Abstract
Purpose
The aim of this meta-analysis was to evaluate differences in functional outcomes between simultaneous bi-unicompartmental knee arthroplasty (Bi-UKA) and total knee arthroplasty (TKA) for the treatment of medial and lateral knee osteoarthritis.
Material and Methods
According to the PRISMA statement, a comprehensive search was conducted to identify studies reporting comparative results of the Bi-UKA versus the TKA. Of 953 titles, 6 studies met the inclusion criteria.
Results
A total of 286 patients were identified, of which 137 underwent Bi-UKA and 149 TKA. TKA reported a mean hip-knee-ankle (HKA) angle of 179.4 ± 2.4 compared to that in Bi-UKA measuring 177.2 ± 2.7 (p = 0.0001, 95% CI − 3.02 to − 1.38). No difference was found in the Western Ontario and McMaster Universities (WOMAC) pain (4 ± 1.6 and 4.2 ± 1.3 for Bi-UKA and TKA, respectively; p = 0.4996, 95% CI − 0.86 to 0.43). Bi-UKA was favorable in terms of WOMAC function (7.5 ± 1.9 and 9 ± 1.9 for Bi-UKA and TKA, respectively; p = 0.001, 95% CI − 2.29 to − 0.61) and WOMAC stiffness (1.6 ± 1 and 2.4 ± 0.7 for Bi-UKA and TKA, respectively; p = 0.0001, 95% CI − 1.18 to − 0.42). Bi-UKA showed a better Knee Society Score (KSS) in comparison to TKA (79.7 ± 7.8 and 75.4 ± 10.5 for Bi-UKA and TKA, respectively; p = 0.0021, 95% CI 1.58–7.02). The differences in postoperative outcomes scores between Bi-UKA and TKA were lower than their respective minimum clinically important differences.
Conclusions
When Bi-UKA and TKA are compared for the treatment of medial and lateral knee osteoarthritis, Bi-UKA are favorable in terms of WOMAC and KSS even though these values are lower than the minimum clinically important differences; moreover, similar postoperative hip-knee-ankle angle can be expected 3 years after Bi-UKA and TKA.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Unicompartmental knee arthroplasty (UKA) is a well-accepted alternative to total knee arthroplasty (TKA) for isolated compartment osteoarthritis (OA) of the knee [1, 2]. Beard et al. suggested that UKA should be considered the first choice for patients with late-stage isolated medial compartment OA [3]; moreover, reliable outcomes after lateral UKA have been reported [4].
In comparison with TKA, UKA offers several potential advantages including less-invasive surgical exposure, less morbidity and mortality, preservation of native bone stock, retention of cruciate ligaments, enhanced postoperative recovery, and improved patient satisfaction [5, 6].
In early reports, medial and lateral UKAs were used in both compartments of the same knee to treat severe OA [7, 8]. This is referred to as “simultaneous” bi-unicompartmental knee arthroplasty (Bi-UKA). Opposed to this is “staged” Bi-UKA in which a lateral or medial UKA is added, due to the progression of contralateral femorotibial OA, to a knee with an existing, well-functioning UKA [9]. An alternative option for lateral compartment OA after medial UKA is a revision to TKA which exposes these patients to the risks of revision knee arthroplasty. Moreover, it has been reported that 28% of total knee replacement candidates had a bicompartmental disease and infrequent impairment of cruciate ligaments, indicating that between one-fourth and one-third of patients undergoing TKA could be considered for bone-sparing Bi-UKA [10].
In recent years, simultaneous Bi-UKA is regaining interest amongst surgeons to treat bi-compartmental knee OA. Therefore, the purpose of this study was to perform a systematic review and meta-analysis of comparative studies evaluating outcomes of simultaneous medial and lateral Bi-UKA versus TKA for the treatment of knee OA.
Materials and Methods
Search Strategy
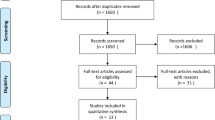
A systematic review of the published literature was conducted and reported according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement (Fig. 1) [11]. PubMed, MEDLINE, Scopus, and Cochrane Central databases were searched in February 2022. The terms “knee”, “arthroplasty”, “replacement”, “bi-unicompartmental”, “biunicompartmental”, “bi-compartmental”, “bicompartmental”, “bi-condylar”, “bicondylar” and “bi-unicondylar” were used in different combinations to retrieve relevant articles. Two authors (MM and DC) independently conducted all the searches and screened the titles and abstracts to identify relevant studies published. Differences were resolved by consulting a third senior reviewer (OG). An additional search was conducted by screening the reference list of each selected article, as well as the available grey literature at our institution.
