Abstract
Traumatic brain injury (TBI) has been named the most complex disease in the most complex organ of the body. It is the most common cause of death and disability in the Western world in people <40 years old and survivors commonly suffer from persisting cognitive deficits, impaired motor function, depression and personality changes. TBI may vary in severity from uniformly fatal to mild injuries with rapidly resolving symptoms and without doubt, it is a markedly heterogeneous disease. Its different subtypes differs in their pathophysiology, treatment options and long-term consequences and to date, there are no pharmacological treatments with proven clinical benefit available to TBI patients. To enable development of novel treatment options for TBI, clinically relevant animal models are needed. Due to their availability and low costs, numerous rodent models have been developed which have substantially contributed to our current understanding of the pathophysiology of TBI. The most common animal models used in laboratories worldwide are likely the controlled cortical impact (CCI) model, the central and lateral fluid percussion injury (FPI) models, and weight drop/impact acceleration (I/A) models. Each of these models has inherent advantages and disadvantages; these need to be thoroughly considered when selecting the rodent TBI model according to the hypothesis and design of the study. Since TBI is not one disease, refined animal models must take into account the clinical features and complexity of human TBI. To enhance the possibility of establishing preclinical efficacy of a novel treatment, the preclinical use of several different experimental models is encouraged as well as varying the species, gender, and age of the animal. In this chapter, the methods, limitations, and challenges of the CCI and FPI models of TBI used in rodents are described.
Access provided by CONRICYT – Journals CONACYT. Download protocol PDF
Similar content being viewed by others
Key words
- Traumatic brain injury
- Controlled cortical impact (CCI)
- Fluid percussion injury (FPI)
- Rats
- Mice
- Neurodegeneration
- Outcome
1 Introduction
Traumatic brain injury (TBI) has been recognized as a silent epidemic and is considered by the World Health Organization to be a health threat at the order of HIV and malaria. Recent epidemiological data suggest that the number of TBI victims worldwide is increasing [1–3] and survivors of TBI commonly suffer from persistent functional deficits, including personality changes, motor impairment and cognitive problems, leading to an impaired capacity for work and a reduced quality of life. Current treatment options include optimized prehospital stabilization, rapid decompressive surgery when needed, neurocritical care and frequently prolonged neurorehabilitation. Despite extensive preclinical and clinical studies for several decades, there is still a lack of pharmacological alternatives [4]. The enormous heterogeneity of TBI has been noted in several recent overviews [5] which is further exacerbated by individual injury factors, age and gender issues and perhaps also the genetics and/or epigenetics of the individual patient. The clinical reality of TBI makes the discovery of a single treatment or pharmacological tool effective in each of the TBI subtypes highly unlikely. Thus, the preclinical TBI research aiming to develop novel pharmacological compounds or rehabilitative strategies faces a challenge when aiming to mimic the clinical setting and it is crucial that clinically relevant TBI models are used. The question is then—how many animal models of TBI are needed to cover the clinical aspects of TBI?
To date, the search of “traumatic brain injury ” AND “animal model” yields 159 hits on PubMed. Several models for repetitive, blast, penetrating, focal and diffuse TBI combined with various secondary insults such as hypotension and hypoxia have been developed [6–11]. Although TBI models developed for higher-order species such as the miniature swine and the primate models are available, rodent models will likely continue to be used in the vast majority of TBI research due to their accessibility and low costs. It may be argued that the task of making rodent models more clinically relevant is not to develop even more animal models—instead it is the refinement of the existing ones [12, 13]. Thus, the selected study treatment may be tested in a range of other relevant parameters such as strain, species, sex, and age of the animal. The use of a rather limited number of animal models also carries the advantage of enabling comparisons among different laboratories. As such, the controlled cortical impact (CCI) and the fluid percussion injury (FPI) models have been used in both rats and mice and all have the advantage of being widely used and mimicking certain aspects of human TBI.
The fluid percussion injury, initially established in the rabbit [14], was in 1987 adopted for use in the rat by Dixon et al., [15], the midline FPI model, and modified in 1989 by McIntosh et al., [16] who established the lateral FPI model. Despite presumed difficulties, both the lateral [17] and recently, the central (midline) fluid percussion model [18, 19], could successfully be adopted to mice. The basic principle behind this TBI model is that a brief pressure pulse is transmitted to the exposed dura, allowing for a degree of brain displacement resulting in cortical, hippocampal, and brain stem injury as well as widespread axonal injury in brain regions such as the corpus callosum, the fimbriae and the brain stem. As described in the following paragraphs below, the brain injury and behavioral deficit created will vary depending on the location of the craniectomy and the delivery and force of the pressure pulse. Two common types of FPI models are in common use—the lateral FPI model [16, 20, 21] where the pressure pulse is delivered over one hemisphere and the central/midline CPI model [15] where the pulse is delivered over the midline, resulting in different brain injuries and behavioral deficits.
The controlled cortical impact (CCI) model of TBI, first used in the ferret [22], was then adopted for use in the rat [23] and then to the mouse [24]. This model uses a pneumatically or electromagnetically [25] driven piston striking (most commonly) the exposed dura allowing for brain penetration of a predetermined depth at a predetermined velocity. This model predominately produces a focal TBI although diffuse neurodegeneration may be observed throughout the rodent brain extending also into the contralateral hemisphere [26]. Although not identical with CCI, the weight-drop model originally developed by Feeney et al., [27], used by many labs including ours [28], reproducibly resulted in a focal contusion extending into the ipsilateral hippocampus when a weight was dropped from a predetermined height onto the exposed dura with the head of the rodent fixed. Arguably, this model may be less precise and adjustable than the CCI, despite the commonly used term “controlled cortical contusion model”, and it is less commonly used to date.
