Abstract
Primary aims in diagnosis and treatment of undescended testes (UDT):
-
1.
Improve fertility.
-
2.
Preserve testosterone production.
-
3.
Reduce cancer risk.
Secondary aims:
-
1.
Repositioning the testis into the dependent scrotum without atrophy.
-
2.
Normal scrotal appearance.
-
3.
Distinction between UDT versus retractile testes.
Summary of evidence for these goals:
-
Limited available data suggest paternity rates in men with former unilateral UDT are similar to those of normal men, whereas paternity rates are diminished with formerly bilateral UDT.
-
One RCT reported preoperative intranasal GNRH improved the fertility index (adult spermatogonia/tubule) over patients undergoing orchiopexy alone.
-
The overall risk that an operated UDT will develop cancer is <0.5 %; risk for nonoperated UDT is unknown.
-
While cancer risk doubles if orchiopexy is done after age 13 versus before, 69 patients have to be operated before that age to prevent one tumor in males between ages 13 and 55 years.
-
Surgical reports on orchiopexy rarely state final testicular position or objectively assess testicular size. Based on “intra-scrotal” position, a RCT reported 94 % success with both tradition inguinal and scrotal orchiopexy for palpable UDT.
-
Meta-analysis found no difference between open versus laparoscopic orchiopexy for nonpalpable testis.
-
A systematic review found a 5 % benefit to two-stage versus single-stage Fowler-Stephens orchiopexy, but cautioned data quality was poor.
-
Our review found a single study using a parent questionnaire that reported no difference in satisfaction between inguinal versus scrotal orchiopexy.
-
Surgeons perform approximately two times more orchiopexies than the rate of UDT, suggesting confusion between UDT versus retractile testes.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
Primary aims in diagnosis and treatment of undescended testes (UDT):
-
1.
Improve fertility.
-
2.
Preserve testosterone production.
-
3.
Reduce cancer risk.
Secondary aims:
-
1.
Repositioning the testis into the dependent scrotum without atrophy
-
2.
Normal scrotal appearance
-
3.
Distinction between UDT versus retractile testes
Summary of evidence for these goals:
-
Limited available data suggest paternity rates in men with former unilateral UDT are similar to those of normal men, whereas paternity rates are diminished with formerly bilateral UDT.
-
One RCT reported preoperative intranasal GNRH improved the fertility index (adult spermatogonia/tubule) over patients undergoing orchiopexy alone.
-
The overall risk that an operated UDT will develop cancer is <0.5 %; risk for nonoperated UDT is unknown.
-
While cancer risk doubles if orchiopexy is done after age 13 versus before, 69 patients have to be operated before that age to prevent one tumor in males between ages 13 and 55 years.
-
Surgical reports on orchiopexy rarely state final testicular position or objectively assess testicular size. Based on “intra-scrotal” position, a RCT reported 94 % success with both traditional inguinal and scrotal orchiopexy for palpable UDT.
-
Meta-analysis found no difference between open versus laparoscopic orchiopexy for nonpalpable testis.
-
A systematic review found a 5 % benefit to two-stage versus single-stage Fowler-Stephens orchiopexy, but cautioned data quality was poor.
-
Our review found a single study using a parent questionnaire that reported no difference in satisfaction between inguinal versus scrotal orchiopexy.
-
Surgeons perform approximately two times more orchiopexies than the rate of UDT, suggesting confusion between UDT versus retractile testes.
UDT is the most common congenital anomaly affecting boys. Three percent of newborns have an undescended testis, but most subsequently descend within the first few months of life, resulting in a prevalence of approximately 0.8 %.
Prevalence at Birth and Natural History
Of term males, 1.5–3 % have UDT.
Presumably stimulated by the postnatal testosterone surge 50 % or more will descend by 3 months, with greater likelihood for descent in bilateral versus unilateral cases.
Scorer reported observations in 3,222 term males, noting 90 (3 %) had UDT. Descent was specifically defined as mid-testicular position greater than 4 cm from the superior border of the pubic bone with downward traction on the testicle. Of these 90, 45 spontaneously descended during the first month of life into the dependent scrotum 7–8 cm from the pubic bone, and another 22 descended between 6 and 12 weeks of life to 5–6 cm from the pubic bone. The others remained undescended (i.e., <4 cm below the pubic bone), comprising 0.7 % of the total study group (Scorer 1964).
A report from 10,000 consecutive army recruits in the 1940s stated 80 (0.8 %) either had prior surgery for UDT or had one on physical examination (Baumrucker 1946).
A prospective study of 7,032 consecutive males examined at birth and again at 3 months using the same measurements as Scorer reported a total of 270 (3.8 %) had UDT, 179 unilateral and 91 bilateral cases. At 3 months, 59 % of unilateral and 72.5 % of bilateral UDT had descended into the dependent scrotum, p = 0.0004, leaving a 1.4 % prevalence of UDT. The authors were uncertain why their rates were higher than those of Scorer earlier, but believed they indicated a true increased prevalence of UDT (John Radcliffe Hospital Cryptorchidism Study Group 1992).
However, another prospective study involving 6,360 term males also using Scorer examinations did not find this apparent increased prevalence, but instead reported very similar results as had Scorer, with 2.2 % of newborns and 0.9 % of 3-month-old males having UDT (Berkowitz et al. 1993).
Finally, another prospective trial examined 6,246 newborn males >34 weeks gestation using Scorer methodology, reporting 95 (1.5 %) had UDT, unilateral in 83 (87 %) and bilateral in 12 (13 %). Repeat examination at 3 months found descent to have occurred in 44 %, leaving unilateral UDT in 94 % and bilateral UDT in 6 %, p = 0.03; four considered to descend by 3 months were noted to be reascended at 12 months (Wagner-Mahler et al. 2011).
UDT Prevalence
Unilateral Versus Bilateral
Bilateral UDT occurs in <20 % of cases.
The prospective study of 7,032 consecutive males described above (John Radcliffe Hospital Cryptorchidism Study Group) reported 99 testes remained undescended at 3 months of age, of which 83 (84 %) were unilateral and 16 (16 %) were bilateral.
Similarly, the prospective trial of 6,246 males reported 52 cases with persistent UDT at 3 months of age, unilateral in 94 % and bilateral in 6 % (Wagner-Mahler et al. 2011).
Prospective evaluation of boys referred to surgical specialists for nonscrotal testis reported UDT were unilateral in 90 % and bilateral in 10 % (Snodgrass et al. 2011).
