Abstract
Background
The choice of the specific modality and treatment duration of renal replacement therapy (RRT) to adopt in metformin-associated lactic acidosis (MALA) is still debated. We aimed to verify if sustained low-efficiency dialysis (SLED) is a rational choice in patients with MALA and acute kidney injury (AKI).
Methods
We collected serial serum metformin measurements, clinical parameters, and outcome data in ten consecutive patients (mean age 77 years [range 58–88], 5 males) admitted to our renal intensive care unit for suspected MALA associated with AKI and hemodynamic instability. Patients underwent a 16-h SLED session performed with either conventional dialysis machines or machines for continuous RRT (CRRT). A 2-compartment open-infusion pharmacokinetic model with first-order elimination was fitted to each subject’s serum concentration–time data to model post-SLED rebound and predict the need for further treatments.
Results
Two patients died within 24 h after SLED start. Three patients needed one further dialysis session. Surviving patients (n = 8) were dialysis-free at discharge. Metformin levels were in the toxic range at baseline (median [range] 32.5 mg/l [13.6–75.6]) and decreased rapidly by the end of SLED (8.1 mg/l [4.5–15.8], p < 0.001 vs. baseline), without differences according to the dialysis machine used (p = 0.84). We observed a slight 4-h post-SLED rebound (9.7 mg/l [3.5–22.0]), which could be predicted by our pharmacokinetic model. Accordingly, we predicted that the majority of patients would need one additional dialysis session performed the following day to restore safe metformin levels.
Conclusions
A 16-h SLED session, performed with either conventional dialysis machines or CRRT machines, allows effective metformin removal in patients with MALA and AKI. However, due to possible post-SLED rebound in serum metformin levels, one additional dialysis treatment is required the following day in the majority of patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Metformin is recommended as first-line treatment in patients with a new diagnosis of type-2 diabetes mellitus (T2DM) [1, 2] as it is effective, inexpensive, has a low risk of hypoglycemia, and may reduce the risk of cardiovascular events [3]. A rare but dangerous side effect of metformin treatment is lactic acidosis (LA), usually observed with inappropriate dose prescriptions in the presence of coexistent risk factors, in particular chronic kidney disease (CKD) [4]. Metformin-associated lactic acidosis (MALA) bears a high mortality risk, especially when diagnosis and/or treatment are missed or delayed [5]. No specific antidote is available to reverse the toxic effects of metformin, and initial treatment for MALA relies on emergency resuscitation and supportive care.
Renal replacement therapy (RRT) is considered the most effective and efficient treatment option in the case of metformin intoxication, as it allows simultaneous drug removal and correction of acidosis [6, 7]. However, no conclusive indications are currently available concerning the timing, modality, or duration of RRT [7]. In fact, while conventional intermittent hemodialysis (IHD) could be regarded as first choice because of its high efficiency in terms of drug removal and acid-base correction, continuous RRT (CRRT) may be preferable in the presence of hemodynamic instability. In critically ill patients with acute kidney injury (AKI), prolonged intermittent RRT modalities such as sustained low-efficiency dialysis (SLED) have been proposed as an adequate compromise between conventional IHD and CRRT because they allow both greater hemodynamic stability compared to IHD and higher depurative efficiency compared to CRRT [8,9,10].
Here we present a case series of ten patients, including one recently reported [11], who had AKI and were treated with SLED due to a strong clinical suspicion of MALA. The diagnosis of severe MALA was confirmed subsequently in all patients by measurement of serum drug levels. Based on a pharmacokinetic analysis of serum metformin removal during SLED, we focus on the effectiveness of an early treatment with this RRT modality in patients strongly suspected of having MALA.
Materials and methods
Patients
We studied 10 patients (mean age 77 years [range 58–88], 5 males) with T2DM on metformin treatment consecutively admitted between January 1st 2016 and October 31st 2017 to the Renal Intensive Care Unit (RICU) of the Parma University Hospital, with AKI and suspected MALA based on the criteria of Lalau et al. [4]. All patients received emergency treatment according to the local institutional protocol for suspected metformin intoxication and AKI. Written informed consent to participate in the study was obtained from the patients when possible or from their closest relatives when available, and the study protocol was in conformity with the Declaration of Helsinki. The Ethics Committee of Parma University Hospital (Comitato Etico per Parma) approved the study (Protocol No. 46489).