Due to the intrinsic differences between rodents and man, a TBI model in the rat or the mouse may never replicate all aspects of the immense complexity of human TBI, particularly with regards to the complex cognitive and behavioral disturbances observed in TBI patients. In order to mimic the clinical situation to the extent possible, a thorough understanding of the behavioral consequences of the TBI models is crucial as well [29]. One example of such a strategy is the evaluation of the long-term clinical problem of post-traumatic epilepsy and both the CCI and lateral FPI models were shown to cause delayed seizures post-injury [30]. The commonly used CCI and FPI TBI models, in the view of this author, may be the most clinically relevant ones available to date, and their histological and behavioral consequences have resemblance to certain aspects of human TBI and their techniques the as well as their advantages and disadvantages are outlined in the following paragraphs.
2 Materials
2.1 Animals
We use Sprague-Dawley male rats at a weight of 350–400 g (9–12 weeks of age, Taconic M&B laboratory, Ry, Denmark) and C57BL/6J mice at a weight of 25–28 g (age 9–12 weeks old; supplied by Taconic, Denmark). The animals should be housed in a colony maintained by trained staff including regular surveillance for common viruses known to potentially infect rodent facilities. All scientists involved in animal research must undergo authorized training in animal welfare, handling and ethics and each study must be approved by the animal ethics board and follow the local and national rules and regulations of animal experiments. Any measure to reduce stress and suffering to the animal is taken (see Notes 1 – 5 ). The animals are housed at 24 °C in cages with three to five mice or two rats per cage with free access to food and water in a 12-h light/dark cycle, and kept in the colony for a minimum of 1 week prior to any surgical procedures.
2.2 Surgical Setup
-
1.
A surgical area, preferably sheltered from other lab spaces, designed and devoted to animal surgery is used. The experimenter involved in the surgery should use a clean lab coat, a surgical face mask, foot covering and gloves. A set of clean, sharpened surgical tools should be available for smooth and controlled surgery.
-
2.
The setup for volatile anesthesia requires specialized equipment including vaporizers. Leakage of volatile gases readily occurs and poses an occupational hazard to the investigator and scavenging systems must be in place and be regularly tested by the responsible authorities and all staff must be trained accordingly. Such scavenging systems for reducing exposure to the researcher is paramount and may include carbon filters, fume hoods or, preferably, a vacuum setup connected to an exhaust system to minimize the risk of inadvertent exposure of volatile anesthetics (see Notes 6 and 7 ).
-
3.
A heating pad, coupled to a rectal probe (CMA150, CMA, Stockholm, Sweden), is needed to maintain the core temperature of the animal at 37 °C and is positioned under the animal during surgery. The body of the animal is covered by towels to reduce hypothermia.
-
4.
A stereotaxic head holder (Kopf Instruments, Tujunga, California, USA) including blunt ear pins to avoid ear drum penetration (both rats and mice) and a snout clamp is used for head fixation.
-
5.
A surgical microscope and a light source is needed.
-
6.
An electric razor for minimal hair trimming is used. The area is sterilized by using sterile swabs with 70 % alcohol and bupivacaine at 5 mg/mL is used for local anesthesia in the scalp (Marcain, AstraZeneca, Sweden).
-
7.
Polyethylene tubing for arterial catheter and/or venous lines if needed (rat; PE 50, Becton Dickinson, Franklin Lakes, NJ, USA) and for intubation (rat) if needed (PE 205, Becton Dickinson).
-
8.
Artificial tear lubricants (Viscotears, Novartis, Inc., Basel, Switzerland) is carefully placed on the cornea of the animal to keep them from drying during surgery.
-
9.
A pencil is needed to carefully mark the exact location of the craniotomy.
-
10.
Trephines for mice and rats, preferably attached to a dental drill, or a 1.0 mm diamond drill head attached to the dental drill is needed. Q-tips and bone wax may be used to control minor bleedings by gentle pressure.
2.3 Fluid Percussion Brain Injury (FPI)
The basic idea of FPI is that a short pressure pulse is delivered to the brain via the intact dura mater, resulting in a rapid rise in intracranial pressure [31] and a degree of brain displacement, which leads to brain injury by cell death, opening of the blood-brain barrier , axonal injury and a neuroinflammatory response [20]. The pressure pulse is created by a pendulum striking a piston at the proximal end of a fluid-filled cylinder and saline is being rapidly injected into the closed cranial cavity of the animal (Fig. 1). The severity of injury is regulated by varying the height from which the pendulum is released, which results in variations of the pressure pulse transmitted to the rodent.
Cartoon of the basic setup for fluid percussion brain injury. (a) The craniectomy for central (midline) FPI is centered over the sagittal suture midway between bregma and lambda. The lower image shows the corresponding impact area of the rodent brain. (b) When the pendulum (right) is released from a predetermined height, it will strike the end of a Plexiglas cylinder filled with isotonic saline. The impact creates a pressure wave of ca. 20 ms which is transmitted to the brain of the rodent using the techniques described in coming sections. The rodent is held by the researcher’s hand and gently attached to the distal end of the cylinder via the Luer-Lok setup cemented onto the skull of the rodent, over the craniectomy. Note the transducer located at the distal end of the cylinder, reading the pressure changes which is displayed on a computer screen. (c) To improve the drilling for the craniectomy, we use a trephine attached to a dental drill at 5000 rpm. For best results of surgery, including control of small bleedings and securing hat the dura is intact, a surgical microscope is preferred
-
1.
The FPI device consists of a Plexiglas cylinder (Fig. 1) filled with physiologic saline and at its distal end, there is a transducer measuring the extracranial pressure wave and then a male Luer-Lok fitting enabling it to be locked on the trauma cap attached to the rodent’s skull for delivering of the pressure pulse. The FPI device needs regular maintenance, including cleaning of the cylinder and replacing the saline as well as lubricating the plunger and its O-rings using for example petroleum jelly or similar (Renolit, Mannheim, Germany). In modern FPI systems, there is less need for calibrating the pressure output from the transducer and amplifier. The pressure is typically measured in atmospheres of pressure per square inch (PSI) where one atmosphere = 14.7 PSI.