Palpable Versus Nonpalpable
Approximately 75 % of UDT are palpable. Of the remaining nonpalpable testes, the condition is unilateral in 90 % and bilateral in 10 %.
Retrospective review of a clinical series of 1,866 patients operated for UDT reported 447 (24 %) had a nonpalpable testis, unilateral in 89 % and bilateral in 11 % (Kirsch et al. 1998).
Location of the Undescended Testis
Palpable
Most palpable testes are below the external ring, while a minority are between the internal and external rings in the inguinal canal.
A retrospective analysis reported surgical location of 488 palpable UDT: 324 (66 %) were distal to the external ring while 164 (34 %) were canalicular (Cendron et al. 1993).
In a surgical series of 120 consecutive palpable UDT, only 12 (10 %) were within the inguinal canal, while all others were in various positions below the external ring (Bianchi and Squire 1989).
Differences in these two reports likely relate to the surgical approach used to expose the testis. Manipulation of the cord structures through an inguinal incision may pull a testis proximally through the external ring, whereas dissection from below in the scrotum could move a testis distally through the external ring.
Unilateral Nonpalpable
Of unilateral nonpalpable testes (comprising 90 % of cases with nonpalpable testes), prenatal testicular loss has occurred in two-thirds. Nearly all of these are represented by a scrotal nubbin.
Of the other third having a viable testis, approximately half are located in the abdomen and the other half are extra-abdominal within the inguinal canal.
Although nonpalpable testes found to be nubbins traditionally have been included in series of UDT, the underlying pathophysiology is different in these cases, as they are presumed to represent intrauterine torsion or other vascular compromise of the testis before or during descent.
Combining two prospective series of consecutive boys with unilateral nonpalpable testes, a total of 83 nonpalpable testes were evaluated. Of these, 53 (64 %) had evidence of prenatal testicular loss, with scrotal nubbins (n = 48), canalicular nubbins (n = 2), or intra-abdominal vanished testis without extra-abdominal nubbin (n = 3). The other 30 (36 %) had a viable testis that was extra-abdominal (despite examination under anesthesia) in 11 (13 %), and intra-abdominal in 19 (23 %) (Snodgrass et al. 2004, 2007).
One-hundred four consecutive males with nonpalpable testes, unilateral in 102 and bilateral in 2, underwent laparoscopy. Testicular loss was diagnosed in 63/104 (60.5 %), an intra-abdominal testis in 23 (22 %), and an inguinal testis in 18 (17 %) (Diamond and Caldamone 1992).
A prospective observational study included 75 patients with unilateral nonpalpable testes who underwent initial laparoscopy, with final diagnosis of testicular loss in 44 (59 %), intra-abdominal testis in 13 (17 %), and extra-abdominal testis in 18 (24 %) (Moore et al. 1994).
Bilateral Nonpalpable
Bilateral nonpalpable testes are most often both viable, with approximately half located intra-abdominally and half extra-abdominally.
Anorchia is found in 5–25 % of patients.
The only prospective study regarding nonpalpable testes that distinguishes unilateral from bilateral cases reported findings in 44 bilateral nonpalpable testes in 22 patients. A viable testis was found in 40/44 testes (91 %), equally likely in the abdomen (20, 48 %) or inguinal canal (19, 45 %). The others sustained prenatal loss. The difference in findings in unilateral (mentioned above) versus bilateral cases was statistically significant (Moore et al. 1994).
Reported findings from surgical series for non-intersex patients with bilateral nonpalpable testes are potentially influenced by preoperative hormonal assessment, which can obviate need for surgical exploration. Anorchia was diagnosed in 5 and 25 % of cases in two series of consecutive patients (Moore et al. 1994; Tennenbaum et al. 1994).
Diagnosis
History and Physical Examination
A positive birth history for UDT greatly increases the likelihood that a boy referred for evaluation has UDT rather than a retractile testis.
Since most UDT are unilateral, visual inspection should precede palpation to detect scrotal asymmetry.
Assessment of the prepubertal boy with unilateral nonpalpable testis should include measurement of the contralateral descended testis for compensatory hypertrophy, which correlates with prenatal testicular loss. Testis length ≥1.8 cm measured with a ruler has a positive predictive value of 90 % that the nonpalpable testis is not viable.
A prospective study of 118 consecutive referrals reported only 50 % had UDT. Boys younger than 1 year of age and those older than 10 years old in puberty were more likely to have a correct diagnosis by PCPs, versus those 1–10 years of age, who were more likely to have retractile testes. UDT was predicted by the following:
-
A positive birth history for UDT, OR 21.4 (95 % CI 3.8–120.8).
-
Scrotal asymmetry (visual inspection before palpation), OR 121.3 (95 % CI 14.3 to >999).
Only 6 % of referred boys with a negative birth history and visual scrotal symmetry had UDT (Snodgrass et al. 2011).
In patients 7 months to 11 years with unilateral nonpalpable testis, a scrotal testis measuring 1.8 cm or greater in length positively predicts monorchidism in nearly 90 % of cases. One study of 60 boys with unilateral nonpalpable testis reported 14/15 1.8 to 2 cm and 14/16 > 2 cm had monorchidism (Hurwitz and Kaptein 2001).
Another prospective study of boys median age 23 months found 26/30 (87 %) had monorchidism for scrotal testis ≥1.8 cm, versus 8/10 (80 %) having a viable testis when the scrotal testis was <1.8 cm (Snodgrass et al. 2007).
Both performed office measurements using rulers, which may differ from ultrasound measurements of testicular length. There are no published data regarding ultrasound-determined compensatory hypertrophy.
UDT Versus Retractile Testis
Orchiopexy rates are approximately two times the prevalence of UDT.
A regional policy was adopted in a British health trust stating that boys in whom there was any doubt as to normal scrotal position of both testes at 8 months of age were to be referred to surgical specialists for evaluation. When this policy was implemented, the number of orchiopexies decreased by 50 %, with most reduction occurring in school-age boys, when testicular retraction is most common (Brown et al. 2004).
A review of a New York Department of Health database for the years 1984–2002 considered orchiopexy rates determined by the number of operations versus live male births. While surgical rates were stable throughout the study period, the average of 1.4 % operations consistently exceeded the expected 0.8 % prevalence of UDT (Capello et al. 2006).
The John Radcliffe Hospital Cryptorchidism Study Group calculated the orchiopexy rate from the earlier Scorer report and noted surgery was done twice as often as the UDT rate (1.9 % vs. 0.9 %). Their own evaluation of newborns and infants using Scorer’s technique found a higher rate of UDT of 1.4 %, but their orchiopexy rate was also higher, at 2.9 % (John Radcliffe Hospital Cryptorchidism Study Group 1960).
