Abstract
It has been more than 80 years since the discovery of vitamin D and its ability to cure rickets in children. Vitamin D is a secosteroid and comes in two distinct forms, vitamin D2 and vitamin D3. During the last 40 years, the synthesis and metabolism of vitamin D were elucidated and more than 50 metabolites of vitamin D have been discovered, though commercial measurement procedures have been developed for only a few of them. The clinical significance of vitamin D in calcium and phosphorus homeostasis is well appreciated. However, recent epidemiological data have indicated that it has several extra-skeletal physiologic actions which are still a matter of scientific debate. Both research findings and the debate around the interpretation of the research results have created increased interest in more measurements of vitamin D. With the ever growing family of measurable vitamin D metabolites and the measuring techniques comes a question: What metabolic product will provide the right answers and which is the best way to measure it. The right choice of analytical technique is connected with the question of which metabolite we aim to measure, what is its serum concentration, and the purpose of the measurement. The aim of the first part of this review is to provide a brief overview of vitamin D metabolism and a more detailed analysis of the existing methods and the status of standardization for the measurement of 25-hydroxyvitamin D.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Vitamin D metabolism
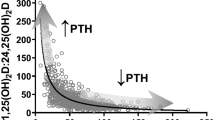
Vitamin D and parathyroid hormone (PTH) are the major regulators of calcium homeostasis and play an important role in bone metabolism [1]. Vitamin D is a fat-soluble steroid hormone and exists in two major forms, vitamin D2 (or ergocalciferol) and vitamin D3 (or cholecalciferol). Both are formed by UV irradiation of either ergosterol, which is found naturally in plants, phytoplankton, and fungi and is also commercially produced by UV irradiation of milk and yeast (mushrooms), or 7-dehydrocholesterol (7-DHC or provitamin D3), which is found in all vertebrates with the exception of fish (Figs. 1 and 2) [2].
When the skin is exposed to UV radiation in the wavelength range 290–315 nm, 7-dehydrocholesterol absorbs this energy, which causes chemical bonds within its molecule to break and re-arrange, resulting in the formation of pre-vitamin D. In the skin, pre-vitamin D undergoes rapid, thermally induced isomerization and vitamin D is produced. Once formed, pre-vitamin D and vitamin D continue to absorb UV. Prolonged exposure to UV radiation results in breakdown of these molecules into biologically inactive photoproducts. For this reason, during prolonged irradiation, a steady state is reached when only 10–15% of 7-dehydrocholesterol is cutaneously converted to pre-vitamin D3. This ensures that no toxic levels of vitamin D are synthesized under excessive sun exposure conditions (the chemical formulas are taken from pubchem https://pubchem.ncbi.nlm.nih.gov)
Production of vitamin D from ergosterol. Ergosterol differs from 7-dehydrocholesterol in its side chain, which contains an extra methyl group at carbon 4 at position C-24. Ultraviolet (UV) radiation in the wavelength range 290–315 nm cleaves the B ring of both ergosterol and 7-dehydrocholesterol, yielding ergocalciferol and cholecalciferol, respectively. Irradiation of milk and yeast is a commercial means of producing D2 from ergosterol, and dihydrotachysterol (DHT) is a synthetic analog of vitamin D2 (the chemical formulas are taken from pubchem https://pubchem.ncbi.nlm.nih.gov)
In humans, vitamin D (D here represents D2, D3, or both) is either produced endogenously in the skin from sun exposure or obtained from foods that naturally contain vitamin D and supplements. Foods rich in vitamin D include cod liver oil, fatty fish, UV-irradiated mushrooms, and foods fortified with vitamin D. Moreover, during exposure to sunlight, 7-DHC in the skin is converted to previtamin D3 (Fig. 1).
These two forms of vitamin D differ in chemical structure and in pharmacokinetic properties. Chemically, they differ in one methyl group at carbon C24 position and a double bond between the carbons at positions C22-23 on their side chain (Fig. 3). As a consequence, they also have different molecular weights (396.65 g/mol and 384.64 g/mol, respectively).
The two forms of vitamin D: ergocalciferol (left) and cholecalciferol (right) (the chemical formulas are taken from pubchem https://pubchem.ncbi.nlm.nih.gov)
Vitamin D synthesized in the skin diffuses into the blood, where it is transported by vitamin D binding protein (VDPB) to the liver. Vitamin D from the diet is absorbed in the small intestine and incorporated into chylomicrons, which are released into the lymphatic system, and enters the venous blood where it binds to VDBP and lipoproteins and is transported to the liver [3]. The hepatic ingress of vitamin D is modulated by its plasma carriers and liver membrane receptors [4].
Vitamin D has no biological activity and its activation involves two hydroxylation steps (Fig. 4). With the first step that takes place in the liver, vitamin D is hydroxylated at the C25 position by the cytochrome p450 enzyme CYP2R1 (also called 25-hydroxylase, located in the endoplasmic reticulum) to yield 25-hydroxyvitamin D [25(OH)D] (Fig. 5). This enzyme hydroxylates both vitamin D2 and D3 and seems to be the main enzyme involved in vitamin D 25-hydroxylation [5]. Experimental evidence has shown that additional enzymes (mitochondrial CYP27A1 as well as microsomal CYP2D11, CYP2D25, CYP2J2/3, and CYP3A4) also contribute to 25(OH)D production by exerting 25-hydroxylase activity [6, 7]. The activity of 25-hydroxylase is poorly regulated by any feedback mechanism in the context of the vitamin D endocrine system and it seems to be dependent primarily on the concentration of vitamin D [8]. Severe liver failure affects the function of the enzyme CYP2R1. Moreover, loss-of-function mutations of the same enzyme are responsible for vitamin D-dependent rickets [VDDR], type 1B [VDDR-1B] [9].
The two steps of activation of vitamin D (the chemical formulas are taken from pubchem https://pubchem.ncbi.nlm.nih.gov)
After hydroxylation, 25(OH)D is transported by VDBP to the kidney, where it is filtered by the glomerulus and reabsorbed by the proximal tubular cells. Entry of 25(OH)D into the proximal tubular cells requires receptor-mediated uptake of the VDBP-25(OH)D complex at the brush border, degradation of VDBP, and endocytic internalization and translocation of 25(OH)D to mitochondria [10]. This is achieved via the megalin/cubulin complex [11]. Both megalin and cubulin are large, multiligand, endocytic-membrane glycoproteins expressed in epithelial cells of several tissues and involved in the endocytic uptake of many ligands, including lipoproteins, vitamin-binding proteins, other carrier proteins, hormones, enzymes, and drugs in several epithelia. The receptors might work independently, but have also been observed to interact to facilitate the uptake of several ligands [11]. It is in the mitochondria of the proximal renal tubule that 25(OH)D is hydroxylated at the carbon to position C1, resulting in the formation of the secosteroid hormone calcitriol or 1α,25-dihydroxy-vitamin D [1,25(OH)2D], the hormonally active form of vitamin D which is responsible for most, if not all, of the biologic actions of vitamin D. Again, a cytochrome p450 enzyme, renal CYP27B1 (also called 25(OH)D-1a-hydroxylase), is responsible for this hydroxylation. This enzyme is predominately present in the kidney (proximal straight tubules) and contributes to the majority of the circulating levels of 1,25(OH)2D. Inactivating mutations of these enzymes are responsible for vitamin D-dependent rickets (VDDR) type 1A [VDDR-1A] [6,7,8, 12].
