Abstract
The importance of cryptorchidism treatment concerns the possibility of diminishing risk of malignant degeneration and improving fertility. Success rates of hormonal treatment vary: 0–55%with human chorionic gonadotropin (hCG) and 9–78% with gonadotropin-releasing hormone (GnRH). Due to uncertainties regarding the effectiveness of this treatment, a systematic review and meta-analysis of randomized controlled trials (RCTs) on hormonal cryptorchidism treatment was done using the methodology of Cochrane Collaboration. Two studies compared hCG with GnRH, with a testicular descent rate of 25% vs. 18%, respectively. Nine trials compared intranasal LHRH with placebo, with complete testicular descent rates of 19% vs. 5%. Two other studies comparing doses and administration intervals could not be pooled together due to heterogeneity. With the information analyzed until the present, the evidence for the use of hCG vs. GnRH shows advantages for hCG, and this review also shows that there is evidence that luteinizing hormone releasing hormone (LHRH) is more effective than placebo. But because this evidence is based on few trials, with small sample sizes and moderated risk of bias, this treatment cannot be recommended for everyone, and there is no evidence that supports hCG’s use in larger doses and larger intervals. Results from this systematic review are important for developing better RCTs that may decrease the uncertainty of cryptorchidism treatment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The importance of cryptorchidism treatment concerns the possibility of diminishing risk of malignant degeneration [1, 2] and improving fertility. The proper treatment of cryptorchidism is still controversial. In the past, it has been dictated by experts in hormonal therapy. Success rates of hormonal treatment vary from 0–55%with human chorionic gonadotropin (hCG) and from 9–78% with gonadotropin-releasing hormone (GnRH) [3]. The surgeon is able to place the undescended testis into the scrotum; however, surgical treatment is not perfect, and complications rates range from 1.5% to 12.2% [4]. Certain outstanding difficulties are encountered in surgical procedures when the scrotum is undeveloped and the testis is malformed, small, and associated with short vessels [5].
By ascertaining the causes of undescended testis, the action of gonadotropic factor, and the efficacy of surgical procedures, one should be able to reconstruct a rational form of treatment. To determine the principles of each treatment method (either surgery or the administration of gonadotropic factor), it is first necessary to comprehend as thoroughly as possible the action of the gonadotropic principle. Nevertheless, the hormonal treatment of cryptorchidism has been uncertain and controversial for the last 200 years.
Therefore, we decided to systematically review and synthesize the available clinical evidence of hormonal treatment of cryptorchidism. The objectives were to evaluate the efficacy and safety of hormonal cryptorchidism treatment with hCG compared with GnRH. This project also aims to compare luteinizing hormone releasing hormone (LHRH) with placebo and the hormonal therapeutic scheme with intramuscular hCG.
Methods
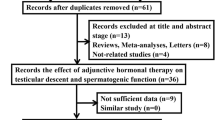
Three systematic reviews with meta-analysis of randomized clinical trials (RCTs) were performed according to the Cochrane Collaboration methodology [6]. The target population was children with cryptorchidism diagnosed by detailed physical exam, and the main groups of interventions to be compared were (1) intramuscular hCG vs. intranasal GnRH, (2) intranasal LHRH vs. placebo, and (3) intramuscular hCG in different doses and intervals of administration. The main outcome to be evaluated was complete testicular descent.
Several sources of information were searched in order to identify RCTs, including (1) the electronic databases Medline, Embase, Lilacs, and Cochrane Controlled Trials, with no restrictions concerning date, language, or otherwise, (2) hand-searching of relevant medical journals (Pediatric Surgery International, Journal of Pediatric Surgery, and Revista de Cirurgia Infantil), (3) cross-checking of the references of identified studies, and (4) personal contact with specialists and representatives of pharmaceutical companies. The last search date was June 2003.
The main procedures for evaluating the identified data were performed by two authors independently. Selection of studies, critical appraisal, collection, analysis, and data interpretation disagreements were solved by consensus. The RCTs’ quality evaluations were made taking into account randomization, blindness, and description of withdrawals and dropouts The main analysis includes all RTCs that presented children with cryptorchidism treated with either hCG, GnRH, or placebo. The main outcomes of interest were dichotomous measures, which were analyzed by the combined logarithm of the Peto odds ratio (fixed-effect model) with the corresponding 95% confidence interval (CI). When overall results were significant, relative risk reduction (RRR), number needed to treat (NNT) to produce (or prevent) one outcome, and 95% CI around these measures were calculated.
Results
Three RCTs comparing intramuscular hCG with intranasal GnRH were found (Rajfer et al. 1986 [7]; Christiansen et al. 1988 [4]; Christiansen et al. 1992 [8]), and two of them were included (Rajfer et al. 1986 [7]; Christiansen et al. 1992 [8]). In the quality evaluation they were classified as having moderate risk of bias because allocation concealment was not properly described.
