Abstract
Immersion testing of medical implants is typically performed under non-loaded conditions to assess susceptibility of metal ion release from a device. However, many implants are subjected to repetitive forces in vivo, which may increase ion release into surrounding tissues. Therefore, the objective of this study was to determine whether fatigue loading of stents with different surface finishes accelerates nickel release. Nitinol stents with an electropolished (EP) oxide or blue oxide (BO) were assigned to the following groups: (1) static immersion without loading, (2) static fluid pressure and bend, (3) dynamic pressure on a static bend, and (4) dynamic bending with static pressure. Immersion fluid was collected periodically and analyzed for nickel concentration using ICP-MS. Results indicated nickel release under dynamic bending was greater by up to 280× for EP and 190× for BO finishes compared to all other groups (p < 0.02). Although not significant (p > 0.27), nickel release under dynamic pressure conditions was up to 50× higher compared to static groups. In addition, BO stents released up to 6× greater levels of nickel compared to EP stents for static immersion, dynamic pressure, and dynamic bending groups (p < 0.05). These findings highlight the impact of fatigue loading on uniform corrosion for different nitinol stent surfaces.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Medical implants such as cardiovascular stents can corrode over time resulting in a release of metal ions. The corrosion susceptibility of metallic implant materials, particularly nitinol, is dependent on surface finishing processes [1]. Nitinol’s protective oxide layer provides a protective barrier to corrosion and can be improved with surface finishing steps such as mechanical polishing, electropolishing, and passivation [2,3,4]. The FDA’s guidance document “Select Updates for Non-Clinical Engineering Tests and Recommended Labeling for Intravascular Stents and Associated Delivery Systems” recommends tests to assess corrosion resistance of stents. The initial test recommended in the guidance document is pitting corrosion testing per ASTM F2129 (Standard Test Method for Conducting Cyclic Potentiodynamic Polarization Measurements to Determine the Corrosion Susceptibility of Small Implant Devices). If the results meet pre-specified acceptance criteria and the implant is manufactured using established surface finishing processes then further testing may not be necessary. However, if results do not meet pre-specified acceptance criteria or the device is not manufactured using established surface finishing processes, nickel ion release testing is then recommended to assess the potential biological risks by comparing the amount of nickel released to an established or derived tolerable intake value that would not cause appreciable harm to patient health [5]. Although patient complications from corrosion are somewhat unclear, pre-clinical studies have shown that corrosion byproducts may cause neointimal growth and in-stent restenosis [6, 7]. Clinical studies have observed adverse events such as contact dermatitis, migraine headaches, bronchospasms, exertional dyspnea, and pericarditis [8,9,10,11,12,13,14]. In addition, nickel allergies in patients with cardiovascular nitinol implants have been widely reported [15,16,17,18,19,20].
Current nickel release testing is conducted in predominantly static conditions where the device is immersed in phosphate-buffered saline (PBS), which is sampled at periodic intervals to characterize the nickel release profile of the device. Previous static immersion studies have shown that surface treatments impact nickel release behavior. For example, polishing and/or passivation of nitinol wires was shown to reduce nickel release compared to untreated wires when immersed in different solutions (e.g., PBS, cell culture media) for up to 6 months [21,22,23,24,25]. In fact, electropolished nitinol was shown to have similar nickel release to stainless steels and cobalt-based alloys [26]. Other immersion studies in wires and stents found increased nickel release with thicker oxides and nickel-rich phases within the oxide [1, 27, 28]. Although immersion in static conditions provides a simple, repeatable in vitro method, stents are subjected to repetitive mechanical forces in vivo. These mechanical loads may negatively affect the oxide layer and thus increase metal ion release. For example, the protective oxide layer may crack under applied strains, creating a conduit for increased nickel release in vivo. However, there is a paucity of data on the effects of mechanical loading on corrosion resistance in nitinol. A previous study found that application of a monotonic 3% bending strain cracked thick oxides resulting in lower breakdown potentials in potentiodynamic polarization testing [4]. Another study showed that radial compression of stents with thick thermal oxides to 7% maximum strain significantly increased nickel release compared to their non-crimped counterparts [27]. In addition, unpublished work showed that nitinol braided-wire devices with thermal oxides had a factor of five increase in nickel release compared to its passivated counterpart after 10 million cycles of crush fatigue. Although this study suggests that the magnitude of nickel leaching is dependent on the quality of the oxide layer, it remains unclear whether static immersion of devices may underestimate the amount of nickel released for devices that are subjected to loading. This is important as in vitro nickel release results are used in assessing biocompatibility of the device. Therefore, objectives of this study were to (1) determine whether fatigue testing of laser-cut nitinol stents accelerates nickel release in vitro and (2) investigate whether surface finishing of laser-cut nitinol stents impacts nickel release under dynamic loading.
