Abstract
Aim of the study
We assessed the role of personality traits, anxiety, and depression in residual pain among patients who underwent total hip (THA) and knee (TKA) arthroplasty.
Method
Eighty-three patients (40 THA and 43 TKA) were interviewed pre-operatively (t0); five days (t1) after surgery; and one (t2), three (t3), six (t4), and 12 months (t5) after surgery. Personality (TCI-R), pain (VAS), anxiety and depression (HADS), quality of life (SF-12), functionality (HHS/KSS), and disability (WOMAC) were evaluated.
Results
Pain reduction and functional improvement were reported at t5 (both p < 0.001) in both THA and TKA patients. THA patients showed earlier and greater functional improvement after surgery (both p < 0.001) in comparison with TKA. Residual pain (VAS > 30 mm) was noted in 15% of the THA patients and 25% of the TKA patients, and it correlated with the SF-12 PCS (r2 = − 0.412; p < 0.001), SF-12 MCS (r2 = − 0.473; p < 0.001), HADS-A (r2 = 0.619; p = <0.001), HADS-D (r2 = 0.559; p < 0.001), functionality (r2 = − 0.482; p < 0.001), and WOMAC (r2 = 0.536; p < 0.001) scores at t5. High pre-operative harm avoidance, persistence, and anxiety scores were predictive of residual pain after both THA and TKA (p < 0.001).
Discussion
The proportion of patients complaining of residual pain in this study was similar to that in previous findings. Multiple predictors of residual pain after THA and TKA have been previously described, and several studies evaluated the influence of psychological factors on the outcome of joint arthroplasty; however, only four studies investigated the role of personality traits in the outcome of THA and TKA patients, and a unique study out of these investigations demonstrated the effect of personality on persisting pain.
Conclusion
The current study demonstrated that personality traits and anxiety predict residual pain; thus, pre-operative evaluation of these factors could be helpful in identifying patients at risk for residual pain.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Total hip (THA) and knee (TKA) arthroplasty are successful and safe operations for managing patients with disabling articular pain, reducing quality of life and functional limitations arising from end-stage joint damage following a number of diseases, such as severe osteoarthritis, rheumatoid arthritis, and fractures.
As longevity increases, the demand for primary TKA and TKA continues to rise. Although joint arthroplasty is widely acknowledged to be one of the most successful procedures in orthopaedic practice, residual pain not attributable to known causes (e.g., infection, stiffness, instability, loosening, fractures, and neurovascular injuries) is commonly present in a considerable percentage of patients [1], posing a challenge to physicians. Overall, 8–17% and 9–20% of patients complain of residual pain of an unknown cause after THA and TKA procedures, respectively [2].
Pain is a subjective, sensorial experience that varies greatly not only from person to person but also within the same subject. Genetics, prior learning, expectations, sociocultural environments, and psychological factors can influence the pain experience. Among these factors, personality traits and psychiatric disorders have been proposed as possible predisposing factors of pain perception [3]. Personality has been defined as the characteristic sets of behaviours, cognitions, and emotional patterns that evolve from biological and environmental factors; different personality traits have been described [4].
Systematic reviews examining the influence of psychological factors have been published [5]; however, to our knowledge, only one study [6] evaluated the influence of personality traits on residual pain in TKA patients. Establishing what kind of psychological distress or disorder has the greatest impact on outcome after total joint arthroplasty may be helpful for physician in order to develop pre-operative interventions with the aim of improving the outcomes after this surgery. This study aimed to assess the role of personality traits, anxiety, and depression in residual pain among patients who undergo THA or TKA. We hypothesized that residual pain would occur more frequently among patients with personality traits.
Materials and methods
Participants
Ninety consecutive patients who underwent primary THA or TKA for osteoarthritis at our institution between May 2015 and July 2017 were initially invited to participate in this study.
Primary osteoarthritis, an age older than 18 years at the time of surgery, the capability to communicate with healthcare professionals and give valid informed consent, and a willingness to participate in a 12-month follow-up were the inclusion criteria. The exclusion criteria were (1) significant cognitive impairment, (2) a diagnosis of or treatment for any psychiatric condition, (3) residual pain after total joint arthroplasty with known causes (e.g., infection, stiffness or loosening, instability, a fracture or neurovascular injury, physical characteristics, or comorbidities), and (4) a failure to complete the questionnaires.