SLED technique
All patients received supportive treatment and therapy focused on the coexistent medical problems. Within 1–2 h from admission patients began a 16-h SLED session with regional citrate anticoagulation. Two different dialysis machines were used, according to their availability in the RICU. Five patients were treated with AK 200 ultra machines (Gambro/Baxter Italy, Rome, Italy) with 1.8 m2 polysulfone F8 HPS filters (Fresenius Medical Care, Cremona, Italy); blood flow rate was 200 ml/min, dialysis fluid rate 300 ml/min, countercurrent flow direction, dialysis fluid bicarbonate concentration 32 mmol/l. Citrate anticoagulation was performed using anticoagulant citrate dextrose solution A (ACD-A), citrate concentration 112.9 mmol/l (SALF SpA, Laboratorio Farmacologico, Cenate Sotto, BG, Italy) infused at 300 ml/h in the extracorporeal circulation, as previously described [10]. Five patients were treated with Prismaflex machines (Baxter Italy) with 1.5 m2 AN69 ST150 filters; blood flow rate was 200 ml/min, dialysis fluid rate 100 ml/min, countercurrent flow direction, dialysis fluid bicarbonate concentration 32 mmol/l. Citrate anticoagulation was performed using ACD-A solution, with the infusion rate being automatically set by the dialysis machine to maintain a target plasma pre-filter citrate concentration of 3 mmol/l. The use of a specific dialysis machine for each patient was at the discretion of the attending nephrologist.
As per institutional routine, in cases of suspected MALA, blood samples were collected at SLED start, at 8 h and at the end of SLED, as well as 1 and 4 h thereafter. In 2 patients, blood samples were also obtained at 2 and 4 h following SLED start, as well as at 8 and 16 h after SLED end. Blood samples were stored at 4 °C and were subsequently sent to an external institution (Toxicology Unit, Istituti Clinici Scientifici Maugeri Spa-SB, IRCCS Pavia Hospital and University of Pavia, Pavia, Italy) for the measurement of serum metformin concentrations by high-performance liquid chromatography-tandem mass spectrometry [12]. Demographic and clinical data, hemodynamic parameters, and the most relevant acid-base and electrolyte-related variables were recorded in the patients’ clinical charts.
Statistical analysis
The time course of serum metformin concentrations during the SLED session and the 8 h following were analyzed by linear mixed models for repeated measures with time and type of dialysis machine as fixed factors and baseline serum metformin levels as a covariate. p < 0.05 was regarded as statistically significant. Stata release 15 software (2017 StataCorp, College Station, TX, USA) was used for the analyses.
Pharmacokinetic analysis
Pharmacokinetic analysis was conducted using Adapt 5 computer software packages (Biomedical Simulations Resource, University of Southern California, Los Angeles, CA, USA) [13].
Differential equations (Eqs. 1 and 2) describing a 2-compartment open-infusion pharmacokinetic model with first-order elimination were fit to each subject’s metformin serum concentration–time data:
where Xc is the amount of metformin in the central compartment, Xp the amount of metformin in the peripheral compartment, Vc the apparent volume of distribution in the central compartment, Vp the apparent volume of distribution in the peripheral compartment, and Cld the distribution clearance between the central and peripheral compartment; Cls is the systemic clearance, ClHD the dialytic clearance and R is an indicator variable that has the value of 0 during the interdialytic period and a value of 1 during dialysis.
Equation 1 shows that the amount of metformin in the central compartment (Xc) increases, per unit time, by the fraction Cld/Vp of Xp (i.e. the amount of metformin in the peripheral compartment) due to the distributional clearance (Cld) from the peripheral to the central compartment, whilst it decreases by the fraction (Cls/Vc + Cld/Vc) of the amount of metformin in the central compartment due to systemic clearance (Cls, equal to renal clearance, assumed to be negligible in AKI) and distributional clearance from the central to the peripheral compartment; and by the fraction ClHD/Vc of the amount of metformin in the central compartment removed by dialytic clearance (ClHD).