Ascending Testes
Secondary ascent of a previously normally descended testis has been proposed to explain higher orchiopexy rates than UDT prevalence.
One prospective study using trained nurses reported testicular ascent in 4 % at 12 months of age. Another prospective study with a single pediatrician performing all examinations reported no testicular ascent at 12 months.
Two studies reported ascending testes were bilateral in over 30 % of cases, versus UDT, which is bilateral in <20 % (see above).
Spontaneous re-descent of ascended testes by mid-puberty was reported by two studies in approximately 60 % of cases.
A prospective study performed by five “trained research nurses” within the Cambridge Baby Growth Study involved longitudinal examinations in newborn males for testicular position. UDT were noted in 6 % at birth, declining to 2 % at age 3 months, but rising to 6.7 % at 12 months from 4 % ascending. Continued exams showed additional new cases of ascending testes, which by 24 months reached 7 % (Acerini et al. 2009).
However, another prospective study involving 6,246 newborns >34 weeks gestation, with examinations by the same pediatrician at birth, 3, and 12 months using Scorer methodology, assigned two controls to each case with UDT. None of 170 controls developed an ascended testis at 12 months (Wagner-Mahler et al. 2011).
Based on a policy of not operating on boys presenting with possible UDT if a normal newborn examination was documented, two studies prospectively evaluated patients diagnosed with ascending testes observed without surgery into puberty.
One reported findings in 557 consecutive patients referred for possible UDT at mean age of 7.4 years (0.3–16.5). Of these, 415 (479 testes) were considered from examination to have UDT, congenital in 116 (129 testes) and acquired (ascending) in 299 (350 testes); 108/350 (31 %) ascended testes were bilateral. There was completed follow-up in 139 patients (164 testes), with spontaneous descent in 98 (60 %) testes; 70 at Tanner stage G2, 26 at Tanner G3-4, and 2 at Tanner 5. Another 32 testes were confirmed to be undescended at ≥Tanner G3 and underwent surgery, while 14 were lost to follow-up and 21 had surgery elsewhere (Sijstermans et al. 2006).
A similar study followed 107 boys (133 testes) with ascended testes. Of these testes, bilateral involvement was diagnosed in 50 (38 %); 75 (57 %) of the testes descended; 3 before puberty, 40 at G2, and 32 at G3-4 (Eijsbouts et al. 2007).
Imaging
Genital US is sometimes used by PCPs to confirm suspicions of UDT before referral to surgical specialists, even though the test does not reliably distinguish between UDT and retractile testes.
Meta-analysis of US for nonpalpable testes reported detection in 97 % extra-abdominal versus 38 % intra-abdominal testes.
MRI was reported by three studies as having 60–85 % accuracy for nonpalpable UDT, with false-negative rates of 8 and 14 %.
Ultrasound
Meta-analysis of 12 studies involving 591 testes reported sensitivity/specificity for US to locate a nonpalpable testis to be 45 % (95 % CI 29–61) and 78 % (95 % CI 43–94), respectively. US detected 97 % of extra-abdominal and 38 % of intra-abdominal viable testes (Tasian and Copp 2011).
Thirty of 118 (25 %) consecutive boys referred in one prospective study had scrotal US ordered by their primary care physician; nonscrotal testes was reported in 29. Physical exam found 15 patients had UDT, while 14 had descended testes (Snodgrass et al. 2011).
MRI for Nonpalpable Testis
MRI was used preoperatively in the evaluation of 47 nonpalpable testes in boys ages 1–12 years, and found to be accurate in 39 (85 %), with a false-negative rate of 4/28 (14 %) and false-positive rate of 4/19 (21 %). All false positives were lymph nodes, and all false-negative testes were found in the inguinal canal at operation. The 24 MRI-identified testes were found “in the inguinal canal or just proximal to the internal ring” (n = 19), in the abdomen (n = 2), or in the scrotum (n = 3) (Kanemoto et al. 2005).
MRI and diffusion-weighted MRI were performed in 36 boys and 38 testes, in which laparoscopy found 19 extra-abdominal, 11 low, and 4 high intra-abdominal testes (<3 cm vs. >3 cm from internal ring), and 4 nubbins. Results were presented from two radiologists, with the combination of the two methods giving overall accuracy in 92 and 86 %. Considering the observer with 92 % accuracy, there were no false positives and 3 (8 %) false-negative assessments, which were not further explained except that one was an intra-abdominal “atrophic” testis (Kantarci et al. 2010).
In a retrospective study in 26 boys with 29 nonpalpable testes, MRI correctly identified 10/12 intra-abdominal testes, 4/6 canalicular testes, 4/10 nubbins, and 0/1 scrotal testis, for an overall accuracy of 62 % (Desireddi et al. 2008).
Diagnosis of Anorchia
Basal LH and FSH levels >3× normal are considered diagnostic for anorchia.
MIS was reported in one study to have 92 %/98 % sensitivity/specificity for anorchia.
Twenty-eight prepubertal boys <11 years of age with bilateral nonpalpable testes had hCG therapy (3,000 u/m2 BSA injection daily for 5 days, then 2× weekly for 5 weeks); 21 had an “adequate” rise in testosterone, and all had viable testes at exploration, versus 7 with no rise in testosterone, of which 6 had surgery, with none having a viable testis. Six of seven with no testosterone response had baseline LH and FSH >3× normal (Jarow et al. 1986).
Nine patients ranging from 10 months to >12 years with surgically confirmed anorchia had endocrine evaluation preoperatively, including LHRH stimulation in five and hCG stimulation in seven using varied protocols. There was no testosterone response to stimulation. FSH was ≥3× normal in 5/9 (56 %), with variation based on age (Lustig et al. 1987).
One series of 107 consecutive patients with nonpalpable testes reported none of 12 with bilateral nonpalpable testes met their criteria of elevated baseline gonadotrophin levels with negative hCG stimulation testing, although 3 were confirmed surgically to have anorchism (Tennenbaum et al. 1994).
One report compared assays for testosterone secretion versus MIS in 17 boys with anorchia. Diagnostic sensitivity and specificity for MIS was 92 and 98 %, versus 69 and 83 % for testosterone. Mean serum concentration of MIS was 0.8 ± 0.6 ng/mL in boys with anorchia, which was significantly less than the concentration of 48.2 ± 42.1 ng/mL in boys with testes (Lee et al. 1997).
Management
Hormonal Monotherapy
Hormone monotherapy results in complete testicular descent in ≤14 % of UDT.