Vitamin D catabolism
Catabolism is an essential component of vitamin D metabolism (Fig. 6). Both 25(OH)D and 1α,25(OH)2D undergo catabolism via multiple side chain hydroxylations to become more polar metabolites, which are subsequently excreted in both urine and feces. The enzyme CYP24A1, a mitochondrial P450 enzyme encoded by the CYP24A1 gene, catalyzes the first step, along with several subsequent steps of the vitamin D catabolic pathway in humans and is capable of catalyzing all of the hydroxylation steps in the catabolism of both 25(OH)D and 1α,25(OH)2D [7]. The 24-hydroxylase pathway generates 24R,25(OH)2D from the hydroxylation of 25(OH)D and 1,24,25(OH)3D from the hydroxylation of 1,25(OH)2D. These metabolites are further oxidized to generate a variety of excretory products [6, 13, 14]. These 24-hydroxylation reactions represent the first steps in the vitamin’s inactivation process, that leads to the biologically inactive product calcitriolic acid (Fig. 6) [13]. On the other hand, the 23-hydroxylase pathway ends up creating the biologically active 1a,25-26,23 lactone. Calcitriol and FGF23 can cause up-regulation of expression of 24-hydroxylase, while PTH and low calcium down-regulate its expression. The expression of the enzyme CYP24A1 (or 24-hydroxylase) in the kidney provides another means of control in vitamin D homeostasis.
Catabolism of vitamin D (the chemical formulas are taken from pubchem https://pubchem.ncbi.nlm.nih.gov)
CYP24A1 has been found in many tissues that express the vitamin D receptor. In the kidney, it is found in the proximal and distal tubules [14, 15]. The CYP24A1 gene is highly inducible by 1α,25(OH)2D in all tissues in which it is found and it acts as a control mechanism to prevent intoxication from 1α,25(OH)2D [16]. The importance of this feedback mechanism was demonstrated when inactivating mutations of CYP24A1 were reported in children and adults with hypercalcemia [9, 17]. Another enzyme, CYP3A4, also plays a role in vitamin D catabolism. This is a microsomal cytochrome P450 enzyme which is found in numerous tissues and catabolizes both 25(OH)D and 1,24R,25(OH)3D in a manner similar to CYP24A1. The quantitative contribution of CYP3A4 to vitamin D catabolism compared to CYP24A1 is not well known [18]. Recently, a gain-of-function mutation in CYP3A4 was described, which leads to vitamin D deficiency through accelerated vitamin D metabolite inactivation (named type 3 vitamin D-dependent rickets or VDDR3) [19].
Other vitamin D metabolites
In addition to the primary pathway of vitamin D metabolism, there are also a number of minor metabolic pathways. It has recently been discovered that vitamin D can alternatively be metabolized through the C3-epimerization pathway that parallels the standard metabolic pathway [20]. This pathway creates the vitamin D epimers, a group of metabolites that has attracted much attention recently. Epimers are molecules with identical structure but different stereochemical configuration. The C3-epimers of vitamin D differ from the primary molecules only in the configuration of the hydroxyl group at the 3 carbon position. Of them, the C3-epimer of the 25(OH)D [C3-epi-25(OH)D] is the most abundant epimer that has been found in the systemic circulation (Fig. 7) [21]. The C3-epi-25(OH)D can also undergo 1α hydroxylation to give C3-epi-1α,25(OH)2D and 24 hydroxylation to give C3-epi-24,25(OH)2D and 1α,24,25(ΟΗ)3D (Fig. 7) [22].
Epimerization pathways of vitamin D metabolites (the chemical formulas are taken from pubchem https://pubchem.ncbi.nlm.nih.gov)
The physiological importance of the vitamin D3 epimer is not as yet very well known. The C3-epi-25(OH)D was initially found in neonates, in a 2006 publication by Singh et al., where it was reported that the C3-epimer was detectable in a significantly high percentage (up to 60%) of neonates and children up to 1 year of age [23]. Recently, it has been reported in adults [20, 24]. Detectable levels of the epimer range from 0 to 100% of the adults tested and it is estimated that, on average, adults have a median concentration (range) epimer of 1.72 (0–9.01) ng/ml and that the epimer makes up to 6.1% (0–47.0%) of the total 25(OH)D [the sum of epimer + 25(OH)D] [21].
Measurement of vitamin D metabolites
Which metabolites can be measured
At present, more than 50 vitamin D metabolites have been described and characterized, with some of them exhibiting biological activity [25]. However, methods for adequate measurement been developed for only five of them (vitamin D, 25(OH)D2 and 25(OH)D3, 1α,25(OH)2D, 24R,25(OH)2D, and C3-epi-25(OH)D) (Table 1), these being metabolites encountered in serum in concentrations that allow for their measurement with these methods [26].
The above metabolites differ significantly in their biological activity. For example, 1α,25(OH)2D is five times more potent than vitamin D in its ability to absorb calcium from the intestines and to mobilize it in the bones [27]. A significant factor that determines the biological activity of a metabolite is its affinity to VDR. Experimental studies have shown that 1,25(OH)2D exhibits the highest affinity to VDR among all vitamin D metabolites [28], while the affinity of the rest of the metabolites is significantly lower. For instance, 25OHD and 24,25(OH)2D exhibit approximately 900 and 5000 times lower affinity to VDR, respectively, compared to that of 1,25(OH)2D [29]..
Pre-analytical considerations
Sample types and collection tubes
Both serum and plasma (EDTA) can be used for the measurement of vitamin D metabolites. However, serum is the preferred matrix, since it has the advantage of being free of anticoagulants used for plasma collection, such as EDTA, heparin, or citrate, which may interfere with their measurement. However, even when serum is the medium, significant interferences are observed with certain commercial assays when Serum Clot Activator Tubes with Gel are used [30]. Saliva has also been explored in several studies and with assays based on different principles, however, often with inconsistent results. More recently, the technological advances achieved in LC-MS/MS sensitivity and novel extraction approaches have made feasible the measurement of 25(OH)D, requiring reduced sample volume and using dried blood spots (DBSs) for sample collection [31].
Sample stability
Vitamin D metabolites are stable in plasma and serum when samples are stored at room temperature (24 °C), or at 4 °C, or frozen, as long as the metabolites are not separated from their binding protein. Therefore, no special precautions are necessary during the transport of samples to the laboratory. In stored samples, repeated cycles of freeze-thaw do not seem to have any significant effect on 25(OH)D levels. Attention is needed only when the samples have already been pretreated and vitamin D has been separated from its binding protein. Then, samples should be kept in dark vials to avoid exposure to light and stored at <− 70 °C [32].
Effect of season of the year on 25(OH)D levels
Due to its biosynthesis, levels of vitamin D are directly dependent upon exposure to UV irradiation from the sun. This results in a seasonal variation and in the fact that 25(OH)D levels depend on the geographical location in which a person lives (distance from equator and altitude) [33]. Generally speaking, people living in the northern hemisphere present the highest levels of 25(OH)D during the summer and autumn and the lowest during winter and spring [34].
Single-nucleotide polymorphisms
Genetic studies have revealed that single-nucleotide polymorphisms (SNPs) of genes that are involved in vitamin D metabolism pathways (i.e., DHCR7, CYP2R1, CY-P3A4, CYP27A1, DBP, LRP2, CUB, CYP27B1, CYP24A1, VDR, and RXRA) have an effect on vitamin D levels. However, the effect exerted by these SNPs on the levels of circulating 25(OH)D can explain only 5% of its variability and can be considered small compared to other environmental factors that have a more significant effect on its levels [7, 35]. Therefore, their presence does not seem to have significant clinical value in everyday practice, also taking into account the fact that most laboratory assays present an analytical variability of approximately 10%.
