Abstract
Background/purpose
Ventriculoperitoneal (VP) shunt is a common procedure used to drain cerebrospinal fluid to treat hydrocephalus. Advances in laparoscopy tools and techniques made it possible to perform this procedure laparoscopically assisted. Complications of this procedure are also amenable to laparoscopic correction. This study outlines the safety and feasibility of laparoscopy in performing the procedure and management of its complications.
Methods
A retrospective file review for all cases underwent laparoscopic-assisted VP shunt or laparoscopic management of one of its complications in the period 2015–2019. Laparoscopic-assisted procedure was done either by 3-port technique or a peritoneocentesis needle technique. Management of complications was done according to its nature.
Results
Over 4 years, we performed 36 laparoscopic-assisted VP shunt placement and 17 laparoscopic interventions for abdominal complications related to VP shunts. There were no intraoperative or postoperative complications related to the laparoscopic technique. Conversion to conventional laparotomy was done in 3 patients presented with hugely infected CSF pseudocysts with amalgamated intestine with the wall of the cyst.
Conclusion
Laparoscopic-assisted VP shunt placement and revisions in children are feasible and safe. No special tools are required for the procedure.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cerebrospinal fluid (CSF) shunting is the most common technique used by neurosurgeons for management of pediatric, adolescent and adult patients with hydrocephalus. Ventriculoperitoneal, lumboperitoneal and ventriculoatrial shunts are used for CSF diversion (1, 2). The reported complications following ventriculoperitoneal (VP) shunts placements were 5%–47% and the majority were related to distal catheter problems. Abdominal complications related to the VP shunt placement include: subcutaneous collection of CSF, distal catheter obstruction, infection, CSF pseudocyst formation, disconnection, displacement, CSF ascites, fracture of the tube, umbilical or inguinal hernia, intestinal obstruction, strangulation and peritonitis (3–6).
The advances in minimal invasive surgery techniques enabled laparoscopic-assisted insertion of peritoneal shunts (7).
In addition, laparoscopy has been employed efficaciously for treatment of distal shunt complications (8–10). We present our experience and outline the role of laparoscopy in VP shunt placement and management of VP shunt distal catheter complications.
Methods
This study is a retrospective file review study. The records of all cases that underwent VPS placements and revisions at Tanta university hospital and its affiliated regional hospitals from September 2015 to September 2019 were reviewed. Cases lost in follow-up or with incomplete files were excluded.
Thirty-six files for patients underwent laparoscopic-assisted VP shunts, and 17 files for patients who underwent laparoscopic intervention for management of abdominal complications of VP shunts were retrieved. Charts were designed to collect the following data from the records: patient demographic, associated conditions, initial shunt placement and indication for revision, investigations done, intra-operative details, length of hospital stay, post-operative outcome and length of follow-up period. Data were presented in descriptive statistics tables.
The study was approved by the ethical committee of Tanta faculty of medicine. All patients underwent laparoscopic-assisted VPS insertions and revisions were performed by interdisciplinary team including a neurosurgeon for the cranial part and a pediatric surgeon for the laparoscopic part of the procedure.
Laparoscopic-assisted VP shunt placement
A dose of prophylactic fourth-generation cephalosporin (50 mg/kg) was given to all patients with induction of general anesthesia. While the patient was in a supine position with the head tilted laterally, the neurosurgeon performed the cranial part of the procedure by making a burr hole in the corner of the anterior fontanel. After placing the ventricular catheter which is connected to a valve, a tunneller was used to lead the catheter subcutaneously in the chest to the point of puncture at the abdominal wall. The pediatric surgeon started the abdominal part at the same time by insertion of a 3–5 mm trocar for 30º scope via open technique. Insufflation of the abdomen by carbon dioxide was made to create a pressure 8–12 mmHg according to the age of the patient. The peritoneocentesis was done by two methods. In the first method, after inspection of the abdomen, a second, 3–5 mm trocar was inserted to the right side of the umbilicus just beneath the costal margin at the end of the catheter tube and another 3–5 mm trocar was inserted in the left iliac region. A grasper was entered into the abdomen from the port in left iliac region to get out through the port in right subcostal site. The grasper catches and withdraws the tip of the catheter from the subcutaneous tissue into the peritoneal cavity under telescopic vision (Fig. 1). In the second method, a peritoneocentesis trocar was inserted under the xiphoid process via a 0.5-cm skin incision just at the site of tip of the tunneled catheter. The trocar punctured the peritoneum and drilled into the falciform ligament of the liver and the stylet was removed, and then the distal catheter was inserted into the abdominal cavity through the trocar (11) (Fig. 2). If there was an old abdominal scar, then the needle can be inserted in another place. The patency of the catheter was confirmed through dripping of CSF in the peritoneal cavity via telescopic vision. Lastly, the abdomen was deflated, the trocars were removed and the skin incisions were closed.