Methods
Study Design and Stent Characterization
Nitinol stents used in this study were 3.0 mm diameter × 14 mm length (approximately 1.0 cm2 surface area). Stents were assigned to the following test conditions: (1) static immersion without loading, (2) static fluid pressure on a static bend, (3) dynamic fluid pressure on a static bend, and (4) static pressure with dynamic bending. To determine the effects of surface finishing, stents were manufactured with either a blue thermal oxide (BO) or electropolished (EP) passivated oxide (Fig. 1). Surface oxide composition and thickness were characterized using Auger Electron Spectroscopy (Evans Analytical Group, Sunnyvale, CA) by alternating an acquisition cycle with a sputter cycle. A random spot on the outer diameter surface of one stent from each processing group was chosen for analysis. The oxide layer thickness was determined based on the Full Width at Half Maximum (FWHM) method.
Immersion Testing
Silicone mock vessels were inspected for uniformity, inner diameter (ID), wall thickness, and vessel compliance prior to testing. Vessels were filled with 10% nitric acid solution (HNO3), flushed, and rinsed with ultrapure distilled water to ensure that vessels were free of nickel. All stents were deployed into these mock vessels, immersed in 1 ml of PBS, and incubated at 37 ± 2 °C for the duration of the study. The stent surface area-to-PBS volume ratio (1 cm2/mL) is within the range recommended for nickel in FDA’s guidance document “Select Updates for Non-Clinical Engineering Tests and Recommended Labeling for Intravascular Stents and Associated Delivery Systems” and ISO 10993-15 “Biological Evaluation of Medical Devices—Part 15: Identification and Quantification of Degradation Products from Metals and Alloys.”
Stents in the first experimental group (static immersion–no loading) were immersed without mock vessels at atmospheric pressure conditions (n = 3–4 per processing group) (Fig. 2). Another static immersion group consisted of stents (n = 5 per processing group) placed into U-shaped silicone vessels (3.0 mm nominal ID, 3–5% compliance) to obtain a static 15 mm radius of curvature (ROC) and subjected to 120 mmHg of static pressure provided by a pressure regulator (static bend group). A dynamic experimental group (dynamic pressure) consisted of pulsatile fatigue in a static bend (15 mm ROC) testing using a stent graft tester (Bose ElectroForce® 9120). Stents were deployed into high-purity U-shaped silicone vessels (3.0 mm nominal ID, 3–5% compliance). Dynamic pressure at 30 Hz was applied to the vessel OD at radial strains simulating pressures of 80 and 160 mmHg at physiological rates for 80 million cycles (n = 5 per processing group). A static pressure was applied to the vessel ID during testing to prevent the vessels from buckling under the dynamic pressure during testing. Another fatigue group (dynamic bend) was conducted using an axial mechanical testing system (Bose ElectroForce® 3200). Stents (n = 5 per processing group) were deployed into high-purity “Omega”-shaped silicone vessels (3.0 mm nominal ID, 3–5% compliance). Stents were dynamically bent at 15 Hz from 15 to 30 mm ROC for 40 million cycles and were verified to be within 2 mm ROC by dimensional analysis using high-speed video. These stented vessels were also subjected to 120 mmHg of static pressure provided by an external pressure regulator.