Age, sex, body mass index, and lifestyle
Age, sex, and body fat seem to have a small effect on the seasonal variation of 25(OH)D levels, although recent studies have shown that the effect of age is small [36]. On the other hand, the lack of association of 25(OH)D levels with age can be explained in these studies, since most of the participants were < 75 years old. It is known that in older adults, (1) calcium absorption is reduced; (2) there is intestinal resistance of calcium absorption to circulating 1,25(OH)2D; (3) the ability of the skin to produce vitamin D is decreased; (4) VDR expression is reduced; (5) the kidneys are not able to produce 1α,25(OH)2D compared to younger kidneys; and finally, (6) there is substrate deficiency of vitamin D [37]. Lastly, older people are more housebound and therefore less exposed to sunshine and to outdoor activities compared to younger people [38].
Body mass index (BMI) is usually increased with age, and there are several mechanisms which can explain its inverse association with low vitamin D levels, namely, physical inactivity, inappropriate diet, and incorporation of vitamin D in body fat, which makes it unavailable in the systemic circulation. Vitamin D deficiency is prevalent among people with obesity, suggesting that adipose tissue might play a role in the low vitamin D levels [39]. However, a causal relationship between obesity and low 25(OH)D levels has not to date been completely elucidated. Different mechanisms have been proposed to explain this inverse association, including such behavioral factors as reduced exposure to sunlight due to less outdoor physical activity and low dietary intake of vitamin D-enriched food. Moreover, decreased intestinal absorption, impaired hydroxylation in adipose tissue, and 25(OH)D accumulation in fat have been proposed to explain hypovitaminosis in obesity. The fact that vitamin D is a fat-soluble molecule may lead to the hypothesis that vitamin D is sequestered in body fat depots, resulting in lower bioavailability in the obese state [40]. On the other hand, some studies have speculated that vitamin D deficiency itself could cause obesity or even prevent weight loss [40].
Several studies have demonstrated that men have higher levels of 25(OH)D, this finding being independent of age, season, and race. Finally, outdoor activities, exposure to sunlight (not only the duration of exposure but also the time of the day), dressing habits, and, most importantly, the coverage of the body (and even the type of clothes) and the use or not of sun protection all significantly affect 25(OH)D levels.
Ethnicity
Although most of the studies were conducted with subjects of European descent, there are studies that have shown that levels of 25(OH)D differ according to ethnicity and skin color. This seems logical, since darker skin color protects from exposure to UV irradiation, thereby increasing the risk of vitamin D deficiency [41]. Vitamin D synthesis is highly dependent on melanin concentration in the skin, as melanin absorbs ultraviolet radiation (UVR), resulting in less efficient conversion of 7-dehydrocholesterol to provitamin D3 [42]. Therefore, dark-skinned individuals will experience slower vitamin D synthesis than light-skinned persons. This is more obvious and important at higher latitudes where the intensity and duration of sunlight are less. Metabolic differences due to race/ethnicity may provide an additional explanation.
Effect of liver and kidney disease
The liver and kidneys are the two most important organs that participate in the metabolism of vitamin D.
The liver is the organ where 25-hydroxylation of vitamin D primarily takes place and the majority of VDBP is synthesized. In patients with liver disease, the prevalence of insufficiency and deficiency is much higher than in the general population, ranging between 64 and 92%, while serum 25(OH)D is inversely related to the severity of liver disease [43]. The high prevalence of vitamin D deficiency in this populations occurs regardless of the etiology of liver disease. Low vitamin D levels in chronic liver disease (CLD) may be the result of a variety of causes and mechanisms, including limited sun exposure and dietary intake, intestinal fat malabsorption due to cholestasis, and decreased hepatic hydroxylation [44]. Decreased production of VDBP and albumin might also be critical in CLD. In addition, hepatic hydroxylation is impaired, leading to low production of 25(OH)D. Hence, there will be less 25(OH)D available for production of the active hormone, whereas catabolism is increased. As VDBP has a single sterol-binding site and only 5% of total circulating DBP actually carries a vitamin D metabolite at any time, liver function would have to be severely impaired for low VDBP to have a significant role in 25(OH)D deficiency in CLD [45].
Total 25(OH)D levels decrease as severity of CLD increases, and there is a lack of correlation between total 25(OH)D levels and PTH and calcium. However, although patients with end-stage liver disease exhibit a high prevalence of low total 25(OH)D, they maintain normal serum corrected calcium levels and do not develop secondary hyperparathyroidism [46]. These observations have led to the hypothesis that total 25(OH)D levels may not be the most accurate biomarker to estimate vitamin D adequacy in patients with advanced CLD and that free 25(OH)D may be a more accurate marker, especially in patients with diminished liver synthetic ability [47].
The kidneys are essential not only for the conversion of 25(OH)D to 1α,25(OH)2D but also for the reabsorption of 25(OH)D from renal ultrafiltrate for its recycling to the circulation to maintain serum 25(OH)D levels. Normal renal function is also essential to maintain the endocrine actions of calcitriol, while normal calcitriol, in turn, contributes to maintaining VDR in target tissues, since, through binding to VDR, it protects the receptor from degradation [48].
In chronic kidney disease (CKD), progressive loss of capacity to produce 1α,25(OH)2D is observed. The mechanisms involved in the decrease of calcitriol production during the course of CKD are reviewed in references [14, 49]. Impaired uptake of 25(OH)D by the kidneys seems to be the main cause of 1α,25(OH)2D deficiency, although CYP abundance and activity are also responsible [14, 50].
Decreased kidney function and calcitriol deficiency lead to hypocalcemia and are the key contributors to secondary hyperparathyroidism [14, 50]. This is more obvious among patients with end-stage renal disease, where 1α,25(OH)2D is almost undetectable. Therefore, calcitriol replacement with the appropriate analog seems to be the therapy of choice to prevent or slow down the progression of SHPT and its adverse effects [51]. CKD is also characterized by low serum 25(OH)D levels. The main causes and risk factors for vitamin D deficiency among CKD patients are also reviewed in [50]. These levels also decrease progressively as renal function deteriorates; however, not all studies show that 25(OH)D insufficiency or deficiency are greater in these patients than in the general population [52]. Maintenance of sufficient levels of 25(OH)D could be a possible objective, since the kidney is not the only site of calcitriol production, and in CKD patients, vitamin D deficiency is also a strong predictor of accelerated renal disease and death [53]. However, the debate over what is the best treatment approach and what is the best biomarker to follow for CKD patients is still ongoing [54, 55].
Kidney disease also disrupts vitamin D catabolism. In the kidneys, 1a-hydroxylase and 24-hydroxylase are under the competing hormonal regulation of FGF23 and PTH. However, the net effect of these two hormones on vitamin D catabolism in CKD is disputed. CKD is also characterized by high levels of FGF23 and increased serum phosphorus levels. Studies have shown that FGF23 is responsible for the reduced expression of 1a-hydroxylase in renal tubular cells and induces the expression of 24-hydroxylase, which is responsible for the catabolism of vitamin D. This may result in reduced production of 1α,25(OH)2D. On the other hand, 24R,25(OH)2D also seems to be lower in patients with CKD compared to healthy subjects [56]. Notably, moreover, ΡΤΗ appears to increase the expression of CYP27B1 mRNA in renal tubular cells [14]. The increased phosphate levels have been correlated with low concentrations of 1α,25(OH)2D, but it is not clear whether this correlation is direct or is induced by FGF23 or is a confounder along with other factors [14]. Furthermore, metabolic disturbances that are observed in patients with CKD, such as diabetes, metabolic acidosis, and uremia, it is possible to reduce the expression of CYP27B1 [57, 58].
