Abstract
The assisted reproductive technologies (ARTs) have been used in the production of rhesus monkey offspring at the Oregon National Primate Research Center (ONPRC) and that experience is summarized here. Additionally these technologies serve as a source of oocytes/embryos for monozygotic twinning, embryonic stem (ES) cell derivation and cloning. High fertilization efficiencies were realized with conventional insemination or following the use of intracytoplasmic sperm injection (ICSI) and approximately 50% of the resulting embryos grew in vitro to blastocysts. Both fresh and frozen sperm were employed in fertilization by ICSI and the resulting embryos could be low temperature stored for subsequent thawing and transfer when a synchronized recipient female was available or after shipment to another facility. Following the transfer of up to 3 embryos, an overall pregnancy rate of 30% was achieved with increasing rates dependent upon the number of embryos transferred. Singleton pregnancy outcomes following the transfer of ART produced embryos were similar to those observed in a control group of animals in the timed mated breeding colony at ONPRC. ICSI produced embryos were used in efforts to create monozygotic twins by blastomere separation or blastocyst splitting. While pregnancies were achieved following the transfer of demi-embryos, only one was a twin and it was lost to spontaneous abortion. ICSI produced embryos have also served as the source of blastocysts for the derivation of embryonic stem cells. These pluripotent cells hold potential for cell based therapies and we consider the monkey an important translational model in which to evaluate safety, efficacy and feasibility of regenerative medicine approaches based on the transplantation of stem cell-derived progeny. Finally, efforts to produce genetically-identical monkeys by nuclear transfer have been briefly summarized.
Similar content being viewed by others
Review
Notable progress has been realized in the past 20 years in both the development and application of the ARTs in monkeys with advances in ovarian follicular stimulation, fertilization by intractyoplasmic sperm injection (ICSI), culture medium development for the production of blastocysts, low temperature storage of sperm and embryos and embryo manipulation including twinning, cloning and the derivation of embryonic stem cells. Unlike in many fields where knowledge flows from non-human primate (NHP) research to clinical application in humans, the development of the ARTs in monkeys historically postdates human application. The experience in NHP, however, while nowhere nearly as robust as that in humans has been associated with several landmark accomplishments and methods for establishing pregnancies are currently available as summarized by us in 2001 [1]. While a few reports in New World monkeys and Great Apes exist, most research efforts have focused on Old World macaques with the rhesus monkey the primary subject and that species is the focus of this review.
The first successful birth of a rhesus macaque following IVF was reported in 1984 by Bavister and coworkers [2] and the total number of infants born to date is approximately one hundred. Development of the ARTs in NHPs has been impacted by resource availability, high expense and lack of compelling incentives to produce large numbers of monkeys using this approach. The latter limitation has recently been eliminated by the need for Indian-origin, rhesus macaques carrying the class 1 MHC allele, A*01 for HIV vaccine development research [3] (Figure 1). In addition to this demand for specific genotypes, many experimental paradigms could benefit from the availability of genetically-identical animals produced by monozygotic twinning or by somatic or ES cell cloning. Finally, development of cell-based therapies for the treatment of disease has gained momentum and a great deal of attention predicated on the availability of stem cells including those isolated from the blastocyst.
Schematic presentation of our approach to producing mamu A*01 positive rhesus monkey offspring. Sperm were acquired from an A*01-positive, homozygous male housed at the New England National Primate Research Center, frozen and shipped to ONPRC. Subsequent fertilization by ICSI produced heterozygous mamu A*01 offspring if the oocyte donor was mamu A*01 negative (over 80% of the colony at ONPRC) or 50% homozygous and 50% heterozygous if the oocyte donor was heterozygous for the mamu A*01 allele. We have now produced in excess of 30 offspring using this approach. Infants have also resulted from transfers of frozen-thawed embryos produced in Oregon and shipped to New England.
While application of the ARTs results in the production of embryos and pregnancies following transfer, information on pregnancy outcome is prerequisite to evaluating the impact of the ARTs on routine animal husbandry and more exotic applications such as the preservation of endangered species. The monkey can also serve as a model for clinical application of the ARTs where fertilization by ICSI has been associated with an increased frequency of genetic problems that may be secondary to the inappropriate expression of imprinted genes [4, 5]. In nonprimate animals, a large offspring syndrome [6] has been associated with in vitro manipulation of embryos and while this does not appear to be a problem in ART produced children, its possible existence in NHPs has not been evaluated.
