Abstract
Heart rate variability (HRV) considered as an indicator of the autonomic activity, shows differences between NREM and REM sleep. However, when evaluating during NREM sleep, some authors evaluate without considering the different stages, while others do it. There are discrepancies between values obtained from stages N2 and N3. Our objective was to evaluate whether differences exist between stages N2 and N3 based on several metrics of HRV that reflect the autonomic activity. Additionally, we analyzed the structure of these metrics through principal component analysis (PCA) at each sleep stage. Polysomnograms were recorded in 24 healthy subjects. We found significant differences in the LF and THM metrics with higher values in stage N2. The relative power of HF metric showed a significant difference with higher value in stage N3, however, this metric showed inconsistencies related to other HF representations. Two factors were extracted with PCA and their structure was stable across sleep stages. One factor accounted for 92% of the variance during stage N2 with moderate to high loadings for metrics most strongly associated with the parasympathetic activity. A second factor accounted for 91% of the variance during stage N3 with moderate to high loadings for metrics associated with parasympathetic and blood pressure control. Physiological mechanisms regulated by central commands that may involve neurons in the hypothalamus, pons, and midbrain may explain the differences in LF and THM metrics. The combination of stages N2 and N3 as NREM should be done according to the type of HRV metrics used.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Heart rate variability (HRV) is the physiological phenomenon associated with variation among the intervals between heartbeats, and these variations can be analyzed by different methods, some of these provide indirect measures of the autonomic regulation of cardiac activity, mainly for the parasympathetic nervous system (PNS) [1]. During non-rapid eye movement (NREM) sleep, a predominance of PNS activity and a decrease in sympathetic nervous system (SNS) activity have been proposed to occur, whereas during rapid eye movement (REM) sleep, a predominance of SNS activity and fluctuations in PNS activity occur [2]. Studies in which HRV analysis has been implemented during sleep have confirmed the existence of differences in the pattern of autonomic activity between NREM and REM sleep [3].
The separation of the NREM sleep into different stages is based only on electroencephalographic activity, as in the case of sleep stages S1 to S4 [4] or N1, N2, and N3 [5]. Stage S1 or N1 presents acute vertex waves, while stage S2 or N2 exhibits the presence of sleep spindles and K complexes. Stages S3, S4, and N3 are characterized by predominant delta activity, S3 and S4 are often known as slow-wave sleep (SWS). In some studies, the HRV analysis was performed considering the separation of NREM sleep into stages [6,7,8], while in others not [9,10,11], even in the same study the HRV analysis was performed in NREM sleep with and without separation into stages [12].
In considering the High-frequency (HF) component of HRV (this component reflects PNS activity) there are discrepancies in the literature with respect to differences between stages N2 and N3, in some studies, the highest value was observed during stage N3 [13,14,15,16], while in others in stage N2 [17, 18], showing significant differences between these two stages [13, 16, 17]. The discrepancies would be related to the absolute and relative representation of HF Power that were compared [19]. There are also inconsistencies between different metrics that reflect PNS activity such as HF and root mean square of successive of RR interval differences (RMSSD), with higher HF power in stage N3 and higher RMSSD in stage N2 [20, 21].
Considering the previously mentioned studies, the relationship between the NREM sleep stage and HRV is not clear. Therefore, the objective of this study was to determine whether differences exist between stages N2 and N3 based on several HRV metrics that reflect the autonomic activity. Additionally, we realized an empirical evaluation of the structure of these metrics at each sleep stage.
Materials and methods
Participants
Thirty healthy volunteers participated in the study. Six subjects did not complete the 5-min duration of cardiac activity in the N2 stage of the first sleep cycle; therefore, the final sample included 24 participants (14 women and 10 men) with an average age of 25 (standard deviation (SD) = 5.1) years.
The inclusion criteria were that participants did not smoke, only consumed alcohol occasionally, and did not use illegal drugs. In addition, participants did not have problems falling or staying asleep. Based on an interview, subjects with medical diagnoses of chronic illness or psychiatric disorders were excluded. All participants were provided with information about the investigation procedure and subsequently signed an informed consent letter. Besides, the evaluation procedures were conducted in accordance with the basic principles established in the Declaration of Helsinki.