Pregnancy
Special attention must be given to pregnancy, since several studies report low levels of 25(OH)D in pregnant women. A recent meta-analysis reported that 54% of pregnant women have levels of vitamin D below 50 nmol/L [59]. Moreover, several studies have suggested that low levels of 25(OH)D during pregnancy are associated with increased risk of pre-eclampsia and gestational diabetes, as well as other complications of pregnancy [60]. However, the results from these studies associating low levels of 25(OH)D during pregnancy with adverse outcomes are conflicting. This has not only to do with possible methodological problems related to the design of the studies but also with the method of 25(OH)D quantitation. In pregnancy, VDBP is known to be increased; thus, when the measurement of 25(OH)D is performed with an immunoassay, the levels may well be underestimated due to incomplete dissociation of 25(OH)D from its binding protein. This causes significant assay variation, so that results from meta-analyses may be subject to error, especially when results are included from studies where measurements were based on immunoassays.
By contrast, when a HPLC or a LC-MS/MS method is used, dissociation of 25(OH)D from its binding protein is enhanced due to the use of strong chemical solvents in the pretreatment step of the samples [61].
Assays for the measurement of 25-hydroxyvitamin D
The measurement of 25(OH)D is performed for two major reasons: (1) to determine the nutritional status of vitamin D and (2) to monitor its therapeutic level. There are two different forms of vitamin D, as mentioned above, and, in order to adequately monitor therapy, both types of vitamin D need to be equally accurately quantitated. In fact, accurate measurement of 25(OH)D for the assessment of vitamin D status has always been a major goal of all clinical laboratories involved in measuring vitamin D metabolites.
25(OH)D is the metabolite of choice for several reasons:
-
Its levels in the blood are higher than those of any other vitamin D metabolite: its serum concentration is in the range of 25–200 nmol/L, which is 1000 times higher than that of 1α,25(ΟΗ)2D, whose concentration is in the range of 50 to 150 pmol/L. Furthermore, most of it is found in the systemic circulation, with limited distribution in less accessible tissues (e.g., fat) [62].
-
Several clinical studies have demonstrated that there is an association between serum levels of 25(OH)D and several clinical outcomes, such as bone mineralization, fracture risk, fall risk, cancer, diabetes, and cardiovascular events.
-
It has a relatively long half-life (2–3 weeks), as compared with 1α,25(ΟΗ)2D (approximately 4–6 h), and, therefore, serum levels vary little within short periods of time [16, 63].
-
The hydroxylase enzymes that metabolize vitamin D to 25(OH)D in vivo behave according to first-order reaction kinetics. This means that its rate of production is dependent on vitamin D levels and, therefore, its level in the systemic circulation is the best indicator of vitamin D nutritional status [64].
-
Furthermore, 25(OH)D represents the sum of vitamin D intake and dermal production [65].
-
Serum levels are relatively stable and not affected by diet (i.e., calcium intake) and lifestyle (i.e., sedative life or regular physical exercise), whereas 1α,25(ΟΗ)2D levels are affected by all the latter [62, 63].
-
Serum levels can determine if there is enough 25(OH)D for the extrarenal tissues to produce 1a,25(OH)2D that has autocrine or paracrine action, since recent data have revealed that many of these tissues also contain the enzyme CYP27B1, responsible for converting 25(OH)D to 1,25(OH)2D. Regulation of CYP27B1 in these non-renal tissues is generally different from that in the kidney and may be more substrate-dependent. This has led to the concept that maintenance of adequate 25OHD levels in the blood is required for vitamin D regulation of a large number of physiologic functions beyond those of the classic actions involved in bone mineral metabolism. Measurement of 1α,25(ΟΗ)2D does not provide this information, since its extrarenal production does not contribute much to the systemic load [29, 66].
The assays that have been developed for the measurement of 25(OH)D can be classified into three types: (1) competitive protein binding assays (CPBA), (2) immunoassays, and (3) chemical assays.
CPBA
This was the first method developed for 25(OH)D measurements and was published in 1971 [67]. In its first edition, this method used VDBP as the primary binding agent and 3H-25(OH)D as tracer. Radiolabeled 3H-25(OH)D “competed” with 25(OH)D in the sample for the available VDBP. Therefore, the concentration of 25(OH)D was estimated by the reduction of radioactivity in 3H-25(OH)D. However, since several vitamin D metabolites, such as 24R,25(OH)2D and even some rare ones like 25,26(OH)2D, have high affinity and bind to VDBP, this method has suffered from interferences. Moreover, it necessitated laborious preparation of the sample prior to analysis with organic solvents, with a chromatographic method, in order to release 25(OH)D in the sample from its binding proteins, which process required silicon columns. This method was supposed to detect with equal sensitivity and specificity both forms of 25(OH)D. Its analytical sensitivity was 10 nmol/L, later modification improving the sensitivity down to 5 nmol/L. Nevertheless, it remained a very laborious method and difficult to apply when large volumes of samples were needed for analysis. The method was largely abandoned by 2001, while an automated method based on this principle was available, but is now out of production. The only method that is still available today based on this principle is a manual ELISA [63].
Immunoassays
These fall into three categories: (1) radioimmunoassays (RIA), (2) enzyme-linked immunosorbent assays (ELISA), and (3) chemiluminescent assays (CLIA). The development of polyclonal antibodies against 25(OH)D enabled the development of the first RIA in the early 1980s [68]. These were also competitive assays, and 25(OH)D in the sample competed with a radiolabeled 25(OH)D [125I-25(OH)D]. Sample preparation was simplified by the use of acetonitrile to separate 25(OH)D from its binding protein. This method too was not free of interferences. The polyclonal antibody also reacted with 24R,25(OH)2D, 25,26(OH)2D, and 25(OH)D-26,23-lactone. Other disadvantages were the short life of reagents, difficulties and risks due to the use of radiolabeled reagents, and the manual character of the method, which excluded automated use. ELISAs were first introduced in the mid-1990s. They are also competitive in their design; however, the radiolabeled tracer was replaced by an enzyme (horse radish peroxidase). These too were manual methods and are still in production. Starting from the early 2000s, the first automated methods were developed and are now the mainstream methods for the quantitation of 25(OH)D. They are again based on the competitive principle, only the tracer is different: it is a chemiluminescent label. These CLIA assays claim better sensitivity and reproducibility, and, of course, automation allowed clinical labs to measure in a small period of time large volumes of samples. Analyzers were easy to handle and they did not require specially trained personnel. Major disadvantages included interferences from other metabolites and the huge variabilities observed between different assays from different manufacturers. This resulted in a lack of comparability, not only of measurements between clinical labs that used assays from different manufactures, but also between research studies [29, 69]. Moreover, immunoassays are affected by various other interferences [70, 71]. Nonetheless, all immunoassays continued to be designed as competitive methods. The reason is that the small size of 25(OH)D impedes the simultaneous binding of two antibodies, and, therefore, the development of non-competitive sandwich immunoassays, which are characterized by superior analytical sensitivity and specificity [72]. Recently, Omi et al. described the development of an automated non-competitive method designed for the quantitation of 25(OH)D based on antimetatype monoclonal antibodies [73]. This non-conventional immunoassay has recently been validated and is commercially available [74].
High-performance liquid chromatography
The use of HPLC for the separation and quantitation of vitamin D metabolites dates back to the early 1970s [75]. HPLC uses the difference of affinity of the molecules towards the solid phase (a resin contained in the column), or towards the liquid phase (a mixture of organic solvents and/or water based solutions known as the eluent). Both the polarity and the size and conformation of the molecule play an important role in the process. The use of columns is of major importance, and their production has evolved over the years to provide better separation between different metabolites. Detection is done primarily using UV detection at 265 nm, although electrochemical detection has been employed in several applications [29, 64, 69]. Though the above method can separate D2 from D3, the procedure, while being accurate for the measurement of 25(OH)D, its performance is wholly inadequate for the measurement of other metabolites that circulate at concentrations well below those of the 25(OH)D sample volume [64]. It has been used mainly as a research method since it requires a time-consuming manual sample preparation and an extraction phase before the sample is introduced to HPLC. The non-automation of this method is the main reason that it has not gained general acceptance by clinical labs. Each lab has to develop its own in-house application and the performance depends greatly on the selection of the instruments, the column used, and the experience of the users. The selection of an appropriate column is essential in order to be able to separate and quantitate different metabolites adequately. Nevertheless, the separation of vitamin D epimers is not done successfully, this being one of the negative sides of this method.