Media Extractions
Immersion fluid was collected and replaced with 1 ml of fresh PBS at day 1, 2, 3, 4, 8, 16, and 32. All instruments and containers used for extraction were rinsed with a 10% nitric acid solution to ensure that these items were free of nickel. At the designated extraction time points, vessels were depressurized and ultrapure distilled water was added if evaporation occurred in order to bring the media volume back to the original 1 ml volume. Extracted media was placed into pre-weighed 15 mL conical tubes and refrigerated. Over 200 total samples were analyzed in this study. Two samples could not be analyzed due to insufficient volume for analysis from PBS leakage out of the container.
Nickel Quantification
Nickel concentration in the PBS solutions was analyzed using inductively coupled plasma mass spectrometer (ICP-MS) (Thermo X-Series II). Samples were diluted by adding equal volume of 4% nitric acid solution before analysis to ensure that any nickel adsorbed onto the PBS salts would dissolve back into solution. The ICP-MS was tuned prior to analysis using 1 ppb Tune A solution (Thermo Fisher) in order to meet the required performance specifications. A calibration curve was prepared using nickel standard solutions (Spex CertiPrep) ranging from 0–1000 ng/mL, and 2% nitric acid was used as the rinse solution. A 50 ng/mL internal standard solution (VHG, contains Bi, Ga, In, Sc, Tb, and Y) was introduced through a T-connector along with the samples to correct for signal drift and matrix effects. PBS blanks possessed Ni values below 0.5 ppb.
Nickel recovery was verified with immediate, static, and dynamic spike and recovery tests (n = 5/group). Immediate spike and recovery consisted of adding 1 ml of PBS with 150 ppb from a NIST traceable standard solution (10 μg/mL Ni in 2% HNO3) into a straight silicone tubing and immediately recovered. For the static spike and recovery, 1 ml of PBS with 150 ppb from a NIST traceable standard solution was carefully pipetted into straight silicone tubing. The samples were incubated at 37 °C for 16 days (longest sampling interval for the study). At the end of 16 days, the solution was carefully removed from the silicone tubing, preserved with 2% nitric acid, and analyzed for nickel concentration using ICP-MS. For the dynamic spike and recovery test, 1 ml of 150 ppb nickel solution was pipetted into “Omega” silicone tubes (dynamic bending group) and mounted on the mechanical testing system. Samples were subjected to dynamic bending (15–30 mm ROC at 15 Hz) and a static 120 mmHg pressure regulator for 16 days. In order to counteract evaporation over the 16-day interval, media was diluted with ultrapure distilled water to the original volume immediately prior to the extraction, PBS samples were extracted from tubing, preserved with 2% nitric acid, and analyzed for nickel concentration using ICP-MS.
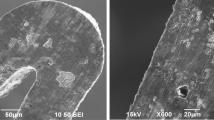
Scanning Electron Microscopy
After immersion, each stent was removed from silicone tubing and the entire length of each stent was inspected using scanning electron microscopy (SEM) (JEOL JSM-6390LV and FEI Quanta 200F). The abluminal (outer surface of stent), laser-cut side wall, and luminal (inner surface of the stent) surfaces of stents were inspected for corrosion and other alterations to the surface (e.g., cracks) and compared to non-tested stents (baseline). In addition, the inner surfaces of the silicone tubing were examined to determine whether alterations to tubing occurred as a result of interaction with the stent during mechanical testing.
Statistics
Three samples (EP stents in static bend group for day 8 and EP stents in dynamic bend for day 1 and 32) were determined to be statistical outliers using the Thompson Tau outlier test. Analysis of Variance (ANOVA) was performed to compare nickel release between groups within EP or BO stent groups. In addition, Student T tests were used to assess differences between surface finishing groups for each test condition. All data are presented as mean ± standard deviation. p values less than 0.05 were considered significant.
Results
Stent Characterization
The electropolished stent surface possessed a distinctly different composition and chemistry compared to the blue oxide stent surface (Fig. 3). The EP stent had a thin oxide layer (7 nm) without any nickel-rich regions evident. In contrast, the BO stent surface oxide was thicker (95 nm) with a nickel-rich sublayer. Both stent groups had a small concentration of nickel (1–2%) present on the surface. Visual inspection using SEM showed that surfaces were mostly smooth with typical manufacturing features (e.g., surface oxide stringers) observed in control EP and BO stents (Fig. 4). No signs of pitting, damage, or cracks were observed in any of the control stents analyzed.