A meta-analysis was performed using Cochrane Collaboration methodology to determine efficacy of hormonal therapy for UDT:
-
Intramuscular hCG versus intranasal GnRH: Data from two RCTs comprising 201 patients reported complete testicular descent was 25 % versus 18 %, absolute risk reduction 7 % (95 % CI 0.012–0.170).
-
Intranasal LHRH versus placebo: Nine RCTs with 1,049 boys reported complete testicular descent in 19 % versus 5 %, OR 3.59 (95 % CI 2.52–5.12).
Age of patients at treatment was not stated (Henna et al. 2004).
Adjunctive Hormonal Therapy
One RCT reported that preoperative intranasal GNRH improved the fertility index over orchiopexy alone.
A RCT randomized 42 boys (63 inguinal testes, 21 unilateral and 21 bilateral UDT) with mean age 33.5 months (11–100) to 1.2 mg/day intranasal GNRH for 4 weeks then orchiopexy versus orchiopexy alone. Intraoperative testis biopsies were obtained from UDT, with fertility index calculated by counting the number of adult spermatagonia per tubule in at least 80 tubules. Treated patients had a significantly higher mean fertility index of 1.05 ± 0.71 (0.27–3.33) spermatagonia/tubule versus nontreated with 0.51 ± 0.39 (0–1.17), p = 0.007. Considering only the 21 with bilateral UDT, the 9 treated had a mean fertility index of 0.96 ± 0.47 versus 12 untreated with 0.56 ± 0.38 (0–1.12), p = 0.005 (Schwentner et al. 2005).
The possibility that hormonal therapy may harm the testis has been proposed. One retrospective study involved patients managed for UDT over a 5-year period, 1985–1990, during which time 19 were given intranasal GHRH then orchiopexy; 8, IM hCG and orchiopexy; and 45, operated without preoperative hormones. Median fertility indexes were 0.07 (0–0.31), 0.06 (0.0025–0.21) and 0.14 (0–0.86), reported as a significant difference between hormonally treated versus only surgery groups. However, the numbers of patients lacking any germ cells was the same in all groups (Cortes et al. 2000). Reasons for hormonal stimulation in some patients and not in others were not stated, nor was the time at which surgery was done after stimulation.
An analysis of testis biopsies taken from the UDT and the descended scrotal testis in 73 patients compared apoptosis of spermatagonia in 43 with preoperative hCG (2 injections/week × 2 weeks, dose per injection: 250 IU if <12 months of age, 500 IU for 1–7 years of age, 1,000 IU if >7 years of age) versus 30 without injection. Effects of hCG were considered for three treated groups, those operated <1 month, at 1–3 months, and at 3–14 months after last injection. Apoptosis was increased in both the scrotal and UDT in treated patients at <1 months, but was similar to untreated patients by >1 month (Heiskanen et al. 1996).
Orchiopexy Timing
Orchiopexy is recommended between ages 6 and 12 months.
One RCT reported UDT had volume less than 50 % of descended testes at 6 months of age, with subsequent growth in those operated versus those not operated.
Current recommendations for surgery between 6 and 12 months are based on the observation that spontaneous descent that occurs after birth does so before 6 months, while decrease in germ cell counts can be diagnosed by 1 year of age (AAP 1996).
A RCT randomized boys with unilateral palpable UDT to orchiopexy at age 9 months versus 3 years, following them with periodic US performed at age <1, 6, 12, and 24 months. From birth to 6 months, scrotal testes increased in volume by 89 % without further increase through age 2 years. UDT also grew from birth through 6 months, but by a significantly less 50 %. Initial and 6-month US demonstrated significantly less volume in UDT versus scrotal testes (median volume at 6 months UDT 0.36 mL vs. scrotal 0.53 mL, p < 0.001). However, further significant growth of the operated UDT was observed by 2 years (0.36–0.47 mL, p < 0.001); this was not seen in the non-operated UDT (Kollin et al. 2007).
Palpable Testes
Traditional orchiopexy includes an inguinal incision to mobilize the testis and ligate an associated patent processus vaginalis and a separate scrotal incision for testis placement.
Observations that up to 90 % of palpable testes have exited the external ring support single-incision orchiopexy through the scrotum as an alternative. Additional inguinal incision to obtain greater spermatic cord length is reported in 0–4 % of cases.
Single upper scrotal incision was used in 104 consecutive boys aged 2–12 years with 120 palpable UDT. Scrotal orchiopexy resulted in a mid- to lower scrotal position in 111 testes, and a testis in the mid- to upper scrotum in 4. The other 5 required an additional inguinal incision to gain sufficient vascular length for orchiopexy. All testes were described as viable, without specific mention of atrophy with follow-up at 6 months to 3 years (mean not stated) (Bianchi and Squire 1989).
A prospective study analyzed single scrotal incision orchiopexy in 114 consecutive patients with 148 palpable UDT, accomplished in all cases without need for additional inguinal incision. With mean follow-up of 10 months (3–22), all were described as palpable within the scrotum, without specific mention of either atrophy or low versus high scrotal position (Callewaert et al. 2010).
A RCT assigned 292 children mean age 40 ±10 months with 398 palpable UDT to either scrotal or inguinal orchiopexy between 2007 and 2010. Surgical success at 12 months was defined as “intrascrotal testis.” With follow-up in 107 children (146 testes) after scrotal orchiopexy and 105 children (141 testes) after inguinal orchiopexy, there was no difference in overall success: 135/146 (92 %) versus 136/141 (96 %). Nine of 201 (4 %) scrotal orchiopexies additionally required inguinal incision (Na et al. 2011).
Nonpalpable Testes
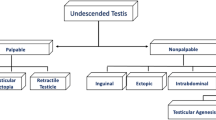
Since exploration for nonpalpable testes can find nubbins, extra-abdominal viable testes, or intra-abdominal viable testes, several management options are available, and approach can be tailored by likely findings in specific cases (Fig. 5.1 ):
-
1.
Unilateral nonpalpable testes with a contralateral scrotal testis measuring ≥1.8 cm have a 90 % probability of prenatal testis loss, with a nubbin found in the scrotum in nearly all cases. Therefore, a scrotal incision can be made initially, reserving laparoscopy for the few without a nubbin (or testis) in the scrotum or inguinal canal (Fig. 5.2 ).
