Abstract
This study was designed to (1) investigate the possible mechanisms through which diabetes-induced advanced glycation end products (AGEs) and receptor for AGEs (RAGE) activation can affect male reproductive function; and (2) corroborate the interaction of previously established independent pathways. Male albino Wistar rats (14-weeks old) weighing 250–300 g received either a single intraperitoneal injection of streptozotocin (30 mg/kg or 60 mg/kg), represented as STZ30 or STZ60 respectively, or citrate buffer (control). Diabetes mellitus (DM) was confirmed if plasma glucose levels were ≥ 14 mmol/L after 1 week. Animals were sacrificed after 8 weeks of treatment by an overdose of sodium pentobarbital (160 mg/kg body weight). The testes and epididymides were harvested. The testes were used for biochemical and Western blot analysis, while sperm was retrieved from the epididymis and analysed with computer-aided sperm analysis. The blood glucose levels of STZ60 animals were above the cut-off point and hence these animals were regarded as diabetic. Diabetic animals presented with a non-significant increase in AGE and RAGE expression. Diabetic animals showed a significant increase in the expression of cleaved caspase 3 compared to control (p < 0.001), and these animals also presented with an increase in the expression of JNK (p < 0.05), PARP (p = 0.059) and p38 MAPK (p = 0.1). Diabetic animals also displayed decreased catalase activity accompanied by a non-significant increase in malondialdehyde levels. Additionally, there was a significant decrease in the percentage of progressively motile spermatozoa (p < 0.05) in diabetic animals. This study has shed some light on the interplay between DM, AGE, RAGE and mitogen-activated protein kinase signalling in the testes of diabetic rats, which can result in altered sperm function and contribute to male infertility. However, more studies are needed to better understand this complicated process.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Diabetes mellitus (DM) is an embodiment of various metabolic pathologies. It represents one of the most appreciable health hazards as its prevalence has increased from 177 to 422 million in only 12 years (2002–2014), which connotes a 60% increase [1, 2]. Infertility, a disease of the reproductive system, has become an integral part of global health as it is estimated to affect 60–80 million couples of which 50% is directly attributed to a male factor [3, 4]. Studies have shown that DM affects male reproductive function adversely. Some of the reported effects include a decrease in sperm motility [5, 6], alteration in sperm kinematic properties, increased abnormal sperm morphology [7, 8], decreased seminiferous tubule diameter, increased spermatogenic disruption [9,10,11] and a decreased number of Leydig and Sertoli cells [9, 12].
Baccetti et al. [13] reported that the gonadotropins released in response to GnRH were lower in diabetic men. This was accompanied by a decrease in sperm motility and a higher percentage of sperm immaturity, which indicates that DM may affect male reproduction by interfering with the hypothalamic-pituitary-testicular axis. Additionally, Jiang et al. [14] reported that streptozotocin (STZ)-induced diabetic rats displayed an increase in testicular tunnel positive cells, Bax/Bcl2 ratio and oxidative damage. In the same vein, Roessner et al. [15] reported increased cleaved caspase 3 in the ejaculate of diabetic men. These findings show that DM may affect male reproduction via apoptotic signalling. Furthermore, DM has been shown to increase testicular oxidative damage, which occurs when reactive oxygen species (ROS) exceeds the seminal antioxidant defence ability [16]. This results in cascading reactions, which subsequently lead to sperm DNA damage, mitochondrial DNA fragmentation, altered sperm parameters and ultimately male infertility [17]. Increased ROS production has also been implicated in the generation of advanced glycation end products (AGEs). AGEs are products of non-enzymatic reactions between sugars and the amino groups of proteins, lipids and DNA under hyperglycaemic conditions. AGEs can alter the normal functioning of macromolecules by generating ROS independently or by activating the receptors for advanced glycated end products (RAGE), which leads to a further increase in ROS production by these mutated proteins. RAGE, a multi-ligand member of the immunoglobulin family, interacts with specific ligands. Binding of RAGE to its ligands leads specifically to altered gene expression.
The role of AGE–RAGE activation in the induction of apoptosis has been widely evaluated. Many of these studies were performed on various cell types such as neuronal and endothelial cells [18, 19], as well as periodontal ligament fibroblasts [20]. Additionally, the binding of AGE–RAGE could trigger mitogen-activated protein kinase (MAPK) signalling and the nuclear factor kappa B (NF-κB) pathway, thereby leading to elevated production of ROS and upregulation of intercellular adhesion molecule-1 (ICAM-1), vascular cell adhesion molecule-1 (VCAM-1) and monocyte chemoattractant protein-1 (MCP-1) [21]. Interestingly, AGEs have been suggested to play a role in instigating harm, as they are known to cause ROS production. Excessive ROS can subsequently lead to OS, to which sperm are highly susceptible. It is believed that AGEs may act as a mediator of damage to the reproductive system of diabetic men [22].
Although there are substantial data available on the effects of DM on sperm function, the mechanism through which the effects are exerted is less clearly understood. The present study therefore aimed to investigate the possibility of AGE–RAGE pathway activation in DM-related sperm function impairment and to furthermore corroborate the interaction of previously established independent pathways.
