Abstract
Traumatic brain injury (TBI) is a leading cause of death and disability in the USA. Common causes of TBI include falls, violence, injuries from wars, and vehicular and sporting accidents. The initial direct mechanical damage in TBI is followed by progressive secondary injuries such as brain swelling, perturbed cerebral blood flow (CBF), abnormal cerebrovascular reactivity (CR), metabolic dysfunction, blood–brain-barrier disruption, inflammation, oxidative stress, and excitotoxicity, among others. Magnetic resonance imaging (MRI) offers the means to noninvasively probe many of these secondary injuries. MRI has been used to image anatomical, physiological, and functional changes associated with TBI in a longitudinal manner. This chapter describes controlled cortical impact (CCI) TBI surgical procedures, a few common MRI protocols used in TBI imaging, and, finally, image analysis pertaining to experimental TBI imaging in rats.
Access provided by CONRICYT – Journals CONACYT. Download protocol PDF
Similar content being viewed by others
Key words
1 Introduction
Traumatic brain injury (TBI) is a leading cause of death and disability, affecting 3.5 million American civilians, with an annual cost exceeding $60 billion [1]. In addition, more than 270,000 US service members have been diagnosed with TBI since the beginning of the global war on terrorism (http://dvbic.dcoe.mil). Common causes of TBI include falls, violence, injuries from wars, and vehicular and sporting accidents. The initial direct mechanical damage in TBI is followed by progressive secondary damage such as brain swelling, perturbed cerebral blood flow (CBF) , abnormal cerebrovascular reactivity (CR), metabolic dysfunction, blood–brain-barrier disruption, inflammation, oxidative stress, and excitotoxicity, among others [2, 3]. Ischemic-like events (such as membrane depolarization, ion dysregulation, oxidative stress, excitotoxicity, and inflammation, among others) subsequently lead to apoptotic and necrotic cell death. The multidimensional cascades of secondary brain injury in TBI offer many potential targets for therapeutic intervention.
Magnetic resonance imaging (MRI) offers the means to noninvasively probe many of these secondary injuries. MRI has been used to image anatomical, physiological, and functional changes associated with TBI in a longitudinal manner [4, 5]. T 1 and T 2 anatomical MRI allows for visualization of gross structural damage, possible hemorrhage, and vasogenic edema in TBI [6, 7]. Diffusion-weighted imaging , in which contrast is based on the apparent diffusion coefficient (ADC) of water, can detect ischemic brain injury within minutes. ADC reduction is often attributed to cytotoxic edema, a common feature of TBI [8–10]. Diffusion tensor imaging (DTI) provides both magnitude and directional information about water diffusion and thus has been used to detect changes in fiber tracts following TBI [11]. Fractional anisotropy (FA), an index of anisotropy of water motion from DTI measurements, is sensitive to white-matter injury, microstructural changes [12, 13], and diffuse axonal injury [13–17] in TBI.
Disruptions in CBF and CR could be the result of either direct mechanical injury to vessels or indirect reduction of local perfusion pressure by elevated intracranial pressure. CBF can be measured using an exogenous intravascular contrast agent or by magnetically labeling the endogenous water in blood [18, 19]. The former is efficient, but it is incompatible with dynamic CBF fMRI as the long half-life of the contrast agent allows only one CBF measurement per bolus injection. Arterial spin labeling (ASL) techniques, on the other hand, are totally noninvasive, and the labeled water has a short half-life (~blood T 1), making it possible to perform multiple repeated measurements that can be used to augment spatial resolution and/or signal-to-noise ratio.
Blood–brain-barrier (BBB) disruption is common following TBI [20, 21]. Traditional histological Evans Blue extravasation has been widely used to measure BBB leakage following TBI [20, 22, 23]. However, this method requires the sacrifice of the animals and does not allow for longitudinal assessments. Dynamic contrast-enhanced (DCE) MRI can longitudinally measure the transport coefficient K trans which reflects BBB permeability [24].
Rodent models have been widely utilized to study TBI; they include the controlled cortical impact (CCI), fluid percussion, acceleration-impact or weight drop , Marmarou, Feeney, and blast injury models [25, 26]. The common areas of impact included somatosensory/motor, auditory, parietal, and visual cortices. Outcomes and lesion sizes are highly variable due to the use of different experimental models and/or different injury parameters [25, 26].
In this chapter, we describe the controlled cortical impact (CCI) TBI surgery procedures, a few common MRI protocols used in TBI imaging, and, finally, image analysis pertaining to experimental TBI imaging in rats.
2 Materials
2.1 TBI Modeling
-
1.
Rats (200–250 g) (Taconic Farms, Hudson, NY; Charles River, Wilmington, MA).
-
2.
Anesthetics (isoflurane or pentobarbital, etc.) (VetOne, MWI, Boise, ID).
-
3.
Common surgical tools and supplies (Fine Science Tools, Foster City, CA; Integra Miltex, Plainsboro, NJ; World Precision Instruments, Sarasota, FL; Ethicon, Somerville, NJ).
-
4.
Pneumatic controlled cortical impactor (Precision Systems and Instrumentation, Fairfax Station, VA).
-
5.
Stereotaxic frame equipped with tooth and ear bars (myNeurolab.com, St. Louis, MO).
-
6.
Bone wax (Ethicon, Somerville, NJ).
-
7.