Fig. 5.2 As discussed above, testicular length ≥1.8 cm in the contralateral descended testis has a 90 % predictive value that prenatal testicular loss has occurred. Patients with nubbins had contralateral testicular length a mean of 2.0 ± 0.56 cm, which was significantly longer than those with a viable testis, whose contralateral testicular length was 1.69 ± 0.09 cm (Hurwitz and Kaptein 2001; Snodgrass et al. 2007).
A prospective observational study in which consecutive patients with unilateral nonpalpable UDT underwent scrotal exploration first followed by laparoscopy reported testicular absence in 23 boys having a scrotal nubbin in 22 and blind ending vas and vessels at the internal ring without a nubbin in the other. Of the 22 scrotal nubbins, six had blind ending vas and vessels at or above the internal ring at laparoscopy, indicating that this finding more often represents the proximal extension of torsion after the testis reaches the scrotum rather than an intra-abdominal event (Snodgrass et al. 2004).
-
2.
Unilateral nonpalpable testes with a contralateral scrotal testis measuring <1.8 cm most often have a viable testis with an equal likelihood to be found extra- versus intra-abdominally.
Preoperative ultrasound can detect the extra-abdominal testes, which are then approached either by inguinal or scrotal incision, as with palpable testes. Without preoperative imaging, scrotal or inguinal incision versus laparoscopy is an option.
Bilateral nonpalpable testes most often are found to have two viable testes. Preoperative ultrasound can be used to detect those that are extra-abdominal, or inguinal incision versus laparoscopy can be done.
Inguinal incision provides exposure to identify scrotal nubbins and extra-abdominal testes, and after opening the internal ring and peritoneum allows intra-abdominal inspection and orchiopexy. A retrospective series of 447 nonpalpable testes reported 181 (40 %) were nubbins or vanished, 175 (40 %) were extra-abdominal, and only 91 (20 %) intra-abdominal. All were managed inguinally, with 33 standard, 38 one-stage Fowler-Stephens, and 4 two-stage orchiopexies. Postoperative follow-up in 76 of the 91 intra-abdominal cases found 55 (72 %) described as having a “good sized” testis in the mid- to low scrotum versus 9 (12 %) in the upper scrotum and another 12 (16 %) with atrophy, including 26 % of those with Fowler-Stephens orchiopexy (Kirsch et al. 1998).
A prospective analysis of initial laparoscopy in 104 boys with 126 nonpalpable testes reported only 33 (26 %) intra-abdominal testes and 8 (5 %) blind ending vas and vessels. Others had vas and vessels exiting the internal ring associated with a patent processus vaginalis in 26 of 75 cases, comprising 19/38 (50 %) with an extra-abdominal testis (meaning the others had a closed internal ring with an extra-abdominal testis) and 7/37 (19 %) with an extra-abdominal nubbin. In 75 cases, there were vas and vessels exiting the internal ring, leading to an extra-abdominal testis in 38. The authors stated that “in most cases” those without a viable extra-abdominal testis had “attenuated” vas and vessels (Moore et al. 1994).
Retrospective review was done for results of laparoscopy in 111 boys with 124 nonpalpable testes, reporting that status of the internal ring correlated with findings of viable testis versus nubbin in those without an intra-abdominal testis. In this series, there were 38 intra-abdominal testes, 7 extra-abdominal testes, and 77 absent/vanished testes. Six extra-abdominal testes had a widely patent processus vaginalis that allowed them to be manipulated back into the abdomen for laparoscopic orchiopexy, whereas in one, “no hernia was visualized” but at inguinal exploration a viable testis with “a small patent processus vaginalis” was encountered (Elder 1994).
From these data, if neither an intra-abdominal testis nor blind ending vas and vessels were found on laparoscopy, extra-abdominal exploration would be mandated, since neither examination under anesthesia nor presence or absence of a patent processus vaginalis (open vs. closed internal ring) predicted whether or not a testis would be found. The possible exception would be those with “attenuated” vessels who might not need further extra-abdominal exploration, but our review did not find objective criteria for this determination.
No RCT evaluates inguinal exploration versus laparoscopy. The primary disadvantage of laparoscopy arises when neither a testis nor blind ending structures are encountered, as extra-abdominal exploration is still needed. Considering all patients undergoing initial laparoscopy in the prospective trial by Moore et al., only 32.5 % had either an intra-abdominal testis or blind ending vas and vessels, meaning the remainder needed extra-abdominal assessment. Whether or not a hernia sac extended through the internal ring did not predict whether an extra-abdominal viable testis or nubbin would be found, as 50 % of the testes had a closed internal ring, while 20 % of the nubbins had an open sac (Moore et al. 1994).
Extra-abdominal exploration after laparoscopy traditionally is done using an inguinal incision, followed by a scrotal incision if a testis is found. Alternatively, a scrotal incision can be used to remove a nubbin or to perform orchiopexy, without an inguinal incision.
Intra-abdominal Orchiopexy
Best management when there is insufficient vascular length to deliver the intra-abdominal testis into the scrotum—staged ochiopexy preserving the spermatic cord vessels versus one- or two-stage Fowler-Stephens orchiopexy—cannot be determined from available data.
A summary of reported orchiopexies included 248 intra-abdominal testes treated with two-stage orchiopexy preserving the spermatic cord vessels, of which 73 % were considered by the various authors to be successful. Success for one-stage Fowler-Stephens orchiopexy was reported as 63 % versus success for two-stage Fowler-Stephens of 77 %. This difference was not considered statistically significant (Docimo 1995).
To date no RCT compares one-stage versus two-stage orchiopexy with spermatic cord division.
No data were found regarding simultaneous bilateral one- or two-stage Fowler-Stephens orchiopexy.
Outcomes
Surgical Success
Surgical success is usually defined as “scrotal position without atrophy,” with few articles reporting actual scrotal position (high, mid, low) or objective measurement of testicular size.
One review of series published before 1995 reported surgical success of 89 % for extra-abdominal and 74.5 % for intra-abdominal testes. Fowler-Stephens orchiopexy success was 67 %, while staged orchiopexy without vessel division was 72.5 %.
No RCT compares intra-abdominal orchiopexy with versus without vessel division, or one-stage versus two-stage Fowler-Stephens procedures.
Review of published literature identified 64 articles with 8,425 UDT with data that could be evaluated to determine surgical success, defined as “scrotal position and absence of atrophy.” Of patients with postoperative evaluations ≥6 months, 420/564 (74.5 %) intra-abdominal testes and 1,000/1,126 (89 %) extra-abdominal testes had surgical success. Fowler-Stephens orchiopexy had overall surgical success in 214/321(67 %), with no difference reportedly found in staged (43/56 [77 %]) versus single-stage (data not shown) procedures. Two-stage orchiopexy without vessel division had surgical success in 180/248 (72.5 %) (Docimo 1995).