All procedures performed in the current study were in accordance with the ethical standards of the institutional review board. The signed informed consent was provided by each patient that completed self-administered questionnaires and was individually interviewed by a trained researcher the day before surgery (t0); five days (t1) after surgery; and one (t2), three (t3), six (t4), and 12 months after surgery (t5). Of the initial 90 patients, 83 were included in the final sample population (40 THA patients and 43 TKA patients). The reasons for exclusion were death by acute myocardial infarction seven months after the surgical procedure (1), periprosthetic knee infection (1), and absence at any of the scheduled follow-ups (5).
Surgical technique
THA was performed using a modified posterolateral approach in the lateral decubitus position with a cementless, proximally coated, tapered stem with cementless, hemispherical acetabular fixation, a ceramic femoral head, and a polyethylene acetabular liner (Corail® femoral stems and Pinnacle® acetabular component; DePuy International Ltd., Leeds, England).
TKA was performed using a medial parapatellar approach while the patient was in the supine position and a cemented implant (Persona® knee implant system; Zimmer Biomet Inc., Warsaw, IN, USA). The patella was not resurfaced in any of the patients.
For both THA and TKA, regional anesthesia, either spinal or epidural, was recommended over general anaesthesia in the absence of specific contraindications. A multimodal analgesia strategy combining an intravenous formulation of acetaminophen (1 g every 12 h for 5 days), an injectable nonsteroidal anti-inflammatory drug (diclofenac 75 mg every 12 h for 4 days), an oral opioid (tapentadol 50 mg every 12 hours for three days), and cryotherapy was used in the absence of specific contraindications to improve post-operative pain and reduce the consumption of each agent. Post-operatively, patients underwent early mobilization the same day of surgery, including early ambulation with walking aids and muscle strengthening exercises. Discharge from the hospital occurred five days post-operatively.
Measures
Personality traits were assessed using the revised Temperament and Character Inventory (TCI-R) [4]. The questionnaire comprises 240 items covering four temperamental dimensions (novelty seeking, harm avoidance, reward dependence, and persistence) and three character dimensions (self-directedness, cooperativeness, and self-transcendence).
Anxiety and depression were assessed by means of the Hospital Anxiety and Depression Scale (HADS) [7]. This valid and reliable tool comprises 14 questions (seven for anxiety, HADS-A, and seven for depression, HADS-D) on a Likert scale (0–3). For each scale, final scores of ≤ 7, 8–10, and ≥ 11 are indicative of no significant anxiety or depression, borderline anxiety or depression, and clinical anxiety or depression, respectively.
The 12-Item Short Form Survey (SF-12) is a 12-item questionnaire used to assess generic health outcomes from the patient’s perspective [8]. Two summary scales (the physical and the mental component summary, PCS and MCS, respectively) can be computed with scores ranging from 0 to 100%; higher scores indicate a better quality of life.
The visual analogue scale (VAS) was used as a subjective measure of pain perception. A VAS score > 30 mm [9] at t5 indicated residual pain.
The Harris hip score (HHS) and the American Knee Society Score (KSS) were used to rate each patient’s joint and functional abilities [10]. For statistical purposes, the score of each outcome domain was first rescaled to a 0 to 100% value with 100% representing the best possible health value for each domain.
The Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) was used to assess pain, stiffness, and physical function disability in patients suffering from knee and hip osteoarthritis [8]. The WOMAC provides either single domain scores or a total score (0–96).
Statistical design
The mean, standard deviation, and range were noted for the continuous variables, and counts were noted for the categorical variables. All data were collected, measured, and reported with one decimal accuracy. The distribution of the numeric samples was assessed with the Kolmogorov-Smirnov normality test. Based on this preliminary analysis, parametric tests were adopted. To evaluate the significance of differences between pre-operative and post-operative values and between patient groups, a two-tailed paired sample Student’s t test, Fisher’s exact test, and χ2 test were used, when appropriate. A general linear model (GLM) repeated-measures ANOVA was conducted to test if outcomes significantly changed over time. Spearman’s correlations between residual pain and post-operative outcomes were calculated. To determine the variables influencing residual pain, a forward stepwise logistic regression was conducted with age (continuous), sex (male = 0; female = 1), novelty seeking (continuous), harm avoidance (continuous), reward dependence (continuous), persistence (continuous), joint (hip = 1; knee = 2), VAS score at t0 (continuous), HADS-A score at t0 (continuous), HADS-D score at t0 (continuous), functional score (HHS/KSS) at t0 (continuous), PCS score at t0 (continuous), MCS score at t0 (continuous), and WOMAC score at t0 (continuous) as independent variables. A p value < 0.05 was considered significant. IBM SPSS Statistics (version 21.0.0.1, IBM Corp., Armonk, NY, USA) software was used for the database construction and statistical analysis.