Materials and methods
Animals
Male albino Wistar rats (14-weeks old) weighing 250–300 g were used in this study. Animals were individually housed in standard cages in the Stellenbosch University’s Animal Unit. Both room temperature (23 °C ± 2 °C) and light (12 h light and 12 h dark) were controlled. Ethical approval was obtained from the Stellenbosch University’s Animal Ethics Committee (SU-ACUD16-00101). Rats were treated according to the recommendations of the Laboratory Animal Care of the National Society of Medical Research and the National Institutes of Health’s Guide for the Care and Use of Laboratory Animals [23]. Animals were acclimatized for one week before treatment commenced and had free access to food [standard Epol™ rat chow; Nutritionhub (PTY) LTD, South Africa] and water.
Study design
Thirty rats were randomly divided into three groups (n = 10), namely, a control group and two treatment groups who received STZ. STZ (S0130-IG) was obtained from Sigma (South Africa), and a stock solution (30 mg/ml) was prepared by dissolving it in freshly prepared sodium citrate buffer (pH 4.5). Animals were treated with a single intraperitoneal injection of STZ, either 30 mg/kg body weight (STZ30) or 60 mg/kg body weight (STZ60), while the control group was treated with an equivalent volume (0.5 ml) of citrate buffer. The successful induction of diabetes was confirmed after one week in animals presenting with a non-fasting blood glucose level of ≥ 14 mmol/l, using a Glucoplus™ glucometer. Glucose levels were monitored throughout the 8 weeks treatment period by measuring (non-fasting) once a week. Blood used for the weekly glucose level measurement was collected by pricking the tail vein of the restrained animal. Blood glucose levels are the mean of consecutive measurements.
Experimental procedures
After 8 weeks of treatment, animals were sacrificed by administering an overdose of sodium pentobarbital (160 mg/kg body weight). At the point of sacrifice, the control group had n = 10, STZ30 group had n = 10, while the STZ60 group had n = 8. The testes and epididymides were harvested, weighed and rinsed. The left testis was frozen at − 80 °C until further analysis.
Sperm motility
The harvested left epididymis was placed in a Petri dish containing a 2 ml solution of Hams F-12 nutrient media (Sigma Chemicals, St Louis, MO, USA), at 37 °C. The mature spermatozoa were retrieved into a separate dish containing 2 ml Hams by dissecting the caudal area of the epididymis and allowing sperm to swim out for 30 s. The retrieved spermatozoa (2 µl) were infused into a chamber slide (20 µm, Leja, Netherlands) and placed on a microscope (Nikon Eclipse E200) with an in-built heating stage (37 °C). Sperm motility was measured via computer-aided sperm analysis (CASA) using the Sperm Class Analyser (SCA, Microptic, Barcelona, Spain). Various motility and kinematic parameters were analysed [24].
Biochemical analysis
Oxidative stress parameters
Catalase
Frozen testicular tissue samples were pulverized in liquid nitrogen to prevent thawing and enzymatic reactions. An equal amount (0.05 g) of each sample was placed in an Eppendorf tube containing 50 mg of homogenization beads and 100 µl of cold lysis buffer (Na3PO4, 0.5% Triton X-100). Samples were homogenized by bullet blending at speed 9 for 3 min with a 1-min interval in-between. After bullet blending, an additional 400 µl of lysis buffer was added to allow for total tissue breakdown. Homogenates were centrifuged at 15,000 rpm for 20 min at 4 °C. The supernatants were transferred to different Eppendorf tubes and kept on ice. Tissue homogenates were diluted to 10 × in deionized water and bicinchoninic acid (BCA) assay was used to determine the protein concentration. From the diluted samples and standards, 5 μl was loaded in triplicate into UV microplate wells. Catalase assay buffer (170 μl) was added into each well using a multichannel pipette. Finally, 50 μl of H2O2 was added into the wells and analysis was performed immediately on a plate reader (Multiskan Spectrum) at 240 nm every 60 s over a 5-min period using SkanIt RE for MSS 2.2 (ThermoScientific™ Inc.) software.
Lipid peroxidation (thiobarbituric acid reactive substances (TBARS/MDA)
Frozen testicular tissue samples were pulverized in liquid nitrogen and 0.05 g of each sample was placed in an Eppendorf tube containing 0.05 g of homogenization beads and 0.5 ml of cold lysis buffer (0.1 M KPi, 1.15% KCl). Samples were homogenized by bullet blending at speed 9 for 3 min with a 1-min interval in-between. Supernatants were retrieved for further analysis (BCA and TBARS assays). In order to measure the MDA levels, 100 µl of standards and samples were pipetted into corresponding 10 ml glass tubes. Subsequently, 1 ml of SDS and 2 ml of 10% TCA-BHT buffer solution were added. Samples were vortexed, and after resting for 10 min, 2 ml of thiobarbituric acid (TBA) was added and vortexed again. The standards and samples were covered with marbles and incubated in a water bath (1 h at 100 °C), where after it was cooled on ice for 15 min. The standards and samples were centrifuged (3000 rpm, 15 min 4 °C) and the supernatants retrieved. From the supernatants, 250 μl of each standard and sample were loaded in triplicate into microplate wells and analysed on a plate reader (Multiskan Spectrum) within 30 min after centrifugation at a wavelength of 532 nm.