Antibiotic ointment (McKesson, Richmond, VA).
-
8.
Analgesic (Buprenex) (Henry Schein, Melville, NY).
-
9.
Warm pad, temperature feedback monitoring , and other monitoring equipment to ensure normal animal physiology (Fisher Scientific, Pittsburgh, PA; Cole-Palmer, Vernon Hills, IL).
-
10.
Cresyl violet acetate for Nissl staining (Sigma, St. Louis, MO).
2.2 MRI
-
1.
Bruker 7 T scanner (Billerica, MA).
-
2.
40-G/cm BGA12 gradient insert (ID = 12 cm, 120 μs rise time).
-
3.
Animal holder (custom-made).
-
4.
Custom-made RF transmitter and receiver coils for brain imaging.
-
5.
Custom-made RF transmitter coil for arterial spin labeling.
-
6.
Actively decoupled switch box to detune RF coils.
-
7.
Other magnet, gradient, and RF coil configurations should also work.
2.3 Peripheral MRI-Compatible Monitor Equipment and Animal Supports
-
1.
Oximetry (heart rate, arterial oxygen saturation ) (Mouse Ox, STARR Life Sciences, Oakmont, PA).
-
2.
Blood pressure (invasive with artery catheterization) (Biopac/Acknowledge, Goleta, CA).
-
3.
Respiration rate via force transducer (Biopac/Acknowledge, Goleta, CA).
-
4.
Forepaw stimulation device—home-made device or Grass stimulators.
-
5.
Circulating warm water bath (Haake water bath, Rheology Solutions, Bacchus Marsh, Victoria, Australia; Cole Palmer, Vernon Hills, IL).
-
6.
Temperature feedback regulator (Digi-Sense, Cole-Palmer, Vernon Hills, IL).
-
7.
Anesthetic delivery, such as vaporizer (Universal Vaporizer Support, Foster City, CA).
3 Methods
3.1 TBI Surgery [24, 27–32]
-
1.
Male rats (250–350 g) are anesthetized with isoflurane (~2 %). Other anesthetics can also be used. Male rats are often used to avoid the effects of female hormones on outcome. Female rats are also widely studied; some female hormones have been found to have neuroprotective effects.
-
2.
Aseptic preparations (Betadine and ethanol washes) should be performed to prevent infection and immunological responses that could affect outcome.
-
3.
The animal is secured in a stereotaxic frame with ear and tooth bars; an incision is made at the level of the cerebellum as posterior from the impact site as possible to prevent artifacts during MRI acquisition. The periosteum is removed over the impact site. A Ø5mm craniotomy is created over the left S1FL (+0.25 mm anterior and 3.5 mm lateral to bregma), exposing the dura matter. The intact dura matter is impacted using a pneumatic-controlled cortical impactor (Precision Systems and Instrumentation, LLC, Fairfax Station, VA) fitted with a Ø3mm tip (5.0 m/s, 250 μs dwell time, 1 mm depth) to produce a mild focal TBI. Following the impact, the cranial opening is sealed with bone wax, the scalp sutured closed, and antibiotic ointment applied. Saline is injected under the skin to facilitate the removal of air pockets between the scalp and the skull, thus minimizing artifacts during MRI acquisition (see Note 1 ). Buprenex (0.05 mg/kg) is given subcutaneously every 12 h for 3 days as needed for pain relief.
-
4.
The right femoral artery is catheterized for blood-gas sampling, continuous blood pressure, and heart-rate monitoring . These physiological parameters are important, because deviations could affect TBI outcome causing an increase in statistical scatters.
-
5.
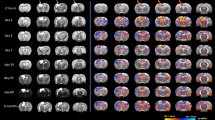
Rats are secured in a supine position on an MR-compatible rat stereotaxic headset, and anesthesia is reduced to ~1.1 % isoflurane. Rats breathe spontaneously. Mechanical ventilation can also be used. Rectal temperature should be maintained at 37.0 ± 0.5 °C. It is strongly suggested that heart rate, respiration rate, mean arterial blood pressure, and oxygen saturation (from oximetry) are monitored. Blood gas should be sampled once during a break between imaging scans. All recorded physiological parameters are within normal physiological ranges. MRI is acquired on the day of the TBI procedure (1–3 h post-TBI), and again on days 1, 2, 7, and 14 after TBI onset.
-
6.
Rectal temperature is maintained at 36.5–37.5 °C and respirations are recorded throughout the study. Body core temperature is critical, because it could affect the outcome.
-
7.
Nissl staining is used to measure morphological changes within and around the impact following TBI [27, 33]. Briefly, anesthetized rats are perfused on day 14 post-TBI with ice-cold heparinized phosphate-buffered saline, followed by ice-cold 4 % buffered paraformaldehyde (PFA). Brains are removed and post-fixed with 4 % PFA and subsequently cryopreserved (30 % sucrose) for 48 h at 4 °C. Coronal section measuring 25-μm are affixed to gelatin-coated slides and dried overnight at 37 °C. Slides are hydrated through a series of graded alcohols to distilled water, followed by 0.1 % cresyl violet acetate for 7 min. Brain sections are then dehydrated, cleared in Histo-clear, xylene and cover-slipped with Permount mounting medium. Images are acquired on an Olympus BX60F microscope equipped with an Olympus DP70 camera. A 5× objective is utilized to acquire images for mosaic full brain images assimilated MRI using Microsoft ICE software. Intact neurons are defined as nonbasophilic neurons with pale nuclei and discrete nucleoli and that had an intact neuronal body. Dark-stained neurons are defined as neurons with abnormal morphology, such as hyperbasophilic neurons and neurons with shrunken morphology.