Results
The characteristics of the study population are summarized in Table 1. Pre-operatively, no significant differences were found between patients treated with THA and TKA, except for the body mass index, which was higher in patients with TKA than in patients with THA.
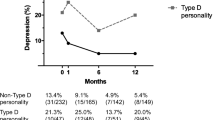
Significant reductions in pain and functional improvements were reported at the last follow-up (both p < 0.001) in both THA and TKA patients. Compared with TKA patients, THA patients showed earlier and greater functional improvement after surgery (both p < 0.001). As shown in Table 2 and Fig. 1, a significant time effect with a large effect size (ƞ2 > 0.5) was noted for all variables except for the SF-12 MCS score (ƞ2 = 0.12). Figure 2 illustrates the score variations (delta percentages between t0 and t5) over 12 months of follow-ups; the largest amounts of variation were found in the functional scores (HHS = 142.7 ± 115.5% and KSS = 182.5 ± 271.9%), and the smallest amounts of variation were found in the HADS-D score (− 8.8 ± 100.0% for THA and − 18.2 ± 51.4% for TKA) and the SF-12 MCS score (5.8 ± 37.0% for THA and 7.2 ± 29.4% for TKA). Comparing the surgical procedures, larger differences between the score at t0 and t5 were noted for the WOMAC (THA = 80.5 ± 15.5% vs TKA = 70.2 ± 19.1%; t = 2.694; p = 0.009) and SF-12 PCS (THA = 57.4 ± 54.3% vs TKA = 30.7 ± 41.6%; t = − 2.529; p = 0.013). No significant VAS differences were found between THA (1.7 ± 1.8) and TKA (2.0 ± 2.0) patients at t5. Residual pain was noted in 15% of the THA patients and 25% of the TKA patients, and the difference was not significant (χ2 = 1.425; df = 1; p = 0.233). Residual pain was correlated with the SF-12 PCS score (r2 = − 0.412; p < 0.001), SF-12 MCS score (r2 = − 0.473; p < .001), HADS-A score (r2 = 0.619; p = <0.001), HADS-D score (r2 = 0.559; p < 0.001), and the functional and WOMAC scores (r2 = − 0.482; p < 0.001 and r2 = 0.536; p < 0.001, respectively) at t5. As shown in Table 3, higher pre-operative harm avoidance, persistence, and anxiety scores were predictive of residual pain after THA and TKA (-2log Likelihood = 63.267; R2Nagelkerke = 0.349; X2 = 20.897; df = 3; p < 0.001).
Variation of VAS (a), HHS/KSS (b), and WOMAC (c) scores across 12 months. VAS, visual analogue scale; HHS, Harris hip score; KSS, Knee Society Scoring; WOMAC, Western Ontario and McMaster Universities Osteoarthritis Index, THA, total hip arthroplasty; TKA, total knee arthroplasty; T0, pre-operative; T1, 5 days post-operatively; T2, 1 month post-operatively; T3, 3 months post-operatively; T4, 6 months post-operatively; T5, 12 months post-operatively
Percentage deltas of tests scores across 12 months. VAS, visual analogue scale; HADS-A, Hospital Anxiety and Depression Scale-Anxiety; HADS-D, Hospital Anxiety and Depression Scale-Depression; PCS, physical component score of SF-12; MCS, mental component score of SF-12; HHS, Harris hip score; KSS, Knee Society Scoring; WOMAC, Western Ontario and McMaster Universities Osteoarthritis Index; THA, total hip arthroplasty; TKA, total knee arthroplasty
Discussion
The current study examined the role of personality traits, anxiety, and depression on residual pain in patients who undergo THA or TKA. These procedures significantly improved the functionality and pain of patients. THA patients showed earlier and greater functional improvement after surgery in comparison with TKA patients. Residual pain was noted in 15% of the THA patients and 25% of the TKA patients, and it was correlated with the SF-12 PCS, SF-12 MCS, HADS-A, HADS-D, functional, and WOMAC scores at t5. Higher pre-operative harm avoidance, persistence, and anxiety scores were predictive of residual pain after THA and TKA.