Procedure
Two 8 h polysomnogram (PSG) were recorded during consecutive nights at the Neurosciences Laboratory of the Psychology Department of the UNAM, Mexico. PSGs were conducted using a Cadwell Easy II equipment (Kennewick, Washington, USA). The first PSG was considered as habituation to recording conditions and served to detect the presence of any indicators of sleep disorders. In the second PSG, the EEG leads F3-M2, F4-M1, C3-M2, C4-M1, O1-M2 and, O2-M1 were recorded, as well as the electrooculogram, the surface electromyogram and, the electrocardiogram. The beginning of the PSG recording was adjusted for each participant according to their usual time to go to sleep. Sleep stages were scored according to AASM rules [5]. For this study, only the data obtained from the second PSG of participants who did not present indications of sleep disorders on the adaptation night were considered.
HRV metrics
Five-minute segments of cardiac activity of stages N2 and N3 corresponding to the first and second NREM-REM cycles were analyzed. These stages were stable without any type of interruptions due to arousal or movements. Periods of cardiac activity were omitted two minutes before and after phase transitions. The inter-beat intervals (IBI) were obtained using the QRSTool software version 1.2.2 [22]. Subsequently, HRV metrics were calculated using the CardioBatch (Brain-Body Center, University of Illinois, 2007) and Kubios HRV [23].
In addition to the interbeat interval (IBI) or heart period (HP) the following HRV metrics were calculated:
High-frequency (HF) band (0.15–0.4 Hz), calculated by mean of the fast Fourier Transform (FFT) using the Welch’s Periodogram method. Expressed as absolute power with natural logarithm (HFAP), relative power (HFRP), and with the coefficient of variation transformation (HFCV) which is obtained as follows:
Respiratory sinus arrhythmia (RSA) (0.12–0.4 Hz), calculated by the Porges–Bohrer method [24]. Expressed as natural logarithm (RSAln) and with the coefficient of variation transformation (RSACV) which is obtained as follows:
Root mean square of successive of RR interval differences (RMSSD), expressed in milliseconds (RMSSD) and with the coefficient of variation transformation (RMSSDCV) which is obtained as follows:
Low-frequency (LF) band (0.04–0.15 Hz), calculated by using the FFT using the Welch´s Periodogram method. Expressed as absolute power with natural logarithm (LFAP), relative power (LFRP), and with the coefficient of variation transformation (LFCV) which is obtained as follows:
Traube–Hering–Mayer wave (THM) (0.06–0.1 Hz), calculated by the Porges–Bohrer method. Expressed as natural logarithm (THMln) and with the coefficient of variation transformation (THMCV) which has the form:
The coefficient of variation transformation is based on De Geus et al., recommendation [25].
Data analysis
The Shapiro–Wilk test was used to corroborate a normal distribution of all HRV measurements; therefore, Student's t test for related samples was used to compare stages N2 and N3. To examine the structure of HF, RSA, RMSSD, LF, and THM at each stage, we conducted principal component analysis (PCA) with varimax rotation (with Kaiser normalization).
Results
Participants displayed the normal sleep patterns organized into cycles integrated by the different phases that repeated across the night. The quantitative characteristics of the sleep parameters were as follows: the average sleep efficiency was 95% (SD = 2); while the percentages of each sleep phase were 8% (SD = 4) for N1, 50% (SD = 9) for N2, 20% (SD = 8) for N3, and 21% (SD = 4) for REM sleep.
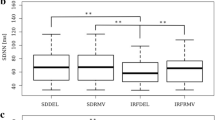
A total of 435 5-min segments of cardiac activity were selected from the polysomnographic recordings; 162 segments corresponded to the stage N2, and 273 segments to the stage N3. Except for HP and HFRP the remaining metrics exhibited the highest values in the stage N2 (Table 1). In the comparison between the sleep stages using Student's t test, significant differences were found in HFRP and all the representations of LF and THM metrics (Table 1).
For PCA, Kaiser–Meyer–Olkin (KMO) measure was 0.71 for stage N2 and 0.74 for stage N3. Significance level of Bartlett's test of sphericity was less than 0.001 for both stages. Factor structure was highly stable across sleep stages (Table 2). Two factors accounted for 92% of the variance during stage N2 and 91% of the variance during stage N3.
In stage N2, factor 1 included moderate to high loadings for all representations of HF, RSA, and RMSSD, this factor includes negative high loading for LFRP. Conversely, factor 2 included high loadings for LFAP, LFCV, and all representations of THM.
In stage N3, factor 1 included moderate for HFCV and high loadings for HFAP and all representations of RSA and RMSSD. Conversely, factor 2 included moderate to high loadings for all representations of LF and THM, this factor includes negative moderate loading for HFRP.
