Abstract
Background
The increasing frequency in the diagnosis of thyroid nodules has raised a growing interest in the search for new diagnostic tools to better select patients deserving surgery. In 2014, the major Italian Societies involved in the field drafted a new cytological classification, to better stratify pre-surgical risk of thyroid cancer, especially for the indeterminate category, split into TIR3A and TIR3B subclasses, associated to different therapeutic decisions.
Materials and methods
This retrospective cross-sectional survey analyzed thyroid fine-needle aspiration biopsy performed at our outpatient clinic before and after the introduction of the new SIAPEC-IAP consensus in May 2014.
Results
8956 thyroid nodules were included in the analysis: 5692 were evaluated according to the old classification and 3264 according to the new one. The new criteria caused the overall prevalence of TIR3 to increase from 6.1 to 20.1%. Of those, 10.7 and 9.4% were included in the TIR3A and TIR3B subgroups, respectively. Each of the 213 TIR3B nodules underwent surgery and 86 (40.4%) were diagnosed as thyroid cancer, while among the 349 TIR3A nodules, only 15 of the 60 that underwent surgery were found to be thyroid cancer.
Conclusions
This analysis shows that the new SIAPEC-IAC criteria significantly increased the proportion of the overall TIR3 diagnosis. The division of TIR3 nodules into two subgroups (A and B) allowed a better evaluation of the oncologic risk and a better selection of patients to be referred to surgery.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
The prevalence of thyroid nodules in the general population is remarkable, with 15–20% of all subjects showing palpable nodules [1,2,3]. Nowadays, the diagnosis of thyroid nodules has become even more frequent because of the use of neck ultrasounds (US), allowing the detection of nodules in 19–67% of the population not clinically suspected for thyroid disease [4, 5]. Despite the large number of affected subjects, malignant thyroid cancer remains confined to a small group of patients. The prevalence of thyroid cancer in clinical series of patients with thyroid nodules has been reported to range between 8 and 16% [3], whereas the estimated incidence of thyroid cancer in the general population is around 0.05–0.2 cases/1000 person * year [5, 6]. The increased accuracy in the diagnosis of thyroid nodules is likely to produce an increase in the estimated incidence of thyroid cancer [6, 7], that is usually well differentiated and shows in most cases an excellent prognosis with survival rates of 95% in 30 years [5]. The development of diagnostic strategies capable of discriminating between malignant and benign nodules becomes, therefore, even more important than in the past.
In patients with thyroid nodules, it is important to evaluate some clinical risk factors, such as nodule features (large size, rapid growth, high consistency, fixation to surrounding structures), positive history for cancer risk (past exposure to ionizing radiation) and patient characteristics (young, age and male sex).
Fine-needle aspiration biopsy (FNAB) is considered to be the best predictive, cost-effective, safe and rapid test for discriminating malignant thyroid nodules [4, 8]. In most cases, thyroid cytology is classified as benign disease (60–70%), while the remaining are included in the categories of indeterminate, suspicious for malignancy, and malignant [4, 8]. Only a small percentage of FNAs result non-diagnostic, requiring a sampling repetition.
Among overall cytological categories, the indeterminate one is the most debated in all classification systems, for the relative low malignancy rate at diagnostic surgery. Both British Thyroid Classification (UK RCPath) and Bethesda Reporting System for Thyroid Cytology (BRSTC) identify two subgroups in the Indeterminate category [9, 10]. The BRSTC distinguishes two groups: atypia of undetermined significance (AUS)/follicular lesion of undetermined significance (FLUS) and follicular neoplasm (FN)/suspicious for FN (SFN). Conversely, the UK RCPath contemplates: Thy3a (atypia), corresponding to the Bethesda AUS/FLUS and Thy3f (follicular neoplasm), corresponding to the FN/SFN [11, 12].
