Abstract
Background
The majority of arthroplasty surgeons use a full duration of tourniquet while doing total knee arthroplasty. Recent literature suggests clinical dilemma about superior function with limited duration use of a tourniquet. The purpose of this study is to evaluate the time-dependent effects and clinical outcome of tourniquet in patients undergoing total knee arthroplasty (TKA) and to assess the incidence of adverse vascular events of the limb in TKA. This study is the first of its kind to evaluate all the serious vascular events prospectively.
Methods
Sixty participants who underwent TKA in the duration of 1.5 years at a large single tertiary care centre were recruited and randomly allocated in two groups: Full duration tourniquet (n = 30) and tourniquet only during cementation (n = 30). All patients underwent preoperative and postoperative arterial and venous Doppler to evaluate the presence of thrombosis. The operative duration, blood loss, and clinical outcome (visual analogue scale, active knee range of motion, Knee Society score, and duration of stay) were recorded.
Results
The incidence of vascular complications was not statistically significant in either group (P = 0.99). Tourniquet during cementation only group exhibited decreased postoperative pain on days 1, 2, and 3 (P < 0.01). But postoperative knee active range of motion was the same between the two groups with no significant postoperative complications.
Conclusion
Tourniquet use only during cementation could result in faster recovery and less pain during the early rehabilitation period with no influence over the incidence of serious vascular events.
Trial Registry Number
AIIMS/IEC/2018/475. This study was approved by the Research Ethics Committee at All India Institute of Medical Sciences, Jodhpur and was carried out at AIIMS (Jodhpur), India.
Graphic abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The recent trend with the tourniquet use in total knee arthroplasty (TKA) is to reconsider the routine use to enhance pain relief and improving the quality of life [1]. Orthopaedic surgeons extensively use the tourniquet in TKA to provide a clear surgical field visualisation, ensuring better cementation in terms of cement bone interdigitation and reduced intraoperative blood loss [2]. Most of the complications are time-dependent complications [3]; only few investigators have focused on the limited application of a tourniquet to reduce the tourniquet time and its incidence of complications [4]. The main thrombotic complications of tourniquet use are Deep Vein Thrombosis (DVT) and arterial thrombosis [5]. Arterial injury associated with total knee arthroplasty is a rare and potentially devastating complication. The injury is associated with a significant increase in the duration of hospital stay and hospital charges [6, 7]. Several studies have asserted that the risk of significant arterial injury increases with tourniquet use, suggesting that tourniquet use should be minimised for routine primary TKA [8,9,10]. A high origin anterior tibial artery lying posterior to the popliteus is the most common type of 'high branch' is an anatomical variation around the knee are not well studied in the context of TKA and is vulnerable during TKA [11].
However, there is continuing debate on the optimal timing of tourniquet application. The purpose of this prospective, double-blinded, randomised controlled study was to assess whether the use of tourniquets only during cementation vs during the full length of surgery will show any difference in the rate of postoperative thrombotic complications in patients undergoing TKA. In addition, in this study, we looked for an anatomical variation of popliteal artery division in patients undergoing TKA. The effect of tourniquet use on functional and clinical outcomes was also evaluated.
Material and Methods
Study Cohort
This study was approved by the institutional review board (IRB), the ethical committee number is AIIMS/IEC/2018/475. The inclusion criteria were advanced osteoarthritis of knee patients undergoing total knee replacement between January 2018 and June 2019 and informed consent was obtained from all individual participants included in this study. The exclusion criteria included coagulopathy, uncontrolled hypertension, uncontrolled diabetes mellitus, and peripheral vascular disease.