3.2 MRI
-
1.
Position of RF coil: Position the RF coil as central to the region of interest as possible. For a surface coil, avoid pressing the coil too hard on the animal’s head as it would increase “loading,” which decreases SNR.
-
2.
Tune and match RF coil: Tune and match RF coil by adjusting the capacitors to 1 H resonance frequency and 50 Ω.
-
3.
Position scan: Position the scan on x, y, and z to ensure that the subject is centered. Open up the FOV if needed.
-
4.
Shimming: Run autoshim or manual shim as needed.
-
5.
Calibrate RF pulses: Calibrate RF pulses for given pulse shapes and durations. This can be set up to be done automatically.
-
6.
Pilot scan: Perform a pilot scan, using a 2D gradient echo FLASH or RARE sequence (10–30 s). Based on the pilot scan, plan 5–8 1.0 mm coronal slices to cover the region of interest.
-
7.
T 2 map (9.5 min): T 2-weighted images are acquired using a fast spin-echo sequence with four effective echo times (18, 54, 90, and 126 ms), and four echo train lengths, where the center of the echo train is taken as the effective TE for T 2 calculation. Typical parameters are spectral width 30–50 kHz, TR = 2–3 s (90° flip angle), pulse shape Gaussian or Sinc3, and pulse duration 1–2 ms.
-
8.
Diffusion tensor-weighted MRI (3.5 min): DTIs are obtained with five b = 0 and 30 directions with a 1200 s/mm2 b max-value. Echo planar imaging (EPI) scans with partial Fourier (3/4) are also acquired using the following settings: seven 1.0 mm coronal images, field of view (FOV) = 2.56 × 2.56 cm, matrix 96 × 96 and reconstructed to 128 × 128, single shot, repetition time (TR) = 3 s, echo time (TE) = 32 msec, separate between diffusion gradient Δ = 14 ms, diffusion gradient duration δ = 5 ms, and 2 transients for signal averaging.
-
9.
CBF: There are two methods to measure CBF , namely continuous arterial spin labeling (cASL) or dynamic susceptibility contrast (DSC) MRI with Magnevist (Gd-DTPA) or Omiscan (another contrast agent). With the latter, measurement can only be made once every hour or so because intravascular half-life of MRI is on the order of 6 min. In TBI, the contrast agent is often trapped; a longer wait time may be necessary.
For the cASL technique, single-shot, gradient-echo, and echo-planar-imaging (EPI) acquisition is used. Paired images are acquired alternately—one with arterial spin labeling and the other without (control). MR parameters are as follows: data matrix = seven 1.0 mm coronal images, field of view (FOV) = 2.56 × 2.56 cm, matrix 96 × 96 and reconstructed to 128 × 128, single shot, repetition time (TR) = 3 s, and echo time (TE) = 10.2 msec. Continuous arterial spin labeling employed a 2.7-s square radiofrequency pulse to the labeling coil in the presence of 1.0 G/cm gradient along the flow direction, such that the condition of adiabatic inversion is satisfied. The sign of the frequency offset is switched for control (non-labeled) images. Number of averages is typically 60–100 depending on the SNR needed.
Parameters for the DSC technique are single-shot, gradient-echo, echo-planar-imaging (EPI) acquisition with matrix =64 × 64, FOV = 2.56 cm × 2.56 cm, 3–5 slices of 1.0 mm, TE = 20 ms, and TR = 0.333 s (22° flip angle). Preload the IV line with 0.15–0.2 ml of Magnevist or Omiscan (typically 3 ft long of PE-50 tubing will hold such volume). About 20 s into the acquisition, deliver the contrast agent in a single bolus flush of saline. Continue DSC acquisition for another 40 s. Note that if DSC is used, Gd-DTPA has a non-negligible intravascular half-life. cASL and fMRI studies cannot be done immediately after Gd-DTPA injection (see Note 2 ).
-
10.
fMRI: Combined CBF and BOLD measurements are made using the continuous arterial spin-labeling technique with single-shot, gradient-echo, and echo-planar-imaging (EPI) acquisition. Paired images are acquired alternately—one with arterial spin labeling and the other without (control). MR parameters are as follows: seven 1.0 mm coronal images, field of view (FOV) = 2.56 × 2.56 cm, matrix 96 × 96 and reconstructed to 128 × 128, single shot, repetition time (TR) = 3 s, and echo time (TE) = 10.2 ms. Continuous arterial spin labeling employed a 2.7-s square radiofrequency pulse to the labeling coil in the presence of 1.0 G/cm gradient along the flow direction, such that the condition of adiabatic inversion is satisfied. The sign of the frequency offset is switched for control (non-labeled) images. For each set of fMRI measurements, 4 min of baseline data acquisition, 3 min of data acquisition during hypercapnic challenge, and 3 min of data acquisition during the post-stimulation surveillance period. Hypercapnic challenges use a premixed gas of 5 % CO2 with 21 % O2 and balance N2.
-
11.