Liquid chromatography coupled with mass spectrometry
While HPLC used UV for the detection of various metabolites, LC-MS/MS uses a mass spectrometer for this task and relies on this to quantify different metabolites. LC-MS/MS relies on MS to differentiate between different molecular entities of vitamin D. As mentioned, in stand-alone HPLC methods, detection is achieved through a UV detector. Although UV detection is a powerful detection method for vitamin D metabolites due to their strong absorption at 264 nm, most metabolites exhibit similar UV patterns and need to be fully separated in the LC step in order to be detected and quantified separately. Therefore, metabolites that cannot be fully resolved by the LC part of the method cannot be independently quantified and will instead be reported as a sum. This is where MS presents a big advantage. In this technique, molecules are detected by their mass-to-charge ratio (m/z), and most vitamin D metabolites have different masses. Therefore, they can be separated, detected, and quantified even if the LC part of the method does not fully separate them. However, a problem arises when some metabolites, called isobars, are present in the sample. These are molecules with the same molecular weight that form product ion pairs with the same m/z ratio. This is a problem that appears particularly with LC/MS/MS methods that typically use short chromatographic run times. For those metabolites, several techniques have been devised, and more advanced MS systems have been developed to overcome these obstacles.
Currently, LC-MS/MS methods present analytical sensitivity < 10 nmol/L well below the 25 nmol/L that signifies the severe deficiency of vitamin D. These methods are also very versatile, since they can measure multiple metabolites in a single sample in a single run (lately, methods have been developed that can quantify up to six different metabolites in a single sample), and they exhibit fewer matrix effects than immunoassays. Currently, the problems with separation of epimers seem to have been solved, as well as problems that can be created from the isobaric compounds with comparable m/z ratios. Finally, there has been significant progress in the automation of sample preparation [76].
To conclude, some drawbacks must be mentioned that are involved in both HPLC and LC-MS/MS methods that are mainly technical in nature. They require high quality water and chemical solvents; they are mostly in-house applications and this may present a problem with regulatory authorities, thus demanding very detailed validation prior to use for measurement of clinical samples; they necessitate very experienced technicians; and the initial instrumentation is expensive and requires large investment by the lab. Moreover, pre-analytical and analytical aspects in these methods need careful consideration, including sample type, protein precipitation, analyte extraction, derivatization, chromatographic separation ionization, and capabilities of the mass spectrometer. Calibration, standardization, and the use of internal standards are other important issues that impact on the accuracy of results. Only well-designed methods that are under continuous internal and external quality control allow accurate and stable measurement of 25(OH)D and other metabolites, such as 1,25(OH)2D 24R,25(OH)2D and the epimer [77].
Analytical variability and the standardization of the 25(OH)D assays
Serum total 25(OH)D, as expressed by the sum of the serum concentrations of 25(OH)D2 and 25(OH)D3, is considered to be the best biological marker of an individual’s vitamin D status. Several medical societies and government agencies have issued vitamin D guidelines; however, differences exist in these guidelines as regards defining deficiency, insufficiency, and sufficiency, this creating a great deal of controversy [78, 79]. However, a fundamental factor that confounds efforts to develop consensus clinical and nutritional public health guidelines for interpreting serum 25(OH)D concentration is the substantial variability that existed (and still exists) in many assays that have been used over the years to measure 25(OH)D in clinical research studies [80]. The lack of assay standardization is the main source of bias, making it impossible to pool research results in order to develop consensus cut-points [81].
What is the VDSP?
To overcome these problems, the Vitamin D Standardization Program (VDSP) was established in 2010 by the Office of Dietary Supplements, National Institutes of Health, as an international collaborative effort with the National Institute for Standards and Technology (NIST), Centers for Disease Control and Prevention (CDC) and Gent University in Belgium, the AACC, the IFCC, and national health and nutrition surveys from Australia, Canada, Germany, Ireland, Mexico, South Korea, United Kingdom and the USA [82].
What is standardization?
In terms of 25(OH)D, a standardized laboratory measurement is one that is “comparable across measurement system, location and time” [83]. This means that every laboratory, regardless of the type of assay it uses, the location, or the time (now or in the future), would report the same 25(OH)D result for the same sample—within certain predetermined statistical limits—as would be obtained using one of the internationally recognized gold standard RMPs developed by the NIST, Ghent University, and the CDC [84]. In other words, each “standardized laboratory” would report the true concentration of serum total 25(OH)D. It is also important to note here that standardization is different from harmonization. Harmonization is a process by which all laboratories report the same value for a given specimen, though the value is not necessarily the true one [85]. Standardization allows for the development and consistent application of evidenced-based guidelines. It is the first crucial step in comparing and contrasting results from different studies, whether they are clinical trials or observational epidemiological studies. With standardization, it is possible to achieve long-term stability of measurement results both in research and patient care.
Development of validated analytical methods
In order to standardize an assay and to develop primary reference materials (PRM), critically evaluated analytical methods are required. The highest level of a validated analytical method is a Reference Measurement Procedure (RMP). A RMP is a measurement procedure that has been validated to measure what it is intended to measure, has been thoroughly assessed for potential sources of bias, and is certified by the Joint Committee for Traceability in Laboratory Medicine (JCTLM). For well-defined, small-molecule clinical markers, RMPs are typically based on isotope dilution Mass Spectrometry (IDMS). To assist in the standardization of measurements of total 25(OH)D, the NIST first developed a RMP based on ID LC-MS/MS for the determination of 25(OH)D2 and 25(OH)D3 in human serum [86]. This method is now recognized by the JCTLM as a RMP. Later, Stepman et al. (at Ghent University, Belgium) also described an ID LC-MS/MS method for the determination of 25(OH)D2 and 25(OH) D3, which was also recognized as a RMP for 25(OH)D by the JCTLM [84]. Finally, the CDC also developed an ID LC-MS/MS method that was subsequently recognized by the JCTLM as a RMP for 25(OH)D [87]. These three methods are currently the only JCTLM-recognized RMPs for the determination of 25(OH)D2 and 25(OH)D3, and these RMPs play a critical role in the VDSP.
What has the VDSP achieved?
The VDSP has developed a reference measurement system that is the backbone for standardizing 25(OH)D measurement in current and future assay systems [88, 89]. The components of this reference measurement system include: [1] the gold standard RMPs, (2) the NIST Standard Reference Materials (SRMs), (3) the VDSP’s Standardization Certification Program which was developed, conducted, and maintained by the CDC, (4) the accuracy-based performance testing or external quality assessment schemes (PT/EQA) conducted by the College of American Pathologists and the Vitamin D External Quality Assessment Scheme or DEQAS [86, 90], (5) methods for retrospective standardization of studies completed in the past, and (6) a set of laboratory performance guidelines for both reference laboratories (those that run the RMP) and for routine laboratories developed by the VDSP [90].
The practical application of the VDSP consists in allowing the results of a clinical laboratory to be traceable to the gold standard RMP. If the lab uses a commercially available method, then the producer of the assay is responsible to ensure the traceability of its commercial method to the RMP. On the other hand, if it is an in-house developed method, then it is the lab’s responsibility to ensure traceability [91]. Health care providers should understand the importance of the knowledge that their clinical assay is traceable to a RMP, since this provides information on both assay mean bias and variability (CV). This has enabled the VDSP to adopt 25(OH)D assay performance criteria developed by Stockl et al. for different types of labs and assays [90]. Specifically, for the RMPs, the limits for total CV and mean bias should be less than or equal to 5% and less than or equal to 1.7%, respectively. For routine laboratories, the limits for total CV and mean bias should be less than or equal to 10% and less than or equal to 5%, respectively. Thus, for a clinical laboratory 25(OH)D assay to be defined as traceable to the NIST-Ghent-CDC RMPs, it must demonstrate a CV less than or equal to 10% and mean bias of less than or equal to ± 5%.
