Abstract
Background
Cost limitations of commercial-grade ultrasound phantoms often prevent ultrasound education from being incorporated into medical curricula (Bahner et al., Acad Med. 89:1681–6, 2014). While production of homemade agar gelatin phantoms to offset costs has been well documented, use of ballistic gelatin has only recently been described (Domenico et al., J Ultrasound. 11 (4):135-42, 2008; Zerth et al., J Emerg Med. 43:1066-9, 2012; Chao et al., J Emerg Med. 45:240-3, 2013; Shobeiri et al., J Ultrasound Med. 32:1393-6, 2013; Woywodt et al., Clin Nephrol. 79:241-5, 2013; Zeiler et al., Can J Neurol Sci. 40:225-9, 2013; Hunt et al., Eur J Radiol. 82:594-600, 2013; Lo et al., Emerg Med J. 29:738-41, 2012; Li et al., J Ultrasound Med. 30:263-72, 2011; Morrow and Broder, J Emerg Med. 49 (3):313-7, 2015). There exists a critical need for learner evaluation of homemade ballistic gelatin phantoms (BGPs) and their comparison to commercial-grade phantoms to better inform BGP introduction into medical education. The primary aim of this study is to describe survey-based evaluation of homemade BGPs and commercial-grade Blue PhantomsTM by medical students. The secondary aim is to compare image quality of BGPs and Blue PhantomsTM.
Materials and Methods
Described are construction of BGPs and introduction in voluntary ultrasound training sessions offered to 61 first through fourth-year medical students. The evaluation and success of this model are reported.
Results
Students reported that versatility of homemade BGPs surpassed that of commercially available phantoms (4.52 ± 0.71) and that they felt more confident in their ultrasound skills after the session (4.82 ± 0.37). Side-by-side evaluation of images generated using BGPs and Blue PhantomsTM had comparable simulated vessel shape and echogenicity, adding objective assessment to subjective survey-based results.
Discussion
Training sessions were enabled by low-cost homemade BGPs at $4 vs $400+ cost of commercial-grade phantoms, a 100-fold reduction in cost.
Conclusion
As students found BGPs and Blue PhantomsTM comparable, the results of this study can equip other institutions struggling with costs of incorporating ultrasound into their medical curricula with not only a cost-effective solution but also a learner-validated one.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
In recent years, ultrasound has become more compact and more accessible. As a result, “point-of-care ultrasonography,” which refers to ultrasonography performed and interpreted by the clinician at the bedside, has become increasingly prevalent in medical practice. A seminal article published in the New England Journal of Medicine describes how point-of-care ultrasonography has successfully enhanced procedural guidance, diagnostic assessment, and screening [1]. In the emergency setting, bedside ultrasound evaluation of free fluid has resulted in reduced time to intervention, shorter hospital stay, lower costs, and lower overall mortality [2]. Additionally, the use of ultrasound to guide central venous access has been shown to reduce risk of complications and number of attempts [3]. Point-of-care ultrasonography has not only improved outcomes for patients but also has resulted in cost savings for hospitals. As hospital reimbursements trend toward bundled payments (payment based on episodes of care), point-of-care ultrasonography has lessened the burden of costly imaging performed by a consulting radiologist [4].
While bedside ultrasound is readily available and beneficial to patients, ultrasound remains a user-dependent technology heavily relying on human factor in data interpretation. As such, the increasing accessibility of ultrasound creates a critical need to ensure physician competence in ultrasound imaging. Integration of ultrasound education programs into medical school and residency curricula provides such an opportunity for exposure to this critical instruction at an early point in the careers of physicians. Responding to this need, the International Federation for Emergency Medicine (IFEM) recently convened a committee of international experts in emergency point-of-care ultrasound (PoCUS) to outline a curriculum for training specialists in emergency PoCUS, and the Society of Radiologists in Ultrasound and the Alliance of Medical School Educators in Radiology recently collaborated on the design of an ultrasound curriculum for medical students [5, 6]. Both organizations recommend the use of ultrasound phantoms for practice of procedures such as venous access. Furthermore, in 2000, the Residency Review Committee for Emergency Medicine announced the requirement for ultrasound training in emergency medicine residency programs [7].
The benefits of ultrasound instruction to trainees extend beyond familiarizing them with an increasingly available imaging modality. At higher levels of medical education, ultrasound phantoms have been used to teach clinicians invasive procedures such as fine-needle aspiration of lesions of the head and neck and diagnostic skills needed to identify pediatric skull fractures [8, 9]. In the emergency setting specifically, ultrasound phantoms have been used to teach identification of superficial soft tissue abscesses and for training in vascular access [10, 11].