-
2.
A hub of a needle needs to be mounted over the craniectomy (Fig. 2) and this injury hub is created from a 23G needle (Becton Dickinson, USA) with a razor blade or a pencil sharpener. Its lower end needs to be angled to be closely fitted into the craniectomy.
Fig. 2 In vivo, “real-life” central fluid percussion injury in the mouse. (a) The surgical draping has been removed to better display the setup and the surgical area. Note the craniectomy (Cr) and the arrow pointing to the sagittal sinus after removal of the bone. The head is firmly held in place by blunt ear pins and by a snout clamp. (b) Lateral view. The mouse is placed on a heating pad to maintain core temperature, which is monitored. Note the homemade nose cone delivering volatile anesthetics. The hub of a needle is placed over the craniectomy, held in place by cement (Ce). The hub is then filled with saline (arrow) and checked that it remains in place securing the tight closure of this now fluid-filled space. (c) Typical reading of the pressure wave from the transducer. In our experience, the peak pressure wave in mice may show some irregularities despite taking all the measures described in the text. In rats, this peak is typically smoother without the “edges” shown in the mouse. (d) Close-up of the transducer. It is crucial that this part is devoid of air and this area need to be flushed with saline (S) prior to each injury and the pressure pulse controlled
-
3.
Dental cement (Dentalon Plus, Heraeus Kulzer GmbH, Hanau, Germany, Fig. 2) and two flat-ended anchoring screws (rat) is used to anchor the hub over the craniectomy as well as a strong adhesive (Loctite Precision Super-glue, Loctite, Westlake, Ohio, USA).
2.4 Controlled Cortical Impact
Following a craniotomy centered over one hemisphere, the idea of the CCI model is that a piston will deliver a force to the exposed and intact dura, allowing rapid deformation of the underlying brain and resulting in necrotic and apoptotic cell death. Although this model is clearly a focal TBI model, it also has diffuse injury components [26].
-
1.
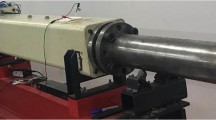
We use a pneumatically controlled CCI-device (VCU Biomedical Engineering Facility, Richmond, Virginia, USA) with a flat tip (Fig. 3).
Fig. 3 CCI procedure. Following cleaning of the scalp, a midline incision is made. Following craniotomy made with a dental drill, a 5 × 6 mm (rats) or 4 × 4 mm (mice) craniotomy centered over the right parietal cortex is made. The piston (left) is gently attached to the exposed dura. To the right, the CCI apparatus including the micrometer gauge is shown
-
2.
To produce the craniotomy, a prefabricated plastic plate may be used to aid in drilling, although it is not used in our lab.
3 Methods
3.1 Animals and Surgery
-
1.
Rodents can be of any age, weight and strain. To reduce the stress reactions associated with the experiments, we recommend pre-injury handling of the animals for five min twice daily for 2 days before taking part in any behavioral experiments (see Note 4 ).
-
2.
The weight and welfare of the animals must be monitored pre- and post-injury, at least daily for the first three post-injury days, then a minimum of twice per week. Animals losing more than ca 15 % body weight following the injury should be excluded from the study (see Note 5 ).
-
3.
Carefully chose the anesthetics and remember that they all influence the results of the injury in one way or the other. Common choices are volatile anesthetics such as isoflurane or halothane with sodium pentobarbital or xylazine/ketamine used as alternatives (see Note 6 and 7 ). A combination of these anesthetic agents may be used, for instance by using sodium pentobarbital to prepare for the injury. Then, after a 24 h recovery, injury may be induced using for example isoflurane or halothane anesthesia [19].
-
4.
We prefer volatile anesthesia where the animal is induced in a chamber with 4 % isoflurane in air and then moved to the stereotaxic frame where a mixture of isoflurane (1.2–1.4 %) and N2O/O2 (70/30 %) is delivered through a nose cone or, in long experiments such as when using intracerebral microdialysis, following intubation using PE 205 tubing (Becton Dickinson) attached to a rodent ventilator (Ugo Basile, Comerio, Italy).
-
5.
In rats, when for example electrophysiological experiments are conducted, xylazine in combination with ketamine is an alternative anesthetic option. We use a 1:6 mixture of xylazine (Rompun Vet, 20 mg/mL; Bayer Animal Health, Lyngby, Denmark) and ketamine (Ketaminol Vet, 50 mg/mL, Intervet Int., Boxmeer, the Netherlands), the mixture administered at a volume of 0.14 mL/100 g body weight intramuscularly into the right thigh. When needed, an i.m. supplemental dose of 0.2 mL of ketamine is used [32], see Note 6 .
-
6.
Intraperitoneal administration of 60 mg/kg sodium pentobarbital anesthesia is common particularly in rats where the duration from a single injection is approximately 60–90 min. The depth of anesthesia may be assessed by for example the toe-pinch reflexes prior to the incision and surgical procedures.
-
7.
The animal is then positioned in a stereotaxic system with the head fixed with blunt ear pins and a bite plate/snout clamp firmly fixing the head. In accordance with the limited shaving used in clinical neurosurgery, we only trim the hair of the rodent immediately prior to incision. The scalp is anesthetized at the incision site using bupivacaine (Marcain, AstraZeneca, Sweden) applied subcutaneously.
-
8.
Physiological parameters such as blood gases (pO2, pCO2), blood pH or arterial blood pressure can be measured invasively using for example tail or femoral artery cannulations and heparinized blood samples repeatedly analyzed using appropriate equipment during the procedure. The evaluations of these physiological parameters should particularly be considered when prolonged anesthesia is used, e.g., for experiments using intracerebral microdialysis [28], and if a pharmacological compound is evaluated.
-
9.