Two hundred and one subjects were evaluated, 109 with bilateral cryptorchidism and 92 with unilateral: 102 were treated with intramuscular hCG (51 bilateral and 51 unilateral, resulting in 153 testis) and 99 with intranasal GnRH (58 bilateral and 41 unilateral, resulting in 157 testis). Patients who received hCG were compared with those who received GnRH: complete testicular descent was 25% vs. 18%, absolute risk reduction (ARR) 7%, and 95% CIs 0.012–0.170.
Nine randomized controlled trials studied the use of intranasal GnRh compared with placebo (Illig et al. 1977 [9], Illig et al. 1980 [10], Karpe et al. 1983 [11], Klidjian et al. 1985 [12], Wit et al. 1986 [13], de Muinck 1988 [14], Hagberg and Westphal 1987 [15], Olsen et al. 1992 [11], Christiansen et al. 1992 [8], Bica and Hadziselimovic 1993 [17]). Only one adequately described the randomization process, 90% (8/9) of the studies were “double blinded,” and in two of them the placebo was described. The concealment procedure was described, and the dropout rates were zero. Of 1,049 patients studied, 585 were treated with LHRH and 544 with placebo. The patients who received LHRH compared with those who received placebo showed complete testicular descent: 19% vs. 5%, Peto odds ratio 3.59, 95% CIs 2.52–5.12.
We identified and selected only two studies on doses and intervals of administration. They were randomized but did not adequately describe the randomization approach. These two clinical trials did not use the same distribution standard of doses and hCG administration intervals; therefore, it was not reasonable to pool the data together. Instead, we evaluated these studies separately. Forest’s 1988 study [18] compared two protocols using seven hCG injections of 1,500 IU on alternate days (G1) vs. four hCG injections of 100 IU/kg/dose every 4–5 days (G4). Hesse’s 1988 study [19] compared 10 hCG injections administrated twice a week, varying the dosage according to the groups’ ages (G3), vs. three hCG injections administrated at 7- or 10-day intervals with larger doses and also according to the groups’ ages (G7). Results for complete testicular descent in unilateral cryptorchidism were Forest: G1=51% vs. G4=51%, ARR 0.03 (95% CI 18–18); Hesse: G3=19% vs. G7=17%, ARR 2% (95% CI 6–10). Results for complete testicular descent in bilateral cryptorchidism were Forest: G1=48% vs. G4=50%, RRA 1.7 (95% CI 15–18); Hesse: G3=26% vs. G7=11%, ARR 14% (95% CI 6–21) and NNT 8 (5–16).
Discussion
Hormonal therapy may play a role in managing undescended testes. Surgery should be reserved for those who fail to respond to therapy and as an alternative for the high testis before surgery in order to elongate the cord structures and enlarge the inguinal canal by stimulating the natural processes of development [13].
The exact age for the use of this treatment may be an important factor for the treatment’s success. De Muinck found the highest success rate in patients ranging from 5–12 years old [14]. This result was in contrast to other studies in which the highest success rates were achieved in boys who were 2–5 years old [8]. The weight of the evidence, therefore, is in favor of early intervention, preferably before age 2 because of morphological changes such as reduction in number and size of the tubules and increase in the intervening stroma [17]. However, most of the boys treated in analyzed trials were older than 2 years of age.
The data of this systematic review have demonstrated that no sufficient evidence exists to recommend hormonal therapy with hCG or LHRH for cryptorchidism because the studies do not have adequate designs, sample sizes, or statistical power. If an intervention reviewed is used, the currently available evidence should be discussed with the patient’s relatives [20].
In this review, every effort was made to reduce biases, although the quality of reporting regarding trial performance and outcomes may have limited this aim. All studies were classified as having a moderate risk of selection bias, thus being more likely to favor the experimental treatment [21].
One of the aims of meta-analysis is to collect the largest number of trials with the same outcome in order to improve statistical power. However, in this review, few and short studies could increase the chance for biased results that do not reflect a population with a normal distribution [22].
Although only randomized and controlled clinical trials were included, none of them reported the randomization procedure for the patients, thus the quality of the randomized allocation process might have been affected. Another limitation we found was related to the small sample sizes, which affect outcomes. None of the included studies reported how their sample size was calculated.
The clinical trials on a hormonal therapeutic scheme with hCG did not adhere to the same standard of distribution of patients, doses, and intervals of hCG administration, so it became difficult to cross the data obtained in relation to the dose-response required to evaluate the studies separately. Grouping different causal factors may lead to meaningless effect sizes estimates, and the failure to relate data to theories may obscure discrepancies [23].
Given the relative lack of success of drugs assessed in this review, it may be necessary to conduct a new set of clinical studies characterized by new research designs.