Equation 2 shows that the amount of metformin in the peripheral compartment (Xp) increases, per unit time, by the fraction Cld/Vc of Xc due to the distributional clearance from the central to the peripheral compartment, and decreases by the fraction Cld/Vp of Xp due to the distributional clearance from the peripheral to the central compartment.
It should be noted that central (Vc) and peripheral (Vp) compartments are merely mathematical parameters predicting drug concentration, rather physical entities. In fact, Vc is the volume of distribution predicted by the pharmacokinetic model at a hypothetical t = 0, that explains the initial serum metformin concentration; Vp, that allows for the change in slope of the declining part of the time-concentration curve, accounts for several biochemical phenomena, namely drug penetration in peripheral tissues, variable intracellular drug-protein binding, and drug elimination.
Rebound of metformin after the end of dialysis was described solely by redistribution from the peripheral compartment. Volumes of distribution were assumed to be constant during the entire study period. Metformin systemic clearance (Cls) and ClHD were assumed to occur from the central compartment only. Pharmacokinetic parameter estimates obtained by this model were Vc, Vp, Cld, ClHD.
Interdialytic and intradialytic periods were fit simultaneously. Because the data available were not sufficient to estimate the amount of metformin accumulated in the body in each patient at the time of SLED start, we decided to make the following assumption. We assumed that the quantity of metformin accumulated in the body of each patient at the time of SLED start was equal to the initial metformin concentration times 276 l (the metformin volume of distribution estimated by Tucker et al. [14] based on a one-compartment model) and that the central volume of distribution (Vc) was half the peripheral volume of distribution (Vc). These assumptions allowed to generate starting values for fitting population models using the Standard Two-Stage (STS) Adapt 5 option, in which individual data were fitted by maximum likelihood (ML) with additive and proportional residual errors.
We predicted the effect of additional once-daily SLED sessions on metformin levels after rebound by performing a population simulation (n = 1000) with output noise using estimated mean and variance–covariance matrix of the parameters from the fitted pharmacokinetic model. Based on the same model, we additionally evaluated the impact on the need for further dialysis sessions of partial recovery of kidney function occurring 24 h from the start of the first SLED session vs. the absence of recovery.
Results
Patients’ condition at admission to the RICU
The median Acute Physiology and Chronic Health Evaluation II (APACHE II) score was 30 (range 27–34), with a calculated 71% (range 58–81) mortality risk. The median metformin daily dose was 2550 mg (range 2000–3000 mg). Six patients had CKD: median estimated glomerular filtration rate (eGFR) 44 ml/min/1.73 m2, range 31–59 (Table 1). All patients were oligoanuric. AKI was attributable to one or more acute comorbidities or precipitating clinical conditions (acute bleeding in one patient, acute coronary syndrome in 2 patients, sepsis and septic shock in 7 patients, concomitant acute stroke in 2 patients). All patients were hypotensive at presentation (median [range] systolic/diastolic blood pressure values: 86 [75–91]/49 [42–61] mmHg), and 7 out of 10 required vasoactive support with norepinephrine (infusion rate range 0.10–0.63 mcg/kg/min); in one case inotropic support with dopamine was also needed. Three patients required noninvasive mechanical ventilation. Initial laboratory workup showed severe anion gap metabolic acidosis with hyperlactatemia (median, [range]: pH 7.08 [6.75–7.22], HCO3− 5.5 mmol/l [2–12]; lactic acid 15.9 mmol/l, [11.1–31.7]; anion gap 36.5 [29–52]). Urine toxicology tests were unremarkable. Other routine laboratory values at baseline are summarized in Table S1 in the Online Resource.
Clinical course and acid-base status during and after SLED
All but one patient showed a gradual improvement in blood pressure; in 6 out of 7 patients norepinephrine was rapidly tapered and eventually discontinued by, or within a few hours following, the end of SLED. One patient needed a progressive increase of vasoactive support and emergency intubation during SLED because of rapid deterioration of the hemodynamic and respiratory status. Acid-base parameters and lactate levels were improved at the end of SLED in 9 out of 10 patients (Table 2).