K trans -MRI (19.4 min): K trans MRI data are acquired using a 2D multi-slice FLASH sequence. A prescan module is used to determine the flip angle and M 0 distribution, which includes 3 FLASH scans with different TRs: 64 ms (scan 1), 200 ms (scan 2), and 3000 ms (scan 3). The rest of imaging parameters are as follows: five 1.0 mm coronal slices, TE = 2 ms, FOV = 2.56 × 2.56 cm2, 128 × 128 data matrix, and 30° nominal flip angle. The prescan takes 7.4 min. Dynamic scans use a TR of 64 ms, and otherwise identical sequence parameters. After baseline data are acquired for 2 min, a bolus (0.2 ml/kg) of gadodiamide (GE Healthcare, USA) is injected intravenously through the tail vein, during which the dynamic scan is continued. A total of 90 dynamic images are acquired with a temporal resolution of 8 s, lasting 12 min total. Because of using gadodiamide, cASL scan cannot be performed after K trans scan (see Note 2 ).
-
12.
Quantitative susceptibility mapping (QSM): QSM data are acquired using a 3D multi-gradient echo (MGE) sequence with the following parameters: FOV = 2.56 × 2.56 × 2.56 cm3, data matrix = 256 × 192 × 128, TE1 = 4.4 ms, echo spacing = 6.1 ms, 4 echoes, and TR = 28 ms.
3.3 Image Analysis
Image calculation and co-registration can be done using codes written in Matlab (MathWorks Inc, Natick, MA) [34, 35]. In addition to Matlab programs, we also use the STIMULATE (University of Minnesota) software for display and plotting. There are also many other free software programs available to calculate and display MRI images.
3.3.1 Map Calculations
-
1.
ADC
ADC maps with intensity in unit of mm2/s are calculated pixel by pixel by using [36, 37],
$$ \mathrm{A}\mathrm{D}\mathrm{C}=- \ln \left({S}_1/{S}_0\right)/\left({b}_1-{b}_0\right) $$where b i = γ 2 G i 2 δ 2(Δ − δ/3), ln is the natural logarithm, and S 0 and S 1 are the signal intensities obtained with b 0 and b 1, respectively. The b-value is proportional to the gradient strength (G), magnetogyric ratio (γ), duration of each gradient pulse (δ), and the time (Δ) between applications of the two gradient pulses. ADC maps are calculated at each time point.
-
2.
Fractional anisotropy (FA) :
FA can be calculated using either Matlab code or other MRI analysis toolboxes (e.g., DTIStudio, BrainVoyager). Three eigenvalues (λ 1, λ 2, and λ 3) are derived from DTI data and FA is calculated using
$$ \mathrm{F}\mathrm{A}=\frac{\sqrt{3\left({\left({\lambda}_1-\mathbb{E}\left[\lambda \right]\right)}^2+{\left({\lambda}_2-\mathbb{E}\left[\lambda \right]\right)}^2+{\left({\lambda}_3-\mathbb{E}\left[\lambda \right]\right)}^2\right)}}{\sqrt{2({\lambda}_1^2+{\lambda}_2^2+{\lambda}_3^2}} $$ -
3.
CBF
For ASL images, CBF images (S CBF) with intensity in units of ml/gram/min are calculated [38, 39] pixel by pixel using
$$ {S}_{\mathrm{CBF}}=l/{T}_1\left({S}_{\mathrm{c}}-{S}_{\mathrm{L}}\right)/\left({S}_{\mathrm{L}}+\left(2a-1\right){S}_{\mathrm{c}}\right), $$where S C and S L are signal intensities of the control and labeled images, respectively. λ—0.9 ml/g—is the partition coefficient [40]. α is the labeling efficiency which is measured to 0.75–0.9 in animal models.
For DSC-CBF calculation, the transverse relaxation rate (ΔR 2 *) is calculated using the equation ΔR 2 *(t) = −ln(S(t)/S 0)/TE, where S(t) is the signal intensity at time t, S 0 is the precontrast baseline signal intensity, and TE is the sequence echo time. A CBF map is then generated by deconvolving the change in tissue concentration over the first pass of contrast agent with an arterial input function using singular value decomposition [41, 42]. Mean transit time and cerebral blood volume can also be obtained with this analysis and they may be useful for stroke analysis. This software can be obtained from many sources.
-
4.
T 2
T 2 maps can be calculated from T 2-weighted MRI with two or more echo times (TE). When using two echoes, T 2 can be calculated directly using
$$ {T}_2=- \ln \left({S}_{\mathrm{TE}2}/{S}_{\mathrm{TE}1}\right)/\left({\mathrm{TE}}_2-{\mathrm{TE}}_1\right), $$where S TE2 and S TE1 are the signal intensities obtained with TE2 and TE1, respectively. If using more than two echoes, a linear fit needs to be used to fit
$$ \ln \left({S}_{\mathrm{TE}}\right)= \ln \left({S}_0\right)-\mathrm{T}\mathrm{E}/{T}_2, $$where S 0 is the maximum signal from the sample.
-
5.