The RCT by Na et al. described above comparing inguinal versus scrotal orchiopexy for palpable UDT reported success as an intrascrotal testis achieved in 271/287 (94 %) testes, with no difference by technique used.
Meta-analysis compared open versus laparoscopic abdominal orchiopexy using data obtained from two RCTs and five case series totaling 263 and 176 cases, reporting no differences in:
-
Testicular retraction, OR 0.6 (95 % CI 0.13–2.72).
-
Viable testis, OR 1.61 (95 % CI 0.30–8.52).
-
Testicular atrophy, OR 1.70 (95 % CI 0.49–5.98) (Guo et al. 2011).
A systematic review was done comparing single- versus two-stage Fowler-Stephens orchiopexy, with nine articles for single-stage, 36 for two-stage, and 16 including both. Pooled estimated success rates were 80 % (95 % CI 75–86) for single-stage versus 85 % (95 % CI 81–90) for two-stage orchiopexy, with no differences as to whether orchiopexy was laparoscopic or open. Despite the apparent increased success for two-stage orchiopexy, quality of the data from which the observations were made was low (Elyas et al. 2010).
Cosmetic Results
One study reported parents equally satisfied with cosmetic results of inguinal versus scrotal orchiopexy.
The RCT by Na et al. described above comparing inguinal versus scrotal orchiopexy included a parent questionnaire with response options of “satisfied,” “not fully satisfied,” or “not satisfied” (questionnaire not shown) regarding cosmetic results. No parent was “not satisfied,” and only 3 % were “not fully satisfied,” with no difference in response based on surgical procedure.
Reoperative Orchiopexy
Two retrospective studies reported outcomes of reoperative orchiopexy via scrotal incision for testicular retraction after prior orchiopexy or hernia repair. Only one (3 %) boy had second testicular retraction, and there was no atrophy.
A retrospective review of operated patients from 2005 to 2009 reported 17/687 (2.5 %) UDT reascended after orchiopexy, of which eight found distal to the external ring were included for study. In another two cases, a testis ascended following inguinal hernia/hydrocele repairs. Three additional patients failed orchiopexy elsewhere, and three had ascent of a testis after hernia surgery elsewhere, giving a total of 16 reoperative orchiopexies all for testes distal to the external ring and approached by scrotal incision. One required additional inguinal incision and “wide preperitoneal” dissection to gain adequate cord length. At mean follow-up of 12 months (3–36), all were reported to have normal scrotal position and no atrophy on physical exam (Karaman et al. 2010).
Retrospective review reported 24 patients mean age 6 years (1–16) undergoing 27 orchiopexies after prior hernia (n = 13) or orchiopexy (n = 6). Scrotal incision was used if it “could be manipulated near or over the testis,” comprising 24/27 (89 %). At mean follow-up of 12 months in 20 of the 21 patients with scrotal surgery, one testis was high and none were atrophic (Dudley et al. 2011).
One retrospective study reported outcomes in 32 reoperations for UDT (15 high scrotum, eight at external ring, and nine in the inguinal canal). Two inguinal testicles were only able to be brought down into the high scrotum, and one patient underwent orchidectomy. Overall, after a mean follow-up period of four (1–7) years following the second operation, 29 (93.5 %) testes were scrotal without evidence of atrophy (Ziylan et al. 2004).
Another retrospective study reported outcomes in 35 patients with recurrent UDT after failed inguinal orchiopexy. Ten inguinal testes were treated directly with open inguinal redo orchidopexy. Laparoscopy-assisted orchiopexy was attempted in the remaining 25 based on an impalpable testis or need for additional vascular length. In two (8 %) of these cases, scarring was present between the cord and the inguinal canal, impeding the laparoscopy approach. After a mean follow-up of 22 months (6–32), all 33 testicles were within the scrotum. Atrophy (not defined) was reported in four (11 %) patients (two with laparoscopy, two after the inguinal procedure) (Tong et al. 2009).
Cancer Risk
The overall risk that a previously operated UDT will develop a germ cell tumor is less than 0.5 %.
Nonoperated UDT are more likely to develop seminoma, whereas tumors developing after orchiopexy are more likely nonseminomas.
It is unclear if orchiopexy performed before puberty is protective against cancer development.
There is a theoretic risk for cancer to develop in nubbins, since germ cells are found in ≤10 %, but no case has been reported.
The overall risk for a germ cell tumor associated with UDT was characterized by a study of 16,983 men surgically treated for UDT and then followed for a mean of 12 ± 7 years (209,984 man-years), during which time only 56 (0.3 %) developed a germ cell tumor (Pettersson et al. 2007).
Meta-analysis of seven reported series found seminomas developed in 74 % of 121 nonoperated UDTs that developed germ cell tumors versus 37 % of 247 previously UDTs repositioned into the scrotum that developed tumors; the others were nonseminomas (Wood and Elder 2009).
Two studies conclude orchiopexy performed before puberty is protective against tumor development:
-
In 56 cases of testis cancer in former UDTs, the relative risk was 2.23 (95 % CI: 1.58–3.06) when surgery was performed before age 13 years, versus 5.40 (95 % CI: 3.20–8.53) when surgery was done after 13 years. Sixty-nine patients had to undergo orchiopexy before age 13 to prevent one malignancy between ages 13 and 55 years (Pettersson et al. 2007).
-
The other report was a meta-analysis of five studies with 80 germ cell malignancies associated with UDTs. Although the authors stated prepubertal orchiopexy was protective, their finding that surgery after approximately age 11 years was three times more likely to be associated with cancer than when surgery was performed earlier was not statistically significant (OR 3.4 95 % CI 0.7–17.7) (Walsh et al. 2007).
Nubbins are found to have germ cell elements in <10 % of cases. A single case found intratubular germ cell neoplasia (Rozanski et al. 1996), but no overt malignancies have been reported arising from a nubbin.
Fertility
Paternity rates for men with previously operated unilateral UDT are considered similar to those of men born with normal testes.
Paternity rates in those with formerly bilateral UDTs are less than in normal men.
Two articles report successful sperm retrieval in >60 % men with prior UDT, similar in one to infertile men without prior UDT.
Paternity data was obtained in 40 men who underwent orchiopexy with testis biopsy between 1950 and 1960. Of 20 men with prior unilateral orchiopexy who attempted to have children, 87 % reported success, versus 33 % of nine men with prior bilateral orchiopexy. Sperm counts were obtained in 16 men, with 75 % having <20 × 106 sperm; findings did not predict reported paternity (Cendron et al. 1989).
