Abstract
Background
The clinicopathological characteristics, treatment response and long-term outcome of immunoglobulin (Ig)A nephropathy with minimal change disease (MCD-IgAN) are not well defined.
Methods
Patients with biopsy-proven MCD-IgAN from the Jinling Hospital IgA nephropathy Registry were systematically reviewed and compared with those with IgA nephropathy without minimal change disease (Non-MCD-IgAN).
Results
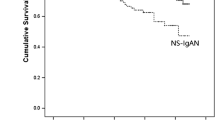
We compared data of 247 MCD-IgAN patients and 1,121 Non-MCD-IgAN patients. Compared to Non-MCD-IgAN, MCD-IgAN patients were younger,with male predominance, had higher levels of proteinuria, total cholesterol and estimated glomerular filtration rate (eGFR), lower incidence of hypertension and microhematuria, lower level of serum creatinine, and had less severe glomerular, tubulointerstitial and vascular lesions in renal pathology. In the Non-MCD-IgAN group, 157 patients (14.0 %) reached the renal endpoint and 103 patients (9.2 %) entered end-stage renal disease (ESRD). The 5-,10-, 15- and 20-year cumulative renal survival rates from ESRD, calculated by Kaplan–Meier method, were 95.0, 83.0, 72.9 and 65.4 %, respectively. In the MCD-IgAN group, no patients entered ESRD and only 4 (1.6 %) reached the renal endpoint. Patients with MCD-IgAN had a significantly better renal outcome than Non-MCD-IgAN (p < 0.01). At multivariate Cox analysis, proteinuria >1.0 g/day, hypertension, eGFR <60 ml/min/1.73 m2, hypoproteinemia and hyperuricemia were independent risk factors of renal survival for Non-MCD-IgAN patients [hazard ratio (HR) 3.43, p < 0.001; HR 1.65, p < 0.05; HR 2.61, p < 0.001; HR 2.40, p < 0.001; HR 2.27, p < 0.001, respectively), but not for patients with MCD-IgAN.
Conclusions
The long-term outcome of patients with MCD-IgAN is significantly better than that of patients with Non-MCD-IgAN.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The long-term renal outcome of immunoglobulin (Ig)A nephropathy (IgAN) is not promising. Our previous study showed that the 20-year cumulative renal survival rate of IgAN was 64 % [1, 2]. Five clinical features—proteinuria >1.0 g/day, hypoalbuminemia, hypertension, decreased estimated glomerular filtration rate (eGFR) and hyperuricemia—have been identified as independent predictors of an unfavorable renal outcome [2–6], whereas the prognostic value of hematuria for renal survival of IgAN remains controversial [7, 8]. Moreover, the new Oxford classification has identified four definitive histological features for predicting renal prognosis of IgAN [9, 10]. Nephrotic range proteinuria is uncommon in IgAN [11]. In some rare cases, IgAN presents with nephrotic syndrome, has a rapid response to corticosteroid therapy, typically has mild glomerular lesions under light microscopy, and diffuse effacement of podocyte foot process and mesangial electron dense deposition under electron microscopy; this special entity of IgAN has been referred to as IgAN with minimal change disease (MCD-IgAN). Many studies have reported the special clinicopathological features of MCD-IgAN [12–19]; however, long-term renal outcome of MCD-IgAN in large cohorts is not well defined and the comparison of its long-term prognosis with that of non-MCD-IgAN remains unclear. We therefore compared 247 cases of MCD-IgAN with 1,121 cases of non-MCD-IgAN from the Jinling Hospital IgAN Registry in order to characterize this unusual entity in terms of clinicopathological features and long-term renal outcomes.
Materials and methods
Patients
A total of 11,885 patients were diagnosed as IgAN in Jinling Hospital between January 1989 and July 2013, of whom 306 patients met the diagnostic criteria for MCD-IgAN. We enrolled 247 patients with MCD-IgAN and another 1121 patients without MCD-IgAN (Non-MCD-IgAN) for comparison purposes. All enrolled patients were followed for more than 1 year with complete records. We excluded those with other chronic diseases, such as diabetic nephropathy or hepatitis B-associated nephropathy, etc. In addition, all enrolled MCD-IgAN patients received oral corticosteroids as initial treatment.