K trans mapping [24]
The steady-state spoiled gradient echo (GRE, acquired using the 2D FLASH sequence) signal amplitude for a given TR (M TR) can be related to M 0, R 1, and α as follows:
$$ {M}_{\mathrm{TR}}={M}_0\left(r,{s}_{\mathrm{coil}}\right)\cdot \sin \alpha \frac{1- \exp \left(-\mathrm{T}\mathrm{R}\cdot {R}_1\right)}{1- \exp \left(-\mathrm{T}\mathrm{R}\cdot {R}_1\right)\cdot \cos \alpha}\cdot \exp \left(-\mathrm{T}\mathrm{E}/{T}_2^{*}\right) $$(1)where M 0 is a function of both spatial location r and coil sensitivity s coil. To minimize the R 2 * signal decay, a single-echo GRE scan is used with minimum TE and a low dose of gadolinium. As an approximation, \( \exp \left(-\mathrm{T}\mathrm{E}/{T}_2^{*}\right)\approx 1 \) is used in the subsequent calculation. A prescan module composed of three GRE scans is used to determine flip angle (α) and tissue magnetization (M 0).
For flip-angle mapping, simulations using Eq. 1 show that the ratio of GRE magnitudes at TRs of 200 and 64 ms depends strongly on α, but very weakly on T 1. Given the narrow T 1 distribution of brain tissue , a raw α (or B 1 +) map can be obtained from the ratio map with a fixed T 1 value. Assuming that α is a smooth function of location, the final α map can be obtained after smoothing.
For M 0 determination, according to Eq. 1, the GRE signal becomes less dependent on T 1 with increasing TR. With a long TR of 3000 ms, GRE magnitude depends primarily on sin(α) for small to medium flip angles (α < 45°), but very weakly on T 1. Given the normal flip angle of 30°, the actual flip angle of the brain tissue is within the range of 15–45°; therefore, M 0 can be determined from the long TR scan and the flip angle distribution as follows:
$$ {M}_0={M}_{3000\mathrm{ms}}/ \sin \alpha $$(2)Given the smooth α distribution, high-SNR M 0 map, and dynamic scans using sensitive surface coil at high field, dynamic R 1 map can be obtained using Eq. 1 with sufficient SNR.
The AIF is determined using the data and the scaling approach by Ewing and colleagues [43, 44]. Briefly, the mean AIF (AIFmean) is measured in a group of male rats (approximately 300 g) using the custom-synthesized radiolabeled Gd-DTPA [43]. Assuming that the plasma volume is 1 % and there is no BBB leakage in the contralesional side of caudate-putamen (CPU), the AIF is determined using the following scaling:
$$ \mathrm{A}\mathrm{I}\mathrm{F}(t)={\mathrm{AIF}}_{\mathrm{mean}}\cdot \left[100\cdot \underset{t=3 \min }{\overset{9 \min }{{\displaystyle \int }}}{R}_{1,\mathrm{C}\mathrm{P}\mathrm{U}}(t)\mathrm{d}t\right]/\left[\underset{t=3 \min }{\overset{9 \min }{{\displaystyle \int }}}{\mathrm{AIF}}_{\mathrm{mean}}\mathrm{d}t\right] $$(3)The R 1 and the AIF are then used to fit the extended Kety model:
$$ {C}_t(t)={K}^{\mathrm{trans}}\underset{\tau =0}{\overset{t}{{\displaystyle \int }}}{C}_{\mathrm{p}}\left(\tau \right){e}^{-{k}_{\mathrm{ep}}\left(t-\tau \right)}d\tau +{\nu}_{\mathrm{p}}{C}_{\mathrm{p}}(t) $$(4)where C t(t) and C p(t) are tissue and plasma gadolinium concentrations, and k ep is the reversible mass transfer coefficient. In this study, the R 1 and scaled AIF values are directly used for data fitting without further conversion to concentrations using the relativity of contrast agent. Since it is difficult to obtain acceptable K trans maps by simultaneously fitting all three parameters, we use the model selection approach by Ewing and colleagues [44] to select a simpler model that could sufficiently describe the dynamic contrast change. Data is fit to the extended Kety model with the two following assumptions as described by Ewing and colleagues [44]:
Irreversible leakage (two-parameter model, or Model 2):
$$ {K}^{\mathrm{trans}}>0,{k}_{\mathrm{ep}}=0 $$(5)Reversible leakage (three-parameter model, or Model 3):
K trans > 0, k ep > 0
For model selection, the irreversible model is selected, unless the reversible model yields a statistically significant better fit. The cutoff criteria use the F-statistic, which can be calculated using the summed squared residues (SSE) and the number of samples (N) as follows:
$$ F=\left[\left({\mathrm{SSE}}_3-{\mathrm{SSE}}_2\right)/1\right]/\left[{\mathrm{SSE}}_3/\left(N-3\right)\right] $$(6)where the subscript represents the corresponding model. The final selection mask is determined as
$$ {M}_{\mathrm{select}}=F>{F}_0 $$(7)The threshold for F-statistic (F 0) is set as 10 (P < 0.05). The final K trans map is then determined as
$$ {K}_{\mathrm{final}}^{\mathrm{trans}}={K}_{\mathrm{Model}1}^{\mathrm{trans}}\cdot \left(1-{M}_{\mathrm{select}}\right)+{K}_{\mathrm{Model}2}^{\mathrm{trans}}\cdot {M}_{\mathrm{select}} $$(8)All the calculations are performed using Matlab R2011b (Mathworks, Natick, MA).
-
6.