Until 2014, the Italian Society for Anatomic Pathology and Cytology joint with the Italian Division of the International Academy of Pathology (SIAPEC-IAP) and the major Italian Societies of Endocrinology (the Italian Thyroid Association, the Italian Society of Endocrinology and the Italian Association of Clinical Endocrinologists) had endorsed a cytological classification of thyroid nodules with only one category of indeterminate lesions, named TIR3 [13]. In 2014, to improve the discriminating capacity of FNAB cytology, TIR3 was separated into two subgroups: TIR3A (Low-risk Indeterminate lesion) and TIR3B (High-risk Indeterminate lesion), approximately corresponding the first to the AUS/FLUS and Thy3a and the second to FN/SFN and Thy3f. The two categories have been reported to possess different risks of malignancy (< 10% for TIR3A and 15–30% for TIR3B) and, consequently, a different clinical management, according to which only TIR3B nodules should undergo surgery. The expected rate of malignancy for TIR3 subcategories is only partially based on the evidence of the published data [14].
The present retrospective study was designed to assess the impact of the new cytological classification of thyroid nodules, verifying its predictive power for thyroid cancer.
Materials and methods
The current study was designed as a retrospective cross-sectional survey, enrolling all patients referred for thyroid nodules to the Thyroid outpatient clinic of the University Hospital of Careggi, Florence between February 1st 2008 and July 31st 2017. All patients provided their written informed consent.
After collecting a complete clinical history, all patients underwent a neck ultrasound examination, assessing the presence of uninodular or multinodular goiter. Size, composition (solid, mixed or cystic), echogenicity (anechoic, hyperechoic or isoechoic, hypoechoic, very hypoechoic), halo (present, absent or present but discontinuous), margins (well defined or smooth, irregular or blurred), shape (taller than wide), echogenic foci (hyperechoic spot, macrocalcifications, microcalcifications), and vascularization (type 1, absence of flow signals; type 2, perinodular and absent or slight intranodular blood flow; type 3, marked intranodular blood flow) were determined and registered for each nodule.
The US and color-Doppler ultrasound (CDU) examinations were performed with a commercially available real-time scanner (ESAOTE Technos) equipped with a linear transducer operating at 10 MHz.
All nodules with suspicious ultrasound parameters were subjected to FNAB, according to the 2009 and 2015 American Thyroid Association (ATA) guidelines [15, 16].
Each FNAB, aimed at tissue sampling was performed by an experienced surgeon, under the guidance of an endocrinologist with large experience in ultrasonography. A 21–23 gauge needle was used with the no-aspiration technique, according to which the needle, held between the thumb and forefinger of one hand, was gently inserted into the nodule and moved in different directions for 2–5 s, with 3 forward and back movements per second, allowing material entering the needle by capillary action. Cytological material from FNA was immediately rinsed into CytoLyt Solutions. According to the manufacturer’s suggestions (CyticMalborough, MA, USA), each sample was centrifuged, resuspended in PreservCyt Solution, and processed using the ThinPrep®Processor. Thereafter thin-layer slides were stained using the Papanicolaou procedure.
The cytologic diagnoses before May 2014 were made in accordance with the 2007 classification of the British Thyroid Association [17], including five diagnostic groups, namely Thy 1—non-diagnostic; Thy 2—non neoplastic, Thy 3—follicular lesions, Thy 4—suspicious for malignancy, Thy 5—diagnostic for malignancy; after 2014, diagnoses were performed according to the new 2014 SIAPEC consensus. All samples were reviewed by two senior pathologists.
Only patients who gave their informed consent to FNAB and to the use of their clinical data were included in the analysis.
Before 2014, the local practice, in accordance with the British Guidelines 2007 [17], was to refer almost all TIR3 nodules to surgery, considering clinical features, as described in “Background” section. After 2014, TIR3B nodules were all referred to surgery, whereas TIR3A nodules were not. However, a minority of TIR3A nodules underwent surgery, based on clinical judgment (N = 60). The surgical samples were cut before fixation for macroscopic examination.