Conclusion
The best existing evidence for using hCG compared with GnRH and placebo shows the advantages of hCG, although there is no evidence that supports the use of hCG in larger doses with larger intervals. These data are not very reliable as a conclusion of this intervention’s effectiveness and safety. Better planned and executed studies could determine the real benefit of hormonal therapy in cryptorchidism treatment so that decisions could be based on more scientifically credible evidence.
References
Martin DC (1979) Germinal cell tumors of the testis after orchiopexy. J Urol 121:422–424
Pottern LM, Brown LM, Hoover RN (1985) Testicular cancer risk among young men. J Nat Canc Institut 74:377–381
Pyörälä S, HuttunenNP, Uhari M (1995) A review and meta-analysis of hormonal treatment of cryptorchidism. J Clin Endocr Metabol 80:2795–2799
Christiansen P, Müller J, Buhl S, et al. (1988) Treatment of cryptorchidism with human gonadotropin or gonadotropin hormone. Horm Res 30:187-192
Gross RE, Jewett JR (1956) Surgical experiences from 1222 operations for undescended testis. JAMA 25:634–641
Egger M, Davey-Smith G (1995) Misleading meta-analysis. BMJ 310:752–754
Rajfer J, Handelsman DJ, Swerdoloff RS, et al. (1986) Hormonal therapy of cryptorchidism. A randomized, double-blind study comparing human chorionic gonadotropin and gonadotropin- releasing hormone. N Engl J Med 314:466–470
Christiansen P, Müller J, Buhl S, et al. (1992) Hormonal treatment of cryptorchidism: hCG or GnRH—a multicentre study. Acta Paediatr 81:605–608
Illig R, Kollmann F, Borkenstein M, et al. (1977) Treatment of cryptorchidism intranasal synthetic lutenising-hormone releasing hormone. Lancet 10:518–520
Illig R, Torrasani T, Bucher H, et al. (1980) Effect of intranasal LHRH therapy on plasma LH, FSH and testosterone, and relation to clinical results in prepubertal boys with cryptorchidism. Clin Endocrinol 12:91–97
Karpe B, Eneroth P, Ritzén M (1983) LHRH treatment in unilateral cryptorchidism: effect on testicular descent and hormonal response. J Pediatr 892–896
Klidjian AM, Swift PGF, Jonhstone JMS (1985) LHRH for incomplete descent of the testis. Arch Dis Child 60:528–571
Wit JM, Delemarre-Van de Waal HA, Bax NMA, Van Den Brande JL (1986) Effect of LHRH treatment on testicular descent and hormonal response in cryptorchidism. Clin Endocrinol 24:539–548
De Muinck Keizer-Schrama SM (1988) Hormonal treatment of cryptorchidism. Horm Res 30:178–186
Hagberg S, Westphal O (1987) Results of combined hormonal and surgical treatment for undescended testis in boys under 3 years of age. Eur J Pediatr 2:S38-S39
Olsen LH, Genster HG, Mosegaard A, et al. (1992) Management of the non-descended testis: doubt value of luteinizing-hormone-releasing-hormone (LHRH). A double-blind, placebo-controlled multicentre study. Int J Androl 15:135–143
Bica DTG, Hadziselimovic F (1993) The behavior of epididymis, processus vaginalis and testicular descent in cryptorchid boys treated with buserelin. Eur J Pediatr 152:S38-S42
Forest MG, David M, David L, et al. (1988) Undescended testis: comparison of two protocols of treatment with human gonadotropin. Horm Res 30:198–206
Hesse V, Fischer G (1988) Three injections of human chorionic gonadotropin are as effective as ten injections in the treatment of cryptorchidism. Horm Res 30:193–197
Del Nero RGM, Atallah AN (1999) Therapeutic scheme (doses, and intervals of administration) with hCG in cryptorchidism: systematic review. Thesis, São Paulo Federal University
Eysenck HJ (1995) Problems with meta-analysis. In: Chalmers I, Altman DG (eds) Systematic reviews. BMJ, London, pp 67–74
Schulz KF, Chalmers I, Hayes RJ, Altman DC (1995) Empirical evidence of bias: dimensions of methodological quality associated with estimates of treatment effects in controlled trials. JAMA 273:408–412
Thorup J, Kvist N, Larsen P, Mauritzen K (1988) Clinical results of early and late operative correction of undescended testes. Br J Urol 56:322–325
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Henna, M.R., Del Nero, R.G.M., Zugaiar S. Sampaio, C. et al. Hormonal cryptorchidism therapy: systematic review with metanalysis of randomized clinical trials. Ped Surgery Int 20, 357–359 (2004). https://doi.org/10.1007/s00383-004-1198-3
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00383-004-1198-3