Abstract
Study design
Retrospective review of consecutive series.
Objective
To assess the clinical and radiographic outcomes after surgical management of post-tuberculous kyphosis.
Summary of background data
Post-tuberculous (TB) kyphosis can lead to progressive pulmonary and neurological deterioration. Surgery is indicated to decompress neural elements and correct the spine deformity. Although posterior vertebral column resection (PVCR) has been established as the treatment of choice for severe TB kyphosis, there is paucity of studies on the clinical outcomes among patients treated in West Africa.
Methods
Clinical and radiographic data of 57 patients (pts) who underwent surgical correction of post-TB kyphosis at a single site in West Africa between 2013 and 2018 (≥ 2-year follow-up in 36 pts, ≥ 1-year FU in 21 pts). Pre- and post-op SRS scores and radiographic outcomes were compared using Paired t test.
Results
57 patients, 36M:21F. Mean age 19 (11–57 years). 22/57 pts (39.3%) underwent pre-op halo gravity traction (HGT) for an average duration of 86 days (8–144 days). HGT pts had a higher baseline regional kyphosis (125.1 ± 20.9) compared to non-HGT pts (64.6 ± 31.8, p < 0.001). Post-HGT regional kyphosis corrected to 101.2 ± 23 (24° correction). 53 pts (92.9%) underwent posterior-only surgery and 4 (7.0%) combined anterior–posterior surgery. 39 (68.4%) had PVCR, 11 (19.3%) PSO, and 16 (28.1%) thoracoplasty. Intraoperative neuromonitoring (IOM) signal changes occurred in 23/57 pts (≈ 40%), dural tear in 5 pts (8.8%), pleural tear in 3 pts (5.3%), ureteric injury in 1 pt (1.7%), and vascular injury in 1 pt (1.7%). Post-op complications included four (7.0%) infection, three (5.3%) implant related, two (3.5%) radiographic (one PJK and one DJK), one (1.7%) neurologic, one (1.7%) wound problem, and two (3.5%) sacral ulcers. IOM changes were similar in the VCR (48.7%) and non-VCR (23.5%) pts, p > 0.05. Complication rates were similar among HGT and non-HGT groups. Significant improvements from baseline were seen in the average SRS Total and domains scores and radiographic measurements for patients who attained 2-year follow-up.
Conclusion
PVCR ± HGT can provide safe and optimal correction in cases of severe post-TB kyphosis with good clinical and radiographic outcomes in underserved regions.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Tuberculosis is considered one of the oldest infections known to man with an estimated 30 million people suffering an active TB infection worldwide. Skeletal TB may be present in up to 10% of patients, of whom 50% (estimated 2 million) have a spinal involvement [1,2,3].
Recently, there has been a dramatic increase in the numbers of TB patients in developing countries, mostly in association with Human Immunodeficiency Virus (HIV) infections. Still, TB remains more associated with low-socioeconomic status which is a problem in developing countries particularly in Africa [4, 5].
Chemotherapy is the treatment of choice for uncomplicated spinal TB which can still lead to an average residual deformity of 15º. Up to 5% of patients develop a deformity higher than 60º with conservative treatment [6,7,8,9]. Patients presenting with neurological deficits, instability or progressive deformity require early surgical decompression and stabilization to limit complications [9, 10].
Post-TB kyphosis is especially problematic in pediatric patients, particularly those under the age of 5 years, as it continues to worsen with growth, leading to progressive spinal deformity [11, 12].
Progressive spine deformity, not only leads to functional and psychological impairment but can also result in restrictive cardiopulmonary disease and potential neurologic deficits even many years after resolution of the initial infection. These complications can be avoided by early surgical decompression and correction of kyphosis if it increases beyond 60° [13,14,15].
In such patients, circumferential resection of the gibbus with spinal cord decompression and reconstruction of the spinal column prevents late neurological complications and helps to create a more physiologically balanced spine which further prevents accelerated degeneration in the adjacent periapical segments.
Different techniques have been described to correct kyphotic thoracic deformities including anterior trans-thoracic, anterolateral, costotransversectomy pedicle subtraction osteotomy (PSO) and posterior vertebral column resection (PVCR).
Historically, anterior trans-throracic osteotomy has been utilized, but provided limited access in severe deformities as well as limited correction when posterior elements are fused. It also posed increased neurological risks due to stretching of the spinal cord [16].
PVCR has been established as a safe and effective technique to correct complex deformities, allowing circumferential neural decompression as well as simultaneous shortening of the posterior column along with lengthening of the anterior column and translation when needed to achieve optimal correction. Compared to other techniques, PVCR is a posterior approach without trans-thoracic invasion [17,18,19,20].
There is paucity of studies on spinal TB patients treated in West Africa. In this study, we report the clinical and radiographic outcomes on 57 patients with severe post-TB kyphosis corrected with PVCR technique with and without pre-operative halo gravity traction (HGT) at a single institution in West Africa.