For all TBI models described in this chapter, a midline scalp incision is made from between the eyes to the neck using a scalpel. After the scalp is reflected, the fascia is scraped from the skull to the crista temporalis with a sharp forceps.
-
10.
Uninjured, sham animals undergo all of the procedures with the exception of being subjected to the actual fluid pulse or piston impact. For most TBI research, is recommended that naïve animals are also included [33].
-
11.
Although clinical experience suggests that pain from a scalp incision as used in these TBI models is relatively short-lasting, post-operative analgesia may be required and also frequently mandated by the animal ethics committee. Although many analgesic compounds may influence the pathophysiology of TBI, opioids such as buprenorphine are commonly used (see Note 8 ).
3.2 Lateral and Midline (Central) Fluid Percussion Injury
-
1.
After the head is fixed in the stereotaxic frame and the scalp has been reflected, a craniotomy is made which is 4.8 mm (rats) or 3.0 mm (mice) for both FPI models. In central (cFPI) models, extreme caution must be taken not to injury the sagittal sinus vessel (Figs. 1 and 2). Carefully elevate the bone flap, which may be slightly adherent towards the midline and gently separate the dura from the bone using a microspatula. Inspect the dura, it must be intact and if it is not, the animal should be excluded from further analysis. Carefully stop any bleeding from the bone edges, typically sufficient with gentle pressure from a Q-tip although a small amount of bone wax may occasionally be needed (see Note 9 ).
-
2.
The craniotomy is for lateral FPI placed over the left parietal cortex, the medial edge 1 mm (mice) to 2 mm (rats) from the midline. For central FPI, it is placed at the midline over the superior sagittal sinus, midway between bregma and lambda (Figs. 1 and 2).
-
3.
Anterior to the bregma and immediately posterior to the lambda, two injury screws with flat distal ends are placed (in rats) lateral to the midline to anchor the cement (see below). The skull bone in mice is too thin to allow for the placement of injury screws.
-
4.
The injury hub, “the trauma cap”, is carefully placed over the craniectomy by holding it with small forceps and secured using Super-glue placed on the bony edges of the craniectomy. Particularly in mice, the process of avoiding glue on the dura is simplified by placing glue around the lower edges of the cap prior to placing it over the craniectomy. It is of paramount importance that glue is not placed on the dura and/or that is obstructs the opening of the trauma cap—this will markedly attenuate the pressure pulse delivered to the brain of the animal.
-
5.
Using a small plastic cup, a semifluid dental acrylic (Dentalon Plus) solution is mixed. Use a 1 cc syringe to withdraw the solution and to place it over the craniectomy site covering and securing the injury screws and trauma cap. It is imperative that the cement gets solid prior to induction of the injury.
-
6.
An important step is filling of the trauma cap with 37 °C saline and this saline needs to stay in the cap (Fig. 2). If the fluid levels sinks, this indicated incomplete closure between the cap and the bony edges.
-
7.
Prime the FPI device by releasing the pendulum and verifying a smooth curve on the reading from the transducer prior to inducing the trauma (Fig. 2). If the curve is jagged, injection of saline back and forth with a syringe attached to the transducer (Fig. 2) may clear the air from the system and improve the pressure reading.
-
8.
Reduce the isoflurane and when the animals starts breathing more shallowly, the animal is ready for trauma since injuring the animal at a surgical plane of anesthesia may cause excessive mortality. The animal is placed towards the male Luer-Lok end of the FPI device, ensuring that there is a continuous saline pillar by injecting saline over the injury cap when placing the animal towards the Luer-Lok. The animal is held firmly without compromising breathing, the head supported against the FPI device.
-
9.
When the pendulum is released and the brain injury produced, there is commonly brief seizure-like motor activity/tonic posturing and an apnea. The pressure of the pulse must be recorded. We use a cutoff limit of 60s apnea for both mice and rats, if it is longer we exclude the animal from the study since we cannot rule out additional hypoxia which could be a confounding variable. Since the post-injury apnea is an important indicator of injury severity, absence of apnea may imply an insufficient injury. Immediately after the injury, the animal should be placed on its back and the duration of seizures and apnea monitored and recorded (see Note 10 ).
-
10.
Only animals with the expected/planned range of apnea should be included and we consider this parameter to be an important assessment of the injury. There is no universally accepted method of determining injury severity when using the FPI method. Usually, the injury response including the apnea as well as mortality ranging from 10 to 20 % (“moderate FPI”) to ca. 40 % (“severe FPI”) is considered and there should be evidence of behavioral disturbance post-injury (see Note 11 ). In addition, depending on whether lateral or midline FPI is analyzed, there should be histological evidence of an injury—e.g., a cortical contusion, ipsilateral hippocampal injury and ipsilateral white matter injury in the lateral FPI model and widespread axonal injury in important white matter tracts including the brain stem in midline FPI (see Note 12 ). After the injury and resumption of breathing, the animals are taken back to the heating pad and isoflurane anesthesia is reinstated. The trauma cap, injury screws and cement is removed by firmly holding down the head and nose of the animal while gently pulling the block of cement upwards. The dura must then be carefully checked for the presence of breach, and if found the animal should be excluded, and the same holds true if there is glue obstructing the craniectomy .
3.3 Controlled Cortical Impact
The CCI device (Fig. 3) uses a pneumatically [23] or, less commonly, an electromagnetically [25] controlled impact which may be with high precision directed to the exposed dura at almost any chosen angle. The material of the end of the rod may be either rigid or a soft (e.g., silicone) and its shape can be either flat or rounded. Depending on the diameter of the rod, the depth of the impact, the velocity with which the rod strikes and its dwell time, i.e., the time the rod remains at the target depth, the tissue injury will change. The basic idea with CCI is to produce a focal TBI with tissue destruction and cell death ipsilateral to the injury, particularly in the injured cortex but also in the hippocampus and the underlying white matter tracts. A motor impairment and learning and memory deficits are also produced in this model in addition to a large tissue loss, depending on the various parameters described above.