Nickel Release
Nickel spike with immediate recovery yielded 148 ± 16 ppb. Recovery after 16 days of incubation was lower for the static spike and recovery testing (138 ± 4 ppb) compared to immediate recovery. Nickel recovery was higher and more variable for dynamic spike and recovery (176 ± 38 ppb) compared to immediate and static nickel recovery.
Nickel release was significantly higher (p < 0.02) for dynamic bending compared to all other groups at every time point for EP stents and after day 1 for BO (Fig. 5). Nickel release was not different (p > 0.27) between dynamic pressure and static conditions (immersion and bend groups). There were also no differences in nickel release between static immersion and static bend groups for either EP or BO surfaces (p > 0.53). In addition, dynamic bending of EP and BO stents resulted in significantly higher nickel release (p < 0.02) at 2.5, 5, 10, 20, and 40 million cycles compared to dynamic pressure loading (Fig. 6).
For the static immersion condition, cumulative nickel release was significantly higher (p < 0.02) for BO stents compared to EP stents (Fig. 7a). Cumulative nickel release was below 150 ng for both stent groups over the 32-day immersion duration. Interestingly, cumulative nickel release was significantly greater (p < 0.01) for EP stents compared to BO stents after day 3 for static bending and pressure loading condition (Fig. 7b). Total nickel concentrations were typically below 300 ng over the 32-day immersion duration. For dynamic pressure loading, cumulative nickel release was significantly greater (p < 0.05) for BO compared to EP stents after day 4 (Fig. 7c). For dynamic bending loading, cumulative nickel release was significantly greater (p < 0.05) for BO stents compared to EP stents after day 3 (Fig. 7d).
Visual Analysis
Both EP and BO stents under static immersion displayed similar morphology to their respective non-tested control stents (images not shown). EP and BO stents under static pressure and bend conditions had smooth consistent surfaces and also appeared similar to their non-tested control stents (Fig. 8). EP stent surfaces under dynamic pressure loading were similar to static conditions and non-tested stents (Fig. 9). In contrast, BO stents under dynamic pressure loading displayed possessed areas with dimpled surfaces and cracks at the intrados post-testing. Similarly, cracks were observed in the intrados of BO stent struts, but not on EP stents after dynamic bending (Fig. 10). Interestingly, surface abrasion was noted particularly at the strut apices for both EP and BO stents (Fig. 10). SEM imaging of the silicone vessel reveals that dynamic bending displayed damage (e.g., wear/fretting) of silicone vessel post-testing in both EP and BO groups, which were absent from static pressure/bend and dynamic pressure conditions (Fig. 11).
Representative SEM images of electropolished (EP) and blue oxide (BO) stent surfaces post-test for the static pressure with dynamic bend group. Surface abrasion was observed in EP and BO stent groups (yellow arrows). In addition, BO stent surfaces possessed dimpled surfaces and cracks at the intrados (Color figure online)
Representative SEM images of silicone vessels post-test for the (left) static pressure and bend pressure, (center) dynamic pressure with static bend, and (right) static pressure with dynamic bending groups. Vessels in dynamic bending group displayed fretting damage in both electropolished (EP) and blue oxide (BO) stent processing groups
Discussion
Immersion testing is performed by device manufacturers to assess the propensity of a medical implant to release metal ions. In fact, these results are frequently used as part of a biocompatibility risk assessment where the cumulative nickel release and rate of nickel release from the device are compared to a tolerable intake values for that metal. Therefore, it is important that in vitro immersion testing accurately estimates levels of metal ion release that may occur in vivo. Although static immersion testing simulates several critical factors (e.g., pH, temperature), one key factor not simulated is the mechanical environment that implants such as stents are subjected to in vivo. This is the first study to investigate whether cyclic strains experienced by cardiovascular stents in vivo increase the potential for uniform corrosion. The results indicate that fatigue loading substantially increases nickel release in nitinol stents with thin passivated oxide and moderately thick thermal oxide. In fact, nickel release for EP stents under dynamic pressure loading had up to a 50× increase compared to static immersion and up to 28× compared to static pressure and bend conditions over the testing duration. Furthermore, nickel release for EP stents under dynamic bending had up to a 280× increase compared to static immersion and up to 19× compared to static pressure and bend conditions. Similarly, nickel release for BO stents under dynamic pressure