For factor 1 the relative power of HF and LF showed reduced loadings from N2 to N3 sleep stages, the loadings for these metrics were low only for the factor 2 of the stage N2. Moreover, in stage N3, these metrics showed an inverse relationship between both factors.
Discussion
Stage N1 was not considered in this analysis because it usually lasts only a few minutes [26] and can be interrupted by awakenings and arousals; thus, it is difficult to obtain 5-min segments for analysis. The LF and THM metrics mainly provide information about PNS and blood pressure (BP) control mechanisms, such as the modulation of vasomotor tone [27] and baroreceptor activity [28], while the HF and RSA metrics are strongly associated with the relationship between cardiorespiratory coupling and PNS cardiac control [1]. RMSSD is a time-domain metric sensitive to PNS activity but less affected by respiration patterns although it is highly correlated with HF [25].
For all metrics with higher values in stage N2, there were significant differences in the LF and THM metrics, and these results coincide with those reported by other authors [8, 13, 14]. As stated previously, there are discrepancies in the literature with respect to HF differences between stages N2 and N3. We found inconsistency with the HFRP metric, which showed a significant difference with a higher value in stage N3; the rest of the metrics (HF, RSA, and RMSSD) showed higher values in stage N2, but these changes did not reach statistical significance. This discrepancy could be explained by the reciprocity or redundancy between LF and HF components expressed as normalized units or relative to total power [27, 29] so that the significant difference found in HFRP was due to the LFRP metric.
As stated by de Geus et al., there is a model in which cardiac chronotropic state (mean HP) has a direct effect on HRV that is independent of PNS activity, which would complicate the use of HRV metrics as indexes of PNS activity. Adjusting for HP avoids overestimation of the influence of PNS on HRV, but if the proposed model is false, adjusting HRV for HP would lead to an underestimation of PNS activity. Until the determination of the veracity of the model, it is recommended to include an adjustment method for the prevailing levels of cardiac chronotropic state [25]. We included the coefficient of variation (CV) as the adjustment method. With the exception of the HFRP metric, the CV did not alter the differences found between stages N2 and N3 for the other HRV metrics. The above results suggest that these differences could not be explained by an error in estimating PNS activity.
It has been proposed that cardiac PNS activity is influenced by the circadian system rather than by the sleep system [8, 30]. Circadian influence has been shown with the HF metric [19], which would explain the lack of significant differences between stages N2 and N3 in the HF, RSA, and RMSSD metrics. However, we found that the LF and THM metrics, which are also related to PNS activity, differed at stages N2 and N3, which suggests that they are more influenced by the sleep system than by the circadian system.
PCA provides a method to assess the degree to which HRV metrics share a similar structure. This method has been used previously to analyze the factor structure of some HRV metrics at rest and during a stressor task [22]. In the PCA, two factors were extracted, and their structure was stable across sleep stages. In both sleep stages, the first factor included all HF metrics and LFRP only, the latter with negative loading, which would confirm the reciprocity between the relative power of LF and HF. By omitting these reciprocal metrics, factor 1 would consist of HF, RSA, and RMSSD, and factor 2 would consist of LF and THM. Although all the metrics relate to PNS control [1, 25, 27], the separation into two different factors coincides with the type of physiological control mechanisms: one factor is related to cardiorespiratory coupling mainly, the other factor is associated with the interaction between PNS and BP control mechanisms. Furthermore, this factor structure coincides with empirical data, and only factor 2 metrics differed between stages N2 and N3.
In agreement with the significantly lower values of LF and THM we observed in stage N3, it has been reported that the lowest levels of arterial BP were reached in stage N3 [31]. Some physiological mechanisms could explain the lower activity of THM and LF in stage N3. In general, the reduction in BP during NREM is mainly caused by baroreflex resetting and generalized cardiovascular deactivation regulated by central commands that may involve neurons in the hypothalamus, pons, and midbrain [32]. For instance, noradrenergic neurons in the locus coeruleus, dopaminergic neurons in the ventral tegmental area, or hypothalamic orexinergic neurons are less active during SWS (N3 in humans) and participate in BP regulation.
