Abstract
Alignment of the prosthesis is one of the most significant factors that affect the long-term clinical outcome following total knee arthroplasty (TKA). There is conflicting evidence whether patient-specific instrumentation (PSI) for TKA improves the component position compared to standard instrumentation. This study aimed to compare the rotational alignment of the femoral and tibial components in TKA patients when performed with either conventional or PSI. Sixty patients with primary knee osteoarthritis were randomly divided into two groups treated surgically with TKA: one with conventional instrumentation and the other with the Visionaire PSI system (Smith and Nephew, Memphis, TN). Computerized tomography (CT) and X-ray imaging were performed preoperatively and 12 weeks after surgery. The rotational alignment of the femoral and tibial component in all patients was assessed postsurgically using CT imaging according to the Berger protocol. Both groups were clinically assessed in a blinded fashion using the Knee Society Score (KSS) and a visual analog scale (VAS). Fifty-eight patients were prospectively assessed. The mean postsurgical follow-up was 3.0 ± 0.4 months. CT images did not reveal any significant improvement in the rotational alignment of the implant components between the groups. X-rays revealed a significant improvement in the deviation from the optimal alignment range of the femoral component in the coronal plane in both groups. Patients operated with Visionaire PSI assistance had poorer functional outcomes. We conclude that there were no improvements in clinical outcomes or knee component alignment in patients treated with PSI compared with those treated with standard instruments. In addition, clinical and functional assessment showed inferior results in terms of KSS and VAS scores at the midterm follow-up in patients treated with PSI.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
- Computerized tomography
- Femoral component rotation
- Knee arthroplasty
- Patient-specific instrumentation
- Rotational alignment
- Tibia
1 Introduction
The primary objective of total knee arthroplasty (TKA) is to improve knee function and relieve pain. Another important factor is the implant longevity that determines the long-term effect of surgery (Mahaluxmivala et al. 2001; Ritter et al. 1994; Jeffery et al. 1991; Petersen and Engh 1988; Rand and Coventry 1988; Lotke and Ecker 1977). A rotational implant alignment is crucial for a long-term success of TKA. It has been reported that the vast majority of TKA procedures have internal rotational errors in the femoral/tibial component alignment (Nicoll and Rowley 2010). A frequent presence of such errors has also been evidenced in a study in which all TKA cases demonstrated knee stiffness due to tibial component misalignment consisting of excessive internal rotation (Bedard et al. 2011).
Patient-specific instrumentation (PSI) for TKA has emerged as a more precise alternative to standard instrumentation. The PSI, employing preoperative three-dimensional imaging, provides personalized jigs based on the anatomic landmarks to determine the placement of conventional cutting blocks, which helps maintain the correct positional relationship of components. Unlike the PSI, standard instrumentation relies on intramedullary or extramedullary alignment rods and the surgeon’s judgment for placement of conventional cutting blocks. There is scarce and conflicting evidence in the literature that compares the accuracy of PSI to standard instrumentation (Stronach et al. 2014; Conteduca et al. 2013; Conteduca et al. 2012; Ng et al. 2012; Nunley et al. 2012). The existing studies emphasize a coronal alignment and largely rely on the long-limb radiographs to establish the measurements. However, to evaluate the true accuracy of PSI, a preoperative 3D plan should be directly compared with the postoperative 3D prosthetic alignment.
The present study was designed to compare the degree of rotation of the femoral and tibial components in TKA patients who underwent joint replacement with either conventional or PSI instrumentation. We also assessed the midterm clinical results.
2 Methods
2.1 Patients and Intervention
The Ethics Committee of Warsaw Medical University in Warsaw, Poland, approved the study. All patients gave informed consent to participate in the study. The study included 60 patients who had been admitted to the Department of Orthopedics and Rehabilitation of Warsaw Medical University between November 2012 and December 2014. The patients’ mean age was 69.9 ± 6.5(SD) years, and they were all qualified for the TKA procedure due to primary knee osteoarthritis. The patients were randomly assigned to one of the two groups. The study group underwent TKA with the Visionaire PSI (VISIONAIRE; Smith and Nephew, Memphis, TN), and the second control group underwent TKA using a conventional instrumentation. A block randomization with a block size of six was performed using a computer-generated random number list that was prepared by an investigator who had no clinical involvement in the trial. The sequence was concealed until all data were analyzed. Each patient in the PSI and conventional groups had CT and X-ray scans on the operated knee, 3 weeks after surgery.