Western blot analysis
To determine the quantity of proteins in a sample through the Bradford method, 0.05–0.07 g of tissue was pulverized and placed into 700 µl lysis buffer. Seven stainless homogenization beads (1.6 mm, Next Advance Inc., USA) were added into each tube to allow for complete homogenization [25, 26]. The pulverized tissue was bullet blended at speed 8 for 3 min at 5 min interval inbetween. The homogenates were centrifuged for 20 min (15,000 rpm, 4 °C) and the supernatants were removed for further analysis. Tissue lysates were prepared by diluting the sample in Laemmli sample buffer and lysis buffer and boiling it for 5 min, where after 50ug protein/µl was separated by electrophoresis on a 12% SDS-PAGE mini-proteon gel. The running protocol consisted of an initial 10 min electrophoresis at 100 V and 200 mA, followed by 40 min at 200 V and 200 mA. Gels were activated using ChemiDoc (BioRad). Thereafter, the proteins were transferred onto a milipore Immobilon-P transfer membrane (0.45 µm) (Immobilon®-P, Merck Millipore Ltd, Germany). Non-specific sites were blocked with 5% fat-free milk in TBS-Tween.
AGE was measured using Anti-AGE antibody (ab23722; Abcam, SA), and the expression of RAGE was quantified using anti-RAGE antibody (ab361; Abcam, SA). The apoptotic markers measured are caspase 3 (Sigma-Aldrich), caspase 7 (Abcam, SA), PARP (Cell Signalling Technology), p38MAPK (Cell Signalling Technology), C-Jun-N-terminal kinase (JNK) (Cell Signalling Technology) and IkBα (Cell Signalling Technology). A goat anti-mouse/rabbit-horseradish peroxidase-conjugated antibody (Sigma-Aldrich) was used as the secondary antibody. Proteins were detected and visualized using a ChemiDoc (BioRad, USA) and were further normalized (stain-free blots as housekeeping proteins) and analysed with ImageLab 5.0 (ImageLab software, USA). All primary antibodies were diluted in TBS-Tween in a 1:1000 ratio while the secondary antibody was diluted in TBS-Tween in a 1:4000 ratio. All data points are from independent biological repeats (n = 4–5).
Statistical analysis
GraphPad Prism™ software (GraphPad™ Software, Version 8.1.2(332), San Diego, CA, USA) was used for statistical analysis. Normal data distribution was measured using the Shapiro–Wilk, Anderson–Darling, Kolmogorov–Smirnov and D'Agostino–Pearson normality tests. When data passed all normality tests, a one-way ANOVA of variance with a Tukey’s post-hoc test was performed. Where data were not evenly distributed, a Kruskal–Wallis test and a Dunns post-hoc test were carried out. A probability level of p < 0.05 was considered statistically significant and results are expressed as mean ± SEM.
Results
Basic biological parameters
After 8 weeks of treatment, STZ60 animals lost a significant amount of body weight compared to both control and STZ30 (p < 0.0001) (Table 1). Additionally, STZ60 animals presented with a significant increase in blood glucose levels compared to both control and STZ30 (p < 0.0001) (n = 8) (Table 1, Fig. 1).
Sperm motility
STZ60 animals displayed a significant decrease in the percentages of motile and progressively motile spermatozoa compared to the control group (p < 0.05) (n = 8) [Fig. 2a, b; Supplementary Figure (SF) 1]. Although there was a decrease in the progressive motility as well as total motility of STZ30 animals compared to control, the reduction was not statistically significant. Additionally, there was a substantial but non-significant decrease in the sperm kinematic parameters (Table 2) of STZ60 animals compared to both the control and STZ30 groups respectively, [curvilinear velocity (VCL): − 30%, − 30%; straight-line velocity (VSL): − 21%, − 17%; average path velocity (VAP): − 18%, − 9%]. The kinematic parameters of STZ30 animals, despite all six being lower, remained very similar to that of control animals (Table 2).
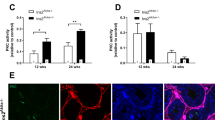
Oxidative stress parameters
STZ60 animals presented with a non-significant decrease (− 65%) of catalase activity compared to the control group, while STZ30 animals displayed a 57.7% reduction of catalase activity compared to control (p = 0.14) (n = 8). This was accompanied by a 96.6% increase in MDA levels in the STZ60 animals and 10% increase in the STZ30 group compared to controls (p = 0.18) (Fig. 3a, b; SF2).
AGE accumulation and RAGE expression
Four different isoforms of AGE proteins were observed, with STZ60 animals showing a non-significant increase in accumulation of each AGE isoform—except for the 70 kDa protein—compared to control (Fig. 4a–f; SF3). Additionally, STZ60 animals displayed a non-significant increase in the total accumulation of AGE isoforms (6.4%) compared to control and STZ30 presented a 2.2% increase compared to the control group (p = 0.6).