-
1.
The anesthesia, placement of the animal and fixation of the head is similar to what is described in the FPI section. Using the diamond drill, a 4.0 mm diameter (mice) and a 5 × 6 mm craniotomy (rat) is created. It is crucial that the dura is kept intact and should be inspected for tears prior to induction of the injury. For mice, the craniotomy is performed over the left parietal cortex centered at 2.5 mm posterior to bregma and 2.5 mm lateral to the midline, anterior margin 1 mm posterior to bregma with the lateral margin at the crista temporalis. We use a flat 2.5 mm tip impounder striking the dura at 2.8–5.0 m/s allowing a 0.5–1 mm compression of the brain in mice [34]. In rats, we use a flat 4 mm diameter piston delivering the impact at 3 m/s allowing a brain deformation of 2.0 mm [35], see Notes 13 – 15 .
-
2.
After the injury, a dural breach is commonly seen at least with the more marked compression depths. After the injury, the rather large bone flap should be reattached using tissue adhesive (e.g., Histoacryl®, B.Braun Surgical, S.A., Rubi, Spain).
-
3.
Similarly for all the models mentioned above after TBI or sham injury, the animal is, following closure of the wound by interrupted and resorbable sutures, removed from the stereotaxic frame and placed in a wake-up cage with an overhead heating lamp.
-
4.
The animal remains in this cage until ambulatory after which it is allowed to return to its home cage.
3.4 Concluding Remarks
The animal models discussed in the present chapter are common worldwide and when used correctly, will continue to increase our knowledge of clinical TBI. A vast majority of experimental TBI research is performed on adolescent/young male animals and TBI scientist should more actively expand their research into other age groups, both genders and when pharmacological treatments are evaluated, also attempt the use of prolonged and more clinically relevant therapeutic windows. This author is not a strong believer in attempting the development of yet additional TBI models unless a specific TBI mechanisms not covered by the models described here (e.g., penetrating TBI, blast) is targeted. The CCI model as well as the lateral and central/midline FPI models can all be used in both rats and mice and they likely cover a large proportion of the heterogeneous TBI population (diffuse axonal injury , focal injury, “mixed” TBI) observed clinically. Thus, continuous refinement of the techniques and setup described here will likely continue to be important aspects of future preclinical TBI research.
4 Notes
Despite all efforts put into these TBI models, they do not produce human injuries due to many factors including different gray-white matter ratios in rodents and humans, the lissencephalic design of the rodent brain and the size differences resulting in considerably different biomechanical properties. Importantly, no rodent model adequately produce the long-lasting coma observed in severe human TBI. Regardless of these difficulties, preclinical TBI research is crucial in the development of novel treatment options. For that reason, there are numerous factors which should be considered when designing rodent TBI research to enhance the possibility of successful clinical translation.
-
(A)
Animals and preoperative considerations
Any effort should be made to reduce variability in research and avoiding bias. All experiments should be planned to minimize pain and suffering of the animals and if possible, reduce the number of animals without compromising with scientific and statistical quality.
-
1.
Prepare thoroughly prior to the start of the investigations including a careful review of existing literature. Are all ethical permissions granted and is the experiment described therein? What injury model best reflects the hypothesis of the study and at what severity? What age and gender should be used? What outcome measure should be used?
-
2.
The investigator performing the surgeries and/or the outcome evaluation must be blinded to the genotype of each animal, and describe it in the scientific publications. There are several guidelines providing tools to avoid bias in preclinical research, including the Collaborative Approach to Meta-Analysis and Review of Animal Data from Experimental Studies (CAMARADES) and ARRIVE guidelines [36].
-
3.
Since rodents are social animals, single housing should not be used and each cage should be equipped with sufficient stimuli supporting the normal behavior of a rodent.
-
4.
Handling of the rodents prior to any experiment is recommended to reduce stress and anxiety , particularly when behavioral outcome analysis is used [37].
-
5.
The included animals should preferably have a narrow weight and age range. Any TBI-induced weight loss should be monitored and documented and if it exceeds more than ~15 % of its original weight, or what is mandated by the animal ethics committee, the animal should be excluded from the study and humanely euthanized. Typically, FPI results in a higher degree of weight loss than the CCI models and the more severe TBI, the more profound the weight loss.
-
6.
All anesthetic agents have profound influence on cerebral and systemic physiology and will influence the outcome aimed to study. In general, sodium pentobarbital anesthesia is not ideal due to its influence on brain energy metabolism, its variable duration—particularly when supplemental doses are used—and its poor analgesic effects. In addition, female animals require less pentobarbital doses to achieve the same plane of anesthesia as male animals. Since it is used clinically for refractory intracranial hypertension in humans, it has obvious effects on cerebral physiology post-injury. It is the view of this author that volatile anesthetic agents are to be recommended, not because they are without influence on brain physiology, although since they can be easily titrated and cause rapid induction and resolution of the anesthesia [38, 39].
-
7.
Anesthetics and the surgery/injury itself will alter systemic parameters and influence breathing and circulation. Physiological monitoring is strongly recommended, either noninvasively [40] using pulse oximetry and/or a blood pressure cuff monitor, or invasively for arterial blood pressure and arterial blood gases using a catheter in either the tail or femoral artery [28].
-
8.
Post-operative pain analgesia is frequently mandated where opioids such as buprenorphine are common choices. If used at all, their potential influence on outcome following experimental TBI and the pathobiology of TBI [41, 42] should be considered. In general, nonsteroidal anti-inflammatory drugs (NSAID) are to be avoided, due to their potential for vasoconstriction, their possibility of increased hemorrhage and since they are not indicated for use in acute clinical TBI.
-
1.
-
(B)
Fluid percussion injury
The possibility of FPI to create widespread axonal injury, a clinically relevant brain displacement, its resulting cognitive deficits and the histological similarities to the human TBI setting makes both the lateral and central/midline FPI models useful and clinically relevant.