Materials and methods
This is a retrospective study conducted on 57 consecutive patients with post-TB kyphosis who underwent surgical correction between 2013 and 2018 (≥ 2-year follow-up in 36 pts and ≥ 1-year follow-up in 21 pts). Pre-operative standing X-rays as well as serial traction (for patients undergoing HGT) and post-operative follow-up X-rays were obtained.
Pre- and post-operative sagittal spinal parameters were measured on all X-rays by two fellowship trained spine surgeons. Pre/post-operative SRS scores were obtained. Paired t test was performed to compare pre-op and post-op SRS scores and radiographic changes. Data on estimated blood loss (ml), estimated blood volume (EBV) loss (%), surgical time and the details of post-op complications were obtained.
Patients who were deemed to have a severe, rigid or short and sharp angular regional kyphosis (Gibbus) pre-operatively exceeding 90º (22 pts) were put in HGT and followed with serial standing traction X-rays for incremental improvement of the deformity. All patients received a nutritional program and physical therapy pre- and post-operatively to optimize physiologic status before surgery.
All patients were followed at regular intervals with a clinical exam, SRS outcome assessment, and standing X-rays for assessment of spinal alignment, implant position and boney fusion.
Traction protocol
Halo gravity traction was recommended for patients with severe and rigid sagittal, curves that did not reduce to less than 100° on hyperextension. Patients requiring pre-operative HGT had halo rings placed under conscious sedation and using standard techniques. In addition, given the severity of the deformity, the ideal design of the halo ring should be open over the occipital region to account for the extreme instrument angulations required during screw placement in upper thoracic pedicles.
Patients were placed in full-time spring-loaded traction devices (20 + h/day) designed to allow walking, sitting and sleeping in traction. They were taken out of the traction systems for meals and personal hygiene.
Traction is started at 20% of body weight and incrementally increased by 10% each week till a maximum of 50% of body weight is reached by end of third or fourth week. Pin sites were checked and cleaned daily and tightened at least once a week. Regular neurologic examinations were done to document any neurologic complications.
All patients had daily physical therapy sessions in traction devices to encourage mobility and optimize pulmonary function. Standing AP/lateral X-rays were obtained every 4 weeks to assess deformity correction.
Surgical technique
The majority of patients underwent posterior vertebral column resection with or without pre-operative HGT.
All procedures were supervised by the senior author (OBA) and done under total intravenous general anesthesia (TIVA) not to interfere with multi-modal Intraoperative Neuromonitoring (IONM) which was done for all cases.
After obtaining a pre-position neuromonitoring baseline, patient was positioned prone on a well-padded radiolucent table with chest and hip supports. Intraoperative traction was utilized in patients with pre-operative HGT. Intraoperatively, patients were put in only “half” the maximum traction weight they reached pre-operatively (which was 50% of body weight); thus, intraoperative traction was roughly 25% of body weight, distributed between halo device on the skull and counter-traction on each lower extremity via traction boots.
Following a midline incision, meticulous subperiosteal exposure was done to at least three levels above and below the apical osteotomy site. Pedicle screws were inserted using free hand technique.
After confirmation of screws position with fluoroscopy, PVCR was undertaken.
At the level of osteotomy, exposure of the ribs on both sides was done followed by resection of the proximal rib including the rib head (3–5 cm). At this point, the thoracic neuro-vascular bundle are ligated to allow better exposure of the anterior column without much traction on the cord. We then proceeded to expose the lateral surface of the vertebral body on both sides all the way to the anterior margin of the body. The maximum number of nerve root transected was three pairs.
At this point, a short temporary rod is placed on one side to stabilize the segment during the osteotomy. A wide laminectomy at the PVCR site and extending to a level above and below is then done to avoid cord impingement following later correction. Extra care should be taken to avoid any injury to the cord that is usually attenuated and draped along the internal gibbus. Special care should be taken in post-infectious cases due to the adhesions and scarring of the dura.
After isolation and excision of the pedicle, a sharp osteotome or high-speed burr is used to cut through the vertebral body mass anteriorly which is often made up of multiple segments in post-TB kyphosis. Care should be taken to remove the intervertebral discs above and below the resected bodies to allow good bony fusion.
After moving the temporary rod to the opposite side, the same steps are repeated on the other side until complete excision of the anterior mass is achieved. Finally, the posterior wall of the vertebral body mass (internal gibbus) should be carefully dissected from the cord and broken free with a special tamp or posterior wall cutting device.
Correction of the deformity can now be done either by incremental compression at the osteotomy site on each side or by simultaneous in situ bending of the temporary rods bilaterally until maximum correction is achieved. Posterior shortening correction maneuvers can be aided by distraction of the anterior column using a laminar spreader.
Finally, a mesh cage with bone graft can be inserted if there is an anterior gap larger than 5 mm which provides anterior column support and better boney union. Small anterior gap below 5 mm were grafted with local bone.
Temporary rods can now be exchanged with final rods. Additional rods can also be added to provide more stability at the osteotomy site till complete boney fusion.
Final position of implants and spinal alignment is confirmed by long X-ray films intraoperatively and IONM checked before closure.