Quantitative susceptibility mapping:
QSM is performed using the STI Suite [45]. Briefly, the brain image is reconstructed with 3D fast Fourier transform. The complex data is separated into magnitude and phase. The magnitude image is used for the extraction of the brain tissue . The phase images are unwrapped using Laplacian-based unwrapping [46] and summed. The background phase is removed using the V-SHARP method [47]. The tissue susceptibility is determined using the LSQR method [48]. The resulting magnetic susceptibility values are directly used for comparison [49].
3.3.2 Abnormal Tissue Volume Analysis
Abnormal tissue volume can be determined using either manually ROI drawing or threshold methods. Manually region of interest (ROI) drawing method usually needs more than two data analyzers to manually delineate the border of the abnormal tissue and then count the number of pixels inside the ROI. Commonly used threshold method is using the mean value ± 2 standard deviations of the homologous contralesional region (see Note 3 ). Depending on the data, it could be two or three standard deviations (see Note 4 ). In TBI abnormal tissue volume analysis, ADC, CBF , FA, T 2, and K trans can all be analyzed using these two methods.
3.3.3 Hypercapnic Responses
Images obtained during the transition period between baseline and stimulus onset (30 s for CO2 challenge) are discarded. BOLD images are obtained from the control (non-labeled) images of the CBF measurements. BOLD and CBF magnitude and percent changes relative to baselines are calculated on a pixel-by-pixel basis.
3.4 Additional Advanced Analysis
3.4.1 Data Co-registration
Image maps of individual subjects are co-registered across time points via the application of a transformation matrix generated by QuickVol and MRIAnalysisPak software [35, 50].
3.4.2 Spatial-temparal Changes of MRI Measures (ADC, FA, CBF, T 2 , K trans, and Hypercapnic Responses)
Three regions of interest (ROIs) are defined along the ipsilesional cortex, along with three ROIs in homologous regions of the contralesional hemisphere. The same ROIs are used to tabulate the MRI measures across all time points using Stimulate software (University of Minnesota). Values of the ipsilesional ROI are normalized with respect to those of the contralesional ROI.
3.4.3 Quantification of White Matter Damage
To evaluate MRI contrast along the white matter tracts and to eliminate the subjectivity of manual region of interest selection, we project the maximum values of magnetic susceptibility, and the minimum values of DTI FA along the corpus callosum. Such an approach is used to minimize the potential partial volume effect due to the small fraction of white matter in rodent brains. The projected values are compared across different time points.
4 Notes
-
1.
Following the TBI impact, the cranial opening needs to be sealed with bone wax and then the scalp sutured closed. The blood, if any, needs to be cleared. Saline should be injected under the skin to facilitate removal of air pockets between the scalp and the skull to minimize artifacts during MRI acquisition. These steps (using bone wax and saline) are very important to avoid MRI artifacts.
-
2.
Gd-DTPA or gadodiamide will change the relaxation time (T 1 and T 2) of blood and tissue. Therefore CBF will not be accurately obtained using cASL after using Gd-DTPA or gadodiamide.
-
3.
In TBI, some parameters can change in the positive or negative direction at the same time due to heterogeneity within the tissue. For example, both decreased and increased ADC can be observed in acute TBI. When calculating abnormal ADC tissue volume, both types of tissues need to be counted.
-
4.
The variances of different parameters are different. For small variance data, the threshold needs to use mean value plus higher times of standard deviations (SD). For example, for T 2 maps, two SDs would be good. For ADC, which has small variance, it may be needed to use mean plus three SDs as the threshold.
References
Nortje J, Menon DK (2004) Traumatic brain injury: physiology, mechanisms, and outcome. Curr Opin Neurol 17:711–718
Werner C, Engelhard K (2007) Pathophysiology of traumatic brain injury. Br J Anaesth 99:4–9
Blennow K, Hardy J, Zetterberg H (2012) The neuropathology and neurobiology of traumatic brain injury. Neuron 76:886–899
Gardner A, Kay-Lambkin F, Stanwell P, Donnelly J, Williams WH, Hiles A, Schofield P, Levi C, Jones DK (2012) A systematic review of diffusion tensor imaging findings in sports-related concussion. J Neurotrauma 29:2521–2538
Albensi BC, Knoblach SM, Chew BGM, O’Reilly MP, Faden AI, Pekar JJ (2000) Diffusion and high resolution MRI of traumatic brain injury in rats: time course and correlation with histology. Exp Neurol 162:61–72