Questionnaires were distributed to patients (numbers not stated) undergoing orchiopexy or other minor surgery (controls) between 1955 and 1969 at Children’s Hospital of Pittsburg, reporting responses from 363 men with former UDTs (313 unilateral and 50 bilateral) and 336 controls. There was no difference in paternity reported by patients formerly with unilateral UDT versus controls (90.2 and 93.1 %, respectively), but there was significantly less paternity after bilateral orchiopexy (64.5 %) (Lee et al. 1995).
Several publications emphasize histological appearance of seminiferous tubules obtained by biopsy during orchiopexy. While a detailed discussion of potential fertility is beyond the scope of this review, it may be noteworthy that two recent reports concern sperm retrieval in men previously undergoing orchiopexy, with successful results in over 60 % of cases despite azoospermia on semen specimens (Wiser et al. 2009); (Haimov-Kochman et al. 2010). Prior orchiopexy at age <10 years versus later did not impact results (Wiser et al. 2009). Success in men after orchiopexy was the same as in other men undergoing sperm retrieval without a history of UDT (Haimov-Kochman et al. 2010).
References
AAP. Timing of elective surgery on the genitalia of male children with particular reference to the risks, benefits, and psychological effects of surgery and anesthesia. Pediatrics. 1996;97(4):590–4.
Acerini CL, Miles HL, Dunger DB, Ong KK, Hughes IA. The descriptive epidemiology of congenital and acquired cryptorchidism in a UK infant cohort. Arch Dis Child. 2009;94(11):868–72.
Baumrucker GO. Incidence of testicular pathology. Bull U S Army Med Dep. 1946;5:312–4.
Berkowitz GS, Lapinski RH, Dolgin SE, Gazella JG, Bodian CA, Holzman IR. Prevalence and natural history of cryptorchidism. Pediatrics. 1993;92(1):44–9.
Bianchi A, Squire BR. Transscrotal orchidopexy: orchidopexy revised. Pediatr Surg Int. 1989;4:189–92.
Brown JJ, Wacogne I, Fleckney S, Jones L, Ni Bhrolchain C. Achieving early surgery for undescended testes: quality improvement through a multifaceted approach to guideline implementation. Child Care Health Dev. 2004;30(2):97–102.
Callewaert PR, Rahnama’i MS, Biallosterski BT, van Kerrebroeck PE. Scrotal approach to both palpable and impalpable undescended testes: should it become our first choice? Urology. 2010;76(1):73–6.
Capello SA, Giorgi Jr LJ, Kogan BA. Orchiopexy practice patterns in New York State from 1984 to 2002. J Urol. 2006;176(3):1180–3.
Cendron M, Keating MA, Huff DS, Koop CE, Snyder 3rd HM, Duckett JW. Cryptorchidism, orchiopexy and infertility: a critical long-term retrospective analysis. J Urol. 1989;142(2 Pt 2):559–62. discussion 72.
Cendron M, Huff DS, Keating MA, Snyder 3rd HM, Duckett JW. Anatomical, morphological and volumetric analysis: a review of 759 cases of testicular maldescent. J Urol. 1993;149(3):570–3.
Cortes D, Thorup J, Visfeldt J. Hormonal treatment may harm the germ cells in 1 to 3-year-old boys with cryptorchidism. J Urol. 2000;163(4):1290–2.
John Radcliffe Hospital Cryptorchidism Study Group. Cryptorchidism: a prospective study of 7500 consecutive male births, 1984–8. Arch Dis Child. 1992;67(7):892–9.
Desireddi NV, Liu DB, Maizels M, Rigsby C, Casey JT, Cheng EY. Magnetic resonance arteriography/venography is not accurate to structure management of the impalpable testis. J Urol. 2008;180(4 Suppl):1805–8. discussion 8–9.
Diamond DA, Caldamone AA. The value of laparoscopy for 106 impalpable testes relative to clinical presentation. J Urol. 1992;148(2 Pt 2):632–4.
Docimo SG. The results of surgical therapy for cryptorchidism: a literature review and analysis. J Urol. 1995;154(3):1148–52.
Dudley AG, Sweeney DD, Docimo SG. Orchiopexy after prior inguinal surgery: a distal approach. J Urol. 2011;185(6):2340–3.
Eijsbouts SW, de Muinck Keizer-Schrama SM, Hazebroek FW. Further evidence for spontaneous descent of acquired undescended testes. J Urol. 2007;178(4 Pt 2):1726–9.
Elder JS. Laparoscopy for impalpable testes: significance of the patent processus vaginalis. J Urol. 1994;152(2 Pt 2):776–8.
Elyas R, Guerra LA, Pike J, DeCarli C, Betolli M, Bass J, et al. Is staging beneficial for Fowler-Stephens orchiopexy? A systematic review. J Urol. 2010;183(5): 2012–8.
Guo J, Liang Z, Zhang H, Yang C, Pu J, Mei H, et al. Laparoscopic versus open orchiopexy for non-palpable undescended testes in children: a systemic review and meta-analysis. Pediatr Surg Int. 2011;27(9):943–52.
Heiskanen P, Billig H, Toppari J, Kaleva M, Arsalo A, Rapola J, et al. Apoptotic cell death in the normal and cryptorchid human testis: the effect of human chorionic gonadotropin on testicular cell survival. Pediatr Res. 1996;40(2):351–6.
Haimov-Kochman R, Prus D, Farchat M, Bdolah Y, Hurwitz A. Reproductive outcome of men with azoospermia due to cryptorchidism using assisted techniques. Int J Androl. 2010, 33(1):e139–43.
Henna MR, Del Nero RG, Sampaio CZ, Atallah AN, Schettini ST, Castro AA, et al. Hormonal cryptorchidism therapy: systematic review with metanalysis of randomized clinical trials. Pediatr Surg Int. 2004;20(5):357–9.
Hurwitz RS, Kaptein JS. How well does contralateral testis hypertrophy predict the absence of the nonpalpable testis? J Urol. 2001;165(2):588–92.
Jarow JP, Berkovitz GD, Migeon CJ, Gearhart JP, Walsh PC. Elevation of serum gonadotropins establishes the diagnosis of anorchism in prepubertal boys with bilateral cryptorchidism. J Urol. 1986;136(1 Pt 2):277–9.
John Radcliffe Hospital Cryptorchidism Study Group. Cryptorchidism: an apparent substantial increase since 1960. Br Med J (Clinical research ed.) 1986;293(6559):1401–4.