How is the performance of assays assessed?
Participation of laboratories in proficiency testing or external quality assessment schemes is necessary to evaluate and improve analytical performance. The accuracy-based surveys are a very special type of EQA [92]. While there are several Vitamin D EQA programs around the world, to our knowledge, there are only two accuracy-based programs, namely, the CAP program in the USA and DEQAS for the rest of the world. Specifically, “accuracy-based” means that each laboratory’s results, for each EQA sample, is compared to the “true value”, as this was determined by one of the three recognized RMPs. The CDC assigns target values to the CAP materials using their RMP. The NIST did the same for DEQAS from October 2012 through July 2018; since then, the CDC has assigned target values to DEQAS serum materials or samples The VDSP suggests that all laboratories should participate in an accuracy-based EQA scheme simply because a laboratory can determine the bias in their assay versus the true concentration, thereby helping to promote assay standardization [83].
Conclusions—key points
Vitamin D produced in the skin or ingested via the diet is biologically inert and requires two successive hydroxylations to form its biologically active form, calcitriol.
Serum total 25(OH)D, the sum of 25(OH)D2 and 25(OH)D3, is the best reflection of vitamin D status. It is the main circulating metabolite of vitamin D, with a long half-life, and its high concentration facilitates its measurement.
Over the years, several methods have been developed for its measurement, with automated immunoassays with liquid chromatography coupled with tandem mass spectroscopy (LC-MS/MS) being the latest methods developed. They are now considered as the preferred methods for the quantitation of 25(OH)D, since they can measure both 25(OH)D2 and 25(OH)D3.
Standardization was a major achievement of the VDSP, as it succeeded in minimizing the substantial variability that was associated with laboratory measurement of 25(OH)D.
Abbreviations
- 7-DHC:
-
dehydrocholesterol or provitamin D3
- 24,25(OH)2D3:
-
24,25-dihydroxyvitamin D3
- 25(OH)D3:
-
calcidiol or 25-hydroxyvitamin D3
- 1α,25(OH)2D3:
-
calcitriol or 1,25-dihydroxyvitamin D3
- C3-epi-25(OH)D:
-
C3-epimer of the 25(OH)D
- CYP27B1:
-
25(OH)D-1a-hydroxylase
- CYP24A1:
-
24-hydroxylase
- PTH:
-
parathyroid hormone
- FGF-23:
-
fibroblast growth factor-23
- VDBP:
-
vitamin D binding protein
- VDDR:
-
vitamin D-dependent rickets
- VDR:
-
vitamin D receptor
- VDSP:
-
Vitamin D Standardization Program
- CLD:
-
chronic liver disease
- CKD:
-
chronic kidney disease
- SHPT:
-
secondary hyperparathyroidism
- UV:
-
ultraviolet
- HPLC:
-
high-performance liquid chromatography
- LC-MS/MS:
-
liquid chromatography coupled with mass spectrometry
- CPBA:
-
competitive protein binding assays
- RIA:
-
radioimmunoassays
- ELISA:
-
enzyme-linked immunosorbent assays
- CLIA:
-
chemiluminescent assays
- RMP:
-
reference measurement procedure
- PRM:
-
primary reference material
- NIST:
-
National Institute for Standards and Technology
- IFCC:
-
International Federation of Clinical Chemistry
- JCTLM:
-
Joint Committee for Traceability in Laboratory Medicine
- AACC:
-
American Association for Clinical Chemistry
- DEQAS:
-
Vitamin D External Quality Assessment Scheme
- CAP:
-
College of American Pathologists
- CDC:
-
Center for Disease Control
- EQA:
-
External Quality Assessment
References
Bikle DD (2012) Vitamin D and bone. Curr Osteoporos Rep 10(2):151–159
Holick MF (1995) Environmental factors that influence the cutaneous production of vitamin D. Am J Clin Nutr 61(3 Suppl):638S–645S
Holick MF (2007) Vitamin D deficiency. N Engl J Med 357(3):266–281
Haddad JG, Matsuoka LY, Hollis BW, Hu YZ, Wortsman J (1993) Human plasma transport of vitamin D after its endogenous synthesis. J Clin Invest 91(6):2552–2555
Jones G (2012) Metabolism and biomarkers of vitamin D. Scand J Clin Lab Investig Suppl 243:7–13
Christakos S, Dhawan P, Verstuyf A, Verlinden L, Carmeliet G (2016) Vitamin D: Metabolism, molecular mechanism of action, and pleiotropic effects. Physiol Rev 96(1):365–408
Jones G, Prosser DE, Kaufmann M (2014) Cytochrome P450-mediated metabolism of vitamin D. J Lipid Res 55(1):13–31
Henry HL (2011) Regulation of vitamin D metabolism. Best Pract Res Clin Endocrinol Metab 25(4):531–541
Jones G, Kottler ML, Schlingmann KP (2017) Genetic diseases of Vitamin D metabolizing enzymes. Endocrinol Metab Clin N Am 46(4):1095–1117
Nykjaer A, Dragun D, Walther D, Vorum H, Jacobsen C, Herz J et al (1999) An endocytic pathway essential for renal uptake and activation of the steroid 25-(OH) vitamin D3. Cell 96(4):507–515
Kaseda R, Hosojima M, Sato H, Saito A (2011) Role of megalin and cubilin in the metabolism of vitamin D(3). Ther Apher Dial 15(Suppl 1):14–17
Takeda E, Yamamoto H, Taketani Y, Miyamoto K (1997) Vitamin D-dependent rickets type I and type II. Acta Paediatr Jpn 39(4):508–513
Bikle DD (2014) Vitamin D metabolism, mechanism of action, and clinical applications. Chem Biol 21(3):319–329
Bosworth C, de Boer IH (2013) Impaired vitamin D metabolism in CKD. Semin Nephrol 33(2):158–168
Jones G, Strugnell SA, DeLuca HF (1998) Current understanding of the molecular actions of vitamin D. Physiol Rev 78(4):1193–1231
Jones G (2008) Pharmacokinetics of vitamin D toxicity. Am J Clin Nutr 88(2):582S–586S
Tebben PJ, Singh RJ, Kumar R (2016) Vitamin D-mediated Hypercalcemia: mechanisms, diagnosis, and treatment. Endocr Rev 37(5):521–547
Gupta RP, He YA, Patrick KS, Halpert JR, Bell NH (2005) CYP3A4 is a vitamin D-24- and 25-hydroxylase: analysis of structure function by site-directed mutagenesis. J Clin Endocrinol Metab 90(2):1210–1219
Roizen JD, Li D, O'Lear L, Javaid MK, Shaw NJ, Ebeling PR et al (2018) CYP3A4 mutation causes vitamin D-dependent rickets type 3. J Clin Invest 128(5):1913–1918
Reddy GS, Muralidharan KR, Okamura WH, Tserng KY, McLane JA (2001) Metabolism of 1alpha,25-dihydroxyvitamin D(3) and its C-3 epimer 1alpha,25-dihydroxy-3-epi-vitamin D(3) in neonatal human keratinocytes. Steroids 66(3–5):441–450
Bailey D, Veljkovic K, Yazdanpanah M, Adeli K (2013) Analytical measurement and clinical relevance of vitamin D(3) C3-epimer. Clin Biochem 46(3):190–196