Direct visualization of human anatomy by ultrasound is a powerful adjunct to the physical diagnosis in preclinical education. One study has shown that integration of ultrasound education into the physical diagnosis course of first-year medical students resulted in significant increases in Objective Standardized Clinical Examination (OSCE) scores, and a second study showed that ultrasound training as an adjunct to traditional means of teaching abdominal examination improved first-year medical student examination technique [12, 13]. A third study has shown that after focused ultrasound training, first-year medical students using point-of-care ultrasound were able to outperform board certified cardiologists in identifying cardiac abnormalities, identifying 75 vs 49 % of conditions identified by cardiologists [14–17].
Preclinical ultrasound education also enhances the teaching of gross anatomy. Implementation of an echocardiography training program in a first-year medical student cardiovascular gross anatomy curriculum resulted in increased accuracy of cardiovascular structure identification [18]. Likewise, introduction of ultrasound in the first-year medical student gross anatomy curriculum at another institution resulted in increased student practical examination scores on ultrasound images [19]. In another study, inclusion of an ultrasound elective course in the second year of one medical school has resulted in significant improvements in knowledge of musculoskeletal, abdominal, and cardiovascular anatomy as measured by pre- and post-course exams [20]. Several recent studies have also detailed the successful implementation of ultrasound training as part of the anatomy curriculum [14, 17, 21, 22].
While ultrasound education has clear benefits, ultrasound integration into medical curricula remains a challenge. A recent survey of curricular administrators in 134 medical schools revealed that 37.8 % of respondents reported that their institution did not integrate ultrasound training into their curriculum. Furthermore, although 78.9 % of respondents agreed or strongly agreed that ultrasound education should be integrated into the medical school curricula, they perceived lack of financial support as one of the most significant barriers to implementation [23]. One such financial barrier is the high cost of commercially available ultrasound phantoms, instruments used to teach clinical ultrasound technique by simulating sonographic appearance of human tissue. For example, the cost of Blue PhantomTM models ranges from $400 to $500 (Blue Phantom Corporation, Redmond, WA/Universal Medical, Inc. Norwood, MA).
At the author’s institution, the University of Alabama at Birmingham School of Medicine, an introductory lecture on ultrasound was incorporated into the first medical school module of the first academic year, Fundamentals 1. However, students struggled to understand image generation. This prompted the authors to explore feasibility of incorporating an ultrasound training course into their medical school curriculum. Due to large student class size of 186+ students, cost of commercial-grade phantoms was prohibitive. In an effort to offer the opportunity for ultrasound training to medical students, the authors sought a more cost-effective alternative.
In a key paper, Domenico et al. described the creation of a homemade agar gelatin model for the purpose of practicing ultrasound-guided vein catheterization at a cost of only $5.50 [24]. Since then, the production of low-cost homemade ultrasound phantoms to minimize costs associated with ultrasound training has been well documented in the literature with agar gelatin being the key material used; the other materials included polony, metamucil, gelatin, and chicken breasts [10, 25–34].
Although ballistic gelatin is a low-cost ammunition-testing medium designed to simulate the density and viscosity of animal soft tissue, Morrow and Broder have only recently reported its use as a material for creation of homemade ultrasound phantoms for use in the Duke University’s Emergency Medicine Residency Program [11]. A combination of ballistic gelatin and ripe clementines has also been used to specifically create anatomical prostate models for surgical skill workshops at the University of Toronto [35]. In contrast to agar, ballistic gelatin retains simulation properties without leaking even when exposed to warmer temperatures or repeated use [11]. Importantly, a recent report from Tanious et al., which assessed the characteristics of ballistic gelatin, found it to be superior over other forms of gelatin [36].
Morrow and Broder note that future studies of learner perceptions/satisfaction are needed to compare the ballistic gelatin model with other models [11]. The purpose of this study is two-fold, (1) to evaluate student perceptions of ballistic gelatin phantoms (BGPs) and the gold standard Blue PhantomsTM using survey-based assessment and (2) to compare image quality of BGPs and the gold standard Blue PhantomsTM.
Materials and Methods
Assembling Ballistic Gelatin Phantoms
A 10 % gelatin mixture was found to result in phantoms with the best consistency after testing varying concentrations of gelatin from 10 to 20 %. The authors found higher concentrations of gelatin difficult to bring into solution using a heated magnetic stir plate. In order to make 2 L of 10 % ballistic gelatin, the following steps were followed:
-
1.
Two hundred grams of Vyse professional grade ballistic gelatin (Gelatin Innovations Inc., Schiller Park, IL) was dissolved in 1.8 L of water for an end volume of 2 L).
-
2.
This mixture was heated to a boil using a heated magnetic stirrer and Teflon stir bar.
-
3.
As the mixture was brought to a boil, four drops of de-foamer (Gelatin Innovations Inc., Schiller Park, IL) were added to prevent excessive foaming.
-
4.
The heated magnetic stirrer was then turned off while allowing the Teflon stir bar to continue stirring in order to prevent congealing.
It should be noted that as an alternative to starting from ballistic gelatin powder, worn ballistic gelatin phantoms may be re-melted.