Diagnostic criteria for IgAN were: diffuse IgA-dominant depositions (IgA depositions weaker than 1+, those with non-mesangial deposition of IgA, or those with greater than 1+ deposition of IgA, but not IgA-dominant deposition were excluded) in the glomerular mesangial region and mesangial electron dense deposition on electron microscopy; we excluded secondary IgAN (e.g. systemic lupus erythematosus, Henoch–Schönlein purpura, psoriasis, rheumatoid arthritis). MCD-IgAN was defined as, in addition to the typical diagnostic criteria for IgAN, the presence of minimal changes in glomeruli at light microscopy and diffuse effacement of podocyte foot processes (>50 % of the capillary surface area involved) at electron microscopy; we excluded secondary MCD (e.g. from non-steroidal anti-inflammatory drugs, antibiotics, infection, tumor, etc.), non-MCD-IgAN was defined as IgAN that did not meet the diagnostic criteria for MCD-IgAN.
Data collection
Clinical data included gender, age, disease duration, initial symptoms, and blood pressure. Treatment protocol data including regimen, time, dosage, combination therapy and renal survival were recorded. Laboratory data included urinary red blood cell count (URBC), 24-h urinary protein excretion (Upr), serum albumin (ALB), serum total cholesterol (Chol), serum creatinine (Scr), uric acid (UA), serum electrolytes, and eGFR calculated using the equation of chronic kidney disease—epidemiology (CKD-EPI) formula [20].
Renal pathology
Renal biopsy specimens were examined using direct immunofluorescence (IM), light microscopy (LM) and electron microscopy (EM). Stains employed included hematoxylin and eosin (H&E), periodic acid-Schiff (PAS), silver methenamine (Meth) and Masson’s trichrome. The location and intensity of IgG, IgM, IgA, C3, C4, C1q and fibrin-related antigens were examined by IM. The presence and location of electron dense deposits and podocyte foot process lesions were examined by EM.
Definitions
Disease duration was defined as time from disease onset to renal biopsy. Hypertension was defined as systolic blood pressure ≥140 mmHg and/or diastolic blood pressure ≥90 mmHg. ESRD was defined as eGFR <15 ml/min/1.73 m2, initiation of dialysis for more than 3 months or transplantation. Renal endpoint (combined event) was defined as a ≥50 % decline in eGFR or ESRD. The scoring sheet was based on the Oxford classification of IgAN [9], and seven pathological variables, namely mesangial hypercellularity (M), endocapillary proliferation (E), segmental sclerosis or adhesion (S), tubular atrophy/interstitial fibrosis (T), crescents (C), glomerulus necrosis (N), and vascular changes (hyaline degeneration and intimal thickening) were assessed. Tubulointerstitial lesions [21] were semi-quantitatively graded as: 0 = no lesions, 1 = mild (<25 %), 2 = moderate (25–49 %), and 3 = severe (≥50 %).
Treatment protocol
Prednisone was administered at a full dose of 1 mg/kg/day (maximum 60 mg/day) until 2 weeks after complete remission, or prolonged to 8 weeks in the case of no remission, or continued to 10 weeks in those with partial remission at the 8th week in MCD-IgAN patients. After that, the dosage was first tapered by 5 mg every 2 weeks down to 30 mg/day; additional immunosuppressants including cyclophosphamide, cyclosporine, tacrolimus or mycophenolate mofetil were administered in some patients if unresponsiveness or relapse occurred after tapering the corticosteroids, then prednisone was tapered by 2.5 mg every 2 weeks to a maintenance dose of 10 mg/day for 1.5 years, and then withdrawn. Relapsers would restart induction therapy of full-dose steroids. Corticosteroids were only used in Non-MCD-IgAN patients with acute crescentic lesions and macroproteinuria. Those with a long history of kidney disease, manifesting as segmental or global glomerulosclerosis pathologically or severe chronic tubulointerstitial lesions often received angiotensin-converting enzyme inhibitors (ACEIs) to delay the progression of kidney disease given its irreversible nature.
Statistical analyses
All data were analyzed using SPSS 19.0 statistical software. Normally distributed variables were expressed as mean ± standard deviation (SD), and differences among groups were analyzed by Student’s t test. Non-parametric variables were expressed as median (range or interquartile range, IQR) and compared using the Mann–Whitney test. Categorical variables were expressed as percentages and compared using Pearson’s χ 2 test or Fisher’s exact test. The relationship between parameters and renal survival was assessed using Cox regression. Analysis of renal survival was estimated with the Kaplan–Meier method and compared using the log-rank test. All p values were two-tailed and values <0.05 were considered statistically significant.
Results
Demographic and clinical characteristics at biopsy
A total of 247 MCD-IgAN patients and 1121 Non-MCD-IgAN patients from Jinling Hospital IgAN Registry were enrolled. Compared to the Non-MCD-IgAN group, patients with MCD-IgAN were younger (27.05 ± 11.03 vs. 33.51 ± 9.16 years, p < 0.001),with male predominance (67.6 vs. 49.4 %, p < 0.001), had a shorter disease duration [1 (0.1–408) vs. 10 (0.2–557) months, p < 0.001], more prominent symptoms of edema (91.9 vs. 22.8 %, p < 0.001), had a lower incidence of hypertension and microhematuria, lower levels of serum creatinine and albumin, and higher levels of proteinuria, total cholesterol and eGFR (p < 0.05) (Table 1).