This chapter will summarize the experience at ONPRC with the ARTs in the rhesus monkey building on two previous reviews [1, 7]. The methodology employed in the conduction of the ARTs in monkeys can also be found in these reviews. My objective is to disseminate the results of our extensive experience in the rhesus macaque in an effort to catalyze research using non-human primates.
Oocyte collection, fertilization and embryo culture
Oocyte recovery from adult, cycling rhesus monkeys subjected to controlled ovarian stimulation has been described previously [1] and reviewed in the contribution by Drs. Stouffer and Zelinski-Wooten. The percentage of oocytes recovered at the mature, fertilizable MII stage varies as a function of the hCG to egg collection time between 27 and 36 hr [8]. Experiments requiring enucleation are ideally conducted immediately after 1st polar body extrusion in which case a shorter time interval such as 27 hr is ideal. Oocytes that are recovered as metaphase I (MI) at the 27 hr interval can be monitored in vitro for release of the first polar body and used promptly thereafter. On the other hand, for routine fertilization, it is usually preferable to recover the maximum number of oocytes at the MII stage, in which case the hCG to collection interval can be lengthened to 33–34 hr. The number of oocytes collected following controlled ovarian stimulation in our experience is high, averaging 38 ± 2 [7]. Although not all are healthy, fertilizable oocytes, this number is considerably higher than that associated with the ARTs in women where a focus on the collection of approximately 10 high quality oocytes is becoming the norm [9]. This difference, along with the use of fixed length stimulation protocols, may be relevant to our efforts to improve ART outcomes in monkeys. A discussion of oocyte quantity and quality in the monkey can be found in the contribution by Drs. Stouffer and Zelinski-Wooten.
The conventional approach to embryo production using the ARTs is IVF and we reported a 61 ± 6% fertilization rate for 23 replicates involving 242 ova [7]. In our hands, complications associated with agglutination following sperm exposure to the capacitating agents, dibutyrylcyclic adenosine monophosphate and caffeine [10], are significant and we have, therefore, adopted ICSI as our routine insemination procedure. Similar if not improved outcomes have been experienced with fresh sperm ICSI, 81 ± 3% for 61 replicates and 714 ova, however, we do not know if the use of ICSI creates problems with regards the transmission of genetic disease or the production of suboptimal embryos. An evaluation would require the direct comparison of pregnancy rates obtained with IVF versus ICSI-produced embryos as well as long-term follow up on the offspring.
In general, conventional IVF is not feasible with frozen thawed sperm because of the rapid motility loss that occurs post-thaw [7]. However, control, fresh sperm fertilization rates can be achieved with cryopreserved sperm when ICSI is conducted 3 or more hours after sperm thawing and cryoprotectant removal. This delay presumably reflects the need for a post-thaw recovery period and restoration of the sperm's oocyte activating potential.
A complex medium, CMRL 1066 supplemented with serum, has historically been used to culture NHP embryos [11, 12]. In early trials, coculture on buffalo rat liver cell monolayers in the presence of CMRL 1066 produced the highest blastocyst development rate [13]. However, while coculture may improve developmental potential, its complexity makes the specific requirements for development in vitro difficult, if not impossible to study, not to mention the probable variability inherent in the coculture system. Attempts to culture embryos in a chemically defined medium (KSOM/AA) supplemented with serum resulted in improved, but inconsistent in vitro development rates [14]. Parenthetically, sequential media developed for human IVF such as G1/G2 have not produced satisfactory results in the monkey (unpublished). Recently, we initiated the use of HECM-9 in the absence of coculture [15–17] and reported a 76 ± 2% ICSI fertilization rate and a 47 ± 4% blastocyst formation rate [7]. Embryo culture in HECM-9 produced faster development than in CMRL/BRL or KSOM-AA with compact morulae present on day 3, cavitating blastocysts on day 5 and expanded blastocysts on day 7 (Figure 2). The rates reported here for HECM-9 may closely approximate the in vivo rates although the latter are based on the recovery and staging of a limited number of embryos flushed from the uterus [see Figure 2; [12, 14, 18]]. A retrospective comparison of pregnancy and implantation rates for embryos produced in these in vitro systems indicated similar results when embryo transfers were conducted with early stage (days 2–4) cleaving embryos. For CMRL/BRL produced embryos, 24 pregnancies were obtained in 96 transfers (25%) and for HECM-9 produced embryos, 20 pregnancies resulted from 77 transfers (26%) [7].