Two patients (20%) died in the RICU within 24 h of SLED start. Urine output rapidly increased to at least 1 l/day within 96 h after SLED in 7 out of the 8 surviving patients (Table S2 in the Online Resource); in 3 out of 8 one further RRT session (1 SLED in 2 patients, 1 conventional IHD in 1 patient) was performed. All patients were dialysis-free at hospital discharge. The median length of stay in the RICU was 10 days (range 1–21), and the median length of hospital stay was 19 days (range 1–49).
Serum metformin kinetics during and after the SLED session
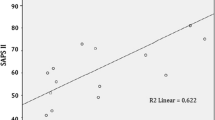
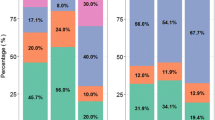
At SLED start serum metformin levels were in the toxic range in all patients (median 32.5 mg/l, range 13.6–75.6; reference value < 2.0 mg/l), and in the potentially lethal range (≥ 50 mg/l) in 4 patients. Serum metformin concentrations decreased rapidly after the first 8 h of treatment (p < 0.001 vs. baseline), and reached a median value of 8.1 mg/l (4.5–15.8) at the end of SLED; the drug reduction ratio ranged between 54.4 and 85.8% (median 78.5). A slight rebound in metformin levels was observed in the majority of patients at 4 h (median 9.7 mg/l; 3.5–22.0) from the end of SLED, which could be predicted by a two-compartment pharmacokinetic model with first-order elimination (Fig. 1; the parameter estimates of the model are reported in the figure legend). Serum metformin levels were not significantly different (p = 0.84) among the patients treated with the two dialysis machines, nor was there a significant interaction (p = 0.90) between time and type of dialysis machine.
Measured metformin levels (hollow circles) and time-concentration curves fitted by the 2-compartment model with first-order elimination (solid lines) in each patient. The dotted vertical line represents the end of the 16-h SLED session. Median metformin clearance during SLED (CLHD) was 12.7 l/h (range 0.1–34.3); median central volume of distribution (Vc), 92.0 l (range 88.4-105.2); median distributional clearance (CLd), 3.2 l/h (range 0.1–30.1); median peripheral volume of distribution (Vp), 230 l (range 1.5–1135). The mean additive (σinter) and proportional (σslope) residual error was 0.39 and 0.05, respectively
In order to predict the need of an additional once-daily 16-h SLED session to correct metformin levels after rebound we performed a population pharmacokinetic simulation, the results of which are reported in Fig. 2. The simulation showed that one additional SLED session performed the following day could easily correct metformin levels in the vast majority of patients, especially in those with early recovery of kidney function (Fig. 2).
Population simulation study of 1000 patients undergoing four once-daily 16-h SLED sessions (shadowed vertical rectangles) in the absence of recovery of kidney function (white boxes), and in the presence of partial recovery of kidney function 24 h after the start of the first SLED session (grey boxes; + 10 l/h increase in systemic clearance CLs). The dotted lines represent 5 mg/l, a safety threshold for serum metformin levels. The simulation is based on the fitted parameters and variances from a 2-compartment population pharmacokinetic model with first-order elimination reported in Fig. 1. The prediction is dependent on the assumptions on the amount of drug accumulated at the time of SLED start. It should therefore not be overinterpreted: it is intended simply to give a visual representation of the rate of change of metformin concentration, the extent of post-SLED rebound, and of the between-subject heterogeneity
Discussion
In the present case series of ten patients with ascertained MALA, treatment with SLED allowed rapid metformin removal, efficient correction of typical acid-base disorders, and improved hemodynamic stability. Also, clinical outcomes were more favorable than those generally reported for patients with MALA treated with different RRT modalities [7]. Although a 16-h SLED session was followed by a slight metformin rebound, a single dialysis session performed the following day could easily restore safe serum metformin levels.