The methodology of the study precluded the possibility of a blinded patient-surgeon relationship. Therefore, to reduce the risk of a systematic bias related to the analysis of outcomes, the radiologist who assessed the degree of rotation in the femoral and tibial components was blinded concerning the technique used in a given patient.
2.2 Outcomes
The primary outcome was the rotational alignment of the femoral and tibial component, based on using the Berger protocol (Berger and Crossett 1998) and assessed postoperatively with CT imaging scans. The findings in the PSI and conventional groups were compared. Secondary endpoints focused on the clinical assessment, including function, which was evaluated in both groups with the Knee Society Score (KSS), and perception of pain evaluated on a visual analog score (VAS). Tertiary endpoints included the assessment of surgery duration, the length of the surgical scar, and the duration of postoperative hospital stay.
2.3 Radiologic Evaluation
Three independent radiologists were involved in the analysis of the 60 sets of CT scans in a random order and in separate rooms to prevent a possible recollection of the previous viewing. Each radiologist was asked to evaluate CT scans according to the Berger protocol. The readings were repeated 6 weeks later to assess intra-observer variability. The radiologists were not provided with any feedback concerning their assessments, and the CT scans were unavailable to them between the readings. A comparison of the imaging results is given in Table 2.
2.4 Statistical Evaluation
A sample size of 30 patients in each group was chosen based upon a recently published study that showed that a computer navigation had some significant benefits when compared with standard instrumentation (Woolson et al. 2014). The evaluation of continuous data was performed with a t-test and the Mann-Whitney U test for normally and non-normally distributed variables, respectively. The χ2 or Fisher’s exact test were used for the analysis of dichotomous outcomes, as appropriate. The relative risk (RR) or mean difference (MD) with 95% confidence intervals (95% CI) was calculated using StatsDirect v2.7.8b software. Differences between the groups were considered statistically significant when a p-value was <0.05, the 95%CI for RR did not exceed 1.0, or the RR for MD did not exceed 0. The results were analyzed using the intention to treat analysis (ITT) for postoperative data and the available case analysis for clinical data after a 12-week long follow-up. Computer software “R” v2.13.1 was used for all analyses.
3 Results
3.1 Study Flowchart
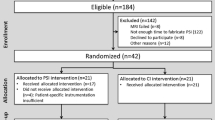
The study included 60 patients who, according to the randomization list, were assigned to the study (TKA with PSI) or control group, 30 patients each. All the data required for the assessment of primary and tertiary endpoints were successfully obtained from all the participants (ITT analysis). With regard to the secondary endpoints, data were obtained from 58 patients (two patients failed to report for follow-up). Therefore, the available case analysis was carried out (Fig. 1). Table 1 lists the patients’ demographic data, the main KSS assessment variables, and the subjective pain scale prior to surgery in the study group and in the control group (conventional TKA).
3.2 Radiologic and CT Evaluations
The CT scans were analyzed to assess the rotation of both femoral and tibial components. In the case of the femoral component, a slightly better positioning was observed in patients who had undergone TKA with PSI (0.2° ± 5.4° vs. −0.9° ± 6.5°; MD = 0.2°, 95% CI -1.27 - 1.67°). No statistically significant differences were found between the study and control groups in terms of mechanical lateral distal femur angle (mLDFA), medial proximal tibia angle (MPTA), or rotational alignment of tibial component. All these data are presented in Table 2.
3.3 Clinical Assessment: Secondary Endpoints
Clinical assessments performed, on average, in the 12th week postoperative follow-up did not reveal any significant differences between the two groups. The results of the assessments of KSS parameters and subjective pain were also comparable (Table 3). At the follow-up, poorer clinical outcomes, according to KSS and VAS scores, were observed in the patients who underwent TKA with PSI.
3.4 Evaluation of Perioperative and Intraoperative Parameters: Tertiary Endpoints
Tertiary endpoints were directly related to perioperative and intraoperative parameters, and they revealed certain significant differences between the two groups. The PSI-TKA group was found to feature, among other factors, a prolonged duration of surgery by more than 30 min (MD 32 min; 95%CI 24.7–39.3 min), a difference in the length of the surgical incision that was more than 2 cm longer (MD 2.1 cm; 95%CI: 1.0–3.2 cm), and approximately 2 additional days of hospital stay (MD 2.2 days; 95%CI: 0.4–4.0 days) (Table 4).