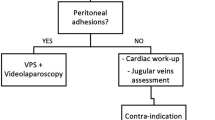
Laparoscopic management of distal catheter complications
A dose of prophylactic fourth-generation cephalosporin (50 mg/kg) was given to all patients with induction of general anesthesia. The patient was placed in the supine position with tilting of the head to the right or left depending on the position of the shunt tube in the previous surgery. Open technique for insertion of a 5 mm umbilical port for a 30º scope was done. The abdominal cavity was explored, and then two 3–5 mm ports were inserted according to the patient’s age. The site of the trocars varied according to the preoperative diagnosis.
In case of mechanical intestinal obstruction due to adhesions between bowel and abdominal wall, adhesiolysis was performed using laparoscopic scissors and bipolar electrocautery and the catheter was extracted and repositioned in the peritoneal cavity.
In cases of CSF peudocyst formation, the pseudocyst was aspirated using a laparoscopic suction device, the cyst wall was partially excised, and the catheter was freed up, extracted and repositioned in the peritoneal cavity away from the amalgamation.
In congenital inguinal hernias, the hernia sac was disconnected using laparoscopic scissors at the internal inguinal ring followed by peritoneal closure using 2/0 or 3/0 absorbable sutures (Vicryl, Ethicon, USA.
In cases of subcutaneous cyst with shunt displacement, aspiration of the cyst, deroofing or complete excision of its wall was performed and the catheter was repositioned in the peritoneal cavity under telescopic vision.
In cases of fistulous opening discharging CSF at the umbilicus, dissection of the fistulous tract was done using laparoscopic scissors; the tract was opened and the catheter was freed up and repositioned under telescopic vision into the peritoneum and the umbilical defect was closed using non-absorbable sutures (Fig. 3).
Results
Over 4 years, we performed 36 laparoscopic-assisted VP shunt placement (30 patients using 3 ports technique and 6 patients using peritoneocentesis needle) and 17 laparoscopic interventions for abdominal complications related to VP shunts. Etiologies for VPS insertion included aqueductal stenosis (n = 16), communicating hydrocephalus (congenital 4 cases, post infection 6 cases, post hemorrhagic 6 cases) and tumors (n = 4).
In laparoscopic insertion using peritoneocentesis trocar (6 patients), there were 4 males and 2 females, their ages ranged from 9 months to 6 years, and the duration of laparoscopic part of the operation ranged from 8 to 16 min (mean, 12.3 ± 1.7 min). Among them, only one patient had history of appendectomy operation. No intra-abdominal complications were detected. The mean follow-up period was 12.11 ± 9.29 months with no detectable postoperative complications related to laparoscopy (Table 1, 2).
In laparoscopic insertion using 3-port technique (30 patients), there were 19 males and 11 females, their ages ranged from 7 months to 15 years, and the duration of the laparoscopic part of the operation ranged from 15 to 26 min (mean 18.5 ± 2.1 min). Among them, 4 patients had history of previous abdominal surgery. No intra-abdominal complications were detected. The mean follow-up period was 9.34 ± 2.25 months. Four patients had post-operative umbilical port infection which was treated with antibiotics and daily dressing (Tables 1, 2).