Descriptive statistics on baseline characteristics, surgical details, and immediate post-op complications were conducted on all the 57 patients. Analysis of clinical outcomes and radiographic outcomes and SRS-22 scores at 2-year follow-up were reviewed for 36 (63.2%) patients.
Results
57 patients, 36M:21F. Mean age 19.6 (11–57 years). There were 34 (59.6%) Sierra Leoneans, 14 (24.6%) Ethiopians, 7 (12.3%) Ghanaians, 1 (1.7%) Nigerian and 1 (1.7%) Tanzanian. Average pre-op BMI was 20.5 kg/m2.
Pre-op HGT was utilized in 22 pts (39.3%) at an average duration of 86 days (8–144 days). Patients who underwent pre-operative HGT had higher baseline regional kyphosis (125.1° ± 20.9°) compared to the non-HGT treatment group (64.6° ± 31.8°, p < 0.001). Mean post-HGT regional kyphosis was corrected to 101.2 ± 23.1 representing about 24° corrections (Table 1). A slight majority of patients (52.6%) had an apex in the thoracic region, 45.6% had lumbar apex and 1.8% in the cervical region. Three patients (5.3%) had baseline paralysis from severe post-TB deformity.
The average surgical time was 305.0 ± 93.3 min. The average surgical blood loss as a percentage of estimated blood volume (i.e., %EBV loss) was 60.5 ± 26.3%. 53 patients (93.0%) underwent posterior-only surgery while four (7.0%) had combined anterior–posterior surgery. 39 (68.4%) had PVCR, 11 (19.3%) had pedicle subtraction osteotomy (PSO), 16 (28.1%) had thoracoplasty, and the remainder had posterior column osteotomy (PCO) only. Three patients (5.3%) had evacuation of psoas abscess in addition to their primary surgeries.
Intraoperatively, the prevalence of neuromonitoring (IOM) signal changes was 23/57 (≈ 40%), dural tear 5 (8.8%), pleural tear 3 (5.3%), ureteric injury 1 (1.7%), vascular thoracoplasty injury 1 (1.7%), and 1 (1.7%) other. Post-operative complications included four (7.0%) infection, three (5.3%) implant related, two (3.5%) radiographic [one proximal junctional kyphosis (PJK) and one distal junctional kyphosis (DJK)], one (1.7%) neurologic, one (1.7%) wound problem, and two (3.5%) sacral ulcers. Rate of IOM changes was similar in the VCR (48.7%) and non-VCR (23.5%) patients, p = 0.154. There was no difference in complication rates between HGT and non-HGT groups.
Significant improvements from baseline were seen in average SRS Total and domains scores among the 36 patients (63.2%) with minimum 2-year follow-up. Significant changes were observed in all sagittal Cobb measurements at follow-up except T2–T12 Cobb (Table 2).
Overall, pre-op regional kyphosis (96.4° ± 36.1°) corrected to 28.9° ± 16.8° (≈ 68.8%° correction) at 2-year follow-up (p < 0.0001). Pelvic tilt significantly improved post-op but not pelvic incidence and sacral slope (Table 2).
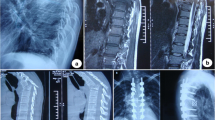
A case study of a TB kyphotic patient treated with pre-op HGT and subsequent PVCR has been presented as shown in Figs. 1, 2, 3, 4, 5, 6, 7.
Discussion
TB is prevalent in developing countries particularly in sub-Saharan Africa. This is mainly due to low-socioeconomic status and crowded living conditions [5]. Due to the deficiency in medical care, a large number of patients suffering from pulmonary and hence spinal TB do not receive early treatment which leads to complications including progressive post-TB kyphotic deformity.
Spinal TB usually starts in the vertebral body through hematogenous spread but can also spread sub-ligamentously to affect multiple contiguous vertebral bodies with delayed destruction of intervertebral discs thus creating a single kyphotic boney mass made up of contiguous fused segments [21,22,23].
Early neurologic complications can occur due to the mass effect of a cold abscess or boney fragments on the cord or in rare instances infection of the cord itself or interruption of arterial blood supply [24, 25].
Delayed neurological complications can also occur many years after healing of the acute phase if a severe and progressive kyphotic deformity develops due to constant compression of the cord by boney internal gibbus [26]. In addition, such deformities can cause restrictive cardiopulmonary dysfunction on patients along with the functional and psychological impairment due to the deformed and unbalanced posture [15, 27].
Various approaches and techniques have been described for management of severe post-TB kyphosis including trans-thoracic anterior decompression alone and fixation with iliac crest graft which provided little correction of the deformity and was mainly utilized for neural decompression in patients with late-onset neural deficits [28, 29].
Chunguang et al. utilized a combined anterior/posterior approach for correction of the deformity with good results; however, the initial angle of kyphosis was relatively small with an average of 55.8° and reduced to 21.7°. This technique required two-staged procedures with prolonged hospital stay. Moreover, the anterior approach is unable to provide good access to severe deformities beyond 60° [30].