4 Discussion
The application of PSI is hypothesized to help achieve the optimal rotational placement of tibial and femoral components in TKA procedures. This prospective, randomized trial demonstrates that Visionaire PSI in patients undergoing TKA had no influence on the femoral and tibial axial rotation as assessed by CT imaging. Further, the choice of the surgical technique had no bearing upon clinical function or pain assessment after a 12-week follow-up.
According to the study by Heyse and Tibesku (2015), application of PSI for TKA considerably reduces the percentage of deviations from the optimal rotational placement of the tibial component in the magnetic resonance imaging assessments. Those authors have emphasized that the anatomy of the proximal end of the tibia is highly variable across the population, a feature that hinders the selection of the optimal points of reference and PSI production. In another article, the same authors have demonstrated a significant improvement in the rotational positioning of the femoral component in the PSI group compared to patients undergoing conventional surgery: akin to the tibia, rotation of the femoral component was assessed by magnetic resonance imaging (Heyse and Tibesku 2014). The incompatibility of the results of those studies with the current study may be influenced by the operator experience and the level of the operator’s comfort with each surgical technique. On the other hand, since the patients of those previous studies did not undergo clinical observation over time, no definite conclusions about the improvement of function can be reached.
The achievement of optimal alignment in the coronal, sagittal, and rotational plane is closely related to the performance of correct bone incisions in the tibia and femur adapted individually to each patient (Jenny et al. 2005; Laskin 2003; Reed and Gollish 1997; Jeffery et al. 1991). As an innovative concept capitalizing on the various advantages of computer technologies, PSI makes it possible to transfer some stages of surgery to preoperative planning. Compared to computer navigation, for instance, PSI does not entail significant additional costs and shortens the duration of surgery. In the current study, duration of surgery was shorter by 30 min in the control group. Likewise, the entire hospital stay of patients in the control group was 2 days shorter compared to the PSI-TKA group.
Despite numerous hypothetical and technical advantages related to the use of PSI, evidence-based data on the benefit of its application in terms of the patients’ improved clinical function are inconsistent. Some authors have concluded that there are such benefits, while others failed to demonstrate any differences compared to classical instrumentation (Fu et al. 2015). The current study also failed to confirm any advantageous effect of this type of instrumentation on the improvement of clinical function in patients after a 12-week postoperative follow-up.
4.1 Strengths and Limitations
We used the acceptable methods to generate the allocation sequence and allocation concealment. We then strived to maintain the blinding of data management and data analyses throughout the study. In addition, the length of follow-up was appropriate. Data on radiological outcomes were obtained for all patients and data on clinical outcomes for more than the 93% of them. All of these features minimize the risk of systematic bias.
We believe that this is the largest randomized trial to date that have assessed the efficacy of PSI by means of CT imaging. The application of CT together with a clinical assessment made it possible to evaluate and compare the efficacy of the two surgical techniques and could also suggest the mechanisms underlying the differences between the two groups.
In conclusion, the results of this study found that PSI and standard surgical techniques were comparable in terms of component alignment and patient-reported outcomes, although operative time and length of stay were longer in the PSI-TKA group. A number of studies have failed to demonstrate any advantages resulting from the use of PSI. Our current findings also failed to reveal any positive effects of PSI in terms of improved rotational component alignment or improved clinical outcomes. In light of the inconsistent data in the literature, further studies are still needed to resolve the contentious issue.