Randomisation
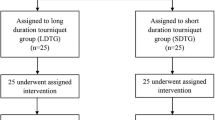
Each patient undergoing total knee arthroplasty was randomly allocated to either full duration tourniquet use or tourniquet use only during cementation (tourniquet inflated just before the cement application and deflated after its hardening and initiation of closure, i.e. two stitches in the quadriceps, one proximal to the patella and one distal to patella). The randomisation sequence was generated by an independent statistician via a computer-generated random number table who was not involved in patient management using Microsoft Excel (Microsoft Inc, Redmond, WA, USA). The randomisation numbers were contained in sealed, opaque (SNOSE technique) envelopes and were retained by a staff who was not involved in outcome measurements. The patients were randomised as individual patients and not as individual knee. The observers collecting data after surgery were uninvolved in the experimental operations and were unaware of the intervention assignments. Randomisation was blinded to the investigator, nursing staff of the inpatient unit, rehabilitation therapists, and the patient. A detailed description of the randomisation procedure is given in the CONSORT Flow diagram in Fig. 1
Preoperative Assessment
Sixty patients undergoing TKA agreed to participate in the randomised study. Demographics of age, sex, diagnosis, and body mass index did not differ (Table 1). All patients underwent preoperative Doppler ultrasound for the arterial, venous system of the lower limb, and all patients were investigated for high origin anterior tibial artery. The anterior tibial artery, which arises from popliteal artery in the popliteal fossa proximal to the popliteus above the middle portion of the posterior surface of the popliteus is defined as ‘high origin- anterior tibial artery’ [12]. All patients who did not have arterial or venous complications were included in this study. The Doppler study of the limb to be operated was performed by a radiologist with at least eight years of experience using a high-frequency linear probe (5–11 MHz), Logiq S8, GE USA. For examinations of a preoperative or postoperative TKA patient, for the venous system of the lower limb, Gray scale images and spectral Doppler waveforms were recorded. For the arterial system of the limb, waveforms in the appropriate arterial segments were looked for abnormality.
Operative Procedure and Postoperative Period
All patients underwent either bilateral simultaneous total knee arthroplasty or unilateral total knee arthroplasty, after randomisation for tourniquet use. One group had tourniquet inflation from the incision through the full duration of surgery till cementation of the implants (operative tourniquet) and the other group had tourniquet inflation only during the cementation of the implants (tourniquet during cementation only). In the operating room before surgery, the nursing assistant opened the sealed cover and informed the surgeons to which group the patient belonged. All patients received the same anaesthesia, combined spinal epidural (no narcotics in the epidural). The epidural catheter was discontinued on the first postoperative day. All operations were performed by two senior arthroplasty surgeons with 10 years of experience in arthroplasty. A midline skin incision and trivector medial parapatellar approach were used in all patients. The duration of surgery from the incision till the end of dressing and the duration of tourniquet inflation were recorded from the tourniquet machine directly (Zimmer ATS 3000 pneumatic tourniquet). The limb was exsanguinated by lifting up for 1 min before tourniquet inflation.
The primary outcomes were to ascertain the incidence of thrombotic complications post-TKA (Arterial and Venous Thrombosis on postoperative day 5 and day 21) and incidence of high origin anterior tibial artery in the population undergoing TKA. Secondary outcome measures, which were the assessment of blood loss based on the Gauze Visual Analogue method intraoperatively and postoperatively by haemogram; assessment of pain by Visual Analogue Scoring (VAS) on postoperative days 1, 2, 3, and on the 21st day; postoperative range of motion on 21st day; duration of hospital stay; and complications, such as pulmonary embolism and surgical site infection (superficial and deep), were noted for comparison between both groups. Arterial thrombosis and deep venous thrombosis assessment were performed on postoperative day 5 and day 21 by clinical examination and Doppler ultrasonography. The patients were screened thoroughly for DVT and arterial thrombosis in the operated lower limb. The patients were monitored for symptomatic pulmonary embolism for 3 weeks post-surgery. The primary outcomes of this study, which are DVT, arterial thrombosis, and pulmonary embolism, are grouped as ‘adverse vascular events’.