Average time in days for ART-produced embryos to reach a given developmental stage. Embryos were cultured in CMRL/BRL (yellow triangles), KSOM-AA supplemented with 10% fetal calf serum (pink squares) or HECM-9 with albumin (blue diamonds). M, morula; B, blastocyst; XB, expanded blastocyst. The results for CMRL/BRL coculture and KSOM-AA came from Weston and Wolf [14] and the embryos were produced by IVF while for culture in HECM-9, the results are from Wolf and coauthors [7] with the embryos produced by ISCI. Estimated in vivo developmental rates (open circles) have been included for reference purposes [12].
Embryo transfer
Parameters known to contribute to pregnancy and implantation rates following embryo transfer to synchronized recipients include the number of embryos transferred, embryo quality and the method of transfer. When increasing numbers of embryos were transferred up to 3, a corresponding increase in pregnancy rate to 36% was realized and implantation rates when expressed per embryo were independent of the number of embryos transferred. However, these databases are not yet large enough to establish statistical significance [7]. Recently we experienced the first triplet pregnancy reported in rhesus monkeys that occurred following the transfer of 3 frozen-thawed embryos. The pregnancy terminated spontaneously at 85 days possibly following intrauterine demise of the smallest member of the triplet set (Male, 0.067 kg; Female, 0.060 kg; Male,0.033 kg).
The ability to cryostore embryos and conduct transfers when recipients are available is essential to any widespread use of the ARTs in monkeys. In our experience, pregnancy and implantation rates for fresh and frozen-thawed ICSI produced embryos were associated with similar outcomes at approximately 30%. However, while the average number of embryos transferred was comparable for fresh (2.3) and frozen (2.1) embryos, substantial embryo loss (35%) was associated with freeze-thawing.
The conventional approach to embryo transfer (ET) in rhesus monkeys involves mini-laparotomy with a pregnancy rate of 27% (25/92) [7]. In order to avoid a surgical procedure, it would be ideal to conduct non-surgical ET with embryo deposition directly into the uterus, similar to the approach currently employed in women. However, the results to date in monkeys have been disappointing reflecting in part difficulty in passing the long tortuous cervix in this species. Laparoscopic ET with oviductal placement of embryos is the most recent variation developed by Dr. John Fanton and the surgical team at ONPRC (Figure 3). Similar pregnancy and implantation results were obtained when mini-laparotomy was compared to laparoscopy and since laparoscopy avoids exposure of the animal to a major surgery, that technique is now preferred by us. Preliminary evidence suggests that embryos at any stage of preimplantation development from 2-cell to expanded blastocyst can be transferred to the oviduct with pregnancy production.
Illustrations of the progressive stages in laparoscopic embryo transfer in rhesus monkeys. In Panel A, the fimbrium is grasped with a Patton retractor and placed in traction. A guide cannula is then introduced into the oviduct (Panel B). Finally the loaded transfer catheter is inserted transabdominally and advanced into the oviduct 1–3 cm in preparation for embryo deposition (Panel C).
The pregnancy success rate depends on the synchrony between the age of the transferred embryos, as measured by culture time in vitro, and the host endometrium, relative to the predicted day of ovulation. Synchronous transfers appear to be optimal in women. However, evidence supports an asynchronous transfer in the rhesus monkey [19, 20] with optimal timing for blastocyst (day 7/8) transfer into a day 4 uterine environment. This may reflect a retarded rate of development of embryos in vitro. In contrast, younger cleavage stage embryos were optimally transferred into synchronized recipients with the highest success rates following the transfer of day 3 embryos into either day 2,3 or 4 recipients.
Finally, pregnancy success rate is likely also to be a function of the psychological and physical health of the recipient. Thus, we have long suspected that imported Chinese rhesus monkeys are inferior to home grown, Indian origin, rhesus macaques as recipients, because the imported animals may not be as physically healthy and are at increased risk for poor psychological health. However, a retrospective review of embryo transfer did not support a statistically significance difference between the two with 13 of 59 (22%) transfers resulting in pregnancy in Chinese rhesus recipients and 35 of 132 (26%) for Indian-origin animals.
Oocyte/embryo manipulation
ART applications as described so far in this review, where ICSI has been used to compensate for poor motility in frozen-thawed sperm preparations, can also be extrapolated to the oocyte. Conventional IVF is a poor choice for fertilizing oocytes following extensive culture when zona hardening is a likely outcome. For instance, in cases were oocytes are matured in vitro. Another example is in the context of preserving fertility in young cancer survivors [21]. The strategy that we recently employed in the monkey model involved heterotropic transplantation of fresh ovarian tissue followed by oocyte recovery from the grafts. ICSI was then employed to fertilize these oocytes and the transfer of the resulting embryos resulted in the production of a pregnancy.