Inclusion Criteria and Study Selection
During title, abstract, and full-text screenings, included studies had to: (1) report comparative outcomes of primary Bi-UKA versus TKA for the treatment of medial and lateral knee OA; (2) report more than five cases treated for each surgical technique; and (3) be written in English. Studies including patellofemoral arthroplasty as an additional procedure, reviews, technical articles, case reports, cadaveric/biomechanical studies, editorials, letters to the editor, and expert opinions were excluded from the analysis but considered for writing the discussion.
Data Extraction and Quality Assessment
Two authors (MM and DC) examined all the identified studies and extracted data. The first author, journal name, year of publication, study design, type of surgery and patient demographics were recorded for each article. Data considered for quantitative analysis consisted of the hip-knee-ankle (HKA) angle, the Western Ontario and McMaster Universities (WOMAC) questionnaire [12, 13] to assess pain, physical function disability and stiffness, and the Knee Society Score (KSS) [14, 15] to rate patient’s knee and functional abilities. The methodological quality of the included studies was assessed independently by three authors (MM, DC, and FF); cohort studies were assessed using the Modified Newcastle–Ottawa Quality Assessment Scale [16]. Based on the total score, quality was classified as “low” (0–3), “moderate” (4–6) and “high” (7–9). Randomized controlled trials were assessed with version 2 of the risk of bias tool (RoB2) [17, 18], recommended by the Cochrane Collaboration. Discrepancies were resolved by consulting a senior reviewer (OG) [19]. Details of this quality assessment are shown in Table 1.
Qualitative Analysis
A study was declared to have found an association for a factor when it was demonstrated with at least one of the outcomes utilized and only if statistically significant. Qualitative analysis was performed through the best evidence synthesis (BES), a concept first described by Slavin [20]. By taking into account the weight of each study in demonstrating an association between an outcome and a factor (weight provided by the risk of bias), the findings were aggregated to determine the strength of the evidence for each association reported in the literature. In particular, (1) strong evidence was found if an association was reported by two or more high-quality studies and by generally consistent findings across the studies (> 75% of the studies); (2) moderate evidence was found with one high-quality study, and two or more moderate/low-quality studies, or by two or more moderate/low-quality studies and generally consistent findings across the studies (> 75%), and (3) limited evidence was found with one or more moderate/low-quality studies or one high-quality study and generally consistent findings across the studies (> 75%). Conflicting evidence was found where the findings were conflicting (< 75% studies reported consistent findings). This algorithm was described by van Tulder et al. [21] and has been adopted in recent systematic reviews [22, 23].
Statistical Analysis
The quantitative data were organized for statistical analysis; all data were collected, measured, and reported with one-decimal accuracy. Weighted means and standard deviations (SD) were calculated for data concerning demographic characteristics and outcomes. When SD were not directly provided, these were calculated with the equation [max range–min range/4], to allow for statistical aggregation. The weighted mean and SD comparisons were performed using unpaired t-tests. All tests were performed with IBM SPSS Statistics software (version 25.0, IBM Corp., Armonk, NY) and GraphPad Prism (version 7.0, GraphPad Software Inc., San Diego, CA), Confidence intervals (CIs) were set at 95% and a p value less than 0.05 was considered significant.