In recent years, posterior based three-column osteotomies such as PSO and PVCR have been established as effective techniques in correcting large deformities. While PSO can provide up to 30–40° of correction per level in the lumbar spine segments and was utilized in our study on some patients, there is generally limited correction obtained in the thoracic spine so it may not be suitable for the high-degree kyphosis usually associated with TB due to destruction of multiple segments. In addition, posterior shortening of the spinal column alone may pose increased risk due to severe kinking of the cord [31, 32].
In a study by Bezer et al. utilizing PSO to correct post-TB kyphosis on 16 patients, they reported no neurological complications and correction of sagittal balance from 68 to 12 mm. The initial regional kyphosis in this study group was low, however, and was corrected from a mean of 30°–12° [33].
Kalra et al. reported on 15 patients with post-TB kyphosis all in the thoracolumbar and lumbar region treated using PSO technique. Mean pre-op kyphosis was 58.8° (34°–100°). The mean immediate post-operative kyphosis was 13.7° (0°–40°). They had no neurologic complications and one case with deep infection requiring debridement [34].
The VCR technique on the other hand was described by Suk et al. [20] for correction of severe spine deformities through a posterior-only approach and is more suitable for rigid post-TB thoracic deformities. In their study on 70 patients with severe kyphosis, a subgroup of 25 patients with post-TB kyphosis had a deformity of 68° ± 34° that was corrected to 12° ± 24° by this technique. They reported the complications in that subgroup to include one complete cord injury, two root injuries, two hematoma, one fixation failure, one infection and three hemopneumothorax. They concluded that although technically demanding, PVCR provided excellent correction while avoiding the complications associated with anterior thoracic approach [20].
Wang and Lenke described a vertebral decancellation technique in correction of severe kyphosis in 45 patients of whom 16 had post-TB deformity with a mean of 98.61° and were able to achieve a mean kyphosis of 31° at 2-year follow-up with 1 patient reported to have post-operative paraplegia and 4 with transient neurological deficit [35].
Wang et al. also reported nine patients with tuberculous kyphosis kyphotic angle of greater than 90° treated by eggshell osteotomy combined with VCR through posterior approach with correction from a mean of 100° down to 16°. All patients achieved fusion at 12 months with no major complications reported [36, 37].
Rajasekaran et al. reported their results in correction of 17 patients with post-TB kyphosis using a closing–opening wedge VCR osteotomy with an anterior cage. Average age was 18.3 ± 10.6 years (range 4–40 years), pre-operative kyphosis was 69.2 ± 25.1° (range 42–104°), post-operative kyphosis was 32.4 ± 19.5° range 8–62°) yielding a correction 56.8 ± 14.6% (range 32–83%). There were two superficial infections, one hardware failure requiring revision and one neurological deterioration from Frankel C to A post-op [38].
Srivastava et al. reported a similar technique combined with anterior distraction on 21 patients, age (21.90 ± 7.85) with post-TB kyphosis with 68.42° ± 13.23° pre-operative corrected to 8.71° ± 4.58° with a mean correction of 87.10% and with no neurological deficits reported. [39].
Rathod and Shah treated 16 patients (mean age 19.4 years) with post-TB rigid kyphosis using PVCR and anterior mesh cage. Mean pre-op kyphosis was 90.08° and corrected 38.06° (57.59%), two patients had neurological complications and one patient had wound complication. [40] In all the above studies, the use of traction before definitive procedure was seldomly mentioned.
In our present study, we performed an analysis on 57 patients with severe post-TB kyphosis. We further divided them into two subgroups depending on the utilization of HGT pre-operatively. The HGT group had a higher baseline regional kyphosis (125.1° ± 20.9°) compared to the non-HGT treatment group with a lower magnitude (64.6° ± 31.8°, p < 0.001). Patients with regional kyphosis that did not correct below 100° on traction X-rays were assigned to pre-op HGT. In addition, patients with very low body mass index (BMI) were put in HGT until BMI was optimized through a nutritional program. Given the setup at the under-resourced site, HGT subgroup was under continued observation by the medical team and received daily physical therapy sessions.
Pre-operative HGT has been proven effective in reducing both coronal and sagittal curves [40, 41]. In addition, it can improve the pulmonary function which is usually severely compromised in patients with post-TB kyphosis [41,42,43]. In the present study, we report partial correction of about 24° (19.2%) in the baseline regional kyphosis after HGT. The partial deformity correction was a little lower in this cohort than what has been previously reported in other studies on HGT correction [43,44,44]. We attribute this to the very rigid nature of post-TB kyphosis as compared to other etiologies such as idiopathic or neuromuscular scoliosis which can yield more correction with HGT (≥ 30%) [43,44,44].