The effect of STZ induction on advanced glycation end products (AGE) accumulation. Four different isoforms of AGE proteins were observed: a 70 kDa; b 43 kDa; c 25 kDa; d 17 kDa; e radar plot showing relative distribution of total and individual AGE isomers as a ratio of their respective controls; f blot (probed). The global p for a p = 0.9; b p = 0.9; c p = 0.4; d p = 0.6
In the same vein, four different isoforms of RAGE proteins were observed. The testicular tissue of STZ60 animals showed a 21.7% (p = 0.054) increase in the expression of RAGE (65 kDa) compared to control and a significant increase compared to STZ30 (p < 0.05). The total combined expression of the four RAGE isoforms was 11.7% higher than that of the control group, while STZ30 animals presented with 1.2% non-significant increase compared to the control group (Fig. 5a–f; SF4).
The effect of STZ induction on receptor for advanced glycation end products (RAGE) accumulation. Four different isoforms of RAGE proteins were observed: a 65 kDa; b 50 kDa; c 43 kDa; d 37 kDa; e radar plot showing relative distribution of total and individual RAGE isomers as a ratio of their respective controls; f blot (probed). *p < 0.05 versus STZ30. The global p for a p = 0.02; b p = 0.9; c p = 0.7; d p = 0.2
Apoptotic markers
STZ60 animals exhibited a highly significant increase in the expression of cleaved caspase 3 compared to both control (p < 0.001) and STZ30 (p < 0.001). Additionally, there was a 30% increase in the total expression of caspase 7 of STZ60 animals compared to control and a 20% increase in STZ30 group compared to the control group (p = 0.056). Although not significant, both of the STZ groups showed increased PARP cleavage compared to the control (p = 0.059) (Fig. 6a–f; SF5).
The effect of STZ induction on apoptosis activation: a cleaved caspase 3; b caspase 7; c PARP; d blot for caspase 3 (probed); e blot for caspase 7 (probed); f blot for PARP (probed). @p < 0.001 versus control; #p < 0.001 versus STZ30. The global p for cleaved caspase 3 p = 0.0008, caspase 7 p = 0.1, PARP p = 0.059
Also observed was a non-significant gradual increase in p38MAPK expression relative to the increase in STZ concentration administered (p = 0.2). STZ60 animals further presented with a significant increase in the expression of JNK 46 kDa (p < 0.05) compared to the control group. A non-significant increase in JNK55kDa was also observed compared to control (25.6%) and STZ30 (36.3%) respectively (p = 0.1) (Fig. 7a–f; SF6).
Discussion
Diabetes has been shown to affect male reproductive function by altering hormone regulation and increasing OS, thereby causing testicular dysfunction and altering spermatogenesis [10, 27, 28]. These effects subsequently result in decreased total and progressively motile spermatozoa and reduced normal sperm morphology [11, 17, 29]. However, the pathway(s) through which the effects are exerted is little understood. Hence, the current study was performed in order to investigate the possibility of alternative pathways through which DM could affect sperm function.
In the current study, STZ60 animals presented with significantly elevated blood glucose levels that were far above the normal reference range, accompanied by a substantial loss in body weight. These are typical features of type 1 DM. STZ30 animals, on the other hand, presented with only a 6.4% non-significant increase in blood glucose, which remained within the normal physiological range. Interestingly, these animals furthermore displayed a significant increase in body weight. The increase in glucose levels and decreased body weight observed in STZ60 animals might be explained by the inability to utilize the glucose derived from the food as a consequence of the ablated pancreatic β-cells and subsequent lack of insulin signalling. Hence, the STZ60 group could be regarded as a typical type 1 DM model [30, 31].
Diabetic animals from the current study presented with a decrease in the percentage of total and progressively motile spermatozoa. This concurs with Bhattacharya et al. [32] who reported decreased sperm motility parameters in diabetic men and is also supported by Singh et al. [30] who showed impaired sperm motility in STZ-induced diabetic rats. DM animals of the present study displayed a decrease in catalase activity and increased MDA levels. This is in agreement with the findings of Adaramoye and Lawal [33], who similarly reported increased lipid peroxidation and decreased activities of catalase, SOD and GPx in diabetic rats. Hyperglycaemia has been reported to cause increased OS in various tissues [34], including testicular tissue [35] and spermatozoa [36]. This is evidenced by another study that reported elevated MDA levels, lipid hydroperoxides and lipid peroxides in the plasma of type 1 diabetic patients [37]. In the diabetic state, lipid peroxidation can be induced by protein glycation and glucose auto-oxidation that can further lead to the formation of free radicals [38]. The damage that these free radicals impose on cells may be quantitatively determined by measuring MDA levels, which is a product of lipid peroxidation [39]. The increase in lipid peroxidation may be the result of the imbalance between the oxidant and antioxidant activities. This is supported by Buttke and Sandstrom [40] who reported that under an elevated OS status, ROS cause cellular injury via several mechanisms, including lipid peroxidation and oxidative damage of proteins and DNA. These findings are backed up by other studies which also reported a relationship between ROS and DNA damage [41, 42].