Somatic cell cloning (SCC) is perhaps the ideal approach to producing genetically identical animals because the clone size is, in theory, infinite. Protocols for SCC have been developed for a number of mammalian species and each appears to require species unique modifications to succeed [22, 23]. Cloned animal production rates are for the most part still very low except in widely studied species such as cattle where live birth rates in the 15–20% range are now realized [Andras Dinnyes, personal communication]. This increased rate in part reflects greater attention to fetal and neonatal monitoring with cloned pregnancies considered at high risk. The high fetal and neonatal wastage that is associated with SCC is thought to reflect incomplete reprogramming of the donor nucleus, perhaps secondary to the inappropriate expression of imprinted genes. Reprogramming is, of course, a bigger challenge when somatic cells are employed as the donor nuclei as opposed to relatively undifferentiated, embryonic cells. In fact, cloning success was first achieved in sheep with embryonic blastomeres or cell lines derived from embryonic cells. In monkeys, we began efforts to produce animals by nuclear transfer before SCC was considered feasible and were successful. Initially in 1997 [24], 3 pregnancies were achieved culminating in 2 live births in 9 embryo transfers. We repeated this success in 2002, with one term pregnancy in 11 embryo transfers, however, the fetus was lost as a stillborn. The most likely cause of death was fetal asphyxia and since no gross abnormalities were observed, we concluded that fetal demise was unrelated to the nuclear transfer process [25]. A number of variables have now been studied in the context of SCC in monkeys, however, we have not yet been successful in achieving a clinical pregnancy. Reconstructed embryos often grow in vitro to the morula stage but seldom to the blastocyst and we have no independent confirmation that the embryonic genome is actived in these cloned embryos. Since oocyte enucleation to produce the cytoplast, donor cell/nucleus fusion or injection to produce a reconstructed embryo, and chemical activation of development is common to both embryonic and SCC, we have concluded that the failure of SCC in the monkey is related to incomplete reprogramming of the somatic cell nucleus. This conclusion differs markedly from a recent report that cloning in primates [26] is precluded by the inadvertent removal of critical spindle related factors during enucleation. Moreover, successful therapeutic cloning in humans, would also argue against the concept that SCC is impossible in primates [27]. In order to follow up on our hypothesis that SCC is related to incomplete reprogramming, we have renewed our efforts to clone from monkey ES cells because these cells are relatively undifferentiated while still available in unlimited numbers supporting the eventual production of large numbers of genetically-identical, cloned animals.
In the absence of a successful protocol for SCC in monkeys, the need for genetically identical animals can be, at least, partly satisfied by producing identical twins. However, the twin rate in macaques is very low at 0.05% and is associated with poor outcomes [28]. Despite this low twinning rate in nature, when 2 ART produced embryos were transferred, the pregnancy rate was 25% (Table 1, top row) and the twinning rate was 20%. The latter statistic, with a different denominator, was derived when all pregnancies produced following transfer of 2 or 3 embryos were considered. A 64% live birth rate was obtained. Therefore, it would seem reasonable, despite the reluctance of free-ranging animals to carry twins to term, that monozygotic twins could be produced following transfer of ART produced demi-embryos. Two approaches to monozygotic twinning; blastomere separation and blastocyst bisection have been considered [29]. Demi-embryo pairs were produced in high efficiency by both methods and shown to be capable of growth to blastocysts in vitro similar to intact controls or able to re-expand following manipulation as in the case of blastocyst-derived, demi-embryos. Differential cell counts indicated that demi-embryos contained one half the total number of cells of their intact counterparts with no change in the ratios of ICM/trophectoderm or ICM to total cells. However, when demi-embryo sets were transferred into recipients, the pregnancy rate was similar to that obtained following the transfer of two intact embryos (Table 1, bottom row) but no term twin pregnancies were realized. Despite these disappointing preliminary results, we are continuing efforts to produce monozygotic twins by these approaches.
Primate embryonic stem cell lines were first generated in rhesus monkeys and marmosets in 1995 [30] and 1996 [31] respectively, followed by the human in 1998 [32] and the cynomolgus macaque in 2001 [33]. A parthenogenote ES cell is also available in the cynomolgus monkey [34]. Derivation of ES cell lines requires dissociation of ICM from trophoblast at the blastocyst stage with culture of the ICM on feeder layers of mitotically-inactivated, mouse embryonic fibroblasts (Figure 4). Initial success in the rhesus monkey by Thomson and colleagues [30] employed in vivo produced blastocysts recovered in uterine flushings. More recently, our group at ONPRC has developed a series of ES cell lines from in vitro produced, ICSI fertilized embryos. The availability of a stem cell bank comprised of 25 or so well characterized lines is crucial to future experimentation and an evaluation of ES cell line specificity. We envision the NHP as an essential translational model required in efforts to bring ES cell-based therapies to clinical trials in human patients.