Once the resulting mixture cooled to a temperature perceived not to damage plastic “Tupperware-style” food storage containers, it was poured into plastic containers of varying shapes and sizes to create a “base layer” of gelatin. This “base layer” was allowed to set by placement in a chilled water bath. Then, a variety of objects such as rubber tubes mimicking blood vessels, water-filled balloons housing pebbles mimicking gallbladders, and mystery objects (screws, keys, and miniature plastic skeleton replicas) were placed on top. To complete the phantom, a second layer of gelatin was added to completely immerse the contained objects, and the gelatin was again allowed to set either by transfer to the anatomy laboratory’s cold room or placement in a chilled water bath. After the final gelatin layer had set, the now assembled BGPs were vacuum-sealed to extend shelf life (Sousvide Supreme VS3000, Broomfield, CO).
Blood vessels were simulated with rubber penrose drain tubing tied at the free ends and filled with water (Coviden LLC., Mansfield, MA). Penrose drain tubing was chosen as it had the best sonographic characteristics when compared to simulated vessels within Blue PhantomsTM. Another possibility is to fill the tubes with gelatin, which prevents water from leaking into the phantom after a needle puncture. To prevent the tubing from floating to the gelatin surface during the setting process, the tubing was affixed to the container walls with an adhesive tape. Fascial planes were simulated with strips of gauze placed either above or below other embedded objects. Gallbladders were simulated with water-filled balloons closed with twine. Gallstones were simulated with pebbles introduced into the balloon prior to closure.
Importantly, BGPs can be made either transparent or opaque with the addition of water-soluble food coloring. Transparent phantoms may be used for novice sonographers to familiarize themselves with the ultrasound device interface. Opaque phantoms effectively increase the difficulty of ultrasound interpretation by blinding the sonographer to structures housed within the phantom. Additionally, hollow structures such as vessels may be filled with dye to serve as an additional positive identifier for vessel penetration (and aspiration).
BGPs described here have a shelf life of 4–8 weeks if stored in a refrigerator or cold room. At room temperature, BGPs are stable for several hours without substantial softening or melting. If a phantom becomes damaged or worn, the gel can be simply re-melted in a microwave oven and reformed as new.
Ultrasound Training Sessions with Medical Students
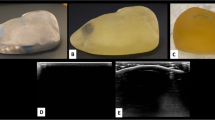
First- through fourth-year medical students were recruited via email to voluntarily participate in 1 of 15 ultrasound training sessions occurring at various times over the course of 1 month. Sessions consisted of an overview of basic ultrasound technique, probe handling, machine controls, and image interpretation as demonstrated by one of the authors. Volunteers then had the opportunity to practice ultrasonography independently scanning both types of phantoms (Blue PhantomsTM and ballistic gelatin phantoms) using either a simpler handheld scanner (Vscan, General Electric Company (GE), Fairfield, CT) or a more sophisticated scanner (Venue 40, General Electric Company (GE), Fairfield, CT). Both BGPs and Blue PhantomsTM were made available simultaneously during the training sessions so that half of students could begin their practice with BGPs and half with Blue PhantomsTM. After approximately 20 min of practice, students were instructed to switch to the second phantom type. Both phantoms are shown side-by-side in Fig. 1.
Survey Design
Permission to conduct the surveys was obtained from UAB’s Institutional Review Board. Two different survey instruments (pre-session and post-session questionnaire) consisting of seven and 19 items, respectively, were designed for this study Appendix A. Items in the pre-session questionnaire were designed to evaluate student expectations for the session as well as their opinion on the relative importance of ultrasound in medical practice.
After this practice session, students were asked to evaluate both homemade and commercial gel phantoms (Blue PhantomTM). The post-session survey asked students to compare the two phantoms and assessed student confidence in their ultrasonography skill Appendix A. All survey questions were rated on a five-point Likert scale, 1 strongly disagree to 5 strongly agree. All surveys were collected anonymously and no incentives were given to participating students.
Data Analysis
The authors developed the questionnaires used in this study in-house to best fit the needs of the specific ultrasound training sessions implemented at their home institution. As such, these survey instruments were not validated within this particular population. Statistical analyses were performed using SAS software v9.2 (SAS Institute, Cary, NC). Survey results are presented as mean scores with standard deviations. Cronbach’s alpha was performed to assess internal consistency of the pre-session questionnaire and the post-session questionnaire, respectively. A lower bound threshold was used for alpha (0.60), due to the small number of scale items in the pre-session questionnaire. An upper bound threshold was used for alpha of 0.90. Missing values were excluded from the analysis.
Results
Evaluating Student Perceptions of Ballistic Gelatin Phantoms and Gold Standard Blue PhantomsTM
Sixty-one students from all four years of medical school volunteered to participate in the study. The participating students were distributed as follows: 27 first-year, 9 second-year, 10 third-year, and 12 fourth-year students (Table 1). Three students did not identify their class year. The majority of students had little to no experience in ultrasound (Table 1). Only five students overall had used ultrasound training phantoms prior to this session, all in conjuncture with ultrasound activities in the school of medicine (led by author DR using homemade trainers). Gender distribution was not recorded, but the surveyors did not detect any bias toward male or female students.