In the current study, as expected, THA patients showed earlier and higher functional improvement after surgery in comparison with TKA patients, and larger differences were noted between the pre-operative and 12-month post-operative WOMAC and SF-12 PCS scores. Lindner et al. reported that more post-operative pain, smaller improvements in range of movement and quality of life, and more physiotherapy sessions occurred after TKA than after THA [11]. Higher joint-specific and general health scores were reported six and 12 months after THA [12]. Higher WOMAC and SF PCS scores for THA patients than for TKA patients were reported three months [11], six months, and one year after surgery [8, 13].
A meta-analysis of 32 studies assessing the health-related quality of life of patients undergoing THA and TKA showed higher functional levels after THA at six- and 12-month follow-ups [14].
In the current study, residual pain was noted in 15% and 25% of the THA and TKA patients, respectively, and it was correlated with SF-12, HADS-A, HADS-D, functional, and WOMAC scores one year post-operatively. The proportion of patients complaining of residual pain in this study was similar to that in previous findings. In one systematic review, post-operative pain was reported in 9% and 20% of patients after THA and TKA, respectively [15]. Higher anxiety and depression in patients with residual pain could be considered a reaction to the pain itself. Improvements in pain and function after lower extremity total joint arthroplasty correlated with lower levels of psychological distress post-operatively [16].
The most important finding of this research concerns the predictors of residual pain: higher pre-operative harm avoidance, persistence, and anxiety scores were predictive of residual pain after THA and TKA. Harm avoidance and persistence are personality traits that represent specific autonomic response to given stimuli. Individuals presenting high levels of harm avoidance are described as cautious, fearful, doubtful, and apprehensive, with unusual sensitivity to criticism and punishment. Individuals with high levels of persistence present perseverance, methodical behaviours, meticulousness, and anticipatory anxiety and search for obsessive perfectionism. Several studies evaluated the influence of psychological factors on the outcome of joint arthroplasty [5]; however, as far as we know, only four studies investigated the role of personality traits in the outcome of THA and TKA patients. In details, three of these studies focused primarily on outcomes in general [17,18,19], and only one study assessed the effect of personality traits on persisting pain [6]. Ramaesh et al. found no independent effect of personality type using the Eysenck questionnaire on the post-operative scores in patients undergoing THA and TKA [17]. Similarly, Benditz et al., using the Freiburg Personality Inventory on 50 THA patients, found that personality traits did not relate to hip functionality five weeks post-operatively [18]. On the contrary, Badura-Brzoza et al. showed that neuroticism, a specific personality trait, is associated with mental and physical performance after 102 THA [19]. The studies previously reported [17,18,19] did not assess the effect of personality on residual pain, whereas Vogel et al. showed that type D personality (TDP) was linked to the persisting pain among 79 TKA patients [6]. TDP refers to a general inclination to psychological distress, with the main source of that distress being the components of TDP, negative affect, and social inhibition. To the best of our knowledge, the current study is the first one that have assessed the relationship between residual pain and personality traits in THA and TKA patients using the Cloninger’s psychobiological model that has been used to evaluate the relationship between specific temperamental traits and a wide variety of chronic pain conditions [3, 20]. The Cloninger’s psychobiological model has proved to be reliable, with internal consistency alpha coefficients ranging from 0.65 for persistence to 0.89 for cooperativeness. Interestingly, these data were confirmed by Fossati et al. that evaluated the reliability and validity of the Italian version of the TCI-R. The authors found that the internal consistency reliabilities ranged from 0.79 (reward dependence) to 0.91 (persistence) for the main TCI-R dimensions; moreover one month test-retest reliabilities ranged from 0.52 (novelty seeking) to 0.80 (self-transcendence), suggesting a moderate-to-good stability of TCI-R scores [4].
Several studies have suggested that high levels of harm avoidance and low levels of self-directedness are the most frequent personality features of chronic pain sufferers [21]. Nahman-Averbuch et al. showed less efficient inhibitory pain modulation responses to typify individuals with high scores of harm avoidance [22]. Following an acute pain experience, some patients are unable to resume their daily levels of activity and tend to regard pain as a threat [23]. Thus, patients execute automatic avoidance behaviours in relation to harmful stimuli to reduce the risk of feeling pain [24], which results in avoiding feared movement and activities.
In our sample, high levels of persistence were also predictive of residual pain. Persistence has been correlated with obsessive-compulsive symptoms, especially when associated with high levels of harm avoidance; it is known that high levels of harm avoidance and persistence indicate the possible presence of anxiety and depression [25].