The prevalence of IOM signal changes was ≈ 40% which is expected in such complicated deformities, particularly given the dural scarring and compromised blood supply to the cord in many cases following TB. This makes the cord very sensitive to any manipulation or drop in blood pressure. Moreover, IOM signal changes are usually expected during surgery in such complex deformity involving the use of VCR [45]. This is mostly attributable to stretching of neural elements during curve correction maneuvers. The IOM signal changes could also happen due to drop in blood pressure, under-resuscitation or prolonged traction. Experienced anesthesia team and neuromonitoring personnel are able to warn surgeons about any signal changes as soon as it is detected so as to reverse causative factors to avoid post-operative neurological complications. As an intervention, the mean arterial pressure (MAP) is often raised after IOM signal changes and traction, if present, is removed. Surgeons also usually prompt the IOM technicians to perform diagnostic test after major corrective maneuvers. The coordination of activities and timely responses by the surgeons, anesthetist and IOM technicians could possibly explain the low risk of new neurologic deficits among our series.
Nevertheless, one patient (1.7%) developed post-operative neurologic complications but regained bowel and bladder control at discharge despite chronic neurologic deficits at 3-year follow-up. This was an 18-year-old male with a baseline sagittal deformity of 110°. He was treated without pre-op HGT. The first stage was PSF T7–S1, VCR T11–L1 and bone grafting (autologous local and ribs). The there was no IOM signal change at this stage. Surgical time was 240 min, blood loss was 1500 ml and was transfused 450 ml of whole blood and 340-ml cell-salvaged blood. Patient was planned for anterior augmentation due to significant defect anteriorly. The second stage was done on the 8th day post-index and consisted of ASF T10–L2, Harms Cage T10–L2, Auto Ribs, Allograft. This was done without spinal cord monitoring. A left-sided T11 retroperitoneal, retro pleural approach was performed to expose the spine at T10–L2 level. Significant amount of scar tissue was present and this required extensive dissection. There was a significant 3-level anterior defect. We decorticated the endplates and a titanium mesh cage was wedged in place. X-rays obtained showed appropriate position of the cage. Post-extubation neurological assessment showed patient had no motors in the lower extremity, and therefore, this necessitated re-exploration and revision on the same day. This involved the removal of the periapical screw at T12, anterior revision instrumentation and cage repositioning. Paraplegia was persistent at this stage with absent motor-evoked potentials (MEPs) signals in the bilateral lower extremities. Patient also developed left pneumothorax requiring chest tube insertion at post-op day 1 after ASF (i.e., post-op day 9 post-index). Post-op magnetic resonance imaging (MRI) showed malpositioned anterior thoracic cage requiring another revision on the 14th day post-second stage. Patient remained paraplegic despite extended physiotherapy for 5 months. Patient remained paraplegic at 3-year follow-up. In retrospect, the second-stage anterior procedure should have been performed under IOM guidance for early detection of neuro-status and early intervention intraoperatively since this was likely a malpositioned cage causing neural element impingement.
We also report baseline neurologic deficits in three patients which we believe reflects the natural course of untreated severe post-TB deformities. The first was a 13-year-old male who was ASIA A and had lost the ability to walk 2 years prior to presentation with bowel and bladder deficits. He remained paraplegic after undergoing HGT for > 3-month duration and surgical intervention involving posterior VCR. He had not made any neurologic improvement at 2-year follow-up. The second was a 22 female who was spastic, wheel chair bound and had ASIA D at baseline with inability to walk 18 months prior to presentation. She underwent staged anterior fusion with apical resection and a PSF. This patient could mobilize with a walker after surgery but was still spastic not regained full neurologic function after 3-month physiotherapy. She was spastic at 9 months post-op and was subsequently lost to follow-up. The third was an 18-year-old male who was severely myelopathy and spastic at presentation. Baseline ASIA was C. He underwent PSF with Instrumentation C7–T11, VCR T5–T7 and bone grafting with local bones and autogenous rips. He regained bladder and bowel function at 12 and 15 days post-op, respectively. The patient was discharged to rehab and improved with physiotherapy. At 9-month follow-up, he was spastic on examination and mobilizing with bilateral leg braces with trunk support in Jewett brace. His lower extremity ASIA had not changed from baseline. He was subsequently lost to follow-up. All other patients had normal baseline neurologic status. One important lesson is that patients who have baseline paralysis should be given realistic expectation about surgery. This is because surgical intervention may not lead to neurologic recovery as seen in this study. Communication with paralytic patients and family should discuss the reason for surgery which is mainly for debridement, decompression and posterior stabilization rather than reversal of the neurologic deficits.
Other post-operative complications included four (7.0%) infections, three (5.3%) implant-related requiring revisions, two (3.5%) radiographic (one PJK and one DJK, both required revision), one (1.7%) wound problem (dehiscence), and two (3.5%) sacral ulcers which were all treated (one sacral ulcer occurred after 6 months post-op in the patient with baseline paralysis). The four patients who developed wound infection required incision and drainage and antibiotics treatment for 6 weeks (one of them also required removal of instrumentation at affected unilateral side only while another required complete explanation, HGT, and reimplantation after 6 weeks of antibiotic treatment).