Iwamoto Y, Yamaki T, Murakami N, Umeda M, Tanaka C, Higuchi T, Aoki I, Naruse S, Ueda S (1997) Investigation of morphological change of lateral and midline fluid percussion injury in rats, using magnetic resonance imaging. Neurosurgery 40:163–167
Van Putten HP, Bouwhuis MG, Muizelaar JP, Lyeth BG, Berman RF (2005) Diffusion-weighted imaging of edema following traumatic brain injury in rats: effects of secondary hypoxia. J Neurotrauma 22:857–872
Ito J, Marmarou A, Barzo P, Fatouros P, Corwin F (1996) Characterization of edema by diffusion-weighted imaging in experimental traumatic brain injury. J Neurosurg 84:97–103
Barzo P, Marmarou A, Fatouros P, Hayasaki K, Corwin F (1997) Contribution of vasogenic and cellular edema to traumatic brain swelling measured by diffusion-weighted imaging. J Neurosurg 87:900–907
Liu AY, Maldjian JA, Bagley LJ, Sinson GP, Grossman RI (1999) Traumatic brain injury: diffusion-weighted MR imaging findings. Am J Neuroradiol 20:1636–1641
Kou ZF, Wu Z, Tong KA, Holshouser B, Benson RR, Hu JN, Haacke EM (2010) The role of advanced MR imaging findings as biomarkers of traumatic brain injury. J Head Trauma Rehabil 25:267–282
Rutgers DR, Toulgoat F, Cazejust J, Fillard P, Lasjaunias P, Ducreux D (2008) White matter abnormalities in mild traumatic brain injury: a diffusion tensor imaging study. Am J Neuroradiol 29:514–519
Inglese M, Makani S, Johnson G, Cohen BA, Silver JA, Gonen O, Grossman RI (2005) Diffuse axonal injury in mild traumatic brain injury: a diffusion tensor imaging study. J Neurosurg 103:298–303
Nakayama N, Okumura A, Shinoda J, Yasokawa YT, Miwa K, Yoshimura SI, Iwama T (2006) Evidence for white matter disruption in traumatic brain injury without macroscopic lesions. J Neurol Neurosur Psychiat 77:850
Mac Donald CL, Dikranian K, Bayly P, Holtzman D, Brody D (2007) Diffusion tensor imaging reliably detects experimental traumatic axonal injury and indicates approximate time of injury. J Neurosci 27:11869–11876
van de Looij Y, Mauconduit F, Beaumont M, Valable S, Farion R, Francony G, Payen JF, Lahrech H (2012) Diffusion tensor imaging of diffuse axonal injury in a rat brain trauma model. NMR Biomed 25:93–103
Arfanakis K, Haughton VM, Carew JD, Rogers BP, Dempsey RJ, Meyerand ME (2002) Diffusion tensor MR imaging in diffuse axonal injury. Am J Neuroradiol 23:794–802
Barbier EL, Lamalle L, Decorps M (2001) Methodology of brain perfusion imaging. J Magn Reson Imaging 13:496–520
Calamante F, Thomas DL, Pell GS, Wiersma J, Turner R (1999) Measuring cerebral blood flow using magnetic resonance imaging techniques. J Cereb Blood Flow Metab 19:701–735
Baskaya MK, Rao AM, Dogan A, Donaldson D, Dempsey RJ (1997) The biphasic opening of the blood-brain barrier in the cortex and hippocampus after traumatic brain injury in rats. Neurosci Lett 226:33–36
Chodobski A, Zink BJ, Szmydynger-Chodobska J (2011) Blood-brain barrier pathophysiology in traumatic brain injury. Transl Stroke Res 2:492–516
Adelson PD, Whalen MJ, Kochanek PM, Robichaud P, Carlos TM (1998) Blood brain barrier permeability and acute inflammation in two models of traumatic brain injury in the immature rat: a preliminary report. Acta Neurochir Suppl 71:104–106
Dempsey RJ, Baskaya MK, Dogan A (2000) Attenuation of brain edema, blood-brain barrier breakdown, and injury volume by ifenprodil, a polyamine-site N-methyl-D-aspartate receptor antagonist, after experimental traumatic brain injury in rats. Neurosurgery 47:399–404, discussion 404-396
Li W, Long JA, Watts LT, Jiang Z, Shen Q, Li YX, Duong TQ (2014) A quantitative MRI method for imaging blood-brain barrier leakage in experimental traumatic brain injury. PLoS One 9:e114173
Cernak I (2005) Animal models of head trauma. NeuroRx 2:410–422
Xiong Y, Mahmood A, Chopp M (2013) Animal models of traumatic brain injury. Nat Rev Neurosci 14:128–142
Watts LT, Long JA, Chemello J, Van Koughnet S, Fernandez A, Huang SL, Shen Q, Duong TQ (2014) Methylene blue is neuroprotective against mild traumatic brain injury. J Neurotrauma 31:1063–1071
Long JA, Watts LT, Chemello J, Huang SL, Shen Q, Duong TQ (2015) Multiparametric and longitudinal MRI characterization of mild traumatic brain injury in rats. J Neurotrauma 32:598–607
Long JA, Watts LT, Li W, Shen Q, Muir ER, Huang S, Boggs RC, Suri A, Duong TQ (2015) The effects of perturbed cerebral blood flow and cerebrovascular reactivity on structural MRI and behavioral readouts in mild traumatic brain injury. J Cereb Blood Flow Metab 35:1852
Talley Watts L, Long JA, Manga VH, Huang S, Shen Q, Duong TQ (2015) Normobaric oxygen worsens outcome after a moderate traumatic brain injury. J Cereb Blood Flow Metab 35:1137–1144
Talley Watts L, Shen Q, Deng S, Chemello J, Duong TQ (2015) Manganese-enhanced magnetic resonance imaging of traumatic brain injury. J Neurotrauma 32:1001–1010
Watts LT, Long JA, Boggs RC, Manga H, Huang S, Shen Q, Duong TQ (2016) Methylene blue improves lesion volume, multi-parametric quantitative MRI measurements, and behavioral outcome following TBI. J Neurotrauma 33:194