Results
A total of 953 relevant articles were identified through the initial search, with 388 abstracts being screened. After this initial screening, 17 full-text articles were assessed for eligibility against our inclusion criteria, leading to 6 comparative studies entering the meta-analysis (Fig. 1) [24,25,26,27,28,29]. All articles were judged to be of high quality, scoring from seven to nine points on the Modified Newcastle–Ottawa Quality Assessment Scale (Table 1). The results of the qualitative analysis performed through the BES algorithm are shown in Table 2. The basic characteristics of these studies are shown in Table 3. A total of 286 patients were identified, of which 137 underwent Bi-UKA and 149 TKA. The mean follow-up was 40.4 months. In total, 56.8% of the cases were females, with a total mean age of the cohort of 65.2 ± 8.3 years (range 45–82). Types of implants, surgical technique, and indications for surgical treatment of the included studies are reported in Table 4. Patellofemoral joint was asymptomatic in two studies [25, 26] and radiological evidence of patellofemoral osteoarthritis was less than Kellgren and Lawrence grade III in the other two studies [24, 29]. Banger et al. [24] and Blyth et al. [29] reported that neither the trochlea nor the patella was resurfaced, nor was there a specific need to remove patellar osteophytes or remove overhanging lateral facets and circumferential denervation of the patella was not performed. Biazzo et al. [25] and Confalonieri et al. [26] reported that the patella was not resurfaced in any patients. Dettmer and Kreuzer [27] did not report detailed data on patella procedures. Fuchs et al. [28] reported that patella replacement was performed only among patients that underwent TKA.
Outcomes
Pre- and postoperative functional outcomes are shown in Table 5. Data on postoperative HKA angle values were available for 73 Bi-UKA and 78 TKA. TKA reported a better neutral alignment with a mean HKA angle of 179.4 ± 2.4 compared to that in Bi-UKA of 177.2 ± 2.7 (p = 0.0001, 95% CI − 3.02 to − 1.38). This outcome was reported in three studies [24,25,26] and the BES confirmed this result with strong evidence of better neutral alignment in favor of the TKA.
The postoperative WOMAC was evaluated in two studies [25, 26] for 41 and 40 Bi-UKA and TKA, respectively. No difference was found in WOMAC pain between the two surgical procedures (4 ± 1.6 and 4.2 ± 1.3 for Bi-UKA and TKA, respectively; p = 0.4996, 95% CI − 0.86 to 0.43). Postoperative pain was also assessed throughout the BES on five studies [25,26,27,28,29]; among these, three studies [25,26,27, 29] found no significant differences between the two surgical procedures while only one study [28] was in favor of the Bi-UKA resulting in limited evidence in favor of the latter.
Bi-UKA was favorable in terms of WOMAC function (7.5 ± 1.9 and 9 ± 1.9 for Bi-UKA and TKA, respectively; p = 0.001, 95% CI − 2.29 to − 0.61) and WOMAC stiffness (1.6 ± 1 and 2.4 ± 0.7 for Bi-UKA and TKA, respectively; p = 0.0001, 95% CI − 1.18 to − 0.42).
Four studies reported comparative outcomes on functionality assessed by KSS [25, 26, 28, 29], and postoperative KSS was available for 88 Bi-UKA and 94 TKA: Bi-UKA showed a better KSS (79.7 ± 7.8 and 75.4 ± 10.5 for Bi-UKA and TKA, respectively; p = 0.0021, 95% CI 1.58–7.02) in comparison to TKA. Five studies reported comparative outcomes on functionality assessed by the Knee Injury and Osteoarthritis Outcome Score (KOOS) [27], the Hospital for Special Surgery (HSS) score [28], the Tegner Activity Score [28], the Forgotten Joint Score (FJS) [29], the Oxford Knee Score (OKS) [29], the University of California, Los Angeles activity scale (UCLA) [29], and a dedicated UKA outcome score (i.e. GIUM) [25, 26] in addition to the KSS [25, 26, 28, 29]. In detail, two studies [27, 28] were in favor of the Bi-UKA while three studies [25, 26] found no significant differences. Therefore, moderate evidence in favor of the Bi-UKA according to the BES was noted in terms of knee functionality.
Discussion
The main findings of this study were that TKA reported a better neutral alignment compared to Bi-UKA, there were no differences in terms of pain between the two surgical procedures, and Bi-UKA was favorable in terms of function as expressed by WOMAC and KSS. The differences in postoperative KSS and WOMAC score between Bi-UKA and TKA were lower than their respective minimum clinically important differences (MCIDs). In addition, the postoperative values of the HKA angle were in the safe zone for either Bi-UKA and TKA.
