Abstract
Study design
Retrospective case series.
Summary of background data
Proximal junctional kyphosis (PJK) is a well-recognised post-operative complication of deformity correction surgery. Our local tuberculosis (TB) endemic is responsible for severe kyphotic deformities. The most challenging is in the paediatric environment where powerful instrumentation is used in immature spines with more flexible disco-ligamentous structures than adults.
Objective
To establish the incidence of PJK and management thereof in our paediatric TB spine patients undergoing corrective surgery.
Methods
Twenty-seven consecutive paediatric patients undergoing fusion surgery for TB spine with 2-year follow-up were identified from our prospectively maintained database. Age at surgery was 8.0 years (2.5–17 ± 3.98) with 14 under the age of 7. Only anterior surgery was performed in 1, posterior only in 13 and combined in 13 with a total of 5 (1–11) levels fused.
Results
Nine (33.3%) patients developed PJK (progression by > = 10°) with an average progression of 16.2°(11–26 ± 5.42) compared the overall cohorts change of 5.1°(− 26–15 ± 9.24). Although not reaching statistical significance, there was a trend to higher incidence of PJK when instrumented, 8/20 (40%) compared to 1/7 (14.3%), more so in posterior only surgery compared to combined, 6/13 (46.2%) compared to 3/13 (23.1%) and when the UIV was at T7 or above, 7/17 (41.2%) compared to 2/10 (20%). There was a higher PJK rate when the number of levels fused was > = 6, 7/12 (58.3%) compared to 2/10 (p = 0.014), when the kyphotic correction was more than 39º, 5/8 (62.5%) compared to 4/19 (21.1%) (p = 0.07) and when < = 7 years old, 7/14 (50%) compared to 2/13 (15.4%) (p = 0.05). Two of the nine PJK cases required revision for junctional failure.
Conclusion
In paediatric TB kyphosis correction, there was a 33% incidence of PJK with 2/9 requiring revision surgery for proximal failure. Our data suggest that this incidence of PJK was related to the magnitude of correction, the number of levels fused with a trend of increase in higher UIVs, posterior approach and instrumentation.This suggests that in young children, one should be cautious of overzealous kyphosis correction due to the risk of catastrophic proximal junctional failure.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Proximal junctional kyphosis (PJK) is a well-recognised postoperative spinal complication which is usually associated with spinal deformity corrective surgery where the most common site is immediately above the uppermost-instrumented vertebrae (UIV). PJK is a radiological diagnosis which may or may not be symptomatic. The most common definition popularised by Glattes described PJK as a proximal junctional angle (PJA) ≥ 10° and at least 10° more than pre-instrumentation, with PJA defined as the angle between the caudal endplate of the upper instrumented vertebrae (UIV) to the cephalad endplate of 2 vertebrae above the upper instrumented level [1, 2]. The reported incidence of PJK ranges between 5% and 46% of patients who undergo spinal instrumentation for deformity correction. The wide variability in the incidence of PJK is mainly due to different radiological definitions [2].
Tuberculosis (TB) is massive health burden globally with 10.4 million new cases in 2015 alone and a prevalence of up to 1% in developing countries, such as South Africa [3]. With population migration exacerbated by geo-political instability, there is a resurgence of TB in the developed world [4]. Spinal TB represents 1–2% of TB cases and results in kyphosis, both in the active and healed disease states. This kyphotic deformity is a major risk factor for neurological deterioration in paediatric patients as it frequently progresses despite disease control [5]. The residual healed kyphosis may result in painful costopelvic impingement, respiratory complications, spinal canal stenosis with paraplegia, thus affecting quality of life and life expectancy. These complications can be avoided by early diagnosis and management of the TB to minimise the kyphosis but due to late presentation often require corrective surgery [6].
Sagittal plane correction in the adult is fraught with PJK and frequently discussed, but to our knowledge, there are currently no studies that define the incidence, risk factors and mechanism of proximal junctional kyphosis following corrective surgery for TB in paediatrics patients. We reviewed our cohort in an attempt to provide this information.