Schematic representation of the derivation of monkey embryonic stem cells. ART-produced embryos are cultured to the expanded blastocyst stage before the trophectoderm is selectively lysed by immunosurgery. The ICM is recovered and cultured on mitotically-inactivated, mouse fetal fibroblasts. Epithelial outgrowths are harvested and dissociated before replating on the coculture. Eventually, ES cell colonies emerge that are selected, expanded and eventually subcloned before characterization [29].
Pregnancy and pregnancy outcome
We recently reviewed the outcome of 87 ART-produced pregnancies, 14 of which were twin gestations [7]. A population of pregnancies from the timed mated breeding colony was included as a gold standard for comparative purposes. In total, 234 of 257 (91%) clinical pregnancies resulted in live birth. In the TMB population, 14 cases of fetal demise were recorded for a 92.5% live birth rate. This value compared favorably with a live birth rate for an indoor TMB rhesus colony at the California Primate Center of 83% (1106/1332) [28].
For ART produced, singleton pregnancies (nuclear transfer, demi-embryos, ICSI and IVF combined; Table 2) 63 of 72 resulted in a live birth for a rate of 87.5%, statistically identical to the TMB population. When ART produced pregnancies were evaluated separately, ICSI and IVF, gave a combined live birth rate of 92.8 % (52/56), while pregnancy outcomes resulting from demi-embryo transfers were significantly lower at 69% (9/13). This impaired outcome with demi-embryos, although preliminary, suggests that despite appearances (high in vitro development rates to the blastocyst stage, ICM to total cell numbers similar to intact controls), demi-embryos are not the same as their intact counterparts.
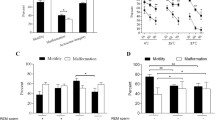
The sex ratios of ART produced pregnancies were the same as those for the TMB colony as were the gestational lengths and birth weights of singleton, live, term infants. The average twin birth weight was 0.37 kg with an average gestational age of only 150.7 days, in both cases significantly different from the corresponding singleton value. Growth rates based on animal weight for singleton and twin pregnancies are plotted in Figure 5. Offspring produced in twin pregnancies were significantly lower in average weight until 1 year of age. Interestingly, despite fetal wastage in multiple pregnancies the outcome of twin pregnancies to date has resulted in the production of an increased number of viable infants with 15 twin pregnancies confirmed as clinically viable producing 18 live, term monkeys.
Growth rates for ART-produced offspring. The average weight in kilograms for singleton (closed diamonds) and twin (closed square) offspring are plotted versus time in years. Results are compared to a group of singleton infants produced in the timed mated breeding colony (closed triangle) at ONPRC. Significant differences were observed between the singleton and twin offspring at birth and up until 1 year of age. Results are from Wolf and coauthors [7].
Conclusions
In the past 15 years, research into and practice of the ARTs in rhesus monkeys at ONPRC has resulted in a number of notable accomplishments. In 1988, the first was monkey produced following the transfer of an embryo that had been frozen, cryobanked and thawed after successful in vitro fertilization. This effort has also achieved the first twin pregnancies in rhesus monkeys, the first non-human primate infants produced by nuclear transfer of embryonic cells, the first rhesus monkey infant born following the transfer of an ICSI-produced blastocyst employing a non-surgical procedure, the first monkey live birth resulting from the transfer of a demi-embryo created by blastomere separation at the 2-cell stage or blastocyst bisection and the first infants produced following laparoscopic embryo transfer. Recently we reported the outcomes of 87 pregnancies (7).
Based on the results summarized in this mini-review, the ARTs in non-human primates would now seem to be ready for widespread application in the propagation of selected, desirable genotypes. This is not to say that there is no longer room for protocol development. However, improvements may be slow in coming because the high cost and limited access to the NHP resource means that relatively few programs will be able to participate. Yet improvements in pregnancy rates should be anticipated based on extrapolation from the clinical experience in women where protocol development over the entire 20+ history of the technology has resulted in ever increasing pregnancy and implantation rates. The current expectations include 50% pregnancy rates in patients under 35 and even higher levels when donor oocytes are used with implantation efficiencies of 0.5/embryo transferred [34–36]. How should we focus efforts in NHPs? This is a difficult challenge but selection of higher, and perhaps fewer, quality oocytes following animal exposure to individualized ovarian stimulation protocols seems a good place to start. Although embryo development in HECM-9 was improved over that obtained on coculture or in KSOM-AA, it is likely that further improvements in embryo culture that translate into higher pregnancy rates are possible. Finally attention focused on embryo transfer is appropriate both from a technical perspective, for instance with regards to pH stability in the oviduct during the insufflation required for laparoscopic ET, as well as recipient selection based on parameters that have not yet been developed but might reasonably include size, age, parity, menstrual cycle regularity and systemic cortisol level as an indirect measure of psychological health. From a longer term perspective, it may be worthwhile to evaluate the possible recovery and maturation of ovarian oocytes from necropsy animals or perhaps even to derive gametes from ES cells as has been accomplished in the mouse [37, 38].