The premise for any surgical operation to obtain satisfactory clinical efficacy and high safety is to strictly grasp its indications and contraindications. In this light, similar inclusion criteria for Bi-UKA and TKA were noted in the studies included in the current review. Furthermore, no significant differences were observed in the preoperative radiological or functional values between the groups that were compared in the current meta-analysis. The similar characteristics of the patients evaluated to allow for an appropriate assessment of the two surgical techniques through the analysis of the objective and reliable outcome data of all comparative studies included in the current meta-analysis.
In striving to improve patient satisfaction, alignment in knee arthroplasty surgery is gaining increased attention in recent years. HKA is a measure of lower limb alignment, defined as the angle between the mechanical axes of the femur and the tibia on a full-length lower-limb radiograph. In healthy adults with a neutral alignment, the HKA measures between 1.0° and 1.5° of varus [30]. In the present review, no differences were noted for the preoperative HKA angles between Bi-UKA and TKA; however, a better postoperative neutral alignment was reported for TKA compared to Bi-UKA in three studies with strong evidence as evaluated through the BES. Interestingly, it was reported a greater sensitivity to the native knee in the Bi-UKA surgery and fewer theoretical limits on the amount of varus or valgus to which the femoral and tibial components can be aligned. Indeed, decoupling the medial and lateral sides of the joint removes the concerns about cantilever loading on monoblock components used in TKA [24]. It should also be considered that the mean postoperative HKA angles here reported for both TKA and Bi-UKA (179.4 ± 2.4 and 177.2 ± 2.7, respectively) resulted within the safe zone of 177° to 183° [31]. Furthermore, it has been suggested [29] that Bi-UKA maintains the natural anatomy of the knee better in the coronal, sagittal, and axial planes and may therefore preserve normal joint kinematics, compared with a mechanically aligned TKA.
With regards to pain, limited evidence in favor of the Bi-UKA according to the BES was found and we were unable to detect a significant WOMAC pain difference between the two surgical procedures. Significantly lower postoperative pain scores for the UKA group than those of the TKA group were reported in a recent study [32]. Fuchs et al. [28] using the visual analogue scale (VAS) for assessment of pain further supported this result while Blyth et al. [29] reported similar VAS scores between Bi-UKA and TKA at both 3 months and 1 year after surgery.
Bi-UKA was favorable in terms of WOMAC function and WOMAC stiffness. This is statistically significant but, probably, clinically irrelevant. Indeed, a significant p value may be too small for a patient to notice or consider important [33]. The MCID has been defined as 11 for pain, 9 for function, 8 for stiffness, and 10 for the total WOMAC score after TKA [34]. Notably, in the current review, the differences between Bi-UKA and TKA in the WOMAC function and stiffness scores (i.e., 1.5 and 0.8, respectively) were lower than MCID.
Bi-UKA showed better patient’s knee and functional abilities assessed by the KSS but the difference (i.e., 4.3) between the groups was lower than the MCID that was reported to be 9 for the KSS-knee score and 10 for the KSS-function score after primary TKA [35]. It has been hypothesized that Bi-UKA can achieve better functional results compared to TKA, probably because it retains both cruciate ligaments and so preserve and maintain knee proprioception [36, 37]. Indeed, patient satisfaction and functional outcome have been closely correlated with knee proprioception [36]. Fuchs et al. emphasized that by maintaining both the cruciate ligaments, a bicondylar sledge prostheses achieves functional results as good as TKA, avoiding the potential complication of progressive OA in the contralateral compartment [28].
To the best of our knowledge, this appears to be the first meta-analysis to compare medial and lateral Bi-UKA and TKA in terms of knee alignment, pain, and function. We conducted the current study in accordance with the PRISMA statement and critically evaluated the quality of all selected studies. The great strength of this study is that it is the only meta-analysis to compare the efficacy objectively and quantitatively between the two surgical techniques. We selected comparative studies only, allowing for pooling of effect sizes. This minimized the bias coming from the aggregation of data of single-arm heterogeneous trials, typical of previous systematic reviews, which gave rigor and credibility to our findings. Notably, we found similar indications for Bi-UKA and TKA and comparable preoperative radiological and clinical characteristics of the patients evaluated in the current work.