Methods
Following institutional ethical approval, a retrospective review was performed on data in a prospectively maintained surgical database. The inclusion criteria were spinal tuberculosis in patients 18 years old or less undergoing corrective surgery. The exclusion criteria were atlanto-axial cervical cases, less than 2-year follow-up and incomplete records. Thirty-eight consecutively managed patients were identified. All had undergone surgery by the senior author over the period 2009 to 2016. Patients undergoing both instrumented and un-instrumented spinal fusion were included with a minimum follow-up period of 2 years. This resulted in 7 (18.4%) patients being excluded due to incomplete post-operative and follow-up imaging. Unfortunately, this is typical of this patient cohort who are poor, often live far from the city and do not have the resources to return for follow-up especially when they feel well. A further 2 (5.2%) were excluded as they were atlanto-axial cervical spines and a final 2 (5.2%) patients had no records available.
The 27 patients (13 male) had an average age at the time of surgery of 8.0 years (2.5–17 ± 3.98) with 14 (51.8%) patients under the age of 7 years.
All the patients presented to our outpatient department after they were initially assessed at the referral hospitals and a provisional diagnosis made. On presentation, patients were assessed clinically and neurological status documented according to ASIA score. Radiological assessment included plain AP and lateral X-rays of the affected area and an MRI of the whole spine. Baseline haematological studies were performed in all the patients on admission.
Tissue samples of the pathological lesion were sent for PCR, histology, microscopy, culture and sensitivity in all the cases. The indications for surgery were myelopathy and progressive kyphosis. The ASIA grading was used to document the neurological status of all the patients. Twenty of the cases had myelopathy—3 ASIA A, 9 C, 8 D. Twenty-two (81.4%) had progressive kyphosis in the active phase of the disease and 5 (18.5%) had progressive myelopathy in the healed phase of the disease.
Three different surgical approaches to the spine were used. These included anterior transthoracic only, posterior approach with vertebral column resection (VCR) and combined anterior transthoracic decompression with posterior spinal fusion (instrumented/onlay bone graft). There was an evolution from anterior–posterior to the pVCR approach over time as it avoided the re-positioning of the patient. In the early part of the study, instrumentation was less accessible and uninstrumented techniques used. The single anterior only was an older child where ongoing asymmetrical spine growth was not a concern.
Intra-operatively, an effort was made to maintain the proximal supraspinous ligaments and not violating the UIV facets when determining pedicle screw entry.
Anti-tuberculous therapy (ATT) was initiated whilst waiting for biopsy and continued for a minimum period of 9 months in the active disease patients. In the very young, three-drug therapy was used, viz. Rifampicin, Isoniazid and Pyrazinamide, whereas in the adolescents, the Ethambutol was added as is our default in adult therapy. Due to the retro-bulbar neuritis concerns of ethambutol and inability to easily monitor vision in the young, we use the above approach. Treatment was stopped once a good clinical, biochemical and radiological response was established.
Post-operative mobilization was initiated from day one by a physiotherapist. X-rays were obtained between days 2 and 5 after surgery. Patients were deemed fit for discharge once they were fully mobilised and those who had residual neurological fallout were referred to a dedicated rehabilitation center for further management. Planned regular follow-ups were scheduled at 6 weeks, 3 months, 6 months, 9 months, 12 months and at 2 years post surgery. At the time of follow-up, an AP and lateral X-ray views of the spine were obtained. Regular ESR was done on every clinic visit for all the patients to monitor the response to anti-tuberculosis treatment.
The lateral X-rays were assessed for local kyphosis and PJA as described by Glattes.
Statistics
All the continuous measurements were analysed for their distribution pattern using Shapiro–Wilk test. Tests for statistical significance were performed using Mann–Whitney U test with the significance cut-off set at < 0.05. The analysis of categorical variables leading to positive cases of PJK was performed using Fisher’s Exact test. The effect of multiple factors, including categorical (with two levels) and continuous, on the 2-year post-operative findings was performed using Binomial Logistic Regression Analysis. All the analyses were performed in IBM SPSS v.26 (IBM, Armonk, NY).
Results
Overall, 27 paediatric TB spine patients (13 male) with an average age of 8.0 years (2.5–17 ± 3.98) were managed for myelopathy (20) and progressive kyphosis. The focal kyphosis was corrected from 58.6º (16–118 ± 25.37) to 31.5º (4–55º ± 15.76).
Of the 27, 9 (33.3%) patients developed PJK (progression by > = 10°) by 2 years with an average progression of 16.2°(11–26 ± 5.42) compared to the overall cohorts change of 5.1°(− 26–15 ± 9.24). The immediate post-operative PJA was an average 17.6º (3–58 ± 16.65) with insignificant progression by two years to 22.7º (4–55º ± 15.36) (p = 0.225).
Two of these patients required revision within the 2-year period.