In laparoscopic revisions of VPS (17 patients), all patients were referred by a neurosurgeons and the previous distal shunt placement was done using open technique. There were 11 males and 6 females, their ages ranged from 4 months to 15 years (Table 1), and the type of complication and the laparoscopic procedure performed for each case were illustrated in (Table 2).
The mean operative time of the laparoscopic procedure varied according to the procedures performed. It was 126 ± 9 min in abdominal pseudocysts, 48 ± 5 min in recurrent inguinal hernias, 112 ± 7 min in adhesive intestinal obstruction, 37 min in subcutaneous cyst, 25 ± 2 min in extraction of rupture distal shunt tube and 35 min in umbilical fistula (Table 3). The length of hospital stay varied according to the procedure performed; it ranged from one day in laparoscopic congenital inguinal hernia repair to 5 days in laparoscopic management of CSF pseudocysts (Table 3). There were no intraoperative or postoperative complications related to the laparoscopic technique except for infection at the port site in 3 cases in laparoscopic insertion of VPS and also in 3 cases in laparoscopic revisions. Conversion to conventional laparotomy was done in 3 patients presented with hugely infected CSF pseudocysts with amalgamated intestine with the wall of the cyst. The mean follow-up period was 8.36 ± 2.18 months in all cases.
Discussion
VP shunt is a common procedure performed by neurosurgeons for treatment of hydrocephalus (12). Various techniques have been advocated for placement of the distal ends of the shunt tubes in the peritoneal cavity, including mini-laparotomy, trocar puncture of the abdominal wall and laparoscopy (13). Advances in minimal invasive surgery have made laparoscopic insertion of VPSs catheters safer and efficacious (14, 15).
Many papers reported favorable outcome of laparoscopic-assisted VP shunt placements in pediatric patients due to many benefits: shorter operative time, minimal access incision, less blood loss, assurance of the proper placement of the tubes in the peritoneal cavity and telescopic confirmation of the free flow of CSF through the distal opening. In addition, previous abdominal surgery with presence of scar tissue and peritoneal adhesions can predispose to intestinal injury, distal catheter misplacement and shunt obstruction during conventional VP shunt placement (16).
Laparoscopy was used to minimize such operative and postoperative complications and reduce the percentage of VP shunt revisions (17).
Theoretically, laparoscopy was thought to carry a high risk in neonates due to limited space of the abdominal cavity and the risk of pneumoperitoneum which may lead to temporary shunt dysfunction (18). Most reports on the use of laparoscopy in VP shunt placements in children proved the safety of this technique in patients older than 1 year of age and over 10 kg. Handler et al. were the first to prove the safety of laparoscopy in VP shunt placement with 10% failure rate in their cohort study (17). This study added evidence to the literature on and the favorable outcome in infants and children.
Many laparoscopic shunt tube placement strategies were reported in the literature, the majority of these techniques enable the surgeon to insert the distal catheter in the peritoneal and pelvic cavity, but this position was changed with the movement of the patients and may be wrapped or engulfed within the omentum (24, 25). In the current study, we used two techniques for VPS placements. Early in the study, we started by 3-port technique. Then, when peritoneocentesis needle became available, it was used in all patients. The peritoneocentesis needle has many advantages over the 3-port technique: it has a short time of insertion, and it required a small single incision with small fascial and peritoneal opening.
Until recently, the intraperitoneal complications of VPS were managed by conventional laparotomy and removal of existing shunt tube. Currently, laparoscopic surgical techniques are used not only for VP shunt placement, but also for revisions and management of its complications (8).
Intra-abdominal migration of VP shunt was reported due to either fracture or disconnection with slippage of the distal catheter into the abdomen. Distal VP shunts disconnection represents 15% of shunt malfunction in children (19). Disconnected catheters may adhere to abdominal organs and it is recommended not to be extracted forcefully to avoid organ injury (20). CSF pseudocyst was first described by Harsh in 1954 (21). It represents 0.7–10% of VP shunt complications (8, 22). Several factors were responsible for CSF pseudocyst accumulation: infection, high CSF protein component and tumors (23).