Pre-session Questionnaire
Prior to the sessions, participating medical students believed knowing ultrasound would help enhance their communication skills with other medical professionals, give them an advantage in residency applications, and help them provide better patient care. The average responses to all questions were all rated greater than 4 on a five-point Likert scale. Students perceived being able to use an ultrasound device as a medical student to be important because they believed it will help them better communicate with colleagues (4.43 ± 0.83), give them an advantage over other applicants for residency programs (4.16 ± 0.97), help them provide better patient care (4.75 ± 0.47), and will be an important skill in general for their career (4.80 ± 0.44). By participating in the session, students hoped to better understand the nature of ultrasound artifacts (4.72 ± 0.58), the correlation of probe orientation and image acquired (4.82 ± 0.53), the functions of the ultrasound device, and how to quickly make adjustments and change scanning modes (4.75 ± 0.51). Results are shown in Table 2.
Post-Session Questionnaire
Students reported that they felt more confident in their ultrasound scanning skills after the session (4.82 ± 0.37). Being able to view structures within the homemade phantoms (commercial phantoms were opaque) was an important feature that helped students understand how the 2-D image differs from the 3-D image (4.77 ± 0.63), understand how to better position the ultrasound probe (4.82 ± 0.43), and understand how to interpret ultrasound images (4.71 ± 0.53).
The second portion of the post-session questionnaire focused specifically on the homemade gelatin phantoms. Students reported that the dimensions of the phantoms were appropriate for practice (4.66 ± 0.55), the phantom’s consistency felt realistic (4.43 ± 0.76), and the phantom was very versatile (4.50 ± 0.74). Structures inside the phantom had similar echogenicity (appearance on the ultrasound screen) to real anatomical structures (4.61 ± 0.65). Students also felt that this phantom type should be available for ad libitum training outside of this practice session for interested students (4.84 ± 0.42). With regard to ultrasound training, students felt that using the gel phantom helped them make the mental connection between the structures inside the gel and the image on the screen (4.80 ± 0.44), helped them understand and reconstruct image artifacts that arise during normal ultrasound scanning (4.55 ± 0.69), and overall, helped them be more confident in probe manipulation and image acquisition (4.80 ± 0.44).
Students did not perceive extra effort required to assemble homemade phantoms as an inconvenience that made the phantoms less attractive (2.73 ± 1.42) (to the opposite statement, that having to make phantoms is an inconvenience that makes them less attractive) and did perceive low cost and ease of manufacturing as appealing (4.89 ± 0.37). In fact, students reported that the versatility and range of applications of homemade phantoms actually surpassed that of commercially available phantoms (4.52 ± 0.71), and critically that overall, the homemade phantoms surpassed the utility of the commercial phantoms (4.20 ± 0.82). Interestingly, students slightly preferred using a handheld scanner in conjunction with the homemade phantoms (4.43 ± 0.81) as opposed to the commercial phantoms (4.05 ± 1.03). Students also agreed that the handheld Vscan units were of value (4.05 ± 1.07). Results are shown in Table 3.
Cronbach’s alphas for the seven-item pre-session questionnaire and for the 19-item post-session questionnaire were 0.60 and 0.76, respectively.
Comparing Image Quality of Ballistic Gelatin Phantoms and Gold Standard Blue PhantomsTM
To illustrate ultrasound image quality of the homemade BGPs as compared with commercial Blue PhantomsTM, an image obtained using both a homemade ballistic gelatin phantom and an image obtained using a commercial Blue PhantomTM are shown side-by-side in Fig. 2. This image depicts an ultrasound-guided vessel puncture acquired with a Venue 40 and high frequency probe. As can be seen from the image, simulated vessel shape and echogenicity are comparable.
Discussion
Phantom Evaluation
One reason this descriptive study was conducted was for students previously unexposed to ultrasound, not professionals, to compare homemade and commercial phantoms. As an additional consideration, two types of scanners in two different price brackets were used—the relatively affordable handheld Vscan (∼$7000) and more expensive Venue 40 ($ ≥ 25,000)—to identify if scanning device type had an impact on results.
After practicing newly learned ultrasound technique using both homemade BGPs and commercial-grade Blue PhantomsTM, students reported that the versatility and range of applications of homemade phantoms surpassed that of commercially available phantoms (4.52 ± 0.71) and that overall, the homemade phantoms surpassed the utility of the commercial phantoms (4.20 ± 1.22). Importantly, students reported that they felt more confident in their ultrasound scanning skills after the session (4.82 ± 0.37). Additionally, students did not perceive extra effort required to assemble homemade phantoms as an inconvenience that made the phantoms less attractive (2.73 ± 1.42) and did perceive low cost and ease of manufacturing as appealing (4.89 ± 0.37).