Blood loss was measured intraoperatively from the drainage collection and blood loss estimation of lap sponges was typically indirectly calculated by estimating the amount of blood absorbed by sponges and gauze using the Gauze Visual Analogue method as described by Algadiem et al. [13]. Patients were given both mechanical and chemical thromboprophylaxis. The pain management protocol used was identical between the two study groups. The patient’s pain was self-graded and recorded by investigator on VAS, using the visual analogue score at an interval of 24 h on a postoperative day one to three and on postoperative day 21. The patient's knee ROM was measured on postoperative days 5 and 21. The patient's Knee Society score was documented preoperatively and postoperatively on day 21 [14]. The patients were monitored for the duration of hospital stay and complications, like pulmonary embolism and surgical site infection. Only patients with clinical symptoms of pulmonary embolism were referred for pulmonary medicine consultation and radiological investigation (computed tomographic pulmonary angiography) [15].
Statistical Analysis
Continuous variables are expressed as means ± standard deviation or medians with IQR, and categorical variables are presented as frequencies or percentages. The Shapiro–Wilks test was used to test for normal distribution. The non-parametric Kruskal–Wallis test was used to test the differences in two group. P values < 0.05 were considered significant. Commercially available software was used (SPSS, release 26.0; SPSS, Chicago, IL).
Results
Participant Characteristics
There were 24 males and 36 females in the two groups. Demographic characteristics are summarised in Table 1. There was no significant difference in age, preoperative final knee score, knee function score, and ROM between the two groups. There were twenty-three simultaneous bilateral total knee arthroplasty participants in this study.
Comparison Between the Two Groups (Full Duration Tourniquet Group and Tourniquet only During Cementation Group)
The incidence of postoperative DVT was nil in full duration tourniquet group and 3.3% in tourniquet only during cementation group; the incidence was not statistically significant (P = 0.99) (Table 2). One patient in each group had postoperative arterial thrombosis, and both the patients were asymptomatic (Table 2). No patient in our study had an anomalous high origin anterior tibial artery. Two patients developed pulmonary embolism.
The mean postoperative pain scores at days 1, 2, and 3 were 5.6 ± 1.2, 4.0 ± 0.9, and 3.0 ± 1.2, respectively, in full duration tourniquet group and 3.4 ± 1.3, 2.3 ± 1.0, and 1.4 ± 1.1, respectively, in tourniquet only during cementation group and were statistically significant (P value, < 0.01). No statistically significant differences (P value = 0 0.54) were found in VAS score between the two groups at postoperative day 21 (Fig. 2).
The group with full duration tourniquet use had less intraoperative blood loss than the tourniquet only during the cementation group (tourniquet during full duration: 162.95 ± 108.62 mL versus tourniquet only during cementation group: 448.33 ± 147.08 mL, P < 0.01). 75.7 ± 2.5 and 75.3 ± 3.8 are postoperative KSS values at day 21 of the full duration tourniquet and tourniquet only during cementation group; statistically significant differences (P value < 0.001) were between the preoperative KSS value and postoperative KSS value of the full duration tourniquet group (Preop KSS 34.5, Postop KSS 75.7) and the tourniquet at cementation only group (Preop KSS 41.1, Postop KSS 75.3).
There is no significant difference in the postoperative haemoglobin, duration of surgery, active range of motion on day 21, surgical site infection, duration of hospital stay, and pulmonary embolism (Table 3). None of the patient received blood transfusion in both the groups.
Discussion
In the present study, the outstanding finding was that no difference was observed in the incidence of postoperative adverse vascular complications of venous or arterial systems with tourniquet use during the full duration of surgery and tourniquet only during cementation; but the tourniquet only during cementation group showed significantly less postoperative pain in the immediate postoperative period (days 1, 2, and 3); however, this group had increased intraoperative blood loss, and there was no significant difference in postoperative range of motion of the knee, haemoglobin levels, and VAS score at 21st day. The prevalence of abnormal high origin anterior tibial artery was not found in any patient who underwent TKA in this study. This RCT have studied the incidence of both arterial thrombosis and venous thrombosis prospectively after total knee arthroplasty.