We next demonstrated that anxious individuals were at greater risk of developing residual pain after THA or TKA. Anxiety and depression have been previously reported to be associated with post-operative pain after THA and TKA [7]. Desmeules et al. found that anxiety and depression influenced SF-36 PCS scores but not WOMAC pain and function scores in patients who underwent TKA [26]. Other predictors of residual pain after THA and TKA such as gender, pre-operative pain [9], comorbidities, body mass index, level of education, and social support have been previously described [15, 27]. In the current study, none of these factors was found to be associated with post-operative pain.
Although the sample size was not very large and bias can be expected from self-administered questionnaires, the prospective design; the number of pre- and post-operative assessments; the comprehensive evaluation of patients by validated tools including personality traits, affective dimensions, pain, quality of life, and joint functionality; and the statistical reliability produced by the forward stepwise logistic regression analysis represent considerable strengths of the present study.
THA patients showed earlier and greater functional improvement as well as less residual pain than TKA patients. Personality traits and anxiety predicted residual pain. In this light, pre-operative psychological evaluation using standardized questionnaires to investigate personality traits and anxiety could be helpful in identifying patients at risk for residual pain. Increased patient education and support before surgery are warranted in patient with psychological distress, and treatment can be delayed as long as the psychological symptoms are under control.
References
Hofmann S, Seitlinger G, Djahani O, Pietsch M (2011) The painful knee after TKA: a diagnostic algorithm for failure analysis. Knee Surg Sports Traumatol Arthrosc 19:1442–1452. https://doi.org/10.1007/s00167-011-1634-6
Izumi M, Petersen KK, Laursen MB et al (2017) Facilitated temporal summation of pain correlates with clinical pain intensity after hip arthroplasty. Pain 158:323–332. https://doi.org/10.1097/j.pain.0000000000000764
Conrad R, Schilling G, Bausch C et al (2007) Temperament and character personality profiles and personality disorders in chronic pain patients. Pain 133:197–209. https://doi.org/10.1016/j.pain.2007.07.024
Fossati A, Cloninger CR, Villa D et al (2007) Reliability and validity of the Italian version of the temperament and character inventory-revised in an outpatient sample. Compr Psychiatry 48:380–387
Sorel JC, Veltman ES, Honig A, Poolman RW (2019) The influence of preoperative psychological distress on pain and function after total knee arthroplasty: a systematic review and meta-analysis. Bone Joint J 101-B:7–14. https://doi.org/10.1302/0301-620X.101B1.BJJ-2018-0672.R1
Vogel M, Riediger C, Krippl M et al (2019) Negative affect, type D personality, quality of life, and dysfunctional outcomes of total knee arthroplasty. Pain Res Manag 2019:1–9. https://doi.org/10.1155/2019/6393101
Duivenvoorden T, Vissers MM, Verhaar JAN et al (2013) Anxiety and depressive symptoms before and after total hip and knee arthroplasty: a prospective multicentre study. Osteoarthr Cartil 21:1834–1840. https://doi.org/10.1016/j.joca.2013.08.022
Zhai H, Geng H, Bai B, Wang Y (2019) Differences in 1-year outcome after primary total hip and knee arthroplasty : a cohort study in older patients with osteoarthritis. Orthopade 48:136–143. https://doi.org/10.1007/s00132-018-3636-2
Erlenwein J, Müller M, Falla D et al (2017) Clinical relevance of persistent postoperative pain after total hip replacement – a prospective observational cohort study. J Pain Res 10:2183–2193. https://doi.org/10.2147/JPR.S137892
van der Wees PJ, Wammes JJ, Akkermans RP et al (2017) Patient-reported health outcomes after total hip and knee surgery in a Dutch University Hospital Setting: results of twenty years clinical registry. BMC Musculoskelet Disord 18:97. https://doi.org/10.1186/s12891-017-1455-y
Lindner M, Nosseir O, Keller-Pliessnig A et al (2018) Psychosocial predictors for outcome after total joint arthroplasty: a prospective comparison of hip and knee arthroplasty. BMC Musculoskelet Disord 19:159. https://doi.org/10.1186/s12891-018-2058-y
Hamilton D, Henderson GR, Gaston P et al (2012) Comparative outcomes of total hip and knee arthroplasty: a prospective cohort study. Postgrad Med J 88:627–631. https://doi.org/10.1136/postgradmedj-2011-130715