The major drawback of these results is high standard deviation, especially with standard deviations for responses to post-session questionnaires ranging from 0.37 to 1.42. Standard deviations for pre-session questionnaire responses showed less variability ranging from 0.44 to 0.97. But certainly, these results suggest that ballistic gelatin phantoms are an effective tool for introducing the novice learner to ultrasonography, and that ballistic gelatin phantoms are at least comparable to if not superior to Blue PhantomsTM.
It is also important to mention that although perceived confidence in ultrasound scanning skills was improved after these sessions, perception may not correlate with actual understanding related to anatomy and examination. In a similarly designed ultrasound training sessions of five to six first- and second-year medical students utilizing in vivo imaging, investigators found that although 2-h session of in vivo training on abdominal anatomy increased student confidence in anatomical knowledge (70 % reported increased confidence), this did not translate to increased skill or understanding related to abdominal anatomy on written exams [37]. However, student retention of hands-on ultrasound skills has been shown to improve on practical exam after between one to three ultrasound training sessions [38, 39]. Thus, it is possible that short-term ultrasound training does not enhance anatomy knowledge retention but does increase hands-on ultrasound skill. The numerous benefits of longitudinal ultrasound education in medical school, including increases in medical knowledge, have been well documented [12–17, 19, 20, 40, 41]. Importantly, concerns related to curricular design would be valid with either type of ultrasound trainer, homemade BGP or commercial-grade Blue PhantomTM.
One explanation for student preference for ballistic gelatin phantoms over opaque Blue PhantomsTM is ballistic gelatin phantom translucency. This is supported by the survey data. Students asserted the ability to view structures within the homemade phantoms “was an important feature that helped students understand how the 2-D image differs from the 3-D image” (4.77 ± 0.63), “understand how to better position the ultrasound probe” (4.82 ± 0.43), and “understand how to interpret ultrasound images” (4.71 ± 0.53). Ballistic gelatin phantom translucency may also explain student preference for handheld Vscan in conjunction with homemade phantoms (4.43 ± 0.81) as opposed to commercial phantoms (4.05 ± 1.03).
Translucent homemade ballistic gelatin phantoms are likely a superior introductory training tool to commercially available Blue PhantomsTM for first-time ultrasound learners, as phantom translucency may enhance initial orientation and “mental rotation” of the 3-D image on the 2-D screen. Supporting this conclusion, Morrow and Broder comment that emergency medicine residents who had not previously performed any ultrasound-guided procedure were better able to re-orient when practicing with homemade translucent BGPs [11]. Additionally, although written comments were not solicited from session participants, four medical students opted to write a comment on their questionnaire. Three of the comments spoke to the benefits of homemade phantoms and one comment noted one limitation of VScans. One student wrote the following comment on his or her survey: “The homemade is best to start out on so you can see the structures. But the commercial is great for testing yourself after you get the orientation down.” The authors recognize that students who chose to comment may have been self-selecting and therefore, a potentially biased group. However, this comment may add insight to student preference for BGPs. It is important to note that homemade ballistic gelatin phantoms can easily be made opaque with the addition of water-soluble food coloring or other suitable dye. Thus, they may also be used for training of more advanced ultrasound learners. BGP applications in training learners at different levels of proficiency are an important area for future study.
To supplement the subjective evaluation of the BGPs with objective data, the authors compared image quality of vessel puncture using both types of phantoms and a Venue 40 using a high frequency probe. Side-by-side images are shown in Fig. 2. Simulated vessel shape and echogenicity are comparable further supporting homemade BGPs as a valid training tool for ultrasound education.
While images generated using the two types of phantoms are comparable, several important considerations exist when choosing to use homemade ballistic gelatin phantoms or commercial phantoms. These considerations are cost, potential for re-use, and shelf life. Compared to commercial phantoms such as Blue PhantomTM retailing between $400 and 500, the cost for the homemade BGPs described here is estimated at $4.00 with individual materials as follows: $1 Tupperware (reusable), penrose drain $1.31, and 200 g ballistic gel $0.70 (12.5 kg = $315 makes up to 125 kg of gel, 113 g de-foamer $21.18 is sufficient for 12.5 kg of gel). This represents a 100-fold reduction in cost making homemade phantoms more accessible. It is also important to note that ballistic gelatin may be re-used over and over again if damaged or worn brining down the cost even further. Commercial phantoms such as Blue PhantomTM cannot be re-melted if damaged.
While cost is an advantage of homemade BGPs, shelf life is an advantage of commercial phantoms. Ballistic gelatin phantoms have a shelf life of 4–8 weeks if refrigerated, while commercial phantoms have an indefinite shelf life and do not require any special storage or refrigeration. As noted by Morrow and Broder and replicated in this study, each needle approach through the homemade BGP leaves a small artifact visible on ultrasound that is not present in commercial phantoms such as Blue PhantomTM [11]. However, such artifacts are easily repaired by heating the homemade ballistic gelatin phantom with a hair dryer on high for 30–60 s.