Although there was a higher incidence of PJK (> 10°) in the instrumented group 8/20 (40%) than the un-instrumented group 1/7 (14.3%), this did not reach statistical significance (p = 0.36).
There was a trend to a higher incidence of PJK in the posterior only approach 6/13 (46.2%) than the combined group 3/13 (23.1%) (p = 0.41). As all instrumented cases except one had pedicle screws, implant effect could not be analysed.
As regards the UIV, 7/17 (41.2%) PJKs occurred when T7 or above compared to 2/10 (20%) below which was insignificant (p = 0.406). The number of levels fused, however, had a significant difference with 7/12 (58.3%) when more than 6 levels as opposed to 2/10 when less (p = 0.014).
The pre-operative local kyphosis measured an average 58.6º (16–118 ± 25.37) with improvement to 31.5º (4–55º ± 15.76) post-operatively representing a significant change of 27.1º (− 8–71 ± 24.11) (p = 0.001). There was a trend to increased PJK rate when the kyphotic correction was more than 39º, 5/8 (62.5%) compared to 4/19 (21.1%) (p = 0.07).
Patients 7 years old or younger had a higher PJK rate of 7/14 (50%) than older 2/13 (15.4%) (p = 0.05) This appeared to place them at risk of revision with the only two revisions being very young.
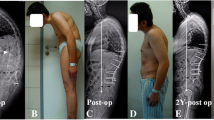
The first case was a 7-year-old male patient with T1 spinal tuberculosis. He presented with severe cervicothoracic kyphosis and progressive myelopathy (ASIA A). An anterior decompression of C7 and T1 was performed, reconstructed with a fibula strut graft and a hanging plate fixed on the superior edge of T2 vertebral body. A posterior spinal fusion was done from C5 to T2. The patient was subsequently discharged. At 3-week follow-up, there was a C3/4 subluxation. Revision surgery was performed with extension posteriorly to C2. (Fig. 1). This child recovered to ASIA E with a successful fusion but stiff neck and no subsequent surgery at 4-year follow-up.
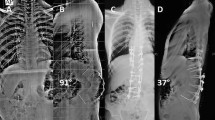
The second case was a 6-year-old male patient who presented with thoracic spine tuberculosis T7/T8 and ASIA C neurology. This patient had posterior vertebral column resection and instrumented fusion from T3 to T9. Subsequently, on follow-up X-rays, patient had PJK at T2/T3 level. Revision surgery by proximal extension of posterior instrumentation was done. He recovered to normal neurological status and no further surgery by 6-year follow-up (Fig. 2).
Discussion
Both socio-economic factors and the insidious nature of spinal tuberculosis result in delayed presentation and significant kyphosis necessitating surgical intervention, both for neurological compromise and the deformity itself. Although many patients are managed with anti-tuberculosis therapy (ATT) alone, surgery is indicated in children with unacceptable deformity (kyphosis), neurological compromise, pain, spinal instability and for tissue biopsy to confirm diagnosis and drug sensitivity [7].
Tuberculous spondylitis during childhood destroys the anterior vertebral bodies, limiting anterior growth potential and progressive kyphosis with continuing growth of posterior column. Therefore, this condition results in an acute angular kyphosis that progresses until the end of growth. This increase of the kyphotic angle can cause pulmonary insufficiency and neurological deficits [8]. Rajasekaran observed that children younger than seven years of age, with three or more affected vertebral bodies in the dorsal or thoracolumbar spine and two or more 'at-risk signs', are likely to have progression of the kyphosis with growth and should undergo surgical correction [9].
Surgical planning includes selection of proximal and distal fusion levels and the correct surgical approach to achieve the desired results. As opposed to scoliosis, the rules are unclear and often dictated by the extent of the TB destruction and intuitively keeping the construct as short as possible to allow maximal growth in the immature spine.
Our incidence of radiographic PJK in paediatric tuberculosis kyphosis correction surgery was 33.3% which is in line with that reported in the literature for deformity surgery in general. The incidence was higher in the younger age group. Most that developed PJK (66.6%) had 3 or more vertebral bodies affected prior to surgery.
Both the degree of apical kyphotic angle correction and the posterior only approach increased the rate of PJK.