Furthermore, an increase in the production of ROS has been shown to cause the non-enzymatic and progressive glycation of proteins with the consequently increased formation of glucose-derived AGEs. The modified proteins further cause an increase in ROS formation and aggravation of OS [43, 44] after binding to the ligand-receptor, RAGE.
AGE–RAGE activation has been implicated in the development and progression of several diseases, both metabolic and non-metabolic. This is evidenced by Chen et al. [18] who showed that the excessive production of oxidants in the endothelial progenitor cells (EPCs) resulted in RAGE-mediated AGE accumulation with resultant inhibition of cell proliferation, migration and adhesion, which were all attenuated after RAGE blockage. In the same vein, inhibition of RAGE aided the protective effect of glucagon-like peptide-1 on AGE-induced apoptotic neuronal cells [45]. Observed in the current study is an increase in the expression of RAGE in the testes of diabetic animals. This result concurs with Mallidis et al. [46] who reported increased RAGE, not only in the testes but also in the epididymis, sperm and seminal plasma of diabetic men. This study further reported that the increased RAGE expression contributed to the elevated levels of damaged nDNA observed in the spermatozoa.
An association has been reported between AGE–RAGE activation and MAPKs signalling [47,48,49]. MAPKs are activated in response to external stimuli. Upon external stimulation, mitogen-activated protein kinase kinase kinase (MAPKKK) is phosphorylated, thereby activating two different subgroups of mitogen-activated protein kinase kinase (MAPKK) (MKK3/MKK6 and MKK4). These dual kinases phosphorylate and activate p38 MAPK and JNK [50]. P38MAPK and JNK have been implicated in the development and progression of human diseases. Adhikary et al. [51] described the accumulation of p38 MAPK in the interstitial macrophages and myofibroblasts in the kidneys of both diabetic male mice and human. It is associated with increased HbA1c levels and albuminuria and ultimately lead to interstitial fibrosis. Additionally, p38 MAPK and JNK accumulation have been associated with apoptosis [52, 53]. Another study reported the activation of p38MAPK, followed by stimulation of cytochrome c release, caspase 8 and 3 activation, PARP cleavage and DNA fragmentation in induced apoptosis of human promyelocytic leukaemia HL‐60 cells. The apoptotic events were repressed when p38 was blocked, which suggests that p38 phosphorylation occurred prior to caspase activation [54]. It was also showed that p38 MAPK is an instigator of Bcl2-x (Bax) activation and mitochondrial apoptosis in primary keratinocytes [55]. In the current study, we investigated if diabetes can affect male reproductive function through the p38 MAPK-apoptotic pathway. Similar to the previous studies, there was an increase in the level of JNK and caspase 3 and an increasing trend in p38 MAPK, caspase 7 and PARP cleavage in the testes of diabetic rats. The activation of p38 has been described to phosphorylate, activate and translocate Bcl2, Bax and Bcl-xl. The translocation causes a change in the mitochondrial membrane potential and thus lead to cytochrome c release, which further activates the cleavage of pro-apoptotic caspases. Additionally, JNK has been shown to induce apoptosis through FASL signalling. Increase in JNK expression stimulates FAS/FASL and subsequent phosphorylation of Bid (a Bcl-2 family) and the release of cytochrome c, or it recruits caspase 8 through adaptor protein FAAD and thus cleaves caspase 3. Jiang et al. [14] reported activation of the apoptotic pathway, as evidenced by increased expression of cleaved caspase 3 and caspase 8 and subsequently altered spermatogenesis. Additionally, Metzler et al. [56] reported that spermatocyte loss in AZFc-deleted patients occurs through apoptotic pathway activation. Furthermore, a significant association was found between caspase 3 activation and increased sperm DNA fragmentation [57]. In corroboration with previous studies, the current study suggests a possible pathway and association between DM and male infertility, as explained in Fig. 8.
The proposed mechanisms through which diabetes may affect male reproductive function. ↓ = decrease, ↑ = increase. In DM, there is altered antioxidant enzyme activity (↓Catalase) which may result in OS. The development of OS can on one arm instigate the breakdown of polyunsaturated fatty acids (MDA) and indirectly increase AGE formation. The peroxidation of PUFA attracts more ROS formation, which can activate apoptotic induction, resulting in impaired sperm function. Due to the presence of RAGE ligand, AGE, binding occurs. The AGE–RAGE complex initiates the activation of the MAPKs, which may induce apoptosis by increasing the cleavage of PARP, hence resulting in nDNA damage. All these effects collectively result in reduced male fertility
The current study highlighted the possible inter-connected mechanism through which diabetes may confer its impact on the male reproductive function, which may further contribute to male infertility (Fig. 8). We therefore conclude that there is an association between AGE–RAGE activation and MAPKs signalling. The increase in the expression of JNK and caspase 3 and the non-significant increase in the expression of p38 MAPK, caspase 7 and PARP cleavage in the testes of diabetic rats reveal a deadly liaison, which can result in altered sperm function and may further contribute to male infertility.