Additionally, some central neural circuits could be involved, such as a circuit through which GABAergic neurons from the parafacial area of the medulla oblongata can trigger SWS [33]. These neurons of the parafacial zone inhibit the parabrachial nucleus (PBN) [34]. The lateral parabrachial nucleus (LPBN) plays a role in the regulation of cardiovascular function since its stimulation causes an increase in blood pressure, sympathetic nervous activity, and tachycardia [35]. Another circuit involves neurons in the ventrolateral preoptic area (VLPO) that participate in the induction and maintenance of SWS. The VLPO sends GABAergic projections to the LPBN, and it has been proposed that reduced activity of PBN neurons may disinhibit the baroreflex at the level of the nucleus of the tractus solitarius. The VLPO also projects to the hypothalamic paraventricular nucleus (PVN) which contains neurons that regulate sympathetic outflow and BP [32].
Thus, NREM sleep is not a uniform state regarding LF and THM metrics, so the combination of stages N2 and N3 should be done according to the type of HRV metrics used. Among the limitations of this study is the small sample size, so future studies with increased samples sizes should be performed that also include measures of BP and other measures associated with baroreceptor activity to better characterize stages N2 and N3.
References
Bernston GG, Bigger JJ, Eckberg DL, Grossman P, Kaufmann PG, Malik M, Nagaraja HN, Porges SW, Saul JP, Stone PH, van der Molen MW. Heart rate variability: origins, methods, and interpretive caveats. Psychophysiology. 1997;34(6):623–48.
Lanfranchi PA, Pépin J, Somers VK. Cardiovascular physiology: autonomic control in health and in sleep disorders. In: Kryger MH, Roth T, Dement WC, editors. Principles and practice of sleep medicine. Philadelphia: Elsevier; 2017. p. 142–54.
Stein PK, Pu Y. Heart rate variability, sleep and sleep disorders. Sleep Med Rev. 2012;16(1):47–66.
Rechtschaffen A, Kales A. A manual of standardized terminology, techniques and scoring system for sleep stages of human subjects. Los Angeles: BI/BR; 1968.
Iber C, Ancoli-Israel S, Chesson AL, Quan SF. The AASM manual for the scoring of sleep and associated events: rules, terminology and technical specifications. Illinois: American Academy of Sleep Medicine; 2007.
Brandenberger G, Ehrhart J, Piquard F, Simon C. Inverse coupling between ultradian oscillations in delta wave activity and heart rate variability during sleep. Clin Neurophysiol. 2001;112(6):992–6.
Scholz UJ, Bianchi AM, Cerutti S, Kubicki S. Vegetative background of sleep: spectral analysis of the heart rate variability. Physiol Behav. 1997;62(5):1037–43.
Trinder J, Kleiman J, Carrington M, Smith S, Breen S, Tan N, Kim Y. Autonomic activity during human sleep as a function of time and sleep stage. J Sleep Res. 2001;10(4):253–64.
Burgess HJ, Penev PD, Schneider R, Van Cauter E. Estimating cardiac autonomic activity during sleep: impedance cardiography, spectral analysis, and Poincaré plots. Clin Neurophysiol. 2004;115(1):19–28.
Kuo TB, Chen CY, Hsu YC, Yang CC. EEG beta power and heart rate variability describe the association between cortical and autonomic arousals across sleep. Auton Neurosci. 2016;194:32–7.
Versace F, Mozzato M, De Min TG, Cavallero C, Stegagno L. Heart rate variability during sleep as a function of the sleep cycle. Biol Psychol. 2003;63(2):149–62.
Ako M, Kawara T, Uchida S, Miyazaki S, Nishihara K, Mukai J, Hirao K, Ako J, Okubo Y. Correlation between electroencephalography and heart rate variability during sleep. Psychiat Clin Neuros. 2003;57(1):59–65.
Bonnet MH, Arand DL. Heart rate variability: sleep stage, time of night, and arousal influences. Electroencephalogr Clin Neurophysiol. 1997;102(5):390–6.
Iellamo F, Placidi F, Marciani MG, Romigi A, Tombini M, Aquilani S, Massaro M, Galante A, Legramante JM. Baroreflex buffering of sympathetic activation during sleep: evidence from autonomic assessment of sleep macroarchitecture and microarchitecture. Hypertension. 2004;43(4):814–9.
Mendez MO, Bianchi AM, Villiantieri OP, Cerutti S, Penzel T. Time-variant spectral analysis of the heart rate variability during sleep in healthy and obstructive sleep apnoea subjects. Comput Cardiol. 2006;33:741–4.