Because metformin blocks the glycerophosphate shuttle via inhibition of the mitochondrial enzyme alpha-glycerophosphate dehydrogenase, it decreases the mitochondrial redox state and increases the cytosolic redox state; thus, the conversion of lactate to pyruvate in the cytosol is decreased [15]. Furthermore, lactate accumulation is also increased due to the inhibition of mitochondrial respiratory chain complex I in peripheral tissues, including liver and skeletal muscle [15, 16]. Hence, notwithstanding a low reported incidence (i.e. less than 10 events/100,000 patient-years of exposure) lactic acidosis can develop as a serious complication of metformin treatment when lactate clearance is reduced [5, 11, 17].
Metformin clearance is strongly dependent on kidney function [14, 18]. Consequently, international guidelines and expert opinion recommend that the drug dose be reduced according to the eGFR value of individual patients [19,20,21,22,23]. In six patients of this series, daily metformin dose was clearly inappropriate given their reduced kidney function. In addition, one patient had an absolute contraindication to the drug (i.e. severe post-ischemic dilated cardiomyopathy), and two patients had undergone surgery without discontinuing the drug. One patient with normal eGFR was being treated with a high dose (3 g/day). Thus, apparently, most of the well-known contraindications/precautions with metformin use [6, 22, 23] had been overlooked systematically in the patients of the present series. Moreover, most of our patients were taking other drugs (e.g. angiotensin-converting enzyme inhibitors, angiotensin receptor blockers) that could potentially interfere with renal hemodynamics and facilitate AKI, especially in the case of coexistent hemodynamic instability. As there was a strong suspicion of MALA, both supportive treatment and therapies focused on the concomitant diseases were implemented, and RRT was started within the shortest possible time interval.
Hemodialysis is considered the therapy of choice for MALA. In fact, besides correcting acidosis and removing lactic acid, it also allows efficient metformin clearance, given the pharmacokinetic properties of the drug [24]. Metformin is a small (MW 165 Da) hydrophilic molecule, with negligible protein binding. As the drug undergoes both glomerular filtration and tubular secretion, total body (i.e. systemic) clearance can exceed 500 ml/min in normal subjects, while it decreases proportionally to the reduction of kidney function [14, 18].
Diffusive extracorporeal techniques allow high metformin clearance from plasma; for instance, effective drug clearance by conventional IHD can approximate 170 ml/min [24]. However, mass metformin removal is limited by its high volume of distribution (1–5 l/kg) [11, 18], as the drug accumulates in erythrocytes and peripheral tissues (“deep” or “distributional” compartment) with continued use (e.g. mean terminal half-life in whole blood approximates 20 h in healthy individuals) [14, 18]. Moreover, drug repartitioning from the distributional compartment to plasma is slower than renal clearance [25]. Thus, not unexpectedly, previous studies have shown a rebound increase in lactate levels in patients with MALA who had been treated with short sessions of conventional IHD [26,27,28]. For these reasons, an extension of the treatment schedule to maximize metformin removal has been proposed [29,30,31,32]. Continuous RRT has been advocated as an alternative option to IHD, especially in patients with severe hemodynamic instability. However, when CRRT is performed with routine volumes of dialysis/replacement fluid (20–30 ml/kg/h) metformin clearance is low, especially during the early phase of treatment when drug plasma levels are very high [7, 29, 33]. Since both severe acidemia and the direct toxic effect of metformin are associated with hemodynamic instability, an ideal RRT technique should combine efficient drug clearance and good hemodynamic stability, while possibly reducing the rebound phenomenon [4, 7, 11]. Prolonged intermittent RRT modalities (e.g. SLED) may be regarded as the best compromise, as they combine most of the advantages of both conventional IHD and CRRT [8,9,10]. However, clinical experience with SLED in metformin intoxication is limited [11, 30, 31]. While Angioi et al. [31] reported a 21.4% mortality, a figure very close to ours, they did not measure serum metformin values. As a comparison, Moioli et al. [32] reported a 31% overall death rate in a series of 16 patients with MALA, 77% of whom were treated by CRRT.