Abbreviations
- AGE:
-
Advanced glycation end product
- BCA:
-
Bicinchoninic acid
- CASA:
-
Computer aided sperm analysis
- DM:
-
Diabetes mellitus
- DNA:
-
Deoxyribonucleic acid
- GnRH:
-
Gonadotropin-releasing hormone
- ICAM-1:
-
Intercellular adhesion molecule-1
- JNK:
-
C-Jun N-terminal kinase
- MAPKs:
-
Mitogen-activated protein kinase
- MCP-1:
-
Monocyte chemoattractant protein-1
- MDA:
-
Malondialdehyde
- Nf-kB:
-
Nuclear factor kappa B
- OS:
-
Oxidative stress
- PARP:
-
Poly adenosine diphosphate-ribose polymerase
- PUFA:
-
Polyunsaturated fatty acid
- RAGE:
-
Receptor for advanced glycation end product
- ROS:
-
Reactive oxygen species
- SF:
-
Supplementary figure
- STZ:
-
Streptozotocin
- TBA:
-
Thiobarbituric acid
- VCAM-1:
-
Vascular cell adhesion molecule-1
References
World Heallth Organization (2010) Diabetes fact sheet. NMH Fact Sheet February 2010
World Health Organization (2014) Global report on diabetes, vol 58, pp 1–88. https://www.who.int/about/licensing/copyright_form/index.html. Accessed 19 Aug 2019
Jacky B, Laura B, John AC, Nygren KG (2007) International estimates of infertility prevalence and treatment-seeking: potential need and demand for infertility medical care. Hum Reprod 22:1506–1512
Zegers-Hochschild F, Adamson GD, de Mouzon J, Ishihara O, Mansour R, Nygren K, Sullivan E, Vanderpoel S (2009) International Committee for Monitoring Assisted Reproductive Technology (ICMART) and the World Health Organization (WHO) revised glossary of ART terminology, 2009. Hum Reprod 24:2683–2687
Ceriello A (2000) Oxidative stress and glycemic regulation. Metabolism 49:27–29
Delfino M, Imbrogno N, Elia J, Capogreco F, Mazzilli F (2007) Prevalence of diabetes mellitus in male partners of infertile couples. Minerva Urol Nefrol 59:131–135
Rehman K, Beshay E (2001) Diabetes and male sexual function. J Sex Reprod Med 1:29–33
Alves MG, Martins AD, Rato L, Moreira PI, Socorro S, Oliveira PF (2013) Molecular mechanisms beyond glucose transport in diabetes-related male infertility. Biochim Biophys Acta Mol Basis Dis 1832:626–635. https://doi.org/10.1016/j.bbadis.2013.01.011
Ballester J, Rigau T, Rodríguez-Gil JE, Muñoz MC, Domínguez J, Guinovart JJ (2004) Insulin-dependent diabetes affects testicular function by FSH- and LH-linked mechanisms. J Androl 25:706–719
Maresch CC, Stute DC, Ludlow H, Hammes HP, de Kretser DM, Hedger MP, Linn T (2017) Hyperglycemia is associated with reduced testicular function and activin dysregulation in the Ins2Akita+/− mouse model of type 1 diabetes. Mol Cell Endocrinol 446:91–101. https://doi.org/10.1016/j.mce.2017.02.020
Omolaoye TS, Skosana BT, du Plessis SS (2018) Diabetes mellitus-induction: effect of different streptozotocin doses on male reproductive parameters. Acta Histochem 120:103–109
Jelodar G, Khaksar Z, Pourahmadi M (2010) Endocrine profile and testicular histomorphometry in neonatal rats of diabetic mothers. Vet Arh 80:421–430
Baccetti B, La Marca A, Piomboni P, Capitani S, Bruni E, Petraglia F, De Leo V (2002) Insulin-dependent diabetes in men is associated with hypothalamo-pituitary derangement and with impairment in semen quality. Hum Reprod 17:2673–2677
Jiang X, Zhang C, Xin Y, Huang Z, Tan Y, Huang Y, Wang Y, Feng W, Li X, Li W, Qu Y, Cai L (2013) Protective effect of FGF21 on type 1 diabetes-induced testicular apoptotic cell death probably via both mitochondrial- and endoplasmic reticulum stress-dependent pathways in the mouse model. Toxicol Lett 219:65–76. https://doi.org/10.1016/j.toxlet.2013.02.022
Roessner C, Paasch U, Kratzsch J, Glander HJ, Grunewald S (2012) Sperm apoptosis signalling in diabetic men. Reprod Biomed 25:292–299
Du Plessis SS, Agarwal A, Halabi J, Tvrda E (2015) Contemporary evidence on the physiological role of reactive oxygen species in human sperm function. J Assist Reprod Genet 32:509–520
Mangoli E, Talebi AR, Anvari M, Pourentezari M (2013) Effects of experimentally-induced diabetes on sperm parameters and chromatin quality in mice. Iran J Reprod Med 11:53–60
Chen J, Song M, Yu S, Gao P, Yu Y, Wang H, Huang L (2010) Advanced glycation endproducts alter functions and promote apoptosis in endothelial progenitor cells through receptor for advanced glycation endproducts mediate overpression of cell oxidant stress. Mol Cell Biochem 335:137–146