-
9.
Many of the technical aspects of creating FPI are mentioned in the Subheading 3. One crucial point is creating the craniotomy and its margin must be very consistent between animals since even small changes in craniotomy position will markedly alter outcome of lateral FPI [43, 44]. The size of the craniectomy must also be consistent since any change alters outcome [45, 46]. When the craniotomy is made using a dental drill, there will be heat generated by the drilling and the site should be regularly flushed with sterile saline at room temperature. During the drilling, the bone plate should regularly be checked and when it feels loose, it may be gently lifted by a pair of micro tweezers. Again, the dura cannot show evidence of a dural tear—if it does, the animal must be excluded from further study.
-
10.
At the moment of impact, there is, at least for an injury at a moderate–severe level, a consistent apnea which we use as a physiological measure of the impact and a “receipt” that the injury was correctly delivered. Thus, we recommend that it be monitored and measured. Unless systemic monitoring ensures that hypoxia does not occur, we suggest a cutoff level of 60s. If the apnea is of longer duration, it may introduce an additional insult to the injured brain and increase the variability of the injury as well as increasing mortality. At impact of experimental TBI, there may be acute electroencephalographic evidence of seizures [47]. Whether the acute motor twitching, which may be clonic in nature, observed at impact are in reality seizures remains to be established although we argue that their duration should be monitored.
-
11.
One important issue of the FPI technique is how to determine injury severity. Righting reflex time, level of atmospheres and—perhaps most commonly—the mortality have all been commonly used [21, 48]. At present there is no consensus on how to assess injury severity. For instance, a 10–20 % mortality is commonly used as a “moderate” injury and a pressure in atmospheres of 0.9–2.1 a mild–moderate injury [48]. We aim for 3.0 ± 0.1 atm for the lateral FPI model and 2.4 ± 0.2 for the central/midline FPI in rats and 1.4 ± 0.1 atm for midline FPI in mice [18] where the aim is a 30–45 s apnea, ca 10 % mortality, a clear cognitive deficit in for example the Morris Water Maze and a consistent and evident histological injury. Thus, it may be argued that one sole parameter may not fully indicate injury severity and comparisons among laboratories using the atm reading also appears difficult. Thus, the FPI should be titrated to the suggested outcome measure of the particular study instead of using one single parameter. Also remember that a “moderate” FPI is not equal to a “moderate” clinical TBI using the Glasgow Coma Scale Score.
-
12.
Histological parameters are important when assessing the quality of the FPI impact and there should be evidence of brain stem and white matter injury in the midline FPI and a cortical contusion, hippocampal injury, and white matter injury evident in for example the corpus callosum and the ipsilateral external capsule following lateral FPI [19, 20, 49].
-
9.
-
(C)
Controlled cortical impact
The CCI is easy to learn and master, it is fast and reproducible, is suitable for both rats and mice and is useful for the study of for example the progression of cortical contusion although it also produces white matter injury and neurodegeneration distant to the impact. Still, its role is mainly to mimic the “focal” TBI observed in the clinical setting.
-
13.
The crucial part of creating the CCI is the craniotomy which can be performed similar to what is described for the FPI. Using a dental drill at the carefully outlined area (some authors use a prefabricated disc glued onto the exposed skull to aid in the drilling), a standardized craniotomy can be produced. Importantly, the commonly used size for the bone flap is large, clinically approaching the size used for a decompressive craniectomy allowing for brain swelling and bulging through the craniotomy area. For that reason and to enhance clinical translation, the bone flap should as soon as possible following the impact be glued back using tissue adhesive (e.g., Histoacryl (see above), or Dermabond, Ethicon, Somerville, NJ; [50, 51]).
-
14.
Similar to the FPI, attempts have been made to characterize the CCI into different severity grades. Similar to our use of the Feeney weight-drop model, a compression depth of 1.5 mm was suggested to be a mild injury, 2.0 mm a moderate, and 2.5 mm a severe injury keeping all other injury parameters (speed, piston diameter, dwell time) the same [52]. However, due to the highly variable use of different piston diameters and materials, piston speed, dwell time and brain compression depths when the CCI is used, comparisons among laboratories are difficult and a standardized grade of “mild”, “moderate,” and “severe” has not been established.
-
15.
CCI should not be used at a very high severity level where a large part of the hemisphere is injured, which in the clinical setting is not an injury compatible with survival. Thus, if your CCI produces a massive destruction of one hemisphere, consider lowering not only the depth of brain compression but also the speed of impact.
-
13.