Before ending, a comment or two relative to cost effectiveness of the ARTs in NHP is appropriate. Clearly, if there is no other way to acquire specific animals i.e., they are priceless, then this discussion is irrelevant. But consider acquiring rhesus macaques of either Indian-origin from local sources, if they are available at all, or Chinese-origin from importers. The cost of the former have been estimated at approximately $7,000 for a SPF, adult male and for the latter, approximately $5,000/yearling or adult (G. Heckman, personal communication). How much financial sense does it make then to use the ARTs in the context of routine animal production? First off, the ARTs can't compete with open corral housing and animal production where infant costs reflect only per diem maintenance rates at approximately $2,000 [7]. When considering the TMB colony where animals are individually caged, per diem increases dramatically and the cost per animal may approach $5,000. For animal production by IVF or ICSI and based on 30% pregnancy rates, the estimated cost per animal is between $7,500 and $9,000. However, modest improvements in outcome to 50% pregnancy rates following the transfer of 2 embryos can bring that cost down to $4,000. This is based on the expectation that a single controlled ovarian stimulation, oocyte collection, embryo production cycle can support 7–8 embryo transfers and 3–4 offspring. The use of frozen sperm ICSI, where a single ejaculate can provide adequate sperm for 100 oocyte cohorts, reduces the male costs to an insignificant level. Thus, the ARTs may soon be used extensively in the routine propagation of valuable animals. These considerations assume that the technical support and the resources already are in place and are based on modest subsidies for ARTCore services at ONPRC. The logistics of providing such services to the wider NHP community could involve the use of one or more centralized facilities or a larger number of local units.
References
Ouhibi N, Zelinski-Wooten MB, Thomson JA, Wolf DP: Assisted fertilization and nuclear transfer in nonhuman primates. In Assisted Fertilization and Nuclear Transfer in Mammals. Edited by: Wolf DP, Zelinski-Wooten M. 2001, New Jersey: Humana Press Totowa, 253-284.
Bavister BD, Boatman DE, Collins K, Dierschke DJ, Eisele SG: Birth of rhesus monkey infant after in vitro fertilization and non surgical embryo transfer. PNAS. 1984, 81: 2218-2222.
Cohen J: Vaccine studies stymied by shortage of animals. Science. 2000, 287: 959-960. 10.1126/science.287.5455.959.
Tarlatzis BC, Bili H: Survey on intracytoplasmic sperm injection: report from the ESHRE ICSI Task Force. European Society of Human Reproduction and Embryology. Hum Reprod. 1998, 13 (Suppl 1): 165-177.
Bonduelle M, Wilikens A, Buysse A, Van Assche E, Wisanto A, Devroey P, Van Steirteghem AC, Liebaers I: Prospective follow-up study of 877 children born after intracytoplasmic sperm injection (ICSI), with ejaculated epididymal and testicular spermatozoa and after replacement of cryopreserved embryos obtained after ICSI. Hum Reprod. 1996, 11 (7): 1558-1564.
Young LE, Fernandes K, McEvoy TG, Butterwith SC, Gutierrez CG, Carolan C, Broadbent PJ, Robinson JJ, Wilmut I, Sinclair KD: Epigenetic change in IGF2R is associated with fetal overgrowth after sheep embryo cultur. Nat Genet. 2001, 27: 153-154. 10.1038/84769.
Wolf DP, Thormahlen S, Ramsey C, Fanton J, Mitalipov S: Use of assisted reproductive technologies in the propagation of rhesus macaque offspring. Biol Reprod. 2004, BOR – Papers in Press, March 24, 2004. 10.1095/biolreprod.103.025932
Wolf DP, Alexander M, Zelinski-Wooten M, Stouffer RL: Maturity and fertility of rhesus monkey oocytes collected at different intervals after an ovulatory stimulus (Human chorionic gonadotropin) in in vitro fertilization cycles. Mol Reprod Dev. 1996, 43: 76-81. 10.1002/(SICI)1098-2795(199601)43:1<76::AID-MRD10>3.0.CO;2-2.