For the severe thoracic hyperkyphotic deformities in this study, PVCR was deemed necessary for the majority of patients. Posterior column osteotomy (PCO) was performed at the apical segments to obtain a more balanced correction. For some of the lumbar-apex deformities, PSO along with adjacent levels PCOs were found to be sufficient to achieve a balanced correction of deformity. Pedicle subtraction osteotomy (PSO) was not done in the thoracic spine due to the limited correction and higher risks in thoracic spine but was utilized in lumbar cases with moderate deformity.
The majority of patients were neglected post-TB deformity patients from very rural areas and nearby countries who either received no treatment at all or only medications. Most had the deformity progressing over a period of years. Patients who had no history of taking anti-TB medication were placed on medication for 6 weeks prior to surgery per our institutional policy. Those who had no history of medical management were treated as new cases for 8 months in total.
Special considerations in this part of the world include but not limited to lack of financial resources dedicated to the high expenses for treating complex spine cases, difficulty obtaining surgical tools, implants and equipment necessary to operate on complex deformity safely. Moreover, there is shortage of intensive care beds, and advanced investigation centers [MRI, computed tomography (CT) scans, and Pulmonary Function Test (PFT)], as well as difficulty in creating a dedicated team of anesthesiologists, nursing, operating room personnel and physiotherapist comfortable in managing such complex cases.
As a private orthopedic facility in West Africa treating TB kyphosis patients from different countries in Africa, follow-up visit often becomes a constraint for some foreign patients due to financial difficulties. It has been our practice to organize bi-annual trips to Sierra Leone and Ethiopia to follow-up on patients. These notwithstanding, optimal follow-up visit is challenging in our context as some patients are unable to show up at designated facilities during foreign trips. This explains why only 63.2% of patients had attained 2-year follow-up. Nevertheless, we believe this study provides an important insight into the clinical and radiographic outcomes in a consecutive patient series from different African nationalities who were surgically treated at a single site in an underserved community in West Africa following the diagnosis of severe post-TB kyphosis. The complication rate in this study, particularly neurologic complications are comparable to other studies on the same pathology. Severe post-TB kyphosis is perhaps one of the most challenging deformities to safely correct. However, we believe that meticulous surgical technique and thorough neural decompression by experienced surgical team working with IOM guidance are crucial to achieve optimal outcomes with acceptable complications in this patient population.
Conclusion
Although the management of severe post-TB kyphosis a very challenging problem in Africa, we demonstrated in this study that the PVCR technique with or without HGT can be safely performed for patients with severe post-TB kyphosis at a well-equipped facility in West Africa with optimal clinical and radiographic outcomes. The availability of skilled surgeons and a multidisciplinary team is extremely important to achieve favorable outcomes. We hope that more resources will be available in the upcoming years to meet the increased patient volume in the underserved regions.
References
World Health Organization (2018) Global tuberculosis report 2018. World Health Organization, Geneva
Esteves S, Catarino I, Lopes D, Sousa C (2017) Spinal tuberculosis: rethinking an old disease. J Spine 6(1):358. https://doi.org/10.4172/2165-7939.1000358
Satyasri S (1993) Global epidemiology of tuberculosis. Text book of pulmonary and extra-pulmonary tuberculosis. Interprint, Madras, pp 13–18
Zumla A, Raviglione M, Hafner R, von Reyn CF (2013) Current concepts: tuberculosis. N Engl J Med 368:745–755. https://doi.org/10.1056/NEJMra1200894
World Health Organization (2017) Global tuberculosis report 2017. World Health Organization, Geneva
Parthasarathy R, Sriram K, Santha T, Prabhakar R, Somasundaram PR, Sivasubramanian S (1999) Short-course chemotherapy for tuberculosis of the spine: a comparison between ambulant treatment and radical surgery–ten-year report. J Bone Jt Surg Br Vol 81(3):464–471. https://doi.org/10.1302/0301-620X.81B3.0810464