There is no clear consensus in the literature regarding different aspects of tourniquet use in TKA. There is an increased risk of DVT formation due to stasis of venous blood in the lower limb with the use of a tourniquet and increased manipulation of the knee joint while performing the surgery; moreover, the surgery itself is a predisposing factor for venous thromboembolism (VTE) as it is a major lower limb surgery involving a high degree of manipulation of the knee joint. DVT is one of the top five causes of readmission within 30 days after surgery [16]. None of the patients in either of the two groups in the present study required readmission within 30 days from surgery for symptomatic DVT. Asymptomatic DVT was detected on day 5 in Doppler study in 1 patient in the tourniquet during cementation group. This patient was put on oral anticoagulation for 6 weeks in addition to mechanical prophylaxis and on Aspirin 75 mg for 3 months. The current study did not reveal any significant difference in the rate of DVT in the postoperative period between full duration tourniquet and tourniquet at cementation only group (Fig. 3). These results were consistent with those of previous studies [17,18,19,20]. The incidence of DVT is 3% which matched with the latest meta-analysis published in the year 2021 [1]. Goel et al. in 2019 reported no incidence of symptomatic DVT in the patients who underwent surgery with full duration tourniquet with a follow-up of 6–8 months [21]. Wang et al. conducted a cross-over trial in 2016 in patients who underwent staged bilateral TKA. Two patients with full duration tourniquet use developed asymptomatic DVT on postoperative day 7 [22]. In both the above studies, preoperative screening for DVT was not performed. On the contrary, in our study preoperative screening was performed to diagnose pre-existing DVT and arterial disease in our study. The patients with pre-existing DVT and arterial disease were excluded from our study.
The incidence of arterial thrombosis following TKA is lower than that might be expected, particularly considering the proximity of the arteries to the knee joint both in extension and flexion and also since most patients requiring the procedure are in the older age group in which there is a higher incidence of peripheral vascular disease, diabetes mellitus, hypertension, and dyslipidemia. In this study, two patients developed arterial thrombosis, one in each group. Both these patients were managed by therapeutic anticoagulation, not requiring any surgical intervention. The incidence was not statistically significant between the two groups. The incidence of arterial thrombosis post-TKA is rare, approximately 0.003% [8], thereby also implying that not all TKA centres, especially the low volume centres, shall witness this particular complication. There is no level 1 evidence till date highlighting the correlation of structural anterior tibial artery variations and incidence of arterial injury and /or thrombosis with respect to tourniquet usage during TKA. The only available literature regarding the same is in the form of case reports [23]. Statz et al. observed that there was no difference between the full or selective tourniquet usage group during TKA, and concluded that tourniquet use did not have any effect on the rate of geniculate artery injury [24]. These results correlated with our study that tourniquet use does not influence the incidence of arterial injury. Padegimas et al. conducted a retrospective single institutional study at Pennsylvania in 2016, 9951 knees were studied in which 0.13% developed an arterial injury in all the patients the tourniquet was used [25], but they did not have full access to demographic, clinical, radiographic, or operative variables of all TKA patients over the study period and there was no standard protocol was followed by the operating surgeon. In our study, we had a standard protocol of physical and radiological examination in the pre- and postoperative period. All the above studies are retrospective studies and case reports without proper preoperative evaluation parameters of risk factors that influence arterial thrombosis or arterial injury. The main strength of this study was a thorough preoperative documentation of the arterial system by clinical and Doppler study of the operative limb which aided postoperative evaluation for any changes, injury or thrombosis in addition to the clinical vascular examination. The prevalence of high origin anterior tibial artery is 1.9% to 4.2% in the cadaveric and angiographic study [7], with a high predisposition to injury when the tibial cut is taken using an oscillating saw. In the present study, none of the patients had a high origin anterior tibial artery on the Doppler ultrasound study.
