silvestri JM, Hanna BD, Volgman AS, Jones PJ, Barnes SD, Weese-Mayer DE. Cardiac rhythm disturbances among children with idiopathic congenital central hypoventilation syndrome. Pediatr Pulmonol. 2000;29(5):351–8.
Trang H, Dehan M, Beaufils F, Zaccaria I, Amiel J, Gaultier C. The French Congenital Central Hypoventilation Syndrome Registry: general data, phenotype, and genotype. Chest. 2005;127(1):72–9.
Trang H, Boureghda S, Denjoy I, Alia M, Kabaker M. 24-hour BP in children with congenital central hypoventilation syndrome. Chest. 2003;124(4):1393–9.
Gronli JO, Santucci BA, Leurgans SE, Berry-Kravis EM, Weese-Mayer DE. Congenital central hypoventilation syndrome: PHOX2B genotype determines risk for sudden death. Pediatr Pulmonol. 2008;43(1):77–86.
Goldberg DS, Ludwig IH. Congenital central hypoventilation syndrome: ocular findings in 37 children. J Pediatr Ophthalmol Strabismus. 1996;33(3):175–80.
Rohrer T, Trachsel D, Engelcke G, Hammer J. Congenital central hypoventilation syndrome associated with Hirschsprung’s disease and neuroblastoma: case of multiple neurocristopathies. Pediatr Pulmonol. 2002;33(1):71–6.
Swaminathan S, Gilsanz V, Atkinson J, Keens TG. Congenital central hypoventilation syndrome associated with multiple ganglioneuromas. Chest. 1989;96(2):423–4.
Haddad GG, Mazza NM, Defendini R, Blanc WA, Driscoll JM, Epstein MA, et al. Congenital failure of automatic control of ventilation, gastrointestinal motility and heart rate. Medicine (Baltimore). 1978;57(6):517–26.
Weese-Mayer DE, Marazita ML, Rand CM, Berry-Kravis EM. Congential Central Hypoventilation Syndrome. In: Pagon RA, Adam MP, Ardinger HH, Wallace SE, Amemiya A, Bean LJH et al, editors. GeneReviews [Internet]. Seattle (WA): University of Washington, Seattle; 1993–2016.
Berry-Kravis EM, Zhou L, Rand CM, Weese-Mayer DE. Congenital central hypoventilation syndrome: PHOX2B mutations and phenotype. Am J Respir Crit Care Med. 2006;174(10):1139–44.
Trochet D, O’Brien LM, Gozal D, Trang H, Nordenskjold A, Laudier B, et al. PHOX2B genotype allows for prediction of tumor risk in congenital central hypoventilation syndrome. Am J Hum Genet. 2005;76(3):421–6.
Katz ES, McGrath S, Marcus CL. Late-onset central hypoventilation with hypothalamic dysfunction: a distinct clinical syndrome. Pediatr Pulmonol. 2000;29(1):62–8.
Fishman LS, Samson JH, Sperling DR. Primary alveolar hypoventilation syndrome (Ondine’s curse). Am J Dis Child. 1965;110:155–61.
Ize-Ludlow D, Gray JA, Sperling MA, Berry-Kravis EM, Milunsky JM, Farooqi IS, et al. Rapid-onset obesity with hypothalamic dysfunction, hypoventilation, and autonomic dysregulation presenting in childhood. Pediatrics. 2007;120(1):e179–88.
Abaci A, Catli G, Bayram E, Koroglu T, Olgun HN, Mutafoglu K, et al. A case of rapid-onset obesity with hypothalamic dysfunction, hypoventilation, autonomic dysregulation, and neural crest tumor: ROHHADNET syndrome. Endocr Pract. 2013;19(1):e12–6.
Jennings LJ, Yu M, Rand CM, Kravis N, Berry-Kravis EM, Patwari PP, et al. Variable human phenotype associated with novel deletions of the PHOX2B gene. Pediatr Pulmonol. 2012;47(2):153–61.
Marcus CL. Sleep-disordered breathing in children. Am J Respir Crit Care Med. 2001;164(1):16–30.
Paton JY, Swaminathan S, Sargent CW, Keens TG. Hypoxic and hypercapnic ventilatory responses in awake children with congenital central hypoventilation syndrome. Am Rev Respir Dis. 1989;140(2):368–72.