Instructors must carefully consider factors of cost, potential for re-use, and shelf life when selecting ultrasound phantoms for their institution. Future studies could include objective student performance on medical school exams as a marker to further inform the comparison between BGPs and Blue PhantomsTM.
Limitations
It should be critically noted that only a minority of invited students chose to volunteer. Therefore, potential for selection bias to influence the study is significant. The recruitment email for the survey was sent out to all 750 students in first- through fourth-years, of which 80 third- and fourth-year students would have been unable to attend the sessions in Birmingham due to campus assignments in Huntsville or Tuscaloosa. Thus, total sample pool was 670, from which 61 students chose to participate in the study. The authors deem it likely that volunteering students had a greater enthusiasm for ultrasound education than others, which decreases general objectivity, but nevertheless still is representative of the subgroup of ultrasound enthusiasts.
The same groups of students were used to evaluate both types of phantoms in each ultrasound training session. This approach was selected due to limited numbers of student volunteers and limited instructor availability. It should be noted that comparing opinions of well-matched but independent groups of students may have produced more valid comparisons.
Regarding student evaluation of phantom types, the survey instrument was developed by the authors and was a subjective assessment that has not been validated in studies outside the authors’ institution. Pre- and post-session questionnaires were administered with the same question order to all students. And, as only the authors had sufficient knowledge of both anatomy and ultrasonography to conduct ultrasound training session as well as sufficient time to devote to such training, author participation in student training sessions could potentially have introduced bias into the results. Finally, due to obvious differences in appearance of BGPs and Blue PhantomsTM, students were not blinded to which phantom was homemade and which was commercially available. However, these limitations are in part offset by the objective use of side-by-side images to validate homemade phantoms against a control, the gold standard in phantom ultrasonography, Blue PhantomTM. The comparison shows that images produced by ballistic gelatin homemade phantoms are comparable to those produced by Blue PhantomsTM.
Related to practical aspects of using handheld Vscan units with homemade phantoms, those seeking to recreate homemade ballistic gelatin phantoms detailed in this study for use with handheld Vscan units must embed structures to a sufficient depth (>6 cm). The handheld VScan system is not designed for superficial structures, and 6 cm is the minimum depth that can be set by the Vscan units. One student’s written comment pointed to this limitation: “The Vscan would probably benefit from having a deeper phantom to work with. The ones used today were a little shallow.”
Conclusions
As students found ballistic gelatin phantoms and Blue PhantomsTM comparable, the results of this study can equip other institutions struggling with costs of incorporating ultrasound into their medical curriculum with not only a cost-effective solution but also a learner-validated one. Ballistic gelatin phantoms are a cost-effective, comparable training tool to commercial phantoms (Blue PhantomTM) that are easily incorporated into medical education as described. Cost, potential for re-use, and shelf life are all key considerations when choosing between homemade ballistic gelatin phantoms or commercially available phantoms for use in ultrasound education. Due to the 100-fold advantage in cost, positive learner perception, and versatility of homemade ballistic gelatin phantoms, the authors believe homemade ballistic gelatin phantoms are a viable and even perhaps superior alternative to commercially available models.
References
Moore CL, Copel JA. Point-of-care ultrasonography. N Engl J Med. 2011;364:749–57.
Melniker LA et al. Randomized controlled clinical trial of point-of-care, limited ultrasonography for trauma in the emergency department: the first sonography outcomes assessment program trial. Ann Emerg Med. 2006;48(3):227–35.
Hind D et al. Ultrasonic locating devices for central venous cannulation: meta-analysis. BMJ. 2003;327(7411):361.
Schoen C, Guterman S, Shih A, Lau J, Kasimow S, Gauthier A, Davis K. Bending the curve: options for achieving savings and improving value in US health spending. Washington, DC; 2007:114.
Atkinson P et al. International Federation for Emergency Medicine point of care ultrasound curriculum. CJEM. 2015;17(2):161–70.
Baltarowich OH et al. National ultrasound curriculum for medical students. Ultrasound Q. 2014;30(1):13–9.
Straus B. Chairman of Residency Review Committee for Emergency Medicine. Speech to the Council of Residency Directors for Emergency Medicine (CORD), Atlanta 2000.
Richardson C, Bernard S, Dinh VA. A cost-effective, gelatin-based phantom model for learning ultrasound-guided fine-needle aspiration procedures of the head and neck. J Ultrasound Med. 2015;34(8):1479–84.
Soucy ZP et al. Creation of a high-fidelity, low-cost pediatric skull fracture ultrasound phantom. J Ultrasound Med. 2015;34(8):1473–8.
Lo MD, Ackley SH, Solari P. Homemade ultrasound phantom for teaching identification of superficial soft tissue abscess. Emerg Med J. 2012;29:738–41.
Morrow DS, Broder J. Cost-effective, reusable, leak-resistant ultrasound-guided vascular access trainer. J Emerg Med. 2015;49(3):313–7.