One of the main aims of TKA is to give a painless joint, and immediate physiotherapy remains a keystone for the success of the surgery. Wang et al. suggested that tourniquet only at the cementation exhibited reduced thigh and knee pain on days 1 and 2 postoperatively compared with the long duration tourniquet group [22]. Tarwala et al. found that mean pain score between patients with full duration tourniquet and tourniquet only at cementation was not statistically different at any time point; this might be due to the multimodality perioperative pain management protocol which was not clear whether it was given as infusion postoperatively or as a single-injection popliteal nerve block; these factors might have masked the initial postoperative difference in pain [26]. The reason is that tourniquet causes direct muscle damage and reperfusion injury, which causes the pain. In this study, there were significant low pain scores in the initial postoperative days in the tourniquet only during the cementation group, which is also clinically significant as we observed there was less analgesic consumption in the tourniquet only during the cementation group when compared to the full duration tourniquet group. The same observation has been made in a systematic review and meta-analysis by Liu et al. [27], wherein the authors have highlighted their finding that 'not using a tourniquet or only using it during the cementation of implants was preferable based on faster functional recovery, lower rate of DVTs and complications compared with using a tourniquet throughout the TKA procedure'. In another systematic review by Burns et al. [28], pain catastrophisation post-TKA has been identified as an independent risk factor for chronic pain post-TKA with a moderate level of evidence. The results of this study add considerable significance to the finding of decreased pain and lower VAS in the early postoperative period, in the tourniquet at cementation only group in our study, as these patients will have a better functional recovery than those having higher VAS scores during the early postoperative period and developing chronic pain post-TKA, thereby becoming contenders for unhappy patients post-TKA.
Two patients in the full duration tourniquet group developed symptomatic pulmonary embolism. The patients recovered absolutely with appropriate treatment. The incidence was not statically significant but correlated with prevailing literature. Nishiguchi et al. revealed an incidence of 7% of PE with the use of a full duration tourniquet during the surgery [29]. In this study, there was significantly less intraoperative blood loss observed in the full duration tourniquet group than in the tourniquet only duration cementation group. The findings of our study, which are similar to the observation of other previous authors, indicate decreased intraoperative blood loss with tourniquet use [17, 22], and this is one of the important factors for which tourniquet is used, as it provides a clear bloodless surgical field. There was no significant difference observed in the active ROM postoperatively in the initial postoperative period and at 3 weeks. Liu et al. [27] concluded that patients who underwent surgery without a tourniquet had improved ROM. Tai et al. [12] and Hasanain et al. [17] have concurrent findings with the present study that a tourniquet during the full duration of TKA affects the overall rehabilitation effect. However, the results of the latter study are challenging to interpret because the types of physiotherapy protocols used in other studies are not the same. The present study found no difference in length of the hospital stay, contrary to Rames et al. [30]. They suggested short duration tourniquet had early discharge rates, which had no economic burden on the patients, and complication rates, such as surgical site infection and pulmonary embolism, were also not significant.
We noticed from our study that the use of full duration tourniquet during the whole surgery provides better visibility intraoperatively, reduces the operating time, and also reduces intraoperative blood loss significantly as compared to tourniquet use only during cementation. The limitations are the small sample size to ascertain thrombotic events after TKA and the incidence of high origin of the anterior tibial artery. Doppler Ultrasound is a user-dependent modality with intra- and interobserver variations, which can affect the quality of observations.
Conclusion
We conclude that, with modern perioperative protocols, tourniquet use during cementation only strategy of modern TKA is not associated with serious vascular complications with evidence of superior in-hospital patient function in terms of postoperative pain on days 1, 2, and 3, when compared with patients where a tourniquet was utilised during the full duration of the surgery. However, limited duration tourniquet use can be associated with faster recovery in terms of pain during the immediate postoperative and early rehabilitation period.
References
Ahmed, I., Chawla, A., Underwood, M., Price, A., Metcalfe, A., Hutchinson, C., et al. (2021). Time to reconsider the routine use of tourniquets in total knee arthroplasty surgery. The Bone & Joint Journal, 103B(5), 830–839.
Mylod, J. A., France, M. P., Muser, D. E., & Parsons, J. R. (1990). Perioperative blood loss associated with total knee arthroplasty. A comparison of procedures performed with and without cementing. The Journal of Bone and Joint Surgery, 72(7), 1010–1012.