Moon MS, Kim I, Woo YK, Park YO (1987) Conservative treatment of tuberculosis of the thoracic and lumbar spine in adults and children. Int Orthop 11(4):315–322. https://doi.org/10.1007/BF00271307
Moon MS (1997) Tuberculosis of the spine: controversies and a new challenge. Spine 22(15):1791–1797
Boachie-Adjei O, Papadopoulos EC, Pellisé F, Cunningham ME, Perez-Grueso FS, Gupta M, Lonner B, Paonessa K, King A, Sacramento C, Kim HJ (2013) Late treatment of tuberculosis-associated kyphosis: literature review and experience from a SRS-GOP site. Eur Spine J 22(4):641–646
Su SH, Tsai WC, Lin CY, Lin WR, Chen TC, Lu PL, Huang PM, Tsai JR, Wang YL, Feng MC, Wang TP (2010) Clinical features and outcomes of spinal tuberculosis in southern Taiwan. J Microbiol Immunol Infect 43(4):291–300. https://doi.org/10.1016/S1684-1182(10)60046-1
Avadhani A, Shetty AP, Rajasekaran S (2010) Isolated tuberculosis of the lumbar apophyseal joint. Spine J 10(3):e1-4
Rajasekaran S (2001) The natural history of post-tubercular kyphosis in children: radiological signs which predict late increase in deformity. J Bone Jt Surg Br Vol 83(7):954–962
Tuli SM (1995) Severe kyphotic deformity in tuberculosis of the spine. Int Orthop 19:327–331. https://doi.org/10.1007/bf00181121
Rajasekaran S (2012) Kyphotic deformity in spinal tuberculosis and its management. Int Orthop 36(2):359–365. https://doi.org/10.1007/s00264-011-1469-2
Jain AK (2002) Treatment of tuberculosis of the spine with neurologic complications. Clin Orthop Relat Res. 398:75–84
Jain AK, Dhammi IK, Jain S, Mishra P (2010) Kyphosis in spinal tuberculosis–prevention and correction. Indian J Orthop 44(2):127
Kawahara N, Tomita K, Baba H, Kobayashi T, Fujita T, Murakami H (2001) Closing–opening wedge osteotomy to correct angular kyphotic deformity by a single posterior approach. Spine 26(4):391–402
Luk KD (2011) Expert’s comment concerning Grand Rounds case entitled “Closing–Opening Wedge Osteotomy for Severe, Rigid Thoraco-Lumbar Post-tubercular Kyphosis” (by S. Rajasekaran, P. Rishimugesh Kanna and Ajoy Prasad Shetty). Eur Spine J. 20(3):349–350
Hamzaoglu A, Alanay A, Ozturk C, Sarier M, Karadereler S, Ganiyusufoglu K (2011) Posterior vertebral column resection in severe spinal deformities: a total of 102 cases. Spine 36:E340–E344
Suk SI, Kim JH, Kim WJ, Lee SM, Chung ER, Nah KH (2002) Posterior vertebral column resection for severe spinal deformities. Spine 27(21):2374–2382
Garg RK, Somvanshi DS (2011) Spinal tuberculosis: a review. J Spinal Cord Med 34(5):440–454. https://doi.org/10.1179/2045772311Y.0000000023
Jain AK, Dhammi IK (2007) Tuberculosis of the spine: a review. Clin Orthop Relat Res (1976–2007) 460:39–49. https://doi.org/10.1097/BLO.0b013e318065b7c3
Jain R, Sawhney S, Berry M (1993) Computer tomography of vertebral tuberculosis: patterns of bone destruction. Clin Radiol 47(3):196–199. https://doi.org/10.1016/S0009-9260(05)81162-6
Jain AK, Kumar J (2013) Tuberculosis of spine: neurological deficit. Eur Spine J 22(4):624–633. https://doi.org/10.1007/s00586-012-2335-7
Hodgson AR, Yau A (1967) Pott’s paraplegia: a classification based upon the living pathology. Spinal Cord 5(1):1–6. https://doi.org/10.1038/sc.1967.2
Jain AK (2010) Tuberculosis of the spine: a fresh look at an old disease. J Bone Jt Surg Br Vol 92(7):905–913. https://doi.org/10.1302/0301-620X.92B7.24668
Yau AC, Hsu LC, O’Brien JP, Hodgson AR (1974) Tuberculous kyphosis: correction with spinal osteotomy, halo-pelvic distraction, and anterior and posterior fusion. J Bone Jt Surg Am 56(7):1419–1434
Bilsel N, Aydıngöz Ö, Hancı M, Erdoğan F (2000) Late onset Pott’s paraplegia. Spinal Cord 38(11):669–674. https://doi.org/10.1038/sj.sc.3101082
Paravastu R (2008) Paraplegia of late onset in adolescents with healed childhood caries of dorsal spine a cause of pressure on the cord and treatment. Indian J Orthop 42(4):454–459. https://doi.org/10.4103/0019-5413.41871
Chunguang Z, Limin L, Rigao C, Yueming S, Hao L, Qingquan K, Quan G, Tao L, Jiancheng Z (2010) Surgical treatment of kyphosis in children in healed stages of spinal tuberculosis. J Pediatr Orthop 30(3):271–276. https://doi.org/10.1097/BPO.0b013e3181d39899
Bridwell KH (2006) Decision making regarding Smith-Petersen vs. pedicle subtraction osteotomy vs. vertebral column resection for spinal deformity. Spine. 31:S171–S178. https://doi.org/10.1097/01.brs.0000231963.72810.38
Kawahara N, Tomita K, Kobayashi T, Abdel-Wanis ME, Murakami H, Akamaru T (2005) Influence of acute shortening on the spinal cord: an experimental study. Spine 30:613–620. https://doi.org/10.1097/01.brs.0000155407.87439.a2
Bezer M, Kucukdurmaz F, Guven O (2007) Transpedicular decancellation osteotomy in the treatment of posttuberculous kyphosis. Clin Spine Surg 20(3):209–215