Dinh VA, Frederick J, Bartos R, Shankel TM, Werner L. Effects of ultrasound implementation on physical examination learning and teaching during the first year of medical education. J Ultrasound Med. 2015;34:43–50.
Butter J et al. Does ultrasound training boost year 1 medical student competence and confidence when learning abdominal examination. Med Educ. 2007;41(9):2007.
Canty DJ et al. Ultrasound simulator-assisted teaching of cardiac anatomy to preclinical anatomy students: a pilot randomized trial of a three-hour learning exposure. Anat Sci Educ. 2015;8(1):21–30.
Kobal SL et al. Comparison of effectiveness of hand-carried ultrasound to bedside cardiovascular physical examination. Am J Cardiol. 2005;96(7):1002–6.
Swamy M, Searle RF. Anatomy teaching with portable ultrasound to medical students. BMC Med Educ. 2012;12:99.
Brown B et al. Introduction of ultrasound into gross anatomy curriculum: perceptions of medical students. J Emerg Med. 2012;43(6):1098–102.
Wittich CM et al. Teaching cardiovascular anatomy to medical students by using a handheld ultrasound device. JAMA. 2002;288(9):1062–3.
Dreher SM, Dephilip R, Bahner D. Ultrasound exposure during gross anatomy. J Emerg Med. 2014;46:231–40.
Kondrashov P, Johnson JC, Boehm K, Rice D, Kondrashova T. Impact of the clinical ultrasound elective course on retention of anatomical knowledge by second-year medical students in preparation for board exams. Clin Anat. 2015;28:156–63.
Moscova M et al. Integration of medical imaging including ultrasound into a new clinical anatomy curriculum. Anat Sci Educ. 2015;8(3):205–20.
Jurjus RA et al. Can anatomists teach living anatomy using ultrasound as a teaching tool. Anat Sci Educ. 2014;7(5):340–9.
Bahner DP, Goldman E, Way D, Royall NA, Liu YT. The state of ultrasound education in U.S. medical schools: results of a national survey. Acad Med. 2014;89:1681–6.
Domenico S et al. Introducing ultrasound-guided vein catheterization into clinical practice: a step-by-step guide for organizing a hands-on training program with inexpensive handmade models. J Ultrasound. 2008;11(4):135–42.
Zerth H, Harwood R, Tommaso L, Girzadas Jr DV. An inexpensive, easily constructed, reusable task trainer for simulating ultrasound-guided pericardiocentesis. J Emerg Med. 2012;43:1066–9.
Chao SL, Chen KC, Lin LW, Wang TL, Chong CF. Ultrasound phantoms made of gelatin covered with hydrocolloid skin dressing. J Emerg Med. 2013;45:240–3.
Shobeiri SA, Rostaminia G, Shobeiri H. Development of an in-house endoanal ultrasound teaching phantom. J Ultrasound Med. 2013;32:1393–6.
Woywodt A, How T, Schulz M. A purpose-built simulator for percutaneous ultrasound-guided renal biopsy. Clin Nephrol. 2013;79:241–5.
Zeiler FA, Unger B, Kramer AH, Kirkpatrick AW, Gillman LM. A unique model for ultrasound assessment of optic nerve sheath diameter. Can J Neurol Sci. 2013;40:225–9.
Hunt A, Ristolainen A, Ross P, Opik R, Krumme A, Kruusmaa M. Low cost anatomically realistic renal biopsy phantoms for interventional radiology trainees. Eur J Radiol. 2013;82:594–600.
Li JW, Karmakar MK, Li X, Kwok WH, Ngan Kee WD. Gelatin-agar lumbosacral spine phantom: a simple model for learning the basic skills required to perform real-time sonographically guided central neuraxial blocks. J Ultrasound Med. 2011;30:263–72.
Wells A, Goldstein L. The polony phantom: a cost-effective aid for teaching emergency ultrasound procedures. Int J Emerg Med. 2010;3(2):115–8.
Kendall JL, Faragher JP. Ultrasound-guided central venous access: a homemade phantom for simulation. CJEM. 2007;9(5):371–3.
Rippey JC, Blanco P, Carr PJ. An affordable and easily constructed model for training in ultrasound-guided vascular access. J Vasc Access. 2015;16:422–7.
Lawrentschuk N, Linder U, Klotz L. Realistic anatomical prostate models for surgical skills workshops using ballistic gelatin for nerve-sparing prostatectomy and fruit for simple prostatectomy. Korean J Urol. 2011;52(2):130–5.
Tanious SF, Cline J, Cavin J, Davidson N, Coleman JK, Goodmurphy CW. Shooting with sound: optimizing an affordable ballistic gelatin recipe in a graded ultrasound phantom education program. J Ultrasound Med. 2015;34:1011–8.
Sweetman GM et al. The benefits and limitations of using ultrasonography to supplement anatomical understanding. Anat Sci Educ. 2013;6(3):141–8.
Yoo MC, Villegas L, Jones DB. Basic ultrasound curriculum for medical students: validation of content and phantom. J Laparoendosc Adv Surg Tech A. 2004;14(6):374–9.