Hernandez, A. J., Almeida, A. M., Favaro, E., & Sguizzato, G. T. (2012). The influence of tourniquet use and operative time on the incidence of deep vein thrombosis in total knee arthroplasty. Clinics (São Paulo), 67(9), 1053–1057.
Fukuda, A., Hasegawa, M., Kato, K., Shi, D., Sudo, A., & Uchida, A. (2007). Effect of tourniquet application on deep vein thrombosis after total knee arthroplasty. Archives of Orthopaedic and Trauma Surgery, 127(8), 671–675.
Langkamer, V. G. (2001). Local vascular complications after knee replacement: a review with illustrative case reports. The Knee, 8(4), 259–264.
Rush, J., Vidovich, J., & Johnson, M. (1987). Arterial complications of total knee replacement. The Australian experience. Journal of Bone and Joint Surgery, 69B, 400.
Dua, A., Zepeda, R., Hernanez, F. C., Igbadumhe, A. A., & Desai, S. S. (2015). The national incidence of iatrogenic popliteal artery injury during total knee replacement. Vascular, 23(5), 455–458.
Ammori, M. B., Evans, A. R., & Mclain, A. D. (2016). Popliteal artery pseudoaneurysm after total knee arthroplasty. The Journal of Arthroplasty., 31(9), 2004–2007.
Arthur, J., & Spangehl, M. (2019). Tourniquet use in total knee arthroplasty. Journal of Knee Surgery. https://doi.org/10.1055/s-0039-1681035
Jawhar, A., Stetzelberger, V., Kollowa, K., & Obertacke, U. (2019). Tourniquet application does not affect the periprosthetic bone cement penetration in total knee arthroplasty. Knee Surgery, Sports Traumatology, Arthroscopy, 27(7), 2071–2081.
Tindall, A., Shetty, A., James, K., Middleton, A., & Fernando, K. (2006). Prevalence and surgical significance of a high-origin anterior tibial artery. Journal of Orthopaedic Surgery, 14(1), 13–16.
Tai, T.-W., Lin, C.-J., Jou, I.-M., Chang, C.-W., Lai, K.-A., & Yang, C.-Y. (2011). Tourniquet use in total knee arthroplasty: a meta-analysis. Knee Surgery, Sports Traumatology, Arthroscopy, 19(7), 1121–1130.
Ali Algadiem, E., Aleisa, A., Alsubaie, H., Buhlaiqah, N., Algadeeb, J., & Alsneini, H. (2016). Blood loss estimation using gauze visual analogue. Trauma Monthly. https://doi.org/10.5812/traumamon.34131
Insall, J. N., Dorr, L. D., Scott, R. D., & Scott, W. N. (1989). Rationale of the Knee Society clinical rating system. Clinical Orthopaedics and Related Research, 248, 13–14.
Bin Abd Razak, H., Binte Abd Razak, N., & Tan, H. (2017). Prevalence of venous thromboembolic events is low in asians after total knee arthroplasty without chemoprophylaxis. The Journal of Arthroplasty, 32(3), 974–979.
Curtis, G., Jawad, M., Samuel, L., George, J., Higuera-Rueda, C., Little, B., et al. (2019). Incidence, causes, and timing of 30-day readmission following total knee arthroplasty. The Journal of Arthroplasty, 34(11), 2632–2636.
Hasanain, M., Apostu, D., Alrefaee, A., & Tarabichi, S. (2018). Comparing the effect of tourniquet vs tourniquet-less in simultaneous bilateral total knee arthroplasties. The Journal of Arthroplasty, 33(7), 2119–2124.
Liu, P., Li, D., Zhang, Y., Lu, Q., Ma, L., Bao, X., et al. (2017). Effects of unilateral tourniquet used in patients undergoing simultaneous bilateral total knee arthroplasty. Orthopaedic Surgery, 9(2), 180–185.