CSF pseudocysts were a frequent complication in the current study, and were managed by laparoscopic aspiration using a laparoscopic suction device, excision or deroofing of the cyst wall and repositioning of catheter in the peritoneal cavity. Conversion to conventional laparotomy was done in two cases due to large infected cyst leading to intraperitoneal abscess with amalgamated intestine with the wall of the cyst.
Infection represents a common complication of VP shunt placements and it occurs in 5–11% of cases (24).
Some reports indicate an increase in this risk with laparoscopy especially with the umbilical incision (25). Fahy et al. report that there was not a statistically significant increase in infection rates in their study (26). This was confirmed in the current study.
The current study confirms the safety and feasibility of laparoscopy in VP shunt placement and management of its distal complications in infants and children. The study limitations include the retrospective design and the lack of randomized control group.
Conclusion
Based on our results, laparoscopic-assisted VP shunt placement and revisions in children is feasible and safe. Interdisciplinary team including a neurosurgeon for the cranial part and a pediatric surgeon for the laparoscopic part of the procedure are needed.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- CSF:
-
Cerebrospinal fluid
- VPS:
-
Ventriculoperitoneal shunt
References
Khaitan L, Brennan EJ Jr (1999) A laparoscopic approach to ventriculoperitoneal shunt placement in adults. Surg Endosc 13(10):1007–1009
Kirshtein B, Benifla M, Roy-Shapira A, Merkin V, Melamed I, Cohen Z et al (2004) Laparoscopically guided distal ventriculoperitoneal shunt placement. Surg Laparosc Endosc Percutan Tech 14(5):276–278
Yu S, Bensard DD, Partrick DA, Petty JK, Karrer FM, Hendrickson RJ (2006) Laparoscopic guidance or revision of ventriculoperitoneal shunts in children. JSLS 10(1):122–125
Schubert F, Fijen BP, Krauss JK (2005) Laparoscopically assisted peritoneal shunt insertion in hydrocephalus: a prospective controlled study. Surg Endosc 19(12):1588–1591
Drake JM, Kestle JR, Milner R, Cinalli G, Boop F, Piatt J Jr et al (1998) Randomized trial of cerebrospinal fluid shunt valve design in pediatric hydrocephalus. Neurosurgery. 43(2):294–303 discussion -5
Martin K, Baird R, Farmer JP, Emil S, Laberge JM, Shaw K et al (2011) The use of laparoscopy in ventriculoperitoneal shunt revisions. J Pediatr Surg 46(11):2146–2150
Fanelli RD, Mellinger DN, Crowell RM, Gersin KS (2000) Laparoscopic ventriculoperitoneal shunt placement: a single-trocar technique. Surg Endosc 14(7):641–643
Acharya R, Ramachandran CS, Singh S (2001) Laparoscopic management of abdominal complications in ventriculoperitoneal shunt surgery. J Laparoendosc Adv Surg Tech A 11(3):167–170
Nfonsam V, Chand B, Rosenblatt S, Turner R, Luciano M (2008) Laparoscopic management of distal ventriculoperitoneal shunt complications. Surg Endosc 22(8):1866–1870
Esposito C, Porreca A, Gangemi M, Garipoli V, De Pasquale M (1998) The use of laparoscopy in the diagnosis and treatment of abdominal complications of ventriculo-peritoneal shunts in children. Pediatr Surg Int 13(5–6):352–354
Wang G, Yu J, Luan Y, Han Y, Fu S (2017) Novel type of peritoneocentesis trocar-assisted distal ventriculoperitoneal shunt placement with supervision via a one-port laparoscope. Exp Ther Med 14(4):3413–3418
Brunori A, Massari A, Macarone-Palmieri R, Benini B, Chiappetta F (1998) Minimally invasive treatment of giant CSF pseudocyst complicating ventriculoperitoneal shunt. Minim Invasive Neurosurg 41(1):38–39
Svoboda SM, Park H, Naff N, Dorai Z, Williams MA, Youssef Y (2015) Preventing distal catheter obstruction in laparoscopic ventriculoperitoneal shunt placement in adults: the "falciform technique". J Laparoendosc Adv Surg Tech A 25(8):642–645