Ramasamy R, Vannucci SJ, Yan SS, Herold K, Yan SF, Schmidt AM (2005) Advanced glycation end products and RAGE: a common thread in ageing, diabetes, neurodegeneration, and inflammation. Glycobiology 15:16–28
Li DX, Deng TZ, Lv J, Ke J (2014) Advanced glycation end products (AGEs) and their receptor (RAGE) induce apoptosis of periodontal ligament fibroblasts. Braz J Med Biol Res 47:1036–1043
Hoefen RJ, Berk BC (2002) The role of MAP kinases in endothelial activation. Vascul Pharmacol 38:271–273
Mallidis C, Agbaje IM, Rogers DA, Glenn JV, Pringle R, Atkinson AB, Steger K, Stitt AW, McClure N (2009) Advanced glycation end products accumulate in the reproductive tract of men with diabetes. Int J Androl 32:295–305
Committee for the Update of the Guide for the Care and Use of Laboratory Animals, National Research Council (2010) Guide for the care and use of laboratory animals, 8th edn. National Research Council, Washington
Oyeyipo IP, Maartens PJ, du Plessis SS (2015) Diet-induced obesity alters kinematics of rat spermatozoa. Asian Pac J Reprod 4:235–239. https://doi.org/10.1016/j.apjr.2015.06.008
Bradford MM, Bradford MM (1976) A rapid and sensitive microgram quantities of protein utilizing the priciple of protein dye biding. Anal Biochem 72:248–254
Marais E, Genade S, Huisamen B, Strijdom JG, Moolman JA, Lochner A (2001) Activation of p38 MAPK induced by a multi-cycle ischaemic preconditioning protocol is associated with attenuated p38 MAPK activity during sustained ischaemia and reperfusion. J Mol Cell Cardiol 33:769–778
Sexton WJ, Jarow JP (1997) Effect of diabetes mellitus upon male reproductive function. Urology 49:508–513
Fedele D (2005) Therapy insight: sexual and bladder dysfunction associated with diabetes mellitus. Nat Clin Pract Urol 2:282
Navarro-Casado L, Juncos-Tobarra MA, Cháfer-Rudilla M, Íñiguez De Onzoño L, Blázquez-Cabrera JA, Miralles-García JM (2010) Effect of experimental diabetes and STZ on male fertility capacity. Study in rats. J Androl 31:584–592
Singh S, Malini T, Rengarajan S, Balasubramanian K (2009) Impact of experimental diabetes and insulin replacement on epididymal secretory products and sperm maturation in albino rats. J Cell Biochem 108:1094–1101
Vikram A, Tripathi DN, Ramarao P, Jena GB (2008) Intervention of d-glucose ameliorates the toxicity of streptozotocin in accessory sex organs of rat. Toxicol Appl Pharmacol 226:84–93
Bhattacharya SM, Ghosh M, Nandi N (2014) Diabetes mellitus and abnormalities in semen analysis. J Obstet Gynaecol Res 40:167–171
Adaramoye OA, Lawal SO (2014) Effect of kolaviron, a biflavonoid complex from Garcinia kola seeds, on the antioxidant, hormonal and spermatogenic indices of diabetic male rats. Andrologia 46:878–886
Giacco F, Brownlee M (2010) Oxidative stress and diabetic complications. Circ Res 107:1058–1070
Ricci G, Catizone A, Esposito R, Pisanti FA, Vietri MT, Galdieri M (2009) Diabetic rat testes: morphological and functional alterations. Andrologia 41:361–368
Khaki A, Fathiazad F, Nouri M, Khaki AA, Maleki NA, Khamnei HJ, Ahmadi P (2010) Beneficial effects of quercetin on sperm parameters in streptozotocin-induced diabetic male rats. Phyther Res 24:1285–1291
Martín-Gallán P, Carrascosa A, Gussinyé M, Domínguez C (2003) Biomarkers of diabetes-associated oxidative stress and antioxidant status in young diabetic patients with or without subclinical complications. Free Radic Biol Med 34:1563–1574
Mullarkey CJ, Edelstein D, Brownlee M (1990) Free radical generation by early glycation products: a mechanism for accelerated atherogenesis in diabetes. Biochem Biophys Res Commun 173:932–939
Mayorga-Torres BJM, Camargo M, Cadavid P, du Plessis SS, Cardona-Maya WD (2017) Are oxidative stress markers associated with unexplained male infertility? Andrologia 49:e12659
Buttke TM, Sandstrom PA (1994) Oxidative stress as a mediator of apoptosis. Immunol Today 15:7–10
Du Plessis SS, McAllister DA, Luu A, Savia J, Agarwal A, Lampiao F (2010) Effects of H2O2 exposure on human sperm motility parameters, reactive oxygen species levels and nitric oxide levels. Andrologia 42:206–210
Mahfouz RZ, du Plessis SS, Aziz N, Sharma R, Sabanegh E, Agarwal A (2010) Sperm viability, apoptosis, and intracellular reactive oxygen species levels in human spermatozoa before and after induction of oxidative stress. Fertil Steril 93:814–821. https://doi.org/10.1016/j.fertnstert.2008.10.068