Pathological features
The scoring sheet was based on the Oxford classification of IgAN. Compared to the Non-MCD-IgAN group, MCD-IgAN patients had a smaller proportion of segmental sclerosis [0 (0–22.2) vs. 13.6 (0–90.0) %, p < 0.001], a lower incidence of mesangial hypercellularity (M1) (10.9 vs. 36.4 %, p < 0.001) and tubular atrophy/interstitial fibrosis (T1/T2) lesion (4.9 vs. 20.1 %, p < 0.001), and less severe interstitial lymphocyte and monocyte infiltration and vascular lesions (p < 0.001) (Table 2).
Long-term follow up and prognosis
During the median follow-up of 5.3 years (range 1.0–21.7), 157 patients (14.0 %) of the 1,121 cases of Non-MCD-IgAN reached the renal endpoint and 103 patients (9.2 %) entered ESRD. The 5-, 10-, 15- and 20-year cumulative renal survival rates from ESRD and the combined event, calculated by the Kaplan–Meier method, were 95.0, 83.0, 72.9, 65.4 % and 91, 77.0, 63.6, 50.4 %, respectively. During the median follow-up of 2.6 years (range 1.0–15.2), none of the 247 cases of MCD-IgAN entered ESRD and only 4 patients (1.6 %) reached the renal endpoint. The 5-year cumulative renal survival rate from the combined event was 97 %. Patients with MCD-IgAN had significantly better renal outcome than Non-MCD-IgAN patients (p < 0.01) (Fig. 1).
At multivariate Cox analysis, proteinuria >1.0 g/day, hypertension, eGFR <60 ml/min/1.73 m2, hypoproteinemia and hyperuricemia emerged as independent risk factors for renal survival in Non-MCD-IgAN [hazard ratio (HR) 3.43, p < 0.001; HR 1.65, p < 0.05; HR 2.61, p < 0.001; HR 2.40, p < 0.001; HR 2.27, p < 0.001, respectively], but these risk factors failed to predict renal survival for MCD-IgAN (Table 3). All four MCD-IgAN patients who reached the renal endpoint achieved complete remission after initial induction therapy, but all had more than two relapses afterwards; 3 cases showed no response to therapy and one achieved partial remission at the last follow-up. These four patients reached the renal endpoint after 2.1, 2.2, 2.5 and 3.4 years of follow-up. As for treatment drugs, MCD-IgAN patients more frequently received immunosuppressive agents and statins, and less frequently received ACEI/angiotensin receptor blockers (ARB) than Non-MCD-IgAN patients (Table 4).
Discussion
Nephrotic range proteinuria is uncommon in IgAN, occurring in only 5–10.2 % of patients with IgAN [11] and, when present, it is usually associated with an increased risk of ESRD [2]. MCD-IgAN is a special type of disease that typically presents with nephrotic syndrome, but has a prompt response to corticosteroid therapy and promising prognosis [12, 17, 19]. The incidence of MCD-IgAN remains unclear. We retrospectively reviewed all patients in Jinling Hospital IgAN Registry during the last 15 years and demonstrated that MCD-IgAN was not uncommon, accounting for 2.57 % of IgAN. Currently available studies are mainly case reports and small series [12–19]; reports on the long-term prognosis in large cohorts and comparison with Non-MCD-IgAN are still limited. We therefore retrospectively analyzed and compared the clinicopathological features and prognosis of these two groups.
During the median follow-up of 2.6 years, none of the 247 cases of MCD-IgAN entered ESRD and only 4 patients (1.6 %) reached the renal endpoint, consistent with previous reports [17, 19]. The 15- and 20-year cumulative renal survival rates from ESRD, calculated by the Kaplan–Meier method, were 72.9 and 65.4 %, indicating that MCD-IgAN patients had a significantly better renal outcome than Non-MCD-IgAN (p < 0.01). Clinicopathological findings showed that patients with MCD-IgAN were younger,more predominantly male, had a higher amount of proteinuria, lower incidence of hypertension and microhematuria, and a lower level of serum creatinine than Non-MCD-IgAN patients. Based on the Oxford classification of IgAN, MCD-IgAN patients had no endocapillary proliferation (E) or segmental sclerosis (S) lesions, and less severe mesangial hypercellularity (M) and tubular atrophy/interstitial fibrosis (T) lesions. MCD-IgAN exhibited markedly different clinical manifestations, biopsy findings and long-term prognosis from Non-MCD-IgAN, supporting the notion that MCD-IgAN should be considered as a special type of IgAN.