Kanemoto K, Hayashi Y, Kojima Y, Maruyama T, Ito M, Kohri K. Accuracy of ultrasonography and magnetic resonance imaging in the diagnosis of non-palpable testis. Int J Urol. 2005;12(7):668–72.
Kantarci M, Doganay S, Yalcin A, Aksoy Y, Yilmaz-Cankaya B, Salman B. Diagnostic performance of diffusion-weighted MRI in the detection of nonpalpable undescended testes: comparison with conventional MRI and surgical findings. AJR Am J Roentgenol. 2010;195(4):W268–73.
Karaman I, Karaman A, Erdogan D, Cavusoglu YH. The transscrotal approach for recurrent and iatrogenic undescended testes. Eur J Pediatr Surg. 2010;20(4):267–9.
Kirsch AJ, Escala J, Duckett JW, Smith GH, Zderic SA, Canning DA, et al. Surgical management of the nonpalpable testis: the Children’s Hospital of Philadelphia experience. J Urol. 1998;159(4):1340–3.
Kollin C, Karpe B, Hesser U, Granholm T, Ritzen EM. Surgical treatment of unilaterally undescended testes: testicular growth after randomization to orchiopexy at age 9 months or 3 years. J Urol. 2007;178(4 Pt 2):1589–93. discussion 93.
Lee PA, O’Leary LA, Songer NJ, Bellinger MF, LaPorte RE. Paternity after cryptorchidism: lack of correlation with age at orchidopexy. Br J Urol. 1995;75(6):704–7.
Lee MM, Donahoe PK, Silverman BL, Hasegawa T, Hasegawa Y, Gustafson ML, et al. Measurements of serum mullerian inhibiting substance in the evaluation of children with nonpalpable gonads. N Engl J Med. 1997;336(21):1480–6.
Lustig RH, Conte FA, Kogan BA, Grumbach MM. Ontogeny of gonadotropin secretion in congenital anorchism: sexual dimorphism versus syndrome of gonadal dysgenesis and diagnostic considerations. J Urol. 1987;138(3):587–91.
Moore RG, Peters CA, Bauer SB, Mandell J, Retik AB. Laparoscopic evaluation of the nonpalpable tests: a prospective assessment of accuracy. J Urol. 1994;151(3):728–31.
Na SW, Kim SO, Hwang EC, Oh KJ, Jeong SI, Kang TW, et al. Single scrotal incision orchiopexy for children with palpable low-lying undescended testis: early outcome of a prospective randomized controlled study. Korean J Urol. 2011;52(9):637–41.
Pettersson A, Richiardi L, Nordenskjold A, Kaijser M, Akre O. Age at surgery for undescended testis and risk of testicular cancer. N Engl J Med. 2007;356(18):1835–41.
Rozanski TA, Wojno KJ, Bloom DA. The remnant orchiectomy. J Urol. 1996;155(2):712–3. discussion 4.
Schwentner C, Oswald J, Kreczy A, Lunacek A, Bartsch G, Deibl M, et al. Neoadjuvant gonadotropin-releasing hormone therapy before surgery may improve the fertility index in undescended testes: a prospective randomized trial. J Urol. 2005;173(3):974–7.
Scorer CG. The descent of the testis. Arch Dis Child. 1964;39:605–9.
Sijstermans K, Hack WW, van der Voort-Doedens LM, Meijer RW, Haasnoot K. Puberty stage and spontaneous descent of acquired undescended testis: implications for therapy? Int J Androl. 2006;29(6):597–602.
Snodgrass W, Chen K, Harrison C. Initial scrotal incision for unilateral nonpalpable testis. J Urol. 2004;172(4 Pt 2):1742–5. discussion 5.
Snodgrass WT, Yucel S, Ziada A. Scrotal exploration for unilateral nonpalpable testis. J Urol. 2007;178(4 Pt 2):1718–21.
Snodgrass W, Bush N, Holzer M, Zhang S. Current referral patterns and means to improve accuracy in diagnosis of undescended testis. Pediatrics. 2011;127(2):e382–8.
Tasian GE, Copp HL. Diagnostic performance of ultrasound in nonpalpable cryptorchidism: a systematic review and meta-analysis. Pediatrics. 2011;127(1):119–28.
Tasian GE, Copp HL, Baskin LS. Diagnostic imaging in cryptorchidism: utility, indications, and effectiveness. J Pediatr Surg. 2011;46(12):2406–13.
Tennenbaum SY, Lerner SE, McAleer IM, Packer MG, Scherz HC, Kaplan GW. Preoperative laparoscopic localization of the nonpalpable testis: a critical analysis of a 10-year experience. J Urol. 1994;151(3):732–4.
Tong Q, Zheng L, Tang S, Mao Y, Wang Y, Liu Y, et al. Laparoscopy-assisted orchiopexy for recurrent undescended testes in children. J Pediatr Surg. 2009;44(4):806–10.
Wagner-Mahler K, Kurzenne JY, Delattre I, Berard E, Mas JC, Bornebush L, et al. Prospective study on the prevalence and associated risk factors of cryptorchidism in 6246 newborn boys from Nice area, France. Int J Androl. 2011;34(5 Pt 2):e499–510.
Walsh TJ, Dall’Era MA, Croughan MS, Carroll PR, Turek PJ. Prepubertal orchiopexy for cryptorchidism may be associated with lower risk of testicular cancer. J Urol. 2007;178(4 Pt 1):1440–6. discussion 6.
Wiser A, Raviv G, Weissenberg R, Elizur SE, Levron J, Machtinger R, et al. Does age at orchidopexy impact on the results of testicular sperm extraction? Reprod Biomed Online. 2009;19(6):778–83.
Wood HM, Elder JS. Cryptorchidism and testicular cancer: separating fact from fiction. J Urol. 2009;181(2):452–61.
Ziylan O, Oktar T, Korgali E, Nane I, Ander H. Failed orchiopexy. Urol Int. 2004;73(4):313–5.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2013 Springer Science+Business Media New York
About this chapter
Cite this chapter
Snodgrass, W.T. (2013). Undescended Testes. In: Snodgrass, W. (eds) Pediatric Urology. Springer, New York, NY. https://doi.org/10.1007/978-1-4614-6910-0_5
Download citation
DOI: https://doi.org/10.1007/978-1-4614-6910-0_5
Published:
Publisher Name: Springer, New York, NY
Print ISBN: 978-1-4614-6909-4
Online ISBN: 978-1-4614-6910-0
eBook Packages: MedicineMedicine (R0)