Melie NA, Adeniyi OA, Igbineweka OM, Ajayi RA: Predictive value of the number of oocytes retrieved at ultrasound-directed follicular aspiration with regard to fertilization rates and pregnancy outcome in intracytoplasmic sperm injection cycles. Fertil Steril. 2003, 80: 1376-1379. 10.1016/S0015-0282(03)02213-1.
Boatman DE, Bavister BD: Stimulation of rhesus monkey sperm capacitation by cyclic nucleotide mediators. J Reprod Fertil. 1984, 71: 357-366. 10.1530/jrf.0.0710357.
Pope CE, Pope VZ, Beck LR: Development of baboon preimplantation embryos to postimplantation stages in vitro. Biol Reprod. 1982, 27: 915-923.
Boatman DE: In vitro growth of non-human primate pre- and peri-implantation embryos. In The Mammalian Preimplantation Embryo. Edited by: Bavister BD. 1987, New York: Plenum Press, 273-308.
Zhang L, Weston AM, Denniston RS, Goodeaux LL, Godke RA, Wolf DP: Developmental potential of rhesus monkey embryos produced by in vitro fertilization. Biol Reprod. 1994, 51: 433-440.
Weston AM, Wolf DP: Differential preimplantation development of rhesus monkey embryos in serum supplemented media. Mol Reprod Dev. 1996, 44: 88-92. 10.1002/(SICI)1098-2795(199605)44:1<88::AID-MRD10>3.3.CO;2-I.
McKiernan SH, Bavister BB: Culture of one-cell hamster embryos with water soluble vitamins:pantothenate stimulates blastocyst production. Hum Reprod. 2000, 15: 157-164. 10.1093/humrep/15.1.157.
VandeVoort CA, Leibo SP, Tarantal AF: Improved collection and developmental competence of immature macaque oocytes. Theriogenology. 2003, 59: 699-707. 10.1016/S0093-691X(02)01129-9.
Schramm RD, Paprocki AM, VandeVoort CA: Causes of developmental failure of in vitro matured rhesus monkey oocytes: Impairments in embryonic genome activation. Hum Reprod. 2003, 18: 1-8. 10.1093/humrep/deg144.
Seshagiri PB, Bridson WE, Dierschke DJ, Eisele SG, Hearn JP: Non-surgical uterine flushing for the recovery of preimplantation embryos in rhesus monkeys: Lack of seasonal infertility. Am J Primatol. 1993, 29: 81-91.
Nusser KD, Mitalipov S, Widmann A, Gerami-Naini B, Yeoman RR, Wolf DP: Developmental competence of oocytes after ICSI in the rhesus monkey. Hum Reprod. 2001, 16: 130-137. 10.1093/humrep/16.1.130.
Wolfgang MJ, Eisele SG, Browne MA, Schotzko ML, Garthwaite MA, Durning M, Ramezani A, Hawley RG, Thomson JA, Golos TG: Rhesus monkey placental transgene expression after lentiviral gene transfer into preimplantation embryos. PNAS. 2001, 98: 10728-10732. 10.1073/pnas.181336098.
Lee DM, Yeoman RR, Battaglia DE, Stouffer RL, Zelinski-Wooten MB, Fanton JW, Wolf DP: Monkey born after ovarian tissue transplant. Nature. 2004, 428: 137-138. 10.1038/428137a.
Wolf DP, Mitalipov S, Norgren RB: Nuclear transfer technology in mammalian cloning. Arch Med Res. 2001, 32: 609-613. 10.1016/S0188-4409(01)00324-1.
Pennisi E, Vogel G: Clones: A hard act to follow. Science. 2000, 288: 1722-1731. 10.1126/science.288.5472.1722.
Meng L, Ely JJ, Stouffer RL, Wolf DP: Rhesus monkeys produced by nuclear transfer. Biol Reprod. 1997, 57: 454-459.
Mitalipov SM, Yeoman RR, Nusser KD, Wolf DP: Rhesus monkey embryos produced by nuclear transfer from embryonic blastomeres and somatic cells. Biol Reprod. 2002, 66: 1367-1373.
Simerly C, Dominko T, Navara C, Payne C, Capuano S, Gosman C, Chong K-Y, Takahashi D, Chace C, Compton D, Hewitson L, Schatten G: Molecular correlates of primate nuclear transfer failures. Science. 2003, 300: 297-10.1126/science.1082091.