Kalra KP, Dhar SB, Shetty G, Dhariwal Q (2006) Pedicle subtraction osteotomy for rigid post-tuberculous kyphosis. J Bone Jt Surg Br Vol 88(7):925–927
Wang Y, Lenke LG (2011) Vertebral column decancellation for the management of sharp angular spinal deformity. Eur Spine J 20(10):1703–1710
Wang Y, Zhang Y, Zhang X, Wang Z, Mao K, Chen C, Zheng G, Li G, Wood KB (2009) Posterior-only multilevel modified vertebral column resection for extremely severe Pott’s kyphotic deformity. Eur Spine J 18(10):1436–1441
Issack PS, Boachie-Adjei O (2012) Surgical correction of kyphotic deformity in spinal tuberculosis. Int Orthop (SICOT) 36:353–357. https://doi.org/10.1007/s00264-011-1292-9
Rajasekaran S, Vijay K, Shetty AP (2010) Single-stage closing–opening wedge osteotomy of spine to correct severe post-tubercular kyphotic deformities of the spine: a 3-year follow-up of 17 patients. Eur Spine J 19(4):583–592
Srivastava SK, Aggarwal RA, Bhosale SK, Roy K, Nemade PS, Purohit S (2019) Apical vertebral column resection with sagittal rotation and controlled anterior opening and posterior closing maneuver for the treatment of severe post-tubercular kyphosis: case series and literature review. Asian Spine J 13(3):478–489
Rathod TN, Shah KA (2020) Vertebral column resection for post tuberculosis severe kyphotic deformity: results of 5-year follow-up. J Orthop 19:122–127. https://doi.org/10.1016/j.jor.2019.11.036
Rinella A, Lenke L, Whitaker C, Kim Y, Park SS, Peelle M, Edwards C, Bridwell K (2005) Perioperative halo-gravity traction in the treatment of severe scoliosis and kyphosis. Spine 30(4):475–482
Sink EL, Karol LA, Sanders J, Birch JG, Johnston CE, Herring JA (2001) Efficacy of perioperative halo-gravity traction in the treatment of severe scoliosis in children. J Pediatr Orthop 21(4):519–524
Bogunovic L, Lenke LG, Bridwell KH, Luhmann SJ (2013) Preoperative halo-gravity traction for severe pediatric spinal deformity: complications, radiographic correction and changes in pulmonary function. Spine Deform 1(1):33–39
Iyer S, Boachie-Adjei O, Duah HO, Yankey KP, Mahmud R, Wulff I, Tutu HO, Akoto H (2019) Halo gravity traction can mitigate preoperative risk factors and early surgical complications in complex spine deformity. Spine 44(9):629–636
Lenke LG, Newton PO, Sucato DJ, Shufflebarger HL, Emans JB, Sponseller PD, Shah SA, Sides BA, Blanke KM (2013) Complications after 147 consecutive vertebral column resections for severe pediatric spinal deformity: a multicenter analysis. Spine 38(2):119–132
Acknowledgment
FOCOS Spine Research Group members are: Oheneba Boachie-Adjei, Henry Ofori Duah, Kwadwo Poku Yankey, Derrick Nyantakyi Owusu, Mabel Adobea Owiredu, Arthur Sackeyfio, Gerhard Ofori-Amankwah, Franklin Coleman, Irene Wulff.
Funding
The paper was funded with a grant from K2M (Grant no: K2M/FC/060216).
Author information
Authors and Affiliations
Consortia
Contributions
Conceptualization and design: AMM, OA, HOD, KPY, DON, AS, MO, TW, GO-A, FC, HA, IW, OB-A. Data collection and cleaning: AMM, OA, HOD, KPY, DON, AS, MO, TW, GO-A, FC, HA, IW, OB-A. Data analysis: HOD, AMM, OA. Interpretation of data results: AMM, OA, HOD, KPY, DON, AS, MO, TW, GO-A, FC, HA, IW, OB-A. Writing—initial draft preparation: AMM, HOD. Writing—critical review for important intellectual content: AMM, OA, HOD, KPY, DON, AS, MO, TW, GO-A, FC, HA, IW, OB-A. Final approval: AMM, OA, HOD, KPY, DON, AS, MO, TW, GO-A, FC, HA, IW, OB-A. Agreement to be accountable for all aspects of the work: AMM, OA, HOD, KPY, DON, AS, MO, TW, GO-A, FC, HA, IW, OB-A. Supervision: OB-A.
Corresponding author
Ethics declarations
Conflict of interest
Dr. Boachie-Adjei reports grants, personal fees and other from K2M, personal fees and other from WEIGAO, outside the submitted work. For the remaining authors, none were declared.
IRB approval statement
The study used secondary data from the FOCOS spine registry database approved by the institutional review board (IRB) of the Noguchi Memorial Institute for Medical Research (NMIMR), College of Health Sciences, University of Ghana, Legon (Study Protocol Number 015/14-15).
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Maziad, A.M., Adogwa, O., Duah, H.O. et al. Surgical management of complex post-tuberculous kyphosis among African patients: clinical and radiographic outcomes for a consecutive series treated at a single institution in West Africa. Spine Deform 9, 777–788 (2021). https://doi.org/10.1007/s43390-020-00258-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43390-020-00258-3