Tshibwabwa ET, Groves HM. Integration of ultrasound in the education programme in anatomy. Med Educ. 2005;39(11):1148.
Arger PH et al. Teaching medical students diagnostic sonography. J Ultrasound Med. 2005;24(10):1365–9.
Syperda VA et al. Ultrasonography in preclinical education: a pilot study. J Am Osteopath Assoc. 2008;108(10):601–5.
Acknowledgments
This project was conducted at the UAB School of Medicine and would not have been possible without the generous support of Dr. Etty (Tika) Benveniste, Professor and Chairman of the Department of Cell, Developmental and Integrative Biology (CDIB). The authors also extend their gratitude to Alex Boles, Financial Officer CDIB for his support in acquisition and allocation of the supplies necessary for this project.
Author information
Authors and Affiliations
Corresponding author
Appendix A
Appendix A
Pre-session Questionnaire
-
1.
Have you ever used an ultrasound phantom before this session, and if so, name the type of phantom _________.
YES/NO
-
2.
Being able to use an ultrasound device already as a medical student is important because:
-
a.
It is an important skill for my career as the technique is becoming more widespread.
1-2-3-4-5
-
b.
It will help me provide better patient care.
1-2-3-4-5
-
c.
I will have an advantage over other applicants for residency programs because few medical schools train their students in ultrasound.
1-2-3-4-5
-
d.
It will help me better communicate with my colleagues.
1-2-3-4-5
-
a.
-
3.
By participating in this practice session with ultrasound phantoms, I hope to:
-
a.
Understand how to use the ultrasound device, its functions, and how to quickly make adjustments and change scanning modes, e.g., color Doppler
1-2-3-4-5
-
b.
Understand the correlation of probe orientation and image acquired, to predict the change in acquired image when the probe is rotated around its long axis, tilted, yawed, pitched, etc.
1-2-3-4-5
-
c.
Better understand the nature of ultrasound artifacts such as acoustic shadowing, reflections, mirror images, etc.
1-2-3-4-5
-
a.
Post-Session Questionnaire
-
1.
I feel more confident in my ultrasound scanning skills, having participated in this training session.
1-2-3-4-5
-
2.
Being able to view the structures that are being imaged within the phantom is a very important feature and it helped me understand:
-
i.
How better to interpret ultrasound images.
1-2-3-4-5
-
ii.
How better to position the ultrasound probe to obtain an accurate image.
1-2-3-4-5
-
iii.
How the 2-D ultrasound image differs from the 3-D image of a structure.
1-2-3-4-5
-
i.
-
3.
Having to make phantoms versus buying ready-made phantoms is an inconvenience that makes them less attractive.
1-2-3-4-5
-
4.
The low cost and ease of manufacturing of these phantoms makes them more accessible.
1-2-3-4-5
-
5.
The versatility of the homemade phantoms makes their range of application surpass that of the commercially available phantoms.
1-2-3-4-5
-
6.
The dimensions of the phantoms are appropriate for practice.
1-2-3-4-5
-
7.
The phantom’s consistency feels realistic.
1-2-3-4-5
-
8.
Structures inside the phantom have a similar echogenicity (appearance on the ultrasound screen) as real anatomical structures (as far as I can tell).
1-2-3-4-5
-
9.
This phantom type should be available for ad libitum training outside of this practice session for interested students.
1-2-3-4-5
-
10.
Using this type of phantom really helps me make the mental connection between the structures inside the gel and the image on the screen.
1-2-3-4-5
-
11.
Training on this phantom makes me more confident in probe manipulation and image acquisition.
1-2-3-4-5
-
12.
This phantom is very versatile.
1-2-3-4-5
-
13.
This phantom helps the trainee understand and reconstruct image artifacts that arise during normal ultrasound scanning.
1-2-3-4-5
-
14.
Overall, the homemade phantoms surpass the utility of the commercial phantoms.
1-2-3-4-5
-
15.
Using a handheld scanner in conjunction with a homemade phantom enabled me to acquire decent images and understand and correlate probe position with the image acquired.
1-2-3-4-5
-
16.
Using a handheld scanner in conjunction with a commercial phantom enabled me to acquire decent images and understand and correlate probe position with the image acquired.
1-2-3-4-5
-
17.
I was able to image structures (even if with less resolution/clarity) in either phantom using only a handheld scanner (Vscan) versus a more sophisticated ultrasound scanner (Venue 40). In other words, for basic training and object recognition the Vscan units are of value.
1-2-3-4-5
Rights and permissions
About this article
Cite this article
Makeeva, V., Gullett, J.P., Dowla, S. et al. Evaluation of Homemade Ballistic Gelatin Phantoms as a Low-Cost Alternative to Commercial-Grade Phantoms in Medical Education. Med.Sci.Educ. 26, 307–316 (2016). https://doi.org/10.1007/s40670-016-0258-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40670-016-0258-3