Kamao M, Tatematsu S, Hatakeyama S, Sakaki T, Sawada N, Inouye K et al (2004) C-3 epimerization of vitamin D3 metabolites and further metabolism of C-3 epimers: 25-hydroxyvitamin D3 is metabolized to 3-epi-25-hydroxyvitamin D3 and subsequently metabolized through C-1alpha or C-24 hydroxylation. J Biol Chem 279(16):15897–15907
Singh RJ, Taylor RL, Reddy GS, Grebe SK (2006) C-3 epimers can account for a significant proportion of total circulating 25-hydroxyvitamin D in infants, complicating accurate measurement and interpretation of vitamin D status. J Clin Endocrinol Metab 91(8):3055–3061
Lensmeyer G, Poquette M, Wiebe D, Binkley N (2012) The C-3 epimer of 25-hydroxyvitamin D(3) is present in adult serum. J Clin Endocrinol Metab 97(1):163–168
Zerwekh JE (2008) Blood biomarkers of vitamin D status. Am J Clin Nutr 87(4):1087S–1091S
Baecher S, Leinenbach A, Wright JA, Pongratz S, Kobold U, Thiele R (2012) Simultaneous quantification of four vitamin D metabolites in human serum using high performance liquid chromatography tandem mass spectrometry for vitamin D profiling. Clin Biochem 45(16–17):1491–1496
Wong RG, Myrtle JF, Tsai HC, Norman AW (1972) Studies on calciferol metabolism. V. the occurrence and biological activity of 1,25-dihydroxy-vitamin D 3 in bone. J Biol Chem 247(18):5728–5735
Norman AW, Okamura WH, Friedlander EJ, Henry HL, Johnson RL, Mitra MN et al (1976) Current concepts of the chemical conformation, metabolism, and interaction of the steroid, vitamin D, with the endocrine system for calcium homeostasis. Calcif Tissue Res 21(Suppl):153–159
Herrmann M, Farrell CL, Pusceddu I, Fabregat-Cabello N, Cavalier E (2017) Assessment of vitamin D status - a changing landscape. Clin Chem Lab Med 55(1):3–26
Heureux N, Vitamin D (2017) Testing-where are we and what is on the horizon? Adv Clin Chem 78:59–101
Makowski AJ, Rathmacher JA, Horst RL, Sempos CT (2017) Simplified 25-Hydroxyvitamin D standardization and optimization in dried blood spots by LC-MS/MS. J AOAC Int 100(5):1328–1336
Hayden Y, Pillay T, Marx G, de Lange W, Kuyl Johannes M. Pre-analytical stability of 25(OH)-vitamin D in primary collection tubes. Clinical Chemistry and Laboratory Medicine (CCLM)2015. p. e55
Maxwell JD (1994) Seasonal variation in vitamin D. Proc Nutr Soc 53(3):533–543
Webb AR, Kline L, Holick MF (1988) Influence of season and latitude on the cutaneous synthesis of vitamin D3: exposure to winter sunlight in Boston and Edmonton will not promote vitamin D3 synthesis in human skin. J Clin Endocrinol Metab 67(2):373–378
Wang TJ, Zhang F, Richards JB, Kestenbaum B, van Meurs JB, Berry D et al (2010) Common genetic determinants of vitamin D insufficiency: a genome-wide association study. Lancet 376(9736):180–188
Guessous I, Dudler V, Glatz N, Theler JM, Zoller O, Paccaud F et al (2012) Vitamin D levels and associated factors: a population-based study in Switzerland. Swiss Med Wkly 142:0
Gallagher JC (2013) Vitamin D and aging. Endocrinol Metab Clin N Am 42(2):319–332
Gloth FM 3rd, Gundberg CM, Hollis BW, Haddad JG Jr, Tobin JD (1995) Vitamin D Deficiency in homebound elderly persons. Jama 274(21):1683–1686
Migliaccio S, Di Nisio A, Mele C, Scappaticcio L, Savastano S, Colao A et al (2019) Obesity and hypovitaminosis D: causality or casualty? Int J Obes Suppl 9(1):20–31
Vanlint S (2013) Vitamin D and obesity. Nutrients 5(3):949–956
Clemens TL, Adams JS, Henderson SL, Holick MF (1982) Increased skin pigment reduces the capacity of skin to synthesise vitamin D3. Lancet 1(8263):74–76
Jablonski NG (2004) The evolution of human skin and skin color. Annu Rev Anthropol 33(1):585–623
Arteh J, Narra S, Nair S (2010) Prevalence of Vitamin D deficiency in chronic liver disease. Dig Dis Sci 55(9):2624–2628
Costa Silva M, Erotides Silva T, de Alentar ML, Honorio Coelho MS, Wildner LM, Bazzo ML et al (2015) Factors associated with 25-hydroxyvitamin D levels in patients with liver cirrhosis. Ann Hepatol 14(1):99–107
Kitson MT, Roberts SK (2012) D-livering the message: the importance of vitamin D status in chronic liver disease. J Hepatol 57(4):897–909
Corey RL, Whitaker MD, Crowell MD, Keddis MT, Aqel B, Balan V et al (2014) Vitamin D deficiency, parathyroid hormone levels, and bone disease among patients with end-stage liver disease and normal serum creatinine awaiting liver transplantation. Clin Transpl 28(5):579–584
Lai JC, Bikle DD, Lizaola B, Hayssen H, Terrault NA, Schwartz JB (2015) Total 25(OH) vitamin D, free 25(OH) vitamin D and markers of bone turnover in cirrhotics with and without synthetic dysfunction. Liver Int 35(10):2294–2300
Wiese RJ, Uhland-Smith A, Ross TK, Prahl JM, DeLuca HF (1992) Up-regulation of the vitamin D receptor in response to 1,25-dihydroxyvitamin D3 results from ligand-induced stabilization. J Biol Chem 267(28):20082–20086
Dusso AS, Tokumoto M (2011) Defective renal maintenance of the vitamin D endocrine system impairs vitamin D renoprotection: a downward spiral in kidney disease. Kidney Int 79(7):715–729
Jean G, Souberbielle JC, Chazot C (2017) Vitamin D in Chronic Kidney Disease and Dialysis Patients. Nutrients 9(4)
Dusso AS (2011) Kidney disease and vitamin D levels: 25-hydroxyvitamin D, 1,25-dihydroxyvitamin D, and VDR activation. Kidney Int Suppl 1(4):136–141
Guessous I, McClellan W, Kleinbaum D, Vaccarino V, Zoller O, Theler JM et al (2014) Comparisons of serum vitamin D levels, status, and determinants in populations with and without chronic kidney disease not requiring renal dialysis: a 24-hour urine collection population-based study. J Ren Nutr 24(5):303–312
Melamed ML, Astor B, Michos ED, Hostetter TH, Powe NR, Muntner P (2009) 25-hydroxyvitamin D levels, race, and the progression of kidney disease. J Am Soc Nephrol 20(12):2631–2639
Agarwal R, Georgianos PI (2016) Con: nutritional vitamin D replacement in chronic kidney disease and end-stage renal disease. Nephrol Dial Transplant 31(5):706–713
Goldsmith DJ (2016) Pro: should we correct vitamin D deficiency/insufficiency in chronic kidney disease patients with inactive forms of vitamin D or just treat them with active vitamin D forms? Nephrol Dial Transplant 31(5):698–705
Bosworth CR, Levin G, Robinson-Cohen C, Hoofnagle AN, Ruzinski J, Young B et al (2012) The serum 24,25-dihydroxyvitamin D concentration, a marker of vitamin D catabolism, is reduced in chronic kidney disease. Kidney Int 82(6):693–700
Lee SW, Russell J, Avioli LV (1977) 25-hydroxycholecalciferol to 1,25-dihydroxycholecalciferol: conversion impaired by systemic metabolic acidosis. Science 195(4282):994–996