Differences in criteria and timing of biopsy across different reports may lead to discrepancies in findings concerning the long-term prognosis of IgAN, but heavy proteinuria, hypertension and lower eGFR have persistently been demonstrated as independent risk factors for the poor long-term prognosis of IgAN by many studies [2–6]. Our study revealed that patients with proteinuria >1.0 g/day had a 3.43-fold higher probability of reaching the combined event than those with proteinuria <1.0 g/day, and patients with eGFR <60 ml/min/1.73 m2 had a 2.61-fold higher risk than those with eGFR ≥60 ml/min/1.73 m2. Hypertension, hypoproteinemia and hyperuricemia could increase the risk by 1.65, 2.4 and 2.27 times, respectively, but these risk factors failed to predict the renal survival among patients with MCD-IgAN, demonstrating that the risk factors were quite different between the two groups.
Then how to explain the more favorable prognosis of MCD-IgAN with nephrotic range proteinuria than Non-MCD-IgAN? First, the Oxford classification of IgAN indicated that the mesangial hypercellularity score (M), segmental glomerulosclerosis (S), endocapillary hypercellularity (E), and tubular atrophy/interstitial fibrosis (T) independently predicts worse renal outcome; however, MCD-IgAN in our study had no prominent glomerular, tubulointerstitial or vascular lesions. Second, MCD-IgAN typically presented with massive proteinuria; some cases were even complicated with water-sodium retention, hypertension and acute kidney injury (AKI), but this entity had a sensitive response to corticosteroid therapy, and there was complete remission in 54.3 and 87.4 % of MCD-IgAN within 4 and 8 weeks of treatment. After remission, proteinuria, water-sodium retention, hypertension and AKI were usually alleviated. Thus, the predictors for poor prognosis disappeared accordingly. As a result, a rapid response to corticosteroid could be one of the reasons for the promising prognosis of MCD-IgAN. Actually, MCD-IgAN exhibit similar clinicopathological features and treatment response to MCD patients, and current studies have identified the response to steroid therapy as a strong predictor for the prognosis of MCD—steroid-sensitive patients have significantly better renal survival than steroid-resistant patients [22]. In our cohort, all four cases of MCD-IgAN who reached the renal endpoint experienced more than two relapses; 3 of the cases had no response to therapy and one achieved a partial remission at the last follow-up. Consequently, more attention should be paid to those patients with a poor response to therapy due to their worse prognosis.
This study has some limitations. First, patients followed for <1 year were excluded to avoid the effect of AKI on the prognosis of MCD-IgAN. Although no patients with MCD-IgAN entered ESRD in this study, the possibility of severe cases progressing to ESRD within 1 year of follow-up could not be excluded. Second, the prevalence of nephrotic range proteinuria and edema as first symptoms in our study is not consistent with other studies. In our center, the Non-MCD-IgAN patients with mild clinical manifestations (such as microscopic hematuria or microalbuminuria) did not undergo renal biopsy. Thus different biopsy indications may have led to a different incidence of proteinuria and edema as first symptoms in our study compared to other reports. Third, the Non-MCD-IgAN patients in our study were drawn from the Jinling Hospital IgAN Registry during the same period with complete records. Although the sample size was quite large, we only included those with complete clinical and follow-up records, thus we could not avoid the impact of a selection bias on prognosis. Since MCD-IgAN patients had a sensitive response to steroid and immunosuppressive therapy, the majority of patients were out of follow-up; thus MCD-IgAN had a much shorter period of follow-up than Non-MCD-IgAN, and this different length of follow-up may have had an effect on the comparison of prognosis. Furthermore, though this retrospective study recorded therapeutic regimen, the different characteristics of the two groups of diseases made it hard to evaluate the impact of treatment on disease progression.
In this large cohort of MCD-IgAN patients with a long observational period, MCD-IgAN accounts for 2.57 % of IgAN, and the long-term outcome of patients with MCD-IgAN is significantly better than that of Non-MCD-IgAN patients. The clinical manifestations and pathological features of MCD-IgAN are quite different from those of Non-MCD-IgAN.