In this case series, we observed a rapid fall of serum metformin levels during the first 8 h of SLED, with an additional and less relevant decrease by the end of treatment. The median percentage of reduction compared to baseline levels was 78.5% at the end of the first SLED session. The reduction rate obtained by SLED was greater than that (up to 60%) reported by other studies using continuous veno-venous hemodialysis (CVVHD) or repeated conventional IHD [7]. Nonetheless, we observed a rebound in plasma metformin concentration at 4 h after the end of the first 16 h SLED session. One study performed in patients with oliguric AKI and MALA undergoing dialysis [33] documented that both erythrocyte and plasma terminal half-lives of the drug were greatly increased (43 and 52 h, respectively); moreover, erythrocyte metformin concentrations exceeded those in plasma at 48 h from admission, with metformin being still detectable in plasma after 13 days in patients treated with dialysis. This very fact suggests increased accumulation in peripheral tissues and prolonged back redistribution into plasma. In our series the drug concentration–time curves (Fig. 2) also show a biphasic pattern of elimination consistent with a two-compartment model. As metformin levels were still in the toxic range after a 16-h SLED session, our data are at variance with those of Seidowsky et al. [34], who observed metformin levels returning into the therapeutic range after a cumulative 15-h IHD duration in 85% of the treated patients. In part, this discrepancy may be explained by lower serum metformin levels in the group of patients with accidental intoxication (n = 29) reported by Seidowsky et al. [34] (median [range] 9 [3–16] mg/l) compared to the patients of the present series (median [range] 32.5 [13.6–75.6] mg/l). In fact, although pharmacokinetic analysis of time-concentration data in a patient with metformin intoxication and extremely high serum drug levels (292 mg/l) demonstrated elevated (22.2 l/h) drug clearance with IHD, metformin levels remained as high as 29.5 mg/l after 3 days of extracorporeal treatment [35]. In patients with high baseline metformin levels submitted to a 16-h SLED session, our pharmacokinetic model simulation predicts that at least one subsequent dialysis session would be required to return drug levels steadily below 5 mg/l, even in patients with early recovery of kidney function. Nonetheless, because we observed rapid kidney function recovery in 7 out of 10 patients, we hypothesize that metformin serum levels abated spontaneously after the first SLED sessions in the five patients not undergoing further treatments given a steady improvement in clinical and acid-base parameters. Moreover, our patients’ clinical characteristics at presentation were remarkably similar to those reported in previous studies.
Since data on individual-level drug dose and timing of AKI onset were not available in full detail, and prior knowledge on metformin pharmacokinetic two-compartment models is currently relatively scarce, our pharmacokinetic model was based on assumptions that we could not thoroughly test, and thus our conclusions cannot be overstated. However, the sparse metformin concentration data that we had available after 3–5 days after SLED start were consistent with the predicted data (data not shown); moreover, the findings from previous studies [24, 25, 33] seem to support our model predictions. Although we acknowledge that this is a retrospective observational single-center study, and that a randomized controlled trial comparing SLED with conventional IHD in patients with MALA would have been more informative, given the severe hemodynamic instability frequently encountered in these patients we deemed as inappropriate treating the patients of the present case series with IHD.
In conclusion, our data suggest that SLED be started within the shortest time frame in patients who present with a high suspicion of MALA, AKI and hemodynamic instability. Because SLED is simply a ‘sustained’ form of IHD, it is also widely available and can be efficiently performed in either dialysis units with conventional machines [10] or in ICUs with CRRT machines.