Pathological evaluation was carried out performing multiple 5-mm slices of the whole thyroid gland to accurately define the dimensions of malignant lesions and their multifocality. Specimens were fixed in buffered formalin, embedded in paraffin and stained with hematoxylin and eosin for histologic study. All neoplastic lesions were staged according to tumor size, nodal involvement and distant metastasis (TNM 2010 and 2017) classification criteria [18,19,20].
Chi square test was used to compare categorical variables. Stepwise multiple binary logistic regression was applied for multivariate analysis, including in the model the variables which had been resulted statistically significant at univariate analysis. All statistical analyses were performed on SPSS for windows 23.0.
Results
9016 patients with thyroid nodules were evaluated between February 2008 and July 2017; of these, 8956 gave their consent to FNAB and were included in the study. The old cytological classification was applied until May 2014; from then on, the new SIAPEC consensus criteria were applied. Therefore, 5692 and 3264 nodules were classified according to the old and new criteria, respectively.
The overall proportion of subjects in the Indeterminate category (TIR3) increased after 2014, when the categorization into TIR3A (Low-risk) and TIR3B (High-risk) was introduced (Fig. 1).
In fact, the prevalence of TIR3 was 6.1% (347 out of 5692) until May 2014, with the old classification, and 20.1% (655 out of 3264), with the new one. Since the introduction of the distinction between TIR3A and TIR3B, of the 655 TIR3, 349 (10.7%) and 306 (9.4%) were classified as TIR3A and TIR3B, respectively.
Of the 347 patients classified as TIR3 (Indeterminate) before May 2014, 209 underwent surgery in our University Hospital where their thyroid was evaluated by our colleagues of the Pathology Department, providing us the histological results of the nodules previously submitted to FNAB. The proportion of subjects with thyroid malignancy was 28.7% (60 out of 209).
After the introduction of the new classification, all patients with TIR3B nodules (Indeterminate High-risk) were advised to undergo surgery. Of the 213 patients receiving surgery in our University Hospital, 86 (40.4%) were affected by thyroid cancer. TIR3B nodules showing Hurthle cell proliferation resulted malignant in a lower proportion (6 out of 31; 19.4%, p < 0.01).
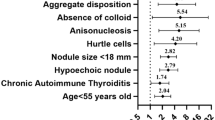
Since the introduction of the new classification, we collected 349 TIR3A nodules. Of those, 179 subjects repeated FNAB within 6 months and the cytological results were as follows: 73 TIR3A, 34 TIR3B, 43 TIR2, 24 TIR1, 3 TIR4, 2 TIR5. All these reclassified nodules were assigned to the corresponding group. In addition, 60 subjects with TIR3A cytology underwent surgery and 15 of them (25%) resulted affected by a thyroid cancer. These 60 patients resulted to have larger nodules, more often multiple, solid, hyper/isoechoic, with macrocalcifications (Table 1). A multivariate analysis was performed, considering referral to surgery as the outcome variable, and including all parameters significantly associated with survey at univariate analysis as putative determinants. At this analysis, nodules size was confirmed as significantly associated with referral to surgery (OR 1.05 [1.02–1.08]; p = 0.0001), together with solid composition (OR 3.77 [1.08–13.12]; p = 0.037), hyper/isoechoic pattern (OR 2.23 [1.14–4.37]; p = 0.019) and macrocalfications (OR 2.80 [1.33–5.87]; p = 0.006), though to a lesser degree. The histological outcomes resulted from the old and new TIR3 that underwent surgery are listed in Table 2.
Discussion
The adoption of a new grading system which modified current diagnostic categories can have a relevant impact on clinical practice. In the case of thyroid nodules, cytological classifications affect the proportion of patients referred to surgery. The modification of cytological grading of thyroid nodules, with the distinction of the previous “Indeterminate” category (AUS/FLUS and FN in USA Bethesda system; Thy3a and Thy3f in UK RCPath; and TIR3 in 2010 Italian SIAPEC-IAP grading system) into two distinct categories of “Low” and “High” risk (TIR3A and TIR3B in the new 2014 SIAPEC-IAP Consensus) is aimed at reducing the number of patients with benign nodules referred to surgery.