loading had up to a 36× increase compared to static immersion and up to 41× compared to static pressure and bend conditions. Under dynamic bending, nickel release for BO stents was up to 170× higher compared to static immersion and up to 190× compared to static pressure and bend conditions over the course of the study. These results highlight the impact of mechanical loading on increased nickel release and may be an important factor in patients with nickel allergies. Currently, there are no definitive tolerable intake values for nickel-based implants. The US Pharmacopeia suggests a Permissible Daily Exposure (PDE) for nickel as a metallic impurity in drug products to be 0.5 µg/kg/day. For a 70 kg person, the PDE would be 35 µg/day. This PDE is substantially greater than the highest rate of nickel release (1 μg/day) for stents under dynamic bending conditions. Although nickel release was below the PDE, this PDE is intended to be protective for only systemic effects and therefore the threshold for local adverse biological effects may be lower. In addition, the size of the stent used in this study (3 mm × 14 mm) was intended for coronary applications and testing duration was only for up to 80 million cycles. Testing of larger stents (e.g., superficial femoral artery) or testing of multiple stents (e.g., overlapped condition) may result in nickel release rates closer to the reported PDE.
Comparisons between surface finishes demonstrated that BO stents released more nickel compared to EP stents for static immersion, dynamic pressure, and dynamic bending groups. It was somewhat expected that BO stents would release more nickel compared to EP stents as our results are in good agreement with a previous study that investigated the effects of surface processing on nickel release in static immersion conditions [27]. In fact, AF stents (blue color in appearance) in the previous study had a similar increase (~ 6×) in cumulative nickel release compared to EP stents as blue oxide stents in this study after approximately 32 days of immersion. However, it was unexpected that a relative increase in nickel release did not occur with fatigue loading for BO stents (2.4 × and 3.8 × increase in dynamic bending and dynamic pressure groups, respectively). For dynamic pressure loading (Fig. 7c), the cumulative nickel release rate (i.e., slope of curve from days 16 to 32) for BO stents is higher (50 ng/day) compared to EP stents (8 ng/day). Over longer testing times, we expect that BO stents would have higher relative rates of nickel release compared to EP surfaces. The same trend, however, was not observed in dynamic bending conditions. A confounding factor in this group is that the high nickel release in dynamic bending was likely due to fretting between stent and silicone vessel (Figs. 10 and 11). This testing artifact may have dominated the nickel release in both surface processing groups and thus prevented comparisons of the relative differences between EP and BO groups.
There are some important limitations that must be considered when interpreting the results of this study. We found that dynamic bending resulted in significantly greater nickel release than pulsatile loading for both EP and BO stents. The loading magnitudes for both groups were chosen were based on typical values reported in literature; however, direct comparisons are difficult as the local mean and alternating strains on the struts were not known between loading modes. Although this study determined that loading modes and magnitudes are important factors in nickel release rates, more studies are needed to comprehensively determine the effects of loading on nickel release. We recommend that further studies be conducted to investigate multiple loading levels for a particular loading mode. In addition, finite element analysis simulations can complement experimental testing and further elucidate the interplay between local mechanics and nickel release. Another limitation is the effect of testing frequency on nickel release was not investigated. Acceleration of frequency may impact nickel release that may not be observed at physiological rates (e.g., 1.2 Hz for blood pulsations). Therefore, we recommend additional research to determine the impact of testing frequency on nickel release. Finally, dynamic spike and recovery testing showed that 117% nickel was recovered on average. The higher nickel concentration suggests that nickel contamination may have occurred from potential sources such as silicone tubing or testing equipment. Although the relative comparisons between groups in our study are likely unaffected, the absolute nickel concentration may be overestimated by up to 20%. This is important when comparing nickel concentrations to reported tolerable intake values for biocompatibility assessments. Identification and elimination of sources of metal ion contamination is critical for nickel release studies that incorporate dynamic loading of devices.