The following limitations of this meta-analysis should be acknowledged. First, only six studies with a small number of cases were included due to limited literature available, and more randomized controlled trials are needed to obtain robust conclusions. Second, there was a great heterogeneity in the reporting of subjective and objective outcomes. Third, it is possible that relevant articles or patient populations were not identified with our search criteria, as with all systematic reviews. Fourth, we included studies with different evaluation times; it is likely that outcome scores are affected by the length of patient follow-up, and these outcomes could also be potentially different between the two procedures if a specific follow-up time was determined. In addition, we selected only literature in the English language, potentially contributing to publication bias even if it has been reported that restricting systematic reviews to English-language publications appears to have little impact on the effect estimates [38]. Another source of limitation was the lack of long-term data. Finally, the results of our systematic analysis may be influenced by different prosthesis types, surgical techniques, and postoperative care and should be interpreted with caution. The search for the best treatment for patients with severe knee OA should not encourage clinicians to ignore that differences in patients’ characteristics might favor a certain treatment option and that appropriate patient selection, newer implant designs, and surgical techniques are critically important to maximize outcomes.
In conclusion, this meta-analysis reveals that when Bi-UKA and TKA are compared for the treatment of medial and lateral knee osteoarthritis, Bi-UKA are favorable in terms of WOMAC and KSS even though these values are lower than the minimum clinically important differences; moreover, the similar postoperative hip-knee-ankle angle can be expected 3 years after Bi-UKA and TKA. Future studies including a higher number of patients and more randomized controlled trials should confirm these findings.
References
Argenson, J.-N.A., Blanc, G., Aubaniac, J.-M., & Parratte, S. (2013). Modern unicompartmental knee arthroplasty with cement: A concise follow-up, at a mean of twenty years, of a previous report. Journal of Bone and Joint Surgery. American Volume, 95, 905–909. https://doi.org/10.2106/JBJS.L.00963
Winnock de Grave, P., Barbier, J., Luyckx, T., et al. (2018). Outcomes of a fixed-bearing, medial, cemented unicondylar knee arthroplasty design: survival analysis and functional score of 460 cases. Journal of Arthroplasty, 33, 2792–2799. https://doi.org/10.1016/j.arth.2018.04.031
Beard, D. J., Davies, L. J., Cook, J. A., et al. (2019). The clinical and cost-effectiveness of total versus partial knee replacement in patients with medial compartment osteoarthritis (TOPKAT): 5-year outcomes of a randomised controlled trial. Lancet Lond Engl, 394, 746–756. https://doi.org/10.1016/S0140-6736(19)31281-4
Seo, S.-S., Kim, C.-W., Lee, C.-R., et al. (2019). Long-term outcomes of unicompartmental knee arthroplasty in patients requiring high flexion: An average 10-year follow-up study. Archives of Orthopaedic and Trauma Surgery, 139, 1633–1639. https://doi.org/10.1007/s00402-019-03268-7
Hauer, G., Sadoghi, P., Bernhardt, G. A., et al. (2020). Greater activity, better range of motion and higher quality of life following unicompartmental knee arthroplasty: A comparative case-control study. Archives of Orthopaedic and Trauma Surgery, 140, 231–237. https://doi.org/10.1007/s00402-019-03296-3
Lyons, M. C., MacDonald, S. J., Somerville, L. E., et al. (2012). Unicompartmental versus total knee arthroplasty database analysis: Is there a winner? Clinical Orthopaedics, 470, 84–90. https://doi.org/10.1007/s11999-011-2144-z
Gunston, F. H. (1971). Polycentric knee arthroplasty. Prosthetic simulation of normal knee movement. Journal of Bone and Joint Surgery. British Volume, 53, 272–277.
Goodfellow, J. W., & O’Connor, J. (1986). Clinical results of the Oxford knee. Surface arthroplasty of the tibiofemoral joint with a meniscal bearing prosthesis. Clinical Orthopaedics and Related Research, 205, 21–42.