References
Tagliaferri F, Compagnone C, Korsic M, Servadei F, Kraus J (2006) A systematic review of brain injury epidemiology in Europe. Acta Neurochir (Wien) 148:255–268
Corrigan JD, Selassie AW, Orman JA (2010) The epidemiology of traumatic brain injury. J Head Trauma Rehabil 25:72–80
Maas AI, Stocchetti N, Bullock R (2008) Moderate and severe traumatic brain injury in adults. Lancet Neurol 7:728–741
Diaz-Arrastia R, Kochanek PM, Bergold P, Kenney K, Marx CE, Grimes CJ, Loh LT, Adam LT, Oskvig D, Curley KC, Salzer W (2014) Pharmacotherapy of traumatic brain injury: state of the science and the road forward: report of the Department of Defense Neurotrauma Pharmacology Workgroup. J Neurotrauma 31:135–158
Saatman KE, Duhaime AC, Bullock R, Maas AI, Valadka A, Manley GT, Workshop Scientific T, Advisory Panel M (2008) Classification of traumatic brain injury for targeted therapies. J Neurotrauma 25:719–738
Brody DL, Benetatos J, Bennett RE, Klemenhagen KC, Mac Donald CL (2015) The pathophysiology of repetitive concussive traumatic brain injury in experimental models; new developments and open questions. Mol Cell Neurosci 66:91–98
Xu L, Nguyen JV, Lehar M, Menon A, Rha E, Arena J, Ryu J, Marsh-Armstrong N, Marmarou CR, Koliatsos VE (2016) Repetitive mild traumatic brain injury with impact acceleration in the mouse: multifocal axonopathy, neuroinflammation, and neurodegeneration in the visual system. Exp Neurol 275(Pt 3):436–449
Schutz C, Stover JF, Thompson HJ, Hoover RC, Morales DM, Schouten JW, McMillan A, Soltesz K, Motta M, Spangler Z, Neugebauer E, McIntosh TK (2006) Acute, transient hemorrhagic hypotension does not aggravate structural damage or neurologic motor deficits but delays the long-term cognitive recovery following mild to moderate traumatic brain injury. Crit Care Med 34:492–501
Feng JF, Zhao X, Gurkoff GG, Van KC, Shahlaie K, Lyeth BG (2012) Post-traumatic hypoxia exacerbates neuronal cell death in the hippocampus. J Neurotrauma 29:1167–1179
Risling M, Davidsson J (2012) Experimental animal models for studies on the mechanisms of blast-induced neurotrauma. Front Neurol 3:30
Plantman S, Ng KC, Lu J, Davidsson J, Risling M (2012) Characterization of a novel rat model of penetrating traumatic brain injury. J Neurotrauma 29:1219–1232
Marklund N, Hillered L (2011) Animal modelling of traumatic brain injury in preclinical drug development: where do we go from here? Br J Pharmacol 164:1207–1229
Morales DM, Marklund N, Lebold D, Thompson HJ, Pitkanen A, Maxwell WL, Longhi L, Laurer H, Maegele M, Neugebauer E, Graham DI, Stocchetti N, McIntosh TK (2005) Experimental models of traumatic brain injury: do we really need to build a better mousetrap? Neuroscience 136:971–989
Lindgren S, Rinder L (1966) Experimental studies in head injury. II. Pressure propagation in “percussion concussion”. Biophysik 3:174–180
Dixon CE, Lyeth BG, Povlishock JT, Findling RL, Hamm RJ, Marmarou A, Young HF, Hayes RL (1987) A fluid percussion model of experimental brain injury in the rat. J Neurosurg 67:110–119
McIntosh TK, Vink R, Noble L, Yamakami I, Fernyak S, Soares H, Faden AL (1989) Traumatic brain injury in the rat: characterization of a lateral fluid-percussion model. Neuroscience 28:233–244
Carbonell WS, Maris DO, McCall T, Grady MS (1998) Adaptation of the fluid percussion injury model to the mouse. J Neurotrauma 15:217–229
Ekmark-Lewen S, Flygt J, Kiwanuka O, Meyerson BJ, Lewen A, Hillered L, Marklund N (2013) Traumatic axonal injury in the mouse is accompanied by a dynamic inflammatory response, astroglial reactivity and complex behavioral changes. J Neuroinflammation 10:44
Greer JE, McGinn MJ, Povlishock JT (2011) Diffuse traumatic axonal injury in the mouse induces atrophy, c-Jun activation, and axonal outgrowth in the axotomized neuronal population. J Neurosci 31:5089–5105
Thompson HJ, Lifshitz J, Marklund N, Grady MS, Graham DI, Hovda DA, McIntosh TK (2005) Lateral fluid percussion brain injury: a 15-year review and evaluation. J Neurotrauma 22:42–75
Kabadi SV, Hilton GD, Stoica BA, Zapple DN, Faden AI (2010) Fluid-percussion-induced traumatic brain injury model in rats. Nat Protoc 5:1552–1563
Lighthall JW (1988) Controlled cortical impact: a new experimental brain injury model. J Neurotrauma 5:1–15
Dixon CE, Clifton GL, Lighthall JW, Yaghmai AA, Hayes RL (1991) A controlled cortical impact model of traumatic brain injury in the rat. J Neurosci Methods 39:253–262
Smith DH, Soares HD, Pierce JS, Perlman KG, Saatman KE, Meaney DF, Dixon CE, McIntosh TK (1995) A model of parasagittal controlled cortical impact in the mouse: cognitive and histopathologic effects. J Neurotrauma 12:169–178
Brody DL, Mac Donald C, Kessens CC, Yuede C, Parsadanian M, Spinner M, Kim E, Schwetye KE, Holtzman DM, Bayly PV (2007) Electromagnetic controlled cortical impact device for precise, graded experimental traumatic brain injury. J Neurotrauma 24:657–673
Hall ED, Bryant YD, Cho W, Sullivan PG (2008) Evolution of post-traumatic neurodegeneration after controlled cortical impact traumatic brain injury in mice and rats as assessed by the de Olmos silver and fluorojade staining methods. J Neurotrauma 25:235–247
Feeney DM, Boyeson MG, Linn RT, Murray HM, Dail WG (1981) Responses to cortical injury: I. Methodology and local effects of contusions in the rat. Brain Res 211:67–77
Marklund N, Lewander T, Clausen F, Hillered L (2001) Effects of the nitrone radical scavengers PBN and S-PBN on in vivo trapping of reactive oxygen species after traumatic brain injury in rats. J Cereb Blood Flow Metab 21:1259–1267
Bondi CO, Semple BD, Noble-Haeusslein LJ, Osier ND, Carlson SW, Dixon CE, Giza CC, Kline AE (2014) Found in translation: Understanding the biology and behavior of experimental traumatic brain injury. Neurosci Biobehav Rev 58:123–146