Cabiddu R, Cerutti S, Viardot G, Werner S, Bianchi AM. Modulation of the sympatho-vagal balance during sleep: frequency domain study of heart rate variability and respiration. Front Physiol. 2012;3:45.
Vaughn BV, Quint SR, Messenheimer JA, Robertson KR. Heart period variability in sleep. Electroencephalogr Clin Neurophysiol. 1995;94(3):155–62.
Werner GG, Ford BQ, Mauss IB, Schabus M, Blechert J, Wilhelm FH. High cardiac vagal control is related to better subjective and objective sleep quality. Biol Psychol. 2015;106:79–85.
Boudreau P, Yeh WH, Dumont GA, Boivin DB. Circadian variation of heart rate variability across sleep stages. Sleep. 2013;36(12):1919–28.
Glos M, Fietze I, Blau A, Baumann G, Penzel T. Cardiac autonomic modulation and sleepiness: physiological consequence of sleep deprivation due to 40 h of prolonged wakefunlness. Physiol Behav. 2014;125:45–53.
Zhang L, Wu H, Zhang X, Wei X, Hou F, Ma Y. Sleep heart rate variability assists the automatic prediction of long-term cardiovascular outcomes. Sleep Med. 2020;67:217–24.
Allen JJB, Chambers AS, Towers DN. The many metrics of cardiac chronotropy: a pragmatic primer and a brief comparison of metrics. Biol Psychol. 2007;74(2):243–62.
Tarvainen MP, Niskanen JP, Lipponen JA, Ranta-aho PO, Karjalainen PA. Kubios HRV—heart rate variability analysis software. Comput Methods Programs Biomed. 2014;113(1):210–20.
Porges SW, Bohrer RE. Analyses of periodic processes in psychophysiological research. In: Cacioppo JT, Tassinary LG, editors. Principles of psychophysiology: physical, social, and inferential elements. New York: Cambridge University Press; 1990. p. 708–53.
De Geus EJC, Gianaros PJ, Brindle RC, Jennings JR, Berntson GG. Should heart rate variability be “corrected” for heart rate? Biological, quantitative, and interpretative considerations. Psychophysiology. 2019;56:e13287.
Carskadon MA, Dement WC. Normal human sleep: an overview. In: Kryger MH, Roth T, Dement WC, editors. Principles and practice of sleep medicine. Philadelphia: Elsevier; 2017. p. 15–24.
Reyes del Paso G, Langewitz W, Mulder LJM, Van Roon A, Duschek S. The utility of low frequency heart rate variability as an index of sympathetic cardiac tone: a review with emphasis on a reanalysis of previous studies. Psychophysiology. 2013;50:477–87.
Goldstein DS, Bentho O, Park MY, Sharabi Y. LF power of heart rate variability is not a measure of cardiac sympathetic tone but may be a measure of modulation of cardiac autonomic outflows by baroreflex. Exp Physiol. 2011;96(12):1255–61.
Burr RL. Interpretation of normalized spectral heart rate variability indices in sleep research: a critical review. Sleep. 2007;30(7):913–9.
Burgess HL, Trinder J, Kim Y, Luke D. Sleep and circadian influences on cardiac autonomic nervous system activity. Am J Physiol. 1997;273:1761–8.
Murali NS, Svatikova A, Somers VK. Cardiovascular physiology and sleep. Front Biosci. 2003;8:s636–52.
Silvani A, Dampney RA. Central control of cardiovascular function during sleep. Am J Physiol Heart Circ Physiol. 2013;305:H1683–92.
Anaclet C, Ferrari L, Arrigoni E, Bass CE, Saper CB, Lu J, Fuller PM. The GABAergic parafacial zone is a medullary slow wave sleep promoting center. Nat Neurosci. 2014;17(9):1217–24.
Anaclet C, Fuller PM. Brainstem regulation of slow-wave-sleep. Curr Opin Neurobiol. 2017;44:139–43.
Davern PJ. A role for the lateral parabrachial nucleus in cardiovascular function and fluid homeostasis. Front Physiol. 2014;5:436.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This research was conducted with human participants.
Informed consent
Informed consent was obtained from all participants in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Mateos-Salgado, E.L., Ayala-Guerrero, F. Comparison of autonomic activity between N2 and N3 stages of NREM sleep: evaluation through heart rate variability metrics. Sleep Biol. Rhythms 19, 181–186 (2021). https://doi.org/10.1007/s41105-020-00305-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s41105-020-00305-6