This retrospective analysis of a large clinical series of nodules shows that the overall proportion of patients classified in TIR3 (TIR3A + TIR3B with the new classification) substantially increased to about 20%, after the modification of the previous SIAPEC system.
The overall increase in TIR3 was associated with a reduction (from 70.9 to 58.8%) of TIR2 nodules. This suggests that, after the introduction of the new classification, some of the nodules previously labeled as TIR2 were prudently classified as TIR3A.
On the other hand, the difference in proportion of TIR2 and TIR3 could have been caused a change in case mix, with a more selected population accessing our tertiary-case Center. Another limitation is that the survey was performed in a single center, where cytological assessment was performed only by local pathologists; it is possible that pathologists from different Centers might have reached different results. Therefore, longitudinal studies verifying the proportion of TIR3 nodules in other clinical Centers are needed. On the other hand, the fact that all the assessments along the time of the survey were performed by the same pathologists is a strength of the study, ruling out the possibility that changes in proportion of TIR3 were determined by changes in the assessors. The subcategory of TIR3B, that has surgical indication, presents a thyroid cancer rate of 40.4%; that is significantly higher than that obtained in patients classified as old TIR3, who underwent surgery before 2014 (28.7%). These results confirm and strengthen the hypothesis that the new SIAPEC classification provides a better specificity in selecting patients with surgical indication. This evidence has also been pointed out by a retrospective study by Rullo et al. [21] that reclassified 290 old TIR3 referred to surgery, into the new subclasses TIR3A and TIR3B, showing a prevalence of thyroid cancer of 10.2 and 43.8%, respectively. Furthermore, this higher percentage of malignancy is in agreement with a recent meta-analysis [22] and the results of two studies performed on a smaller number of patients [23, 24].
On the other hand, a large percentage of TIR3B nodules (about 60%) referred to surgery turns out to be benign. This means that 3 out of 5 patients undergoing surgery receive no benefit from the treatment while being exposed to unnecessary surgical risks. Further, clinical, instrumental or biomolecular parameters with stronger diagnostic correlation need to be identified in this population. Notably, among TIR3B nodules those with Hurthle cell proliferation had a lower rate of positive histology (19.4% vs 44.0% in the rest of TIR3B cases). This finding is consistent with that of Straccia et al. [23], who showed, in a similar series, a lower malignancy rate (9% vs 50%; p < 0.05) [23]. The significance of this cytological finding is still under debate so that Hurthle cell proliferation does not ultimately prove to be a good predictor of either follicular or Hurthle cell carcinoma [25].
Thyroidectomy is not the primary option for TIR3A nodules, so the analysis was limited to patients who underwent surgery. As a consequence, cancer rate in this category is affected by an upstream bias selection: because of the relatively small number of cases undergoing surgery, the present study does not allow any definite estimate of prevalence of malignancy in TIR3A. Apparently, in this case series, the prevalent independent predictor for referral to surgery was the nodule size.
In conclusion, the new SIAPEC classification appears as an advancement in diagnosing thyroid cancer in patients with indeterminate cytology. Nevertheless, considering the high proportion of benign nodules in TIR3B, a more effective strategy is required to better select thyroid nodules deserving surgery.