References
Bedard M, Vince KG, Redfern J, Collen SR (2011) Internal rotation of the tibial component is frequent in stiff total knee arthroplasty. Clin Orthop Relat Res 469(8):2346–2355
Berger RA, Crossett LS (1998) Determining the rotation of the femoral and tibial components in total knee arthroplasty: a computed tomography technique. Oper Tech Orthop 8:128–133
Conteduca F, Iorio R, Mazza D, Caperna L, Bolle G, Argento G, Ferretti A (2012) Are MRI-based, patient matched cutting jigs as accurate as the tibial guides? Int Orthop 36(8):1589–1593
Conteduca F, Iorio R, Mazza D, Caperna L, Bolle G, Argento G, Ferretti A (2013) Evaluation of the accuracy of a patient-specific instrumentation by navigation. Knee Surg Sports Traumatol Arthrosc 21(10):2194–2199
Fu H, Wang J, Zhou S, Cheng T, Zhang W, Wang Q, Zhang X (2015) No difference in mechanical alignment and femoral component placement between patient-specific instrumentation and conventional instrumentation in TKA. Knee Surg Sports Traumatol Arthrosc 23(11):3288–3295
Heyse TJ, Tibesku CO (2014) Improved femoral component rotation in TKA using patient-specific instrumentation. Knee 21(1):268–271
Heyse TJ, Tibesku CO (2015) Improved tibial component rotation in TKA using patient-specific instrumentation. Arch Orthop Trauma Surg 135(5):697–701
Jeffery RS, Morris RW, Denham RA (1991) Coronal alignment after total knee replacement. J Bone Joint Surgery Br 73(5):709–714
Jenny JY, Clemens U, Kohler S, Kiefer H, Konermann W, Miehlke RK (2005) Consistency of implantation of a total knee arthroplasty with a non-image-based navigation system: a case-control study of 235 cases compared with 235 conventionally implanted prostheses. J Arthroplast 20(7):832–839
Laskin RS (2003) Instrumentation pitfalls: you just can’t go on autopilot! J Arthroplast 18(3 Suppl 1):18–22
Lotke PA, Ecker ML (1977) Influence of positioning of prosthesis in total knee replacement. J Bone Joint Surg Am 59(1):77–79
Mahaluxmivala J, Bankes MJ, Nicolai P, Aldam CH, Allen PW (2001) The effect of surgeon experience on component positioning in 673 press fit condylar posterior cruciate-sacrificing total knee arthroplasties. J Arthroplast 16(5):635–640
Ng VY, DeClaire JH, Berend KR, Gulick BC, Lombardi AV Jr (2012) Improved accuracy of alignment with patient-specific positioning guides compared with manual instrumentation in TKA. Clin Orthop Relat Res 470(1):99–107
Nicoll D, Rowley DI (2010) Internal rotational error of the tibial component is a major cause of pain after total knee replacement. J Bone Joint Surg Br 92(9):1238–1244
Nunley RM, Ellison BS, Zhu J, Ruh EL, Howell SM, Barrack RL (2012) Do patient-specific guides improve coronal alignment in total knee arthroplasty? Clin Orthop Relat Res 470(3):895–902
Petersen TL, Engh GA (1988) Radiographic assessment of knee alignment after total knee arthroplasty. J Arthroplast 3(1):67–72
Rand JA, Coventry MB (1988) Ten-year evaluation of geometric total knee arthroplasty. Clin Orthop Relat Res (232):168–173
Reed SC, Gollish J (1997) The accuracy of femoral intramedullary guides in total knee arthroplasty. J Arthroplast 12(6):677–682
Ritter MA, Faris PM, Keating EM, Meding JB (1994) Postoperative alignment of total knee replacement. Its effect on survival. Clin Orthop Relat Res (299):153–156
Stronach BM, Pelt CE, Erickson JA, Peters CL (2014) Patient-specific instrumentation in total knee arthroplasty provides no improvement in component alignment. J Arthroplast 29(9):1705–1708
Woolson ST, Harris AH, Wagner DW, Giori NJ (2014) Component alignment during total knee arthroplasty with use of standard or custom instrumentation: a randomized clinical trial using computed tomography for postoperative alignment measurement. J Bone Joint Surg Am 96(5):366–372
Conflicts of Interest
The authors declared no conflicts of interest in relation to this article.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2018 Springer International Publishing AG, part of Springer Nature
About this chapter
Cite this chapter
Stolarczyk, A., Nagraba, L., Mitek, T., Stolarczyk, M., Deszczyński, J.M., Jakucinski, M. (2018). Does Patient-Specific Instrumentation Improve Femoral and Tibial Component Alignment in Total Knee Arthroplasty? A Prospective Randomized Study. In: Pokorski, M. (eds) Rehabilitation Science in Context . Advances in Experimental Medicine and Biology(), vol 1096. Springer, Cham. https://doi.org/10.1007/5584_2018_193
Download citation
DOI: https://doi.org/10.1007/5584_2018_193
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-95707-4
Online ISBN: 978-3-319-95708-1
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)