Pandit, H., Mancuso, F., Jenkins, C., et al. (2017). Lateral unicompartmental knee replacement for the treatment of arthritis progression after medial unicompartmental replacement. Knee Surgery, Sports Traumatology, Arthroscopy, 25, 669–674. https://doi.org/10.1007/s00167-016-4075-4
Heekin, R., & Fokin, A. (2013). Incidence of bicompartmental osteoarthritis in patients undergoing total and unicompartmental knee arthroplasty: is the time ripe for a less radical treatment? The Journal of Knee Surgery, 27, 077–082. https://doi.org/10.1055/s-0033-1349401
Moher, D., Liberati, A., Tetzlaff, J., et al. (2009). Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. BMJ, 339, b2535. https://doi.org/10.1136/bmj.b2535
Grappiolo, G., Bruno, C. F., Loppini, M., et al. (2020). Conversion of fused hip to total hip arthroplasty: long-term clinical and radiological outcomes. Journal of Arthroplasty. https://doi.org/10.1016/j.arth.2020.09.030
Salaffi, F., Leardini, G., Canesi, B., et al. (2003). Reliability and validity of the Western Ontario and McMaster Universities (WOMAC) Osteoarthritis Index in Italian patients with osteoarthritis of the knee. Osteoarthritis Cartilage, 11, 551–560. https://doi.org/10.1016/s1063-4584(03)00089-x
Insall, J. N., Dorr, L. D., Scott, R. D., & Scott, W. N. (1989). Rationale of the Knee Society clinical rating system. Clinical Orthopaedics and Related Research, 248, 13–14.
Mercurio, M., Gasparini, G., Carbone, E. A., et al. (2020). Personality traits predict residual pain after total hip and knee arthroplasty. International Orthopaedics, 44, 1263–1270. https://doi.org/10.1007/s00264-020-04553-6
Wells, G., Wells, G., & Shea, B. et al. (2014). The Newcastle–Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. undefined
Galasso, O., Gasparini, G., De Benedetto, M., et al. (2012). Tenotomy versus tenodesis in the treatment of the long head of biceps brachii tendon lesions. BMC Musculoskeletal Disorders, 13, 205. https://doi.org/10.1186/1471-2474-13-205
Sterne, J. A. C., Savović, J., Page, M. J., et al. (2019). RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ, 366, l4898. https://doi.org/10.1136/bmj.l4898
Familiari, F., Castricini, R., Galasso, O., et al. (2021). The 50 highest cited papers on rotator cuff tear. Arthroscopy, 37, 61–68. https://doi.org/10.1016/j.arthro.2020.07.044
Slavin, R. E. (1995). Best evidence synthesis: An intelligent alternative to meta-analysis. Journal of Clinical Epidemiology, 48, 9–18. https://doi.org/10.1016/0895-4356(94)00097-a
van Tulder, M., Furlan, A., Bombardier, C., et al. (2003). Updated method guidelines for systematic reviews in the cochrane collaboration back review group. Spine, 28, 1290–1299. https://doi.org/10.1097/01.BRS.0000065484.95996.AF
Fanelli, D., Mercurio, M., Gasparini, G., & Galasso, O. (2021). Predictors of meniscal allograft transplantation outcome: a systematic review. The Journal of Knee Surgery, 34, 303–321. https://doi.org/10.1055/s-0039-1695043
Mercurio, M., Castioni, D., Iannò, B., et al. (2019). Outcomes of revision surgery after periprosthetic shoulder infection: A systematic review. Journal of Shoulder and Elbow Surgery. https://doi.org/10.1016/j.jse.2019.02.014
Banger, M. S., Johnston, W. D., Razii, N., et al. (2020). Robotic arm-assisted bi-unicompartmental knee arthroplasty maintains natural knee joint anatomy compared with total knee arthroplasty: a prospective randomized. The Bone & Joint Journal, 102, 8.
Biazzo, A., Manzotti, A., & Confalonieri, N. (2018). Bi-unicompartmental versus total knee arthroplasty: Long term results. Acta Orthopaedica Belgica, 84, 237–244.