Song, K., Xu, Z., Rong, Z., Yang, X., Yao, Y., Shen, Y., et al. (2016). The incidence of venous thromboembolism following total knee arthroplasty. Blood Coagulation & Fibrinolysis, 27(3), 266–269.
Mittal, R., Ko, V., Adie, S., Naylor, J., Dave, J., Dave, C., et al. (2012). Tourniquet application only during cement fixation in total knee arthroplasty: a double-blind, randomised controlled trial: RCT tourniquet during cementing in TKA. ANZ Journal of Surgery, 82(6), 428–433.
Goel, R., Rondon, A., Sydnor, K., Blevins, K., O’Malley, M., Purtill, J., et al. (2019). Tourniquet use does not affect functional outcomes or pain after total knee arthroplasty. The Journal of Bone and Joint Surgery, 101(20), 1821–1828.
Wang, K., Ni, S., Li, Z., Zhong, Q., Li, R., Li, H., et al. (2017). The effects of tourniquet use in total knee arthroplasty: a randomised, controlled trial. Knee Surgery, Sports Traumatology, Arthroscopy, 25(9), 2849–2857.
Sharma, K., Haque, M., & Mansur, D. (2012). Bilateral high-origin anterior tibial arteries and its clinical importance. Kathmandu University Medical Journal, 10(1), 83–84.
Statz, J., Ledford, C., Chalmers, B., Taunton, M., Mabry, T., & Trousdale, R. (2018). Geniculate artery injury during primary total knee arthroplasty. American Journal of Orthopedics. https://doi.org/10.1278/ajo.2018.0097
Padegimas, E. M., Levicoff, E. A., McGinley, A. D., Sharkey, P. F., & Good, R. P. (2016). Vascular complications after total knee arthroplasty—a single institutional experience. The Journal of Arthroplasty, 31(7), 1583–1588.
Tarwala, R., Dorr, L. D., Gilbert, P. K., Wan, Z., & Long, W. T. (2014). Tourniquet use during cementation only during total knee arthroplasty: a randomised trial. Clinical Orthopaedics and Related Research, 472(1), 6.
Liu, Y., Si, H., Zeng, Y., Li, M., Xie, H., & Shen, B. (2019). More pain and slower functional recovery when a tourniquet is used during total knee arthroplasty. Knee Surgery, Sports Traumatology, Arthroscopy, 28(6), 1842–1860.
Burns, L., Ritvo, S., Ferguson, M., Clark, H., & Seltzer, Z. (2015). Katz J (2015) Pain catastrophizing as a risk factor for chronic pain after total knee arthroplasty: a systematic review. Journal of Pain Research, 8, 21–32.
Nishiguchi, M., Takamura, N., Abe, Y., Kono, M., Shindo, H., & Aoyagi, K. (2005). Pilot study on the use of tourniquet: a risk factor for pulmonary thromboembolism after total knee arthroplasty? Thrombosis Research, 115(4), 271–276.
Rames, R. D., Haynes, J., Hellman, M., Barrack, T., & Barrack, R. (2019). Impact of tourniquet strategy on perioperative results of modern TKA. Journal of Knee Surgery. https://doi.org/10.1055/s-0039-1688919
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
JN did preoperative evaluation, enrolled patients, randomisation, participated in the design of the study, performed statistical analyses, and wrote the manuscript. AE and SB coordinated and did the surgeries and contributed in writing the manuscript. AE and SB have reviewed and analysed the data and attest to the integrity of the original data reported in this manuscript. PKG did the preoperative and postoperative radiological evaluation of the patients in this study.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethics Approval
The study was performed only after the approval of the Research Ethics Committee (AIIMS/IEC/2018/475).
Informed Consent
For this study informed consent was obtainted from the participants.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Netaji, J., Banerjee, S., Garg, P.K. et al. Reappraisal of Limited Duration Tourniquet in Total Knee Arthroplasty: A Double-Blinded RCT. JOIO 55, 1186–1194 (2021). https://doi.org/10.1007/s43465-021-00506-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43465-021-00506-2