In conclusion, dynamic pulsatile loading accelerated nickel release by up to 50 × in vitro compared to typical static immersion conditions and may be an important factor in accurately simulate nickel release levels in vivo. In addition, surface finishing was another key factor in immersion testing as blue oxide stents released greater levels of nickel compared to electropolished stents for static and dynamic loading groups. Although the nickel levels reported from fatigue testing are substantially lower than previously reported tolerable nickel intake for adults, larger devices and longer testing durations may have a negative biological effect, particularly on devices with thick thermal oxides. Nickel ion release during fatigue testing in this study provided initial insight into the impact of dynamic mechanical loading on uniform corrosion in nitinol stents, but is also technically challenging and further studies are needed to develop best practices for this more complicated test method.
References
Decker JF, Trepanier C, Vien L, Pelton AR (2011) The Effect of material removal on the corrosion resistance and biocompatibility of nitinol laser-cut and wire-form products. J Mater Eng Perform 20(4–5):802–806
Trepanier C, Tabrizian M, Yahia L, Bilodeau L, Piron D (1996) Improvement of the corrosion resistance of NiTi stents by surface treatments. MRS Proceedings, Cambridge Univ Press, Cambridge, p. 363
Trepanier C, Tabrizian M, Yahia LH, Bilodeau L, Piron DL (1998) Effect of modification of oxide layer on NiTi stent corrosion resistance. J Biomed Mater Res 43(4):433–440
Zhu L, Trepanier C, Pelton A, Fino JM (2003) Oxidation of nitinol and its effect on corrosion resistance, ASM Materials and Processes for Medical Devices Conference, ASM Publication, Materials Park
Saylor DM, Craven BA, Chandrasekar V, Simon DD, Brown RP, Sussman EM (2018) Predicting patient exposure to nickel released from cardiovascular devices using multi-scale modeling. Acta Biomater 70:304–314
Santin M, Mikhalovska L, Lloyd AW, Mikhalovsky S, Sigfrid L, Denyer SP, Field SN, Teer D (2004) In vitro host response assessment of biomaterials for cardiovascular stent manufacture. J Mater Sci 15(4):473–477
Wataha JC, O’Dell NL, Singh BB, Ghazi M, Whitford GM, Lockwood PE (2001) Relating nickel-induced tissue inflammation to nickel release in vivo. J Biomed Mater Res 58(5):537–544
Lai DW, Saver JL, Araujo JA, Reidl M, Tobis J (2005) Pericarditis associated with nickel hypersensitivity to the Amplatzer occluder device: a case report. Catheter Cardiovasc Interv 66(3):424–426
Rigatelli G, Cardaioli P, Giordan M, Aggio S, Chinaglia M, Braggion G, Roncon L (2007) Nickel allergy in interatrial shunt device-based closure patients. Congenit Heart Dis 2(6):416–420
Gimenez-Arnau A, Riambau V, Serra-Baldrich E, Camarasa JG (2000) Metal-induced generalized pruriginous dermatitis and endovascular surgery. Contact Dermat 43(1):35–40
Slavin L, Tobis JM, Rangarajan K, Dao C, Krivokapich J, Liebeskind DS (2007) Five-year experience with percutaneous closure of patent foramen ovale. Am J Cardiol 99(9):1316–1320
Fukahara K, Minami K, Reiss N, Fassbender D, Koerfer R (2003) Systemic allergic reaction to the percutaneous patent foramen ovale occluder. J Thorac Cardiovasc Surg 125(1):213–214
Kim KH, Park JC, Yoon NS, Moon JY, Hong YJ, Park HW, Kim JH, Ahn Y, Jeong MH, Cho JG (2008) A case of allergic contact dermatitis following transcatheter closure of patent ductus arteriosus using Amplatzer ductal occluder. Int J Cardiol 127(2):e98–e99
Khodaverdian RA, Jones KW (2009) Metal allergy to Amplatzer occluder device presented as severe bronchospasm. Ann Thorac Surg 88(6):2021–2022
Jetty P, Jayaram S, Veinot J, Pratt M (2013) Superficial femoral artery nitinol stent in a patient with nickel allergy. J Vasc Surg 58(5):1388–1390