Frank Y, Kravath RE, Inoue K, Hirano A, Pollak CP, Rosenberg RN, et al. Sleep apnea and hypoventilation syndrome associated with acquired nonprogressive dysautonomia: clinical and pathological studies in a child. Ann Neurol. 1981;10(1):18–27.
Proulx F, Weber ML, Collu R, Lelievre M, Larbrisseau A, Delisle M. Hypothalamic dysfunction in a child: a distinct syndrome? Report of a case and review of the literature. Eur J Pediatr. 1993;152(6):526–9.
Jiang D, Morrison GA. The influence of long-term tracheostomy on speech and language development in children. Int J Pediatr Otorhinolaryngol. 2003;67 Suppl 1:S217–20.
Kremer B, Botos-Kremer AI, Eckel HE, Schlondorff G. Indications, complications, and surgical techniques for pediatric tracheostomies—an update. J Pediatr Surg. 2002;37(11):1556–62.
Hasegawa H, Kawasaki K, Inoue H, Umehara M, Takase M. Epidemiologic survey of patients with congenital central hypoventilation syndrome in Japan. Pediatr Int. 2012;54(1):123–6.
Fauroux B, Lavis JF, Nicot F, Picard A, Boelle PY, Clement A, et al. Facial side effects during noninvasive positive pressure ventilation in children. Intensive Care Med. 2005;31(7):965–9.
Villa MP, Pagani J, Ambrosio R, Ronchetti R, Bernkopf E. Mid-face hypoplasia after long-term nasal ventilation. Am J Respir Crit Care Med. 2002;166(8):1142–3.
Tibballs J, Henning RD. Noninvasive ventilatory strategies in the management of a newborn infant and three children with congenital central hypoventilation syndrome. Pediatr Pulmonol. 2003;36(6):544–8.
Simonds AK. Home ventilation. Eur Respir J. 2003;47:38s–46.
Migliori C, Cavazza A, Motta M, Bottino R, Chirico G. Early use of Nasal-BiPAP in two infants with Congenital Central Hypoventilation syndrome. Acta Paediatr. 2003;92(7):823–6.
DiFeo N, Meltzer LJ, Beck SE, Karamessinis LR, Cornaglia MA, Traylor J, et al. Predictors of positive airway pressure therapy adherence in children: a prospective study. J Clin Sleep Med. 2012;8(3):279–86.
Sawyer AM, Gooneratne NS, Marcus CL, Ofer D, Richards KC, Weaver TE. A systematic review of CPAP adherence across age groups: clinical and empiric insights for developing CPAP adherence interventions. Sleep Med Rev. 2011;15(6):343–56.
Ellis ER, McCauley VB, Mellis C, Sullivan CE. Treatment of alveolar hypoventilation in a six-year-old girl with intermittent positive pressure ventilation through a nose mask. Am Rev Respir Dis. 1987;136(1):188–91.
Berry RB, Chediak A, Brown LK, Finder J, Gozal D, Iber C, et al. Best clinical practices for the sleep center adjustment of noninvasive positive pressure ventilation (NPPV) in stable chronic alveolar hypoventilation syndromes. J Clin Sleep Med. 2010;6(5):491–509.
Vagiakis E, Koutsourelakis I, Perraki E, Roussos C, Mastora Z, Zakynthinos S, et al. Average volume-assured pressure support in a 16-year-old girl with congenital central hypoventilation syndrome. J Clin Sleep Med. 2010;6(6):609–12.
Ambrogio C, Lowman X, Kuo M, Malo J, Prasad AR, Parthasarathy S. Sleep and non-invasive ventilation in patients with chronic respiratory insufficiency. Intensive Care Med. 2009;35(2):306–13.
Storre JH, Seuthe B, Fiechter R, Milioglou S, Dreher M, Sorichter S, et al. Average volume-assured pressure support in obesity hypoventilation: a randomized crossover trial. Chest. 2006;130(3):815–21.
Hartmann H, Jawad MH, Noyes J, Samuels MP, Southall DP. Negative extrathoracic pressure ventilation in central hypoventilation syndrome. Arch Dis Child. 1994;70(5):418–23.