Argo JL, Yellumahanthi DK, Ballem N, Harrigan MR, Fisher WS 3rd, Wesley MM et al (2009) Laparoscopic versus open approach for implantation of the peritoneal catheter during ventriculoperitoneal shunt placement. Surg Endosc 23(7):1449–1455
Sekula RF Jr, Marchan EM, Oh MY, Kim DK, Frederickson AM, Pelz G et al (2009) Laparoscopically assisted peritoneal shunt insertion for hydrocephalus. Br J Neurosurg 23(4):439–442
Johnson BW, Pimpalwar A (2009) Laparoscopic-assisted placement of ventriculo-peritoneal shunt tips in children with multiple previous open abdominal ventriculo-peritoneal shunt surgeries. Eur J Pediatr Surg 19(2):79–82
Handler MH, Callahan B (2008) Laparoscopic placement of distal ventriculoperitoneal shunt catheters. J Neurosurg Pediatr 2(4):282–285
Soleman J, Schneider CA, Pfeifle VA, Zimmermann P, Guzman R (2017) Laparoscopic-assisted ventriculoperitoneal shunt placement in children younger than the age of 1 year. World Neurosurg 99:656–661
Aldrich EF, Harmann P (1990) Disconnection as a cause of ventriculoperitoneal shunt malfunction in multicomponent shunt systems. Pediatr Neurosurg. 16(6):309–311 discussion 12
Kaplan M, Ozel SK, Donmez O, Kazez A (2007) Treatment approaches for abdominal migration of peritoneal catheter of ventriculoperitoneal shunt. Turk Neurosurg 17(2):158–162
Harsh GR (1954) 3rd Peritoneal shunt for hydrocephalus, utilizing the fimbria of the fallopian tube for entrance to the peritoneal cavity. J Neurosurg 11(3):284–294
Birbilis T, Kontogianidis K, Matis G, Theodoropoulou E, Efremidou E, Argyropoulou P (2008) Intraperitoneal cerebrospinal fluid pseudocyst. A rare complication of ventriculoperitoneal shunt. Chirurgia (Bucur). 103(3):351–353
Yount RA, Glazier MC, Mealey J Jr, Kalsbeck JE (1984) Cerebrospinal fluid ascites complicating ventriculoperitoneal shunting. Rep Four Cases J Neurosurg 61(1):180–183
Tamber MS, Klimo P Jr, Mazzola CA, Flannery AM (2014) Pediatric hydrocephalus: systematic literature review and evidence-based guidelines Part 8: management of cerebrospinal fluid shunt infection. J Neurosurg Pediatr. 14(Suppl 1):60–71
Bani A, Telker D, Hassler W, Grundlach M (2006) Minimally invasive implantation of the peritoneal catheter in ventriculoperitoneal shunt placement for hydrocephalus: analysis of data in 151 consecutive adult patients. J Neurosurg 105(6):869–872
Fahy AS, Tung S, Lamberti-Pasculli M, Drake J, Kulkarni AV, Gerstle JT (2019) Laparoscopic insertion of ventriculoperitoneal shunts in pediatric patients—a retrospective cohort study. J Pediatr Surg 54(7):1462–1466
Acknowledgements
Not applicable.
Funding
This study had no funding from any resource.
Author information
Authors and Affiliations
Contributions
HAA gave the idea and collected the patients’ data and analyzed them. MAS wrote the paper with revision and the corresponding author. MAM put study design and followed the patients postoperatively. All authors have read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
All authors have no conflicts of interest or financial ties to disclose. Content have not published elsewhere, and the paper not being submitted elsewhere.
Ethics approval and consent to participate
This study was approved by the Review Board of the Department of General Surgery, Faculty of Medicine, Tanta University, Egypt.
Consent for publication
Not applicable.
Rights and permissions
About this article
Cite this article
Almetaher, H.A., Shadad, M.N., Hassan, H.S. et al. Laparoscopic insertion and revision of ventriculo-peritoneal shunts in children. J Ped Endosc Surg 2, 195–200 (2020). https://doi.org/10.1007/s42804-020-00071-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s42804-020-00071-9