Köster R, Vieluf D, Kiehn M, Sommerauer M, Kähler J, Baldus S, Meinertz T, Hamm CW (2000) Nickel and molybdenum contact allergies in patients with coronary in-stent restenosis. Lancet 356(9245):1895–1897
Hillen U, Haude M, Erbel R, Goos M (2002) Evaluation of metal allergies in patients with coronary stents. Contact Dermat 47(6):353–356
Iijima R, Ikari Y, Amiya E, Tanimoto S, Nakazawa G, Kyono H, Hatori M, Miyazawa A, Nakayama T, Aoki J (2005) The impact of metallic allergy on stent implantation: metal allergy and recurrence of in-stent restenosis. Int J Cardiol 104(3):319–325
Romero-Brufau S, Best PJ, Holmes DR, Mathew V, Davis MD, Sandhu GS, Lennon RJ, Rihal CS, Gulati R (2012) Outcomes after coronary stent implantation in patients with metal allergy. Circulation 5(2):220–226
Rabkin DG, Whitehead KJ, Michaels AD, Powell DL, Karwande S (2009) Unusual presentation of nickel allergy requiring explantation of an Amplatzer atrial septal occluder device. Clin Cardiol 32(8):E55–E57
McLucas E, Rochev Y, Carroll WM, Smith TJ (2008) Analysis of the effects of surface treatments on nickel release from nitinol wires and their impact on candidate gene expression in endothelial cells. J Mater Sci Mater Med 19(3):975–980
Wever DJ, Veldhuizen AG, de Vries J, Busscher HJ, Uges DRA, van Horn JR (1998) Electrochemical and surface characterization of a nickel-titanium alloy. Biomaterials 19(7–9):761–769
Wu S, Chu PK, Liu X, Chung C, Ho J, Chu C, Tjong S, Yeung K, Lu W, Cheung K (2006) Surface characteristics, mechanical properties, and cytocompatibility of oxygen plasma-implanted porous nickel titanium shape memory alloy. J Biomed Mater Res, Part A 79(1):139–146
Pérez LM, Gracia-Villa L, Puértolas JA, Arruebo M, Irusta S, Santamaria J (2009) Effect of Nitinol surface treatments on its physico-chemical properties. J Biomed Mater Res, Part B 91(1):337–347
Cui Z, Man H, Yang X (2005) The corrosion and nickel release behavior of laser surface-melted NiTi shape memory alloy in Hanks’ solution. Surf Coat Technol 192(2):347–353
Thierry B, Tabrizian M, Trepanier C, Savadogo O, Yahia LH (2000) Effect of surface treatment and sterilization processes on the corrosion behavior of NiTi shape memory alloy. J Biomed Mater Res 51(4):685–693
Sullivan SL, Dreher M, Zheng J, Chen L, Madamba D, Miyashiro K, Trépanier C, Nagaraja S (2015) Effects of oxide layer composition and radial compression on nickel release in nitinol stents. Shape Mem Superelasticity 1(3):319–327
Clarke B, Carroll W, Rochev Y, Hynes M, Bradley D, Plumley D (2006) Influence of nitinol wire surface treatment on oxide thickness and composition and its subsequent effect on corrosion resistance and nickel ion release. J Biomed Mater Res, Part A 79(1):61–70
Acknowledgements
This study was made possible through research collaborative agreements between FDA and Medical Device Testing (now Element Materials Technology Corporation) and G. Rau Inc. The authors would like to thank FDA researchers Shiril Sivan and Stacey Sullivan for technical assistance and David Saylor for manuscript review. The authors would like to acknowledge the FDA White Oak Nanotechnology Core Facility for instrument use, scientific and technical assistance. The findings and conclusions in this paper have not been formally disseminated by the Food and Drug Administration, are the views of the authors, and should not be construed to represent any agency determination or policy. The mention of commercial products, their sources, or their use in connection with material reported herein is not to be construed as either an actual or implied endorsement of such products by Department of Health and Human Services.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Nagaraja, S., Chandrasekar, V., Ormonde, D. et al. The Impact of Fatigue Testing and Surface Processing on Nickel Release in Nitinol Stents. Shap. Mem. Superelasticity 4, 462–471 (2018). https://doi.org/10.1007/s40830-018-00196-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40830-018-00196-0