Glenn WW, Holcomb WG, McLaughlin AJ, O’Hare JM, Hogan JF, Yasuda R. Total ventilatory support in a quadriplegic patient with radiofrequency electrophrenic respiration. N Engl J Med. 1972;286(10):513–6.
Hunt CE, Matalon SV, Thompson TR, Demuth S, Loew JM, Liu HM, et al. Central hypoventilation syndrome: experience with bilateral phrenic nerve pacing in 3 neonates. Am Rev Respir Dis. 1978;118(1):23–8.
Weese-Mayer DE, Hunt CE, Brouillette RT, Silvestri JM. Diaphragm pacing in infants and children. J Pediatr. 1992;120(1):1–8.
Ali A, Flageole H. Diaphragmatic pacing for the treatment of congenital central alveolar hypoventilation syndrome. J Pediatr Surg. 2008;43(5):792–6.
DiMarco AF. Phrenic nerve stimulation in patients with spinal cord injury. Respir Physiol Neurobiol. 2009;169(2):200–9.
Weese-Mayer DE, Morrow AS, Brouillette RT, Ilbawi MN, Hunt CE. Diaphragm pacing in infants and children. A life-table analysis of implanted components. Am Rev Respir Dis. 1989;139(4):974–9.
Zelko FA, Nelson MN, Leurgans SE, Berry-Kravis EM, Weese-Mayer DE. Congenital central hypoventilation syndrome: neurocognitive functioning in school age children. Pediatr Pulmonol. 2010;45(1):92–8.
Marcus CL, Jansen MT, Poulsen MK, Keens SE, Nield TA, Lipsker LE, et al. Medical and psychosocial outcome of children with congenital central hypoventilation syndrome. J Pediatr. 1991;119(6):888–95.
Idiopathic congenital central hypoventilation syndrome: diagnosis and management. American Thoracic Society. Am J Respir Crit Care Med. 1999;160(1):368–73.
Silvestri JM, Weese-Mayer DE, Flanagan EA. Congenital central hypoventilation syndrome: cardiorespiratory responses to moderate exercise, simulating daily activity. Pediatr Pulmonol. 1995;20(2):89–93.
Chen ML, Turkel SB, Jacobson JR, Keens TG. Alcohol use in congenital central hypoventilation syndrome. Pediatr Pulmonol. 2006;41(3):283–5.
Strauser LM, Helikson MA, Tobias JD. Anesthetic care for the child with congenital central alveolar hypoventilation syndrome (Ondine’s curse). J Clin Anesth. 1999;11(5):431–7.
Sritippayawan S, Hamutcu R, Kun SS, Ner Z, Ponce M, Keens TG. Mother-daughter transmission of congenital central hypoventilation syndrome. Am J Respir Crit Care Med. 2002;166(3):367–9.
Silvestri JM, Chen ML, Weese-Mayer DE, McQuitty JM, Carveth HJ, Nielson DW, et al. Idiopathic congenital central hypoventilation syndrome: the next generation. Am J Med Genet. 2002;112(1):46–50.
Straus C, Trang H, Becquemin MH, Touraine P, Similowski T. Chemosensitivity recovery in Ondine’s curse syndrome under treatment with desogestrel. Respir Physiol Neurobiol. 2010;171(2):171–4.
Di Zanni E, Bachetti T, Parodi S, Bocca P, Prigione I, Di Lascio S, et al. In vitro drug treatments reduce the deleterious effects of aggregates containing polyAla expanded PHOX2B proteins. Neurobiol Dis. 2012;45(1):508–18.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer Science+Business Media New York
About this chapter
Cite this chapter
Healy, F., Marcus, C.L. (2016). Care of the Child with Congenital Central Hypoventilation Syndrome. In: Sterni, L., Carroll, J. (eds) Caring for the Ventilator Dependent Child. Respiratory Medicine. Humana Press, New York, NY. https://doi.org/10.1007/978-1-4939-3749-3_17
Download citation
DOI: https://doi.org/10.1007/978-1-4939-3749-3_17
Published:
Publisher Name: Humana Press, New York, NY
Print ISBN: 978-1-4939-3747-9
Online ISBN: 978-1-4939-3749-3
eBook Packages: MedicineMedicine (R0)