There is little published on paediatric PJK following TB as a single-plane sagittal deformity with more focus on scoliosis surgery. Kim et al. reviewed 249 patients with idiopathic scoliosis undergoing combined anterior and posterior surgery with a PJK incidence of 42 (17%) patients [10]. Lee et al. reviewed 69 adolescent idiopathic scoliosis (AIS) patients and confirmed 46% had PJK at 2-year follow-up [11]. Rhee et al. found 35% PJK incidence in their AIS patients managed with posterior instrumented fusion and postulated that interrupting the posterior tension band and the use of compression forces through claw hook constructs at the UIV may lead to a PJK [12].
This posterior-related surgery increase has been confirmed by Yagi et al. who reported 27% PJK in posterior instrumented fusion compared to anterior instrumented fusion group and combined anteroposterior instrumented fusion group [2].
The use of instrumentation in TB spine has been studied and certain indications for the use of instrumentation have been identified. Indications for instrumented fusion in tuberculous spine are panvertebral disease, long segment disease requiring a bone graft length greater than two vertebral bodies and when kyphosis correction is contemplated [13, 14]. In our review, the 8 (40%) instrumented patients that developed PJK were all involving the thoracic and thoracolumbar spine. The number of fused levels was 5 on average and all the cases had pedicle screw only construct at the upper most instrumented vertebrae. These findings have been supported by Kim et al., who looked at the risk factors associated with PJK when they analyzed three different types of posterior instrumentation used in patients with AIS. They reported that the all-pedicle screw group had the highest prevalence of PJK (35%) compared with the hook only (22%) and hybrid (29%) [15]. Helgeson et al. also reported a higher prevalence of PJK in the all-screw group compared with the hybrid and the all-hook groups [16]. Only 1 (14%) patient in the un-instrumented group developed PJK and the upper thoracic spine was involved in this case. This patient had anterolateral decompression and fibular strut graft insertion plus posterior un-instrumented fusion with onlay bone graft.
Our revision rate for PJK was 2 of 9 cases, both cases had extension of instrumentation proximally. In a study by Lee et al., there was a 46% prevalence of PJK but only one patient required revision surgery by extending the fusion proximally [11]. Yagi et al., reported that 6 of 32 PJK patients were symptomatic and four patients underwent revision surgery due to local pain [2]. The rate of symptomatic PJK in tuberculous spine resulting in revision surgery has not been established.
We recognize that this is a small series due to the nature of the pathology and, thus, the paucity of publications on the topic. It is retrospective with typical loss of follow-up for such a developing world cohort of patients coming from up to 1000 km away. In addition, additional clinically significant PJK may occur as the patients grow following our 2-year cut-off. This makes conclusive statistical analysis difficult, but our data suggest that the posterior surgical approach particularly when instrumented with aggressive correction of the kyphotic deformity, increases the chance of PJK. Our data suggest that longer fusions increase this incidence with a trend of higher UIVs contributing as well.
UIV and age of less than 7 years are the risk factors for the development of PJK post-tuberculous kyphosis corrective surgery in paediatrics. The magnitude of kyphosis correction was noted to be a contributing factor in the development of PJK in patients that had posterior only surgery.
Modern instrumentation allows massive correction which may be beyond what the patient can accommodate. Although our deformities may not seem large at 58 degrees, these are focal kyphosis and not global T4-12 as referenced in other more global type pathologies, such as Scheuermann’s. Thus, the correction is significant, against tight anterior structures which may precipitate the PJK.
There are many possible contributors to PJK, such as soft tissue and superior facet injury, but in these young kyphotic patients, there is the additional risk of the soft tissue laxity of immaturity and the very tight, shortened, anterior chest wall to compete against. The modern powerful instrumentation makes correction relatively easy, lengthening the spine with the superior structures under tension from the relatively short anterior chest wall which may result in the proximal failure.
Conclusion
In our series of paediatric TB kyphosis correction, there was a 33% incidence of PJK with 2/9 requiring revision surgery for proximal failure.
Our data suggest that the incidence of PJK was related to the magnitude of correction, the number of levels fused with a trend of increase in higher UIVs, posterior approach and instrumentation.
This suggests that in young children, one should be cautious of overzealous kyphosis correction due to the risk of catastrophic proximal junctional failure.
Key Points
-
Paediatric patients with spinal tuberculosis can develop severe kyphosis.
-
Dramatic correction is possible, but at the risk of PJK.
-
PJK is common post-TB kyphosis correction (33%) when instrumenting.
-
PJK can be catastrophic requiring early revision.
-
Temper kyphotic correction in severe kyphosis and young (< y7 years old).