Liebensteiner M, Wurm A, Gamper D, Oberaigner W, Dammerer D, Krismer M (2019) Patient satisfaction after total knee arthroplasty is better in patients with pre-operative complete joint space collapse. Int Orthop 43:1841–1847. https://doi.org/10.1007/s00264-018-4185-3
Ethgen O, Bruyère O, Richy F et al (2004) Health-related quality of life in total hip and total knee arthroplasty. A qualitative and systematic review of the literature. J Bone Joint Surg Am 86:963–974. https://doi.org/10.2106/00004623-200405000-00012
Beswick AD, Wylde V, Gooberman-Hill R et al (2012) What proportion of patients report long-term pain after total hip or knee replacement for osteoarthritis? A systematic review of prospective studies in unselected patients. BMJ Open 2:e000435. https://doi.org/10.1136/bmjopen-2011-000435
Hassett AL, Marshall E, Bailey AM et al (2018) Changes in anxiety and depression are mediated by changes in pain severity in patients undergoing lower-extremity total joint arthroplasty. Reg Anesth Pain Med 43:14–18. https://doi.org/10.1097/AAP.0000000000000682
Ramaesh R, Jenkins P, Macdonald D et al (2014) Personality, function and satisfaction in patients undergoing total hip or knee replacement. J Orthop Sci 19:275–281. https://doi.org/10.1007/s00776-013-0509-8
Benditz A, Jansen P, Schaible J et al (2017) Psychological factors as risk factors for poor hip function after total hip arthroplasty. Ther Clin Risk Manag 13:237–244. https://doi.org/10.2147/TCRM.S127868
Badura-Brzoza K, Zajac P, Brzoza Z et al (2009) Psychological and psychiatric factors related to health-related quality of life after total hip replacement - preliminary report. Eur Psychiatry 24:119–124. https://doi.org/10.1016/j.eurpsy.2008.06.009
Gustin SM, Burke LA, Peck CC et al (2016) Pain and personality: do individuals with different forms of chronic pain exhibit a mutual personality? Pain Pract 16:486–494. https://doi.org/10.1111/papr.12297
Naylor B, Boag S, Gustin SM (2017) New evidence for a pain personality? A critical review of the last 120 years of pain and personality. Scand J Pain 17:58–67. https://doi.org/10.1016/j.sjpain.2017.07.011
Nahman-Averbuch H, Yarnitsky D, Sprecher E et al (2016) Relationship between personality traits and endogenous analgesia: the role of harm avoidance. Pain Pract 16:38–45. https://doi.org/10.1111/papr.12256
Burns LC, Ritvo SE, Ferguson MK et al (2015) Pain catastrophizing as a risk factor for chronic pain after total knee arthroplasty: a systematic review. J Pain Res 8:21–32. https://doi.org/10.2147/JPR.S64730
Vlaeyen JW, Linton SJ (2000) Fear-avoidance and its consequences in chronic musculoskeletal pain: a state of the art. Pain 85:317–332
Halvorsen M, Wang CE, Richter J et al Early maladaptive schemas, temperament and character traits in clinically depressed and previously depressed subjects. Clin Psychol Psychother 16:394–407. https://doi.org/10.1002/cpp.618
Desmeules F, Dionne CE, Belzile ÉL et al (2013) Determinants of pain, functional limitations and health-related quality of life six months after total knee arthroplasty: results from a prospective cohort study. BMC Sports Sci Med Rehabil 5:2. https://doi.org/10.1186/2052-1847-5-2
Núñez-Cortés R, Chamorro C, Ortega-Palavecinos M, Mattar G, Paredes O, Besoaín-Saldaña Á, Cruz-Montecinos C (2019) Social determinants associated to chronic pain after total knee arthroplasty. Int Orthop 43:2767–2771. https://doi.org/10.1007/s00264-019-04370-6
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by Michele Mercurio, Cristina Segura-Garcia, and Giorgio Gasparini. The first draft of the manuscript was written by Michele Mercurio, Cristina Segura-Garcia, Giorgio Gasparini, and Olimpio Galasso, and all authors commented on previous versions of the manuscript. Elvira Anna Carbone aided in interpreting the results and worked on the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Ethical approval
“All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee (Mater Domini Ethics committee n. 14/2015) and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.”
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Mercurio, M., Gasparini, G., Carbone, E.A. et al. Personality traits predict residual pain after total hip and knee arthroplasty. International Orthopaedics (SICOT) 44, 1263–1270 (2020). https://doi.org/10.1007/s00264-020-04553-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-020-04553-6