References
Belfiore A, Rosa GL, Giuffrida D, Regalbuto C, Lupo L, Fiumara A, Ippolito O (1995) The management of thyroid nodules. J Endocrinol Investig 18:155–158
Frates MC, Benson CB, Charboneau JW, Cibas ES, Clark OH, Coleman BG, Cronan JJ, Doubilet PM, Evans DB, Goellner JR, Hay ID, Hertzberg BS, Intenzo CM, Jeffrey RB, Langer JE, Larsen PR, Mandel SJ, Middleton WD, Reading CC, Sherman SI, Tessler FN (2005) Society of Radiologists in Ultrasound Management of thyroid nodules detected at US: Society of Radiologists in ultrasound consensus conference statement. Radiology 237(3):794–800
Hegedüs L (2004) Clinical practice. The thyroid nodule. N Engl J Med 351(17):1764–1771
Tan GH, Gharib H (1997) Thyroid incidentalomas: management approaches to nonpalpable nodules discovered incidentally on thyroid imaging. Ann Intern Med 126(3):226–231
Knobel M (2015) Etiopathology, clinical features, and treatment of diffuse and multinodular nontoxic goiters. J Endocrinol Investig. https://doi.org/10.1007/s40618-015-0391-7
Siegel R, Ma J, Zou Z, Jemal A (2014) Cancer statistic 2014. CA Cancer J Clin 64:9–29
Chen AY, Jemal A, Ward EM (2009) Increasing incidence of differentiated thyroid cancer in the United States, 1988–2005. Cancer 115(16):3801–3807
Mazzaferri EL (1993) Management of a solitary thyroid nodule. N Engl J Med 328(8):553–559
Ali SZ, Cibas ES (2010) The Bethesda system for reporting thyroid cytopathology: definitions, criteria and explanatory notes. Springer, New York
British Thyroid Association, Royal College of Physicians (2014) Guidelines for the management of thyroid cancer. In: Perros P (ed) Report of the thyroid cancer guidelines update group, vol 3. Royal College of Physicians, London
Lobo C, McQueen A, Beale T, Kocjan G (2011) The UK Royal College of Pathologist thyroid fine needle aspiration diagnostic classification is a robust tool for the clinical management of abnormal thyroid nodules. Acta Cytol 55:499–506
Kocjan G, Chandra A, Cross PA et al (2011) The interobserver reproducibility of thyroid fine needle aspiration using the UK Royal College of Pathologists’ classification system. Am J Clin Pathol 135:852–859
Fadda G, Basolo F, Bondi A et al (2010) Cytological classification of thyroid nodules. Proposal of the SIAPEC-IAP Italian Consensus Working Group. Pathological 102:405–408
Nardi F, Basolo F, Crescenzi A et al (2014) Italian consensus for the classification and reporting of thyroid cytology. J Endocrinol Investig 37:593–599
Cooper DS, Doherty GM, Haugen BR, Kloos RT, Lee SL, Mandel SJ, Mazzaferri EL, McIver B, Pacini F, Schlumberger M, Sherman SI, Steward DL, Tuttle RM (2009) American Thyroid Association (ATA) guidelines taskforce on thyroid nodules and differentiated thyroid. Thyroid. https://doi.org/10.1089/thy.2009.0110
Haugen BR, Alexander EK, Bible KC et al (2016) American thyroid association management guidelines for adult patients with thyroid nodules and differentiated thyroid cancer. Thyroid 26(1):1–133
British Thyroid Association, Royal College of Physicians (2007) Guidelines for the management of thyroid cancer. In: Perros P (ed) Report of the thyroid cancer update group, 2nd edn. Royal College of Physicians, London
De Lellis RA, Lloyd RV, Heitz PU, Eng C (eds) (2004) Pathology and genetics of tumors of endocrine organs. IARC Press, Lyon. World Health Organization Classification of Tumors
Edge SB (2010) American Joint Committee on Cancer: AJCC cancer staging manual, 7th edn. Springer, New York
Amin MB (2017) American Joint Committee on Cancer: AJCC cancer staging manual, 8th edn. Springer, New York
Rullo E, Minelli G, Bosco D, Nardi F, Ascoli V (2017) Evaluation of the Italian cytological subclassiication of thyroid indeterminate nodules into TIR-3A and TIR-3B: a retrospective study of 290 cases with histological correlation from a single institution. J Endocrinol Investig. https://doi.org/10.1007/s40618-017-0763-2
Trimboli P, Crescenzi A, Giovanella L (2017) Performance of Italian consensus for the classification and reporting of thyroid cytology (