Vanholder R, Patel S, Hsu CH (1993) Effect of uric acid on plasma levels of 1,25(OH)2D in renal failure. J Am Soc Nephrol 4(4):1035–1038
Saraf R, Morton SM, Camargo CA Jr, Grant CC (2016) Global summary of maternal and newborn vitamin D status - a systematic review. Matern Child Nutr 12(4):647–668
Christesen HT, Elvander C, Lamont RF, Jorgensen JS (2012) The impact of vitamin D in pregnancy on extraskeletal health in children: a systematic review. Acta Obstet Gynecol Scand 91(12):1368–1380
Heijboer AC, Blankenstein MA, Kema IP, Buijs MM (2012) Accuracy of 6 routine 25-hydroxyvitamin D assays: influence of vitamin D binding protein concentration. Clin Chem 58(3):543–548
Lips P (2007) Relative value of 25(OH)D and 1,25(OH)2D measurements. J Bone Miner Res 22(11):1668–1671
Su Z, Narla SN, Zhu Y (2014) 25-Hydroxyvitamin D: analysis and clinical application. Clin Chim Acta 433:200–205
Bikle DD, Vitamin D (2018) Assays. Front Horm Res 50:14–30
Holick MF (2009) Vitamin D status: measurement, interpretation, and clinical application. Ann Epidemiol 19(2):73–78
Gil A, Plaza-Diaz J, Mesa MD (2018) Vitamin D: Classic and novel actions. Ann Nutr Metab 72(2):87–95
Haddad JG, Chyu KJ (1971) Competitive protein-binding radioassay for 25-hydroxycholecalciferol. J Clin Endocrinol Metab 33(6):992–995
Hollis BW, Napoli JL (1985) Improved radioimmunoassay for vitamin D and its use in assessing vitamin D status. Clin Chem 31(11):1815–1819
Couchman L, Moniz CF (2017) Analytical considerations for the biochemical assessment of vitamin D status. Ther Adv Musculoskelet Dis 9(4):97–104
Sturgeon CM, Viljoen A (2011) Analytical error and interference in immunoassay: minimizing risk. Ann Clin Biochem 48(Pt 5):418–432
Ward G, Simpson A, Boscato L, Hickman PE (2017) The investigation of interferences in immunoassay. Clin Biochem 50(18):1306–1311
Ekins RP (1989) Multi-analyte immunoassay. J Pharm Biomed Anal 7(2):155–168
Omi K, Ando T, Sakyu T, Shirakawa T, Uchida Y, Oka A et al (2015) Noncompetitive immunoassay detection system for haptens on the basis of antimetatype antibodies. Clin Chem 61(4):627–635
Cavalier E, Lukas P, Bekaert AC, Peeters S, Le Goff C, Yayo E et al (2016) Analytical and clinical evaluation of the new Fujirebio Lumipulse(R)G non-competitive assay for 25(OH)-vitamin D and three immunoassays for 25(OH)D in healthy subjects, osteoporotic patients, third trimester pregnant women, healthy African subjects, hemodialyzed and intensive care patients. Clin Chem Lab Med 54(8):1347–1355
Jones G, DeLuca HF (1975) High-pressure liquid chromatography: separation of the metabolites of vitamins D2 and D3 on small-particle silica columns. J Lipid Res 16(6):448–453
Jones G, Kaufmann M (2016) Vitamin D metabolite profiling using liquid chromatography–tandem mass spectrometry (LC–MS/MS). J Steroid Biochem Mol Biol 164:110–114
Zelzer S, Goessler W, Herrmann M (2018) Measurement of vitamin D metabolites by mass spectrometry, an analytical challenge. J Lab Precis Med 3
Holick MF, Binkley NC, Bischoff-Ferrari HA, Gordon CM, Hanley DA, Heaney RP et al (2012) Guidelines for preventing and treating vitamin D deficiency and insufficiency revisited. J Clin Endocrinol Metab 97(4):1153–1158
Io M (2011) In: Ross AC, Taylor CL, Yaktine AL, Del Valle HB (eds) Dietary reference intakes for calcium and Vitamin D. The National Academies Press, Washington, p 1132
Binkley N, Krueger D, Cowgill CS, Plum L, Lake E, Hansen KE et al (2004) Assay variation confounds the diagnosis of hypovitaminosis D: a call for standardization. J Clin Endocrinol Metab 89(7):3152–3157
Sempos CT, Durazo-Arvizu RA, Binkley N, Jones J, Merkel JM, Carter GD (2016) Developing vitamin D dietary guidelines and the lack of 25-hydroxyvitamin D assay standardization: the ever-present past. J Steroid Biochem Mol Biol 164:115–119
Sempos CT, Vesper HW, Phinney KW, Thienpont LM, Coates PM, Vitamin DSP (2012) Vitamin D status as an international issue: national surveys and the problem of standardization. Scand J Clin Lab Investig Suppl 243:32–40
Binkley N, Carter GD (2017) Toward clarity in clinical Vitamin D status assessment: 25(OH)D assay standardization. Endocrinol Metab Clin N Am 46(4):885–899
Stepman HCM, Vanderroost A, Van Uytfanghe K, Thienpont LM (2011) Candidate reference measurement procedures for serum 25-Hydroxyvitamin D3 and 25-Hydroxyvitamin D2 by using isotope-dilution liquid chromatography–tandem mass spectrometry. Clin Chem 57(3):441–448
Greg Miller W, Myers GL, Lou Gantzer M, Kahn SE, Schonbrunner ER, Thienpont LM et al (2011) Roadmap for harmonization of clinical laboratory measurement procedures. Clin Chem 57(8):1108–1117
Tai SS, Bedner M, Phinney KW (2010) Development of a candidate reference measurement procedure for the determination of 25-hydroxyvitamin D3 and 25-hydroxyvitamin D2 in human serum using isotope-dilution liquid chromatography-tandem mass spectrometry. Anal Chem 82(5):1942–1948
Mineva EM, Schleicher RL, Chaudhary-Webb M, Maw KL, Botelho JC, Vesper HW et al (2015) A candidate reference measurement procedure for quantifying serum concentrations of 25-hydroxyvitamin D(3) and 25-hydroxyvitamin D(2) using isotope-dilution liquid chromatography-tandem mass spectrometry. Anal Bioanal Chem 407(19):5615–5624
Binkley N, Sempos CT, Vitamin DSP (2014) Standardizing vitamin D assays: the way forward. J Bone Miner Res 29(8):1709–1714
Sempos CT, Betz JM, Camara JE, Carter GD, Cavalier E, Clarke MW et al (2017) General steps to standardize the laboratory measurement of serum Total 25-Hydroxyvitamin D. J AOAC Int 100(5):1230–1233
Stockl D, Sluss PM, Thienpont LM (2009) Specifications for trueness and precision of a reference measurement system for serum/plasma 25-hydroxyvitamin D analysis. Clin Chim Acta 408(1–2):8–13
Vesper HW, Thienpont LM (2009) Traceability in laboratory medicine. Clin Chem 55(6):1067–1075
Miller WG, Jones GR, Horowitz GL, Weykamp C (2011) Proficiency testing/external quality assessment: current challenges and future directions. Clin Chem 57(12):1670–1680
Acknowledgments
None of the authors declares any funding or grant related to this article.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Makris, K., Sempos, C. & Cavalier, E. The measurement of vitamin D metabolites: part I—metabolism of vitamin D and the measurement of 25-hydroxyvitamin D. Hormones 19, 81–96 (2020). https://doi.org/10.1007/s42000-019-00169-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s42000-019-00169-7