Bolkvadze T, Pitkanen A (2012) Development of post-traumatic epilepsy after controlled cortical impact and lateral fluid-percussion-induced brain injury in the mouse. J Neurotrauma 29:789–812
Clausen F, Hillered L (2005) Intracranial pressure changes during fluid percussion, controlled cortical impact and weight drop injury in rats. Acta Neurochir 147:775–780
Axelson HW, Winkler T, Flygt J, Djupsjo A, Hanell A, Marklund N (2013) Plasticity of the contralateral motor cortex following focal traumatic brain injury in the rat. Restor Neurol Neurosci 31:73–85
Cole JT, Yarnell A, Kean WS, Gold E, Lewis B, Ren M, McMullen DC, Jacobowitz DM, Pollard HB, O’Neill JT, Grunberg NE, Dalgard CL, Frank JA, Watson WD (2011) Craniotomy: true sham for traumatic brain injury, or a sham of a sham? J Neurotrauma 28:359–369
Clausen F, Hanell A, Israelsson C, Hedin J, Ebendal T, Mir AK, Gram H, Marklund N (2011) Neutralization of interleukin-1beta reduces cerebral edema and tissue loss and improves late cognitive outcome following traumatic brain injury in mice. Eur J Neurosci 34:110–123
Clausen F, Lindh T, Salimi S, Erlandsson A (2014) Combination of growth factor treatment and scaffold deposition following traumatic brain injury has only a temporary effect on regeneration. Brain Res 1588:37–46
Kilkenny C, Browne WJ, Cuthill IC, Emerson M, Altman DG (2010) Improving bioscience research reporting: the ARRIVE guidelines for reporting animal research. J Pharmacol Pharmacother 1:94–99
Hanell A, Marklund N (2014) Structured evaluation of rodent behavioral tests used in drug discovery research. Front Behav Neurosci 8:252
Todd MM, Weeks J (1996) Comparative effects of propofol, pentobarbital, and isoflurane on cerebral blood flow and blood volume. J Neurosurg Anesthesiol 8:296–303
Statler KD, Alexander H, Vagni V, Dixon CE, Clark RS, Jenkins L, Kochanek PM (2006) Comparison of seven anesthetic agents on outcome after experimental traumatic brain injury in adult, male rats. J Neurotrauma 23:97–108
Thal SC, Plesnila N (2007) Non-invasive intraoperative monitoring of blood pressure and arterial pCO2 during surgical anesthesia in mice. J Neurosci Methods 159:261–267
Gentile NT, McIntosh TK (1993) Antagonists of excitatory amino acids and endogenous opioid peptides in the treatment of experimental central nervous system injury. Ann Emerg Med 22:1028–1034
Armstead WM (1997) Role of opioids in the physiologic and pathophysiologic control of the cerebral circulation. Proc Soc Exp Biol Med 214:210–221
Vink R, Mullins PG, Temple MD, Bao W, Faden AI (2001) Small shifts in craniotomy position in the lateral fluid percussion injury model are associated with differential lesion development. J Neurotrauma 18:839–847
Floyd CL, Golden KM, Black RT, Hamm RJ, Lyeth BG (2002) Craniectomy position affects morris water maze performance and hippocampal cell loss after parasagittal fluid percussion. J Neurotrauma 19:303–316
Sato M, Chang E, Igarashi T, Noble LJ (2001) Neuronal injury and loss after traumatic brain injury: time course and regional variability. Brain Res 917:45–54
D'Ambrosio R, Fairbanks JP, Fender JS, Born DE, Doyle DL, Miller JW (2004) Post-traumatic epilepsy following fluid percussion injury in the rat. Brain 127:304–314
Nilsson P, Ronne-Engstrom E, Flink R, Ungerstedt U, Carlson H, Hillered L (1994) Epileptic seizure activity in the acute phase following cortical impact trauma in rat. Brain Res 637:227–232
Alder J, Fujioka W, Lifshitz J, Crockett DP, Thakker-Varia S (2011) Lateral fluid percussion: model of traumatic brain injury in mice. J Vis Exp (54):pii: 3063
Flygt J, Djupsjo A, Lenne F, Marklund N (2013) Myelin loss and oligodendrocyte pathology in white matter tracts following traumatic brain injury in the rat. Eur J Neurosci 38:2153–2165
Hanell A, Clausen F, Djupsjo A, Vallstedt A, Patra K, Israelsson C, Larhammar M, Bjork M, Paixao S, Kullander K, Marklund N (2012) Functional and histological outcome after focal traumatic brain injury is not improved in conditional EphA4 knockout mice. J Neurotrauma 29:2660–2671
Zweckberger K, Stoffel M, Baethmann A, Plesnila N (2003) Effect of decompression craniotomy on increase of contusion volume and functional outcome after controlled cortical impact in mice. J Neurotrauma 20:1307–1314
Washington PM, Forcelli PA, Wilkins T, Zapple DN, Parsadanian M, Burns MP (2012) The effect of injury severity on behavior: a phenotypic study of cognitive and emotional deficits after mild, moderate, and severe controlled cortical impact injury in mice. J Neurotrauma 29:2283–2296
Acknowledgments
The author would like to thank Dr. Fredrik Clausen, Malin Olsen (for designing the FPI cartoon), and Dr. Johanna Flygt for their invaluable help with the animal models and for comment on the manuscript; Dr. Tracy K. McIntosh and Dr. John Povlishock for teaching the author the animal models described herein. This work was supported by funds from the Swedish Research council, European Union and the Uppsala University Hospital.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer Science+Business Media New York
About this protocol
Cite this protocol
Marklund, N. (2016). Rodent Models of Traumatic Brain Injury: Methods and Challenges. In: Kobeissy, F., Dixon, C., Hayes, R., Mondello, S. (eds) Injury Models of the Central Nervous System. Methods in Molecular Biology, vol 1462. Humana Press, New York, NY. https://doi.org/10.1007/978-1-4939-3816-2_3
Download citation
DOI: https://doi.org/10.1007/978-1-4939-3816-2_3
Published:
Publisher Name: Humana Press, New York, NY
Print ISBN: 978-1-4939-3814-8
Online ISBN: 978-1-4939-3816-2
eBook Packages: Springer Protocols