References
Koyama A, Igarashi M, Kobayashi M (1997) Natural history and risk factors for immunoglobulin A nephropathy in Japan. Research Group on Progressive Renal Diseases. Am J Kidney Dis 29:526–532
Le W, Liang S, Hu Y et al (2012) Long-term renal survival and related risk factors in patients with IgA nephropathy: results from a cohort of 1155 cases in a Chinese adult population. Nephrol Dial Transplant 27:1479–1485
Moriyama T, Itabashi M, Takei T et al (2015) High uric acid level is a risk factor for progression of IgA nephropathy with chronic kidney disease stage G3a. J Nephrol 28:451–456
Barbour SJ, Cattran DC, Kim SJ et al (2013) Individuals of Pacific Asian origin with IgA nephropathy have an increased risk of progression to end-stage renal disease. Kidney Int 84:1017–1024
Reich HN, Troyanov S, Scholey JW et al (2007) Remission of proteinuria improves prognosis in IgA nephropathy. J Am Soc Nephrol 18:3177–3183
Donadio JV, Bergstralh EJ, Grande JP et al (2002) Proteinuria patterns and their association with subsequent end-stage renal disease in IgA nephropathy. Nephrol Dial Transplant 17:1197–1203
Tanaka K, Moriyama T, Iwasaki C et al (2015) Effect of hematuria on the outcome of IgA nephropathy with mild proteinuria. Clin Exp Nephrol 19:815–821
Le W, Liang S, Chen H et al (2014) Long-term outcome of IgA nephropathy patients with recurrent macroscopic hematuria. Am J Nephrol 40:43–50
Cattran DC, Coppo R, Cook HT et al (2009) The Oxford classification of IgA nephropathy: rationale, clinicopathological correlations, and classification. Kidney Int 76:534–545
Zeng CH, Le W, Ni Z et al (2012) A multicenter application and evaluation of the oxford classification of IgA nephropathy in adult chinese patients. Am J Kidney Dis 60:812–820
Barratt J, Feehally J (2005) IgA nephropathy. J Am Soc Nephrol 16:2088–2097
Lai KN, Lai FM, Ho CP et al (1986) Corticosteroid therapy in IgA nephropathy with nephrotic syndrome: a long-term controlled trial. Clin Nephrol 26:174–180
Cheng IK, Chan KW, Chan MK (1989) Mesangial IgA nephropathy with steroid-responsive nephrotic syndrome: disappearance of mesangial IgA deposits following steroid-induced remission. Am J Kidney Dis 14:361–364
Westhoff TH, Waldherr R, Loddenkemper C et al (2006) Mesangial IgA deposition in minimal change nephrotic syndrome: coincidence of different entities or variant of minimal change disease. Clin Nephrol 65:203–207
Barbiano DBG, Mazzucco G, Casanova S et al (1986) Steroid-sensitive nephrotic syndrome with mesangial IgA deposits: a separate entity? Observation of two cases. Am J Nephrol 6:141–145
Gallego N, Gonzalo A, Mampaso F et al (1988) Steroid-dependent nephrotic syndrome with minimal glomerular changes and mesangial IgA deposits. Child Nephrol Urol 9:98–100
Qin J, Yang Q, Tang X et al (2013) Clinicopathologic features and treatment response in nephrotic IgA nephropathy with minimal change disease. Clin Nephrol 79:37–44
Wang J, Juan C, Huang Q et al (2013) Corticosteroid therapy in IgA nephropathy with minimal change-like lesions: a single-centre cohort study. Nephrol Dial Transplant 28:2339–2345
Herlitz LC, Bomback AS, Stokes MB et al (2014) IgA nephropathy with minimal change disease. Clin J Am Soc Nephrol 9:1033–1039
Levey AS, Stevens LA, Schmid CH et al (2009) A new equation to estimate glomerular filtration rate. Ann Intern Med 150:604–612
Waldman M, Crew RJ, Valeri A et al (2007) Adult minimal-change disease: clinical characteristics, treatment, and outcomes. Clin J Am Soc Nephrol 2:445–453
Szeto CC, Lai FM, Chow KM et al (2015) Long-term outcome of biopsy-proven minimal change nephropathy in Chinese adults. Am J Kidney Dis 65:710–718
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflict of interest to declare.
Ethical approval
For this type of study formal consent is not required. This article does not contain any studies with animals performed by any of the authors.
Informed consent
For this type of study formal consent is not required.
Funding
This study was funded by the National Basic Research Program of China 973 Program No.2012CB517600 (No. 2012CB517606) and the National Science Foundation of China (810-2010-8016).
Rights and permissions
About this article
Cite this article
Li, XW., Liang, SS., Le, WB. et al. Long-term outcome of IgA nephropathy with minimal change disease: a comparison between patients with and without minimal change disease. J Nephrol 29, 567–573 (2016). https://doi.org/10.1007/s40620-015-0242-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40620-015-0242-9