References
Inzucchi SE, Bergenstal RM, Buse JB, Diamant M, Ferrannini E, Nauck M et al (2015) Management of hyperglycemia in type 2 diabetes, 2015: a patient-centered approach: update to a position statement of the American Diabetes Association and the European Association for the Study of Diabetes. Diabetes Care 38:140–149
Garber AJ, Abrahamson MJ, Barzilay JI, Blonde L, Bloomgarden ZT, Bush MA et al (2016) Consensus statement by the American Association of Clinical Endocrinologists and American College of Endocrinology on the comprehensive type 2 diabetes management algorithm. 2016 Executive summary. Endocr Pract 22:84–113
Holman RR, Paul SK, Bethel MA, Matthews DR, Neil HA (2008) 10-year follow-up of intensive glucose control in type 2 diabetes. N Engl J Med 359:1577–1589
Lalau JD, Arnouts P, Sharif A, De Broe ME (2015) Metformin and other antidiabetic agents in renal failure patients. Kidney Int 87:308–322
Lalau JD, Kajbaf F, Protti A, Christensen MM, De Broe ME, Wiernsperger N (2017) Metformin-associated lactic acidosis (MALA): moving towards a new paradigm. Diabetes Obes Metab 19:1502–1512
Weisberg LS (2015) Lactic acidosis in a patient with type 2 diabetes mellitus. Clin J Am Soc Nephrol 10:1476–1483
Calello D, Liu KD, Wiegand TJ, Roberts DM, Lavergne V, Gosselin S et al (2015) Extracorporeal treatment for metformin poisoning: systematic review and recommendations from the extracorporeal treatments in poisoning workgroup. Crit Care Med 43:1716–1730
Palevsky PM, Liu KD, Brophy PD, Chawla LS, Parikh CR, Thakar CV et al (2013) KDOQI US commentary on the 2012 KDIGO clinical practice guideline for acute kidney injury. Am J Kidney Dis 61:649–672
James M, Bouchard J, Ho J, Klarenbach S, LaFrance JP, Rigatto C et al (2013) Canadian Society of Nephrology commentary on the 2012 KDIGO clinical practice guideline for acute kidney injury. Am J Kidney Dis 61:673–685
Fiaccadori E, Regolisti G, Cademartiri C, Cabassi A, Picetti E, Barbagallo M et al (2013) Efficacy and safety of a citrate-based protocol for sustained low-efficiency dialysis in AKI using standard dialysis equipment. Clin J Am Soc Nephrol 8:1670–1678
Regolisti G, Antoniotti R, Fani F, Greco P, Fiaccadori E (2017) Treatment of metformin intoxication complicated by lactic acidosis and acute kidney injury: the role of prolonged intermittent hemodialysis. Am J Kidney Dis 70:290–296
Frid A, Sterner GN, Löndahl M, Wiklander C, Cato A, Vinge E et al (2010) Novel assay of metformin levels in patients with type 2 diabetes and varying levels of renal function: clinical recommendations. Diabetes Care 33:1291–1293
D’Argenio DZ, Schumitzky A (1997) Adapt II release 4, user’s guide. In: Biomedical simulations resource. University of Southern California, Los Angeles
Tucker GT, Casey C, Phillips PJ, Connor H, Ward JD, Woods HF (1981) Metformin kinetics in healthy subjects and in patients with diabetes mellitus. Br J Clin Pharmacol 12:235–246
Madiraju AK, Erion DM, Rahimi Y, Zhang XM, Braddock DT, Albright RA et al (2014) Metformin suppresses gluconeogenesis by inhibiting mitochondrial glycerophosphate dehydrogenase. Nature 510:542–546
Luengo A, Sullivan LB, Heiden MG (2014) Understanding the complex-I-ty of metformin action: limiting mitochondrial respiration to improve cancer therapy. BMC Biol 12:82
Boucaud-Maitre D, Ropers J, Porokhov B, Altman JJ, Bouanick B, Doucet J et al (2016) Lactic acidosis: relationship between metformin levels, lactate concentration and mortality. Diabet Med 33:1536–1543
Graham GG, Punt J, Arora M, Day RO, Doogue MP, Duong JK et al (2011) Clinical pharmacokinetics of metformin. Clin Pharmacokinet 50:81–98
Guideline development group (2015) Clinical Practice Guideline on management of patients with diabetes and chronic kidney disease stage 3b or higher (eGFR < 45 ml/min). Nephrol Dial Transpl 30(Suppl2):ii1–i142