Deitch AD, Moses MJ (1957) The Nissl substance of living and fixed spinal ganglion cells. II. An ultraviolet absorption study. J Biophys Biochem Cytol 3:449–456
Shen Q, Ren H, Cheng H, Fisher M, Duong TQ (2005) Functional, perfusion and diffusion MRI of acute focal ischemic brain injury. J Cereb Blood Flow Metab 25:1265–1279
Liu ZM, Schmidt KF, Sicard KM, Duong TQ (2004) Imaging oxygen consumption in forepaw somatosensory stimulation in rats under isoflurane anesthesia. Magn Reson Med 52:277–285
Stejskal EO, Tanner JE (1965) Spin diffusion measurements: spin echoes in the presence of a time-dependent field gradient. J Chem Phys 42:288–292
Shen Q, Meng X, Fisher M, Sotak CH, Duong TQ (2003) Pixel-by-pixel spatiotemporal progression of focal ischemia derived using quantitative perfusion and diffusion imaging. J Cereb Blood Flow Metab 23:1479–1488
Silva AC, Lee S-P, Yang C, Iadecola C, Kim S-G (1999) Simultaneous blood oxygenation level-dependent and cerebral blood flow functional magnetic resonance imaging during forepaw stimulation in the rat. J Cereb Blood Flow Metab 19:871–879
Duong TQ, Silva AC, Lee S-P, Kim S-G (2000) Functional MRI of calcium-dependent synaptic activity: cross correlation with CBF and BOLD measurements. Magn Reson Med 43:383–392
Herscovitch P, Raichle ME (1985) What is the correct value for the brain-blood partition coefficient for water? J Cereb Blood Flow Metab 5:65–69
Ostergaard L, Sorensen AG, Kwong KK, Weisskoff RM, Gyldensted C, Rosen BR (1996) High resolution measurement of cerebral blood flow using intravascular tracer bolus passages. Part II: Experimental comparison and preliminary results. Magn Reson Med 36:726–736
Ostergaard L, Weisskoff RM, Chesler DA, Gyldensted C, Rosen BR (1996) High resolution measurement of cerebral blood flow using intravascular tracer bolus passages. Part I: Mathematical approach and statistical analysis. Magn Reson Med 36:715–725
Nagaraja TN, Karki K, Ewing JR, Divine GW, Fenstermacher JD, Patlak CS, Knight RA (2010) The MRI-measured arterial input function resulting from a bolus injection of Gd-DTPA in a rat model of stroke slightly underestimates that of Gd-[14C]DTPA and marginally overestimates the blood-to-brain influx rate constant determined by Patlak plots. Magn Reson Med 63:1502–1509
Ewing JR, Bagher-Ebadian H (2013) Model selection in measures of vascular parameters using dynamic contrast-enhanced MRI: experimental and clinical applications. NMR Biomed 26:1028–1041
Li W, Avram AV, Wu B, Xiao X, Liu C (2014) Integrated Laplacian-based phase unwrapping and background phase removal for quantitative susceptibility mapping. NMR Biomed 27:219–227
Langkammer C, Schweser F, Krebs N, Deistung A, Goessler W, Scheurer E, Sommer K, Reishofer G, Yen K, Fazekas F, Ropele S, Reichenbach JR (2012) Quantitative susceptibility mapping (QSM) as a means to measure brain iron? A post mortem validation study. Neuroimage 62:1593–1599
Wu B, Li W, Guidon A, Liu CL (2012) Whole brain susceptibility mapping using compressed sensing. Magn Reson Med 67:137–147
Li W, Wu B, Liu CL (2011) Quantitative susceptibility mapping of human brain reflects spatial variation in tissue composition. Neuroimage 55:1645–1656
Li W, Wu B, Batrachenko A, Bancroft-Wu V, Morey RA, Shashi V, Langkammer C, De Bellis MD, Ropele S, Song AW, Liu C (2014) Differential developmental trajectories of magnetic susceptibility in human brain gray and white matter over the lifespan. Hum Brain Mapp 35:2698–2713
Schmidt KF, Ziu M, Schmidt NO, Vaghasia P, Cargioli TG, Doshi S, Albert MS, Black PM, Carroll RS, Sun Y (2004) Volume reconstruction techniques improve the correlation between histological and in vivo tumor volume measurements in mouse models of human gliomas. J Neurooncol 68:207–215
Acknowledgements
This work is supported in part by NIH/NINDS R01 NS45879, a TL1 and KL2 TR001118, and Mike Hogg Fund via the Clinical Translational Science Awards (CTSA, parent grants UL1TR000149, TL1TR001119, and KL2TR001118). We thank our former and current colleagues who have participated on these TBI projects.
Author information
Authors and Affiliations
Corresponding authors
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer Science+Business Media New York
About this protocol
Cite this protocol
Shen, Q., Watts, L.T., Li, W., Duong, T.Q. (2016). Magnetic Resonance Imaging in Experimental Traumatic Brain Injury. In: Kobeissy, F., Dixon, C., Hayes, R., Mondello, S. (eds) Injury Models of the Central Nervous System. Methods in Molecular Biology, vol 1462. Humana Press, New York, NY. https://doi.org/10.1007/978-1-4939-3816-2_35
Download citation
DOI: https://doi.org/10.1007/978-1-4939-3816-2_35
Published:
Publisher Name: Humana Press, New York, NY
Print ISBN: 978-1-4939-3814-8
Online ISBN: 978-1-4939-3816-2
eBook Packages: Springer Protocols