Nicholl ID, Bucala R (1998) Advanced glycation endproducts and cigarette smoking. Cell Mol Biol (Noisy-le-grand) 44:1025–1033
Valencia JV, Weldon SC, Quinn D, Kiers GH, DeGroot J, TeKoppele JM, Hughes TE (2004) Advanced glycation end product ligands for the receptor for advanced glycation end products: biochemical characterization and formation kinetics. Anal Biochem 324:68–78
Chen S, Yin L, Xu Z, An FM, Liu AR, Wang Y, Yao WB, Gao XD (2016) Inhibiting receptor for advanced glycation end product (AGE) and oxidative stress involved in the protective effect mediated by glucagon-like peptide-1 receptor on AGE induced neuronal apoptosis. Neurosci Lett 612:193–198. https://doi.org/10.1016/j.neulet.2015.12.007
Mallidis C, Agbaje I, Rogers D, Glenn J, McCullough S, Atkinson AB, Steger K, Stitt A, McClure N (2007) Distribution of the receptor for advanced glycation end products in the human male reproductive tract: prevalence in men with diabetes mellitus. Hum Reprod 22:2169–2177
Yang J, Zhu T, Liu X, Zhang L, Yang Y, Zhang J, Guo M (2015) Heat shock protein 70 protects rat peritoneal mesothelial cells from advanced glycation end-products-induced epithelial-to-mesenchymal transition through mitogen-activated protein kinases/extracellular signal-regulated kinases and transforming growth fact. Mol Med Rep 11:4473–4481
Wu Q, Li S, Li X, Sui Y, Yang Y, Dong L, Xie B, Sun Z (2015) Inhibition of advanced glycation endproduct formation by lotus seedpod oligomeric procyanidins through RAGE-MAPK signaling and NF-κB activation in high-fat-diet rats. J Agric Food Chem 63:6989–6998
Taguchi A, Blood DC, Del-Toro G, Canet A, Lee DC, Qu W, Tanjl N, Lu Y, Lalla E, Fu C, Hofmann MA, Kislinger T, Ingram M, Lu A, Tanaka H, Hori O, Ogawa S, Stern DM, Schmidt AM (2000) Blockade of RAGE-amphoterin signalling suppresses tumour growth and metastases. Nature 405:354–360
Ichijo H, Nishida E, Irie K, Dijke PT, Saitoh M, Moriguchi T, Takagi M, Matsumoto K, Miyazono K, Gotoh Y (1997) Induction of apoptosis by ASK1, a mammalian MAPKKK that activates SAPK/JNK and p38 signaling pathways. Science 275:90–94
Adhikary L, Chow F, Nikolic-Paterson DJ, Stambe C, Dowling J, Atkins RC, Tesch GH (2004) Abnormal p38 mitogen-activated protein kinase signalling in human and experimental diabetic nephropathy. Diabetologia 47:1210–1222
Farley N, Pedraza-Alva G, Serrano-Gomez D, Nagaleekar V, Aronshtam A, Krahl T, Thornton T, Rincón M (2006) p38 Mitogen-activated protein kinase mediates the Fas-induced mitochondrial death pathway in CD8+ T cells. Mol Cell Biol 26:2118–2129
Taylor CA, Zheng Q, Liu Z, Thompson JE (2013) Role of p38 and JNK MAPK signaling pathways and tumor suppressor p53 on induction of apoptosis in response to Ad-eIF5A1 in A549 lung cancer cells. Mol Cancer 12:1–11
Park SJ, Kim IS (2005) The role of p38 MAPK activation in auranofin-induced apoptosis of human promyelocytic leukaemia HL-60 cells. Br J Pharmacol 146:506–513
Nys K, Van Laethem A, Michiels C, Rubio N, Piette JG, Garmyn M, Agostinis P (2010) A p38MAPK/HIF-1 pathway initiated by UVB irradiation is required to induce noxa and apoptosis of human keratinocytes. J Invest Dermatol 130:2269–2276. https://doi.org/10.1038/jid.2010.93
Metzler-Guillemain C, Grillo J-M, Mitchell MJ, Karsenty G, Saias-Magnan J, Streichemberger E, Perrin J, Malzac P (2012) Case report of apoptosis in testis of four AZFc-deleted patients: increased DNA fragmentation during meiosis, but decreased apoptotic markers in post-meiotic germ cells. Hum Reprod 27:1939–1945
Manente L, Pecoraro S, Picillo E, Gargiulo U, Gargiulo P, De Luca A, Politano L (2015) Molecular evidence of apoptotic pathway activation in semen samples with high DNA fragmentation. Vivo (Brooklyn) 29:289–294
Acknowledgements
The authors would like to thank Dr. Michelle Smit-van Schalkwyk and Dr. Shantal Windvogel for the generous donation of tissue samples and Harry Crossley Foundation for the research grant provided.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Omolaoye, T.S., Du Plessis, S.S. The effect of streptozotocin induced diabetes on sperm function: a closer look at AGEs, RAGEs, MAPKs and activation of the apoptotic pathway. Toxicol Res. 37, 35–46 (2021). https://doi.org/10.1007/s43188-020-00040-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43188-020-00040-7