Kidney Disease: Improving Global Outcomes (KDIGO) CKD Work Group (2013) KDIGO 2012 clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney Int 84(3):1–150
National Institute for Health and Care Excellence. NICE guidelines [NG28] (2015) Type 2 diabetes in adults: management. https://www.nice.org.uk/guidance/NG28/chapter/1-Recommendations. Accessed 24 Nov 2017 (Published date: December 2015. Last updated: May 2017)
Inzucchi SE, Lipska J, Mayo H, Bailey CJ, McGuire DK (2014) Metformin in patients with type 2 diabetes and kidney disease, a systematic review. JAMA 312:2668–2675
Lipska KJ, Bailey CJ, Inzucchi SE (2011) Use of metformin in the setting of mild-to-moderate renal insufficiency. Diabetes Care 34:1431–1437
Lalau JD, Andrejak M, Morinière P, Coevoet B, Debussche X, Westeel PF et al (1989) Hemodialysis in the treatment of lactic acidosis in diabetics treated by metformin: a study of metformin elimination. Int Clin Pharmacol Ther Toxicol 27:285–288
Xie F, Ke AB, Bowers GD, Zamek-Glisczynski MJ (2015) Metformin’s intrinsic blood-to-plasma partition ratio (B/P): reconciling the perceived high in vivo B/P> 10 with the in vitro equilibrium value of unity. J Pharmacol Exp Ther 354:225–229
Heaney D, Majid A, Junor B (1997) Bicarbonate haemodialysis as a treatment of metformin overdose. Nephrol Dial Transpl 12:1046–1047
Chalopin JM, Tanter Y, Besancenot JF, Cabanne JF, Rifle G (1984) Treatment of metformin-associated lactic acidosis with closed recirculation bicarbonate buffered hemodialysis. Arch Intern Med 144:203–205
Panzer U, Kluge S, Kreymann G, Wolf G (2004) Combination of intermittent haemodialysis and high-volume continuous haemofiltration for the treatment of severe metformin-induced lactic acidosis. Nephrol Dial Transpl 19:2157–2158
Guo PY, Storsley LJ, Finkle SN (2006) Severe lactic acidosis treated with prolonged hemodialysis: recovery after massive overdoses of metformin. Semin Dial 19:80–83
Teutonico A, Libutti P, Lomonte C, Antonelli M, Casucci F, Basile C (2008) Treatment of metformin-associated lactic acidosis with sustained low-efficiency daily dialysis. NDT Plus 1:380–381
Angioi A, Cabiddu F, Conti M, Pili G, Atzeni A, Matta V et al (2018) Metformin associated lactic acidosis: a case series of 28 patients treated with sustained low-efficiency dialysis (SLED) and long term follow-up. BMC Nephrol 19:77
Moioli A, Maresca B, Manzione A et al (2016) Metformin associated lactic acidosis (MALA): clinical profiling and management. J Nephrol 29:783–789
Kajbaf F, Bennis Y, Hurtel-Lemaire AS, Andréjak M, Lalau JD (2016) Unexpectedly long half-life of metformin elimination in cases of metformin accumulation. Diabet Med 33:105–110
Seidowsky A, Nseir S, Houdret N, Fourrier F (2009) Metformin-associated lactic acidosis: a prognostic and therapeutic study. Crit Care Med 37:2191–2196
Chiew AL, Wright DFB, Dobos NM et al (2018) “Massive” metformin overdose. Br J Clin Pharmacol. https://doi.org/10.1111/bcp.13582
Funding
None.
Author information
Authors and Affiliations
Contributions
Research idea and study design: PG, GR, UM, EnFi; data acquisition: PG, ElFe, FF, EP, CM, IG; data analysis/interpretation: UM, GR, PG; statistical analysis: UM, GR; supervision and mentorship: EnFi, GR. Each author contributed important intellectual content during manuscript drafting or revision and accepts accountability for the overall work by ensuring that questions pertaining to the accuracy or integrity of any portion of the work are appropriately investigated and resolved.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in this study, involving human participants, were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Greco, P., Regolisti, G., Maggiore, U. et al. Sustained low-efficiency dialysis for metformin-associated lactic acidosis in patients with acute kidney injury. J Nephrol 32, 297–306 (2019). https://doi.org/10.1007/s40620-018-00562-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40620-018-00562-2