References
Glattes RC, Bridwell KH, Lenke LG, Kim YJ, Rinella A, Edwards C (2005) Proximal junctional kyphosis in adult spinal deformity following long instrumented posterior spinal fusion: incidence, outcomes, and risk factor analysis. Spine (Phila Pa 1976) 30:1643–1649
Yagi M, Akilah KB, Boachie-Adjei O (2010) Incidence, risk factors and classification of proximal junctional kyphosis: surgical outcomes review of adult idiopathic scoliosis. Spine 36(1):E60–E68
WHO. WHO TB global report 2016 2016 [Available from: https://apps.who.int/iris/bitstream/10665/250441/1/9789241565394-eng.pdf. Accessed 2 Jul 2017
MacPherson DW, Gushulak BD, Baine WB, Bala S, Gubbins PO, Holtom P et al (2009) Population mobility, globalization, and antimicrobial drug resistance. Emerg Infect Dis 15(11):1727–1731
Lau D, Clark AJ, Scheer JK et al (2014) Proximal junctional kyphosis and failure after spinal deformity surgery. A systematic review of the literature as a background to classification development. Spine 39(25):2093–2102
Enam SA, Shah AA (2006) Treatment of spinal tuberculosis: role of surgical intervention. Pak J Neurol sci 1(3):145–151
Reid C, Dunn R (2009) The surgical management of spinal tuberculosis in children and adolescents. S Afr Orthop J 8(4):56–62
Jain AK, Dhammi IK, Jain S, Mishra P (2010) Kyphosis in spinal tuberculosis: prevention and correction. Indian J Orthop 44:127–136
Rajasekaran S (2007) Buckling collapse of the spine in childhood spinal tuberculosis. Clin Orthop Relat Res 460:86–92
Kim HJ, Yagi M et al (2012) Combined anterior-posterior surgery is the most important risk factor for developing proximal junctional kyphosis in idiopathic scoliosis. Clin Orthop Relat Res 470:1633–1639
Lee GA, Betz RR, Clements DH III et al (1999) Proximal kyphosis after posterior spinal fusion in patients with idiopathic scoliosis. Spine 24:795–799
Rhee JM, Bridwell KH, Won D et al (2002) Sagittal plane analysis of adolescent idiopathic scoliosis: the effect of anterior versus posterior instrumentation. Spine 27:2350–2356
Rajasekaran S, Soundarapandian S (1989) Progression of kyphosis in tuberculosis of the spine treated by anterior arthrodesis. J Bone Jt Surg Am 71(9):1314–1323 (22)
Cho W, Kang C, Park Y, Kim H, Cho J (2007) Surgical correction of fixed kyphosis. Asian Spine J 1(1):12–18
Kim YJ, Bridwell KH, Lenke LG, Kim J, Cho SK (2005) Proximal junctional kyphosis in adolescent idiopathic scoliosis following segmental posterior spinal instrumentation and fusion: minimum5-yearfollow-up. Spine (Phila Pa 1976) 30(18):2045–2050
Helgeson MD, Shah SA, Newton PO et al (2010) Harms study group: evaluation of proximal junctional kyphosis in adolescent idiopathic scoliosis following pedicle screw, hook, or hybrid instrumentation. Spine (Phila Pa 1976) 35(2):177–181
Funding
No funding received for study.
Author information
Authors and Affiliations
Contributions
SM: fellow supervised by senior author to obtain ethical approval, collate patient data from sources, prepare spreadsheets for analysis, initial analysis, preparation of primary manuscript for senior author revision. RD: conceptualisation, design, his patient cohort, owner and manager of patient database, review of data, revision of manuscript. Approval of final manuscript and upload process.
Corresponding author
Ethics declarations
Conflict of interest
Dr Mkize has no conflicts. Prof Dunn has in the past served as a speaker for J and J, Medtronic, Nuvasive, Globus and Smith and Nephew. The department receives educational grants from J and J, Medtronic, and Smith and Nephew.
Ethical approval (IRB)
University Ethics approval R039/2013.
Informed consent
During the surgical consent process in our teaching hospital our patients are advised that their data may be used for research in a delinked manner. They are asked for verbal consent whenever clinical photographs are taken – none were used in this article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Mkize, S., Dunn, R. Proximal junctional kyphosis post tuberculous spine corrective surgery in paediatric patients. Spine Deform 9, 169–174 (2021). https://doi.org/10.1007/s43390-020-00186-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43390-020-00186-2