Hwang WS, Ryu YJ, Park JH, Park ES, Lee EG, Koo JM, Chun HY, Lee BC, Kang SK, Kim SJ, Ahn C, Hwang JH, Park KY, Cibelli JB, Moon SY: Evidence of a pluripotent human embryonic stem cell line derived from a cloned blastocyst. Science. 2004, 303: 1669-1674. 10.1126/science.1094515.
Hendrie TA, Peterson PE, Short JJ, Tarantal AF, Rothgarn E, Hendrie MI, Hendricxx AG: Prequency of prenatal loss in a macaque breeding colony. Am J Primatol. 1996, 40: 41-53. 10.1002/(SICI)1098-2345(1996)40:1<41::AID-AJP3>3.3.CO;2-4.
Mitalipov SM, Yeoman RR, Huo H-C, Wolf DP: Monozygotic twining in rhesus monkeys by manipulation of in vitro derived embryos. Biol Reprod. 2002, 66: 1449-1455.
Thomson JA, Kalishman J, Golos TG, Durning M, Harris CP, Becker RA, Hearn JP: Isolation of a primate embryonic stem cell line. Proc Natl Acad Sci USA. 1995, 92: 7844-7848.
Thomson JA, Kalishman J, Golos TG, Durning M, Harris CP, Hearn JP: Pluripotent cell lines derived from the common marmoset (Callithrix jacchus) blastocysts. Biol Reprod. 1996, 55: 254-259.
Thomson JA, Itskovitz-Eldor J, Shapiro SS, Waknitz MA, Swiergiel JJ, Marshall VS, Jones JM: Embryonic stem cell lines derived from human blastocysts. Science. 1998, 282: 1145-1147. 10.1126/science.282.5391.1145.
Suemori H, Tada T, Torri T, Hosoi Y, Kobayashi K, Imahie H, Kondo Y, Iritani A, Nakatsuji N: Establishment of embryonic stem cell lines from cynomolgus monkey blastocysts produced by IVF or ICSI. Dev Dyn. 2001, 222: 273-279. 10.1002/dvdy.1191.
Cibelli JB, Grant KA, Chapman KB, Cunniff K, Worst T, Green HL, Walker SJ, Gutin PH, Vilner L, Tabar V, Dominko T, Kane J, Wettstein PJ, Lanza RP, Studer L, Vrana KE, West MD: Parthenogenetic stem cells in nonhuman primates. Science. 2002, 295: 819-10.1126/science.1065637.
Gardner DK, Surrey E, Minjarez D, Leitz A, Stevens J, Schoolcraft WB: Single blastocyst transfer: a prospective randomized trial. Fertil Steril. 2004, 81: 551-555. 10.1016/j.fertnstert.2003.07.023.
Shen S, Khabani A, Klein N, Battaglia D: Statistical analysis of factors affecting fertilization rates and clinical outcome associated with intracytoplasmic sperm injection. Fertil Steril. 2003, 79: 355-360. 10.1016/S0015-0282(02)04675-7.
Hubner K, Fuhrmann G, Christenson LK, Kehler J, Reinbold R, De La Fuente R, Wood J, Strauss JF, Boiani M, Scholer HR: Derivation of oocytes from mouse embryonic stem cells. Science. 2003, 300: 1251-1256. 10.1126/science.1083452. Originally published in Science Express May 2003 10.1126/science 1083452
Geljsen N, Horoschak M, Kim K, Gribnau J, Eggan K, Daley GQ: Derivation of embryonic germ cells from embryonic stem cells. Nature. 2004, 427: 148-154. 10.1038/nature02247.
Acknowledgments
Appreciation is expressed to Drs. Richard Stouffer, Mary Zelinski-Wooten, Shoukhrat Mitalipov, John Fanton, Richard Yeoman, David Hess and Gwen McGinnis for their participation in the development of the ARTs in rhesus macaques at ONPRC. The competent technical support of S Thormahlen, C Ramsey, A Widmann-Browning, C Greenberg, C Gagliardi and M Spermann is acknowledged along with the surgical services of D Jacob, J Kelly and N Dewey. Ms Julianne White is recognized for her excellent administrative support services. Serono Reproductive Biology Institute, a member of Serono, International, graciously provided the recombinant human gonadotropins and Antide used in cited studies. Finally, recognition is made of the financial support provided by NIH grants funding ONPRC (RR00163), and the author (RR15199 and NS44330 to DPW).
Author information
Authors and Affiliations
Corresponding author
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Wolf, D.P. Assisted reproductive technologies in rhesus macaques. Reprod Biol Endocrinol 2, 37 (2004). https://doi.org/10.1186/1477-7827-2-37
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1477-7827-2-37