Confalonieri, N., Manzotti, A., Cerveri, P., & De Momi, E. (2009). Bi-unicompartmental versus total knee arthroplasty: A matched paired study with early clinical results. Archives of Orthopaedic and Trauma Surgery, 129, 1157–1163. https://doi.org/10.1007/s00402-008-0713-8
Dettmer, M., & Kreuzer, S. W. (2015). Bi-unicompartmental, robot-assisted knee arthroplasty. Operative Techniques in Orthopaedics, 25, 155–162. https://doi.org/10.1053/j.oto.2015.03.004
Fuchs, S., Tibesku, C. O., Genkinger, M., et al. (2004). Clinical and functional comparison of bicondylar sledge prostheses retaining all ligaments and constrained total knee replacement. Clinical Biomechanics, 19, 263–269. https://doi.org/10.1016/j.clinbiomech.2003.11.004
Blyth, M. J. G., Banger, M. S., Doonan, J., et al. (2021). Early outcomes after robotic arm-assisted bi-unicompartmental knee arthroplasty compared with total knee arthroplasty: a prospective, randomized controlled trial. Bone Jt J, 103B, 1561–1570. https://doi.org/10.1302/0301-620X.103B10.BJJ-2020-1919.R2
Moreland, J. R., Bassett, L. W., & Hanker, G. J. (1987). Radiographic analysis of the axial alignment of the lower extremity. Journal of Bone and Joint Surgery. American Volume, 69, 745–749.
Winnock de Grave, P., Luyckx, T., Claeys, K., et al. (2020). Higher satisfaction after total knee arthroplasty using restricted inverse kinematic alignment compared to adjusted mechanical alignment. Knee Surgery, Sports Traumatology, Arthroscopy. https://doi.org/10.1007/s00167-020-06165-4
Leiss, F., Götz, J. S., Maderbacher, G., et al. (2020). Pain management of unicompartmental (UKA) vs total knee arthroplasty (TKA) based on a matched pair analysis of 4144 cases. Scientific Reports, 10, 17660. https://doi.org/10.1038/s41598-020-74986-x
Leopold, S. S., & Porcher, R. (2017). Editorial: The minimum clinically important difference-the least we can do. Clinical Orthopaedics, 475, 929–932. https://doi.org/10.1007/s11999-017-5253-5
Clement, N. D., Bardgett, M., Weir, D., et al. (2018). What is the minimum clinically important difference for the WOMAC Index after TKA? Clinical Orthopaedics, 476, 2005–2014. https://doi.org/10.1097/CORR.0000000000000444
Lizaur-Utrilla, A., Gonzalez-Parreño, S., Martinez-Mendez, D., et al. (2020). Minimal clinically important differences and substantial clinical benefits for Knee Society Scores. Knee Surgery, Sports Traumatology, Arthroscopy, 28, 1473–1478. https://doi.org/10.1007/s00167-019-05543-x
Al-Dadah, O., Hawes, G., Chapman-Sheath, P. J., et al. (2020). Unicompartmental vs segmental bicompartmental vs total knee replacement: comparison of clinical outcomes. Knee Surgery & Related Research, 32, 47. https://doi.org/10.1186/s43019-020-00065-0
Parratte, S., Pauly, V., Aubaniac, J.-M., & Argenson, J.-N.A. (2010). Survival of bicompartmental knee arthroplasty at 5 to 23 years. Clinical Orthopaedics, 468, 64–72. https://doi.org/10.1007/s11999-009-1018-0
Dobrescu, A. I., Nussbaumer-Streit, B., Klerings, I., et al. (2021). Restricting evidence syntheses of interventions to English-language publications is a viable methodological shortcut for most medical topics: A systematic review. Journal of Clinical Epidemiology, 137, 209–217. https://doi.org/10.1016/j.jclinepi.2021.04.012
Funding
No funding was received for conducting this study.
Author information
Authors and Affiliations
Contributions
Each author fulfils each of the authorship requirements. MM conceived and designed the study, performed the statistical analysis, participated in the acquisition and interpretation of data, and drafted the manuscript; GG conceived and coordinated the study and approved the final version of the manuscript as submitted; FF participated in the design of the study, in the acquisition and interpretation of data and drafted the manuscript; DC participated in the acquisition of data and drafted the manuscript; and OG conceived and coordinated the study and revised critically the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
The authors have no conflicts of interest to declare that are relevant to the content of this article.
Ethical Approval
Not applicable because this study evaluated data from already published studies.
Informed Consent
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Mercurio, M., Gasparini, G., Familiari, F. et al. Outcomes of Bi-unicompartmental Versus Total Knee Arthroplasty for the Treatment of Medial and Lateral Knee Osteoarthritis: A Systematic Review and Meta-analysis of Comparative Studies. JOIO 56, 963–972 (2022). https://doi.org/10.1007/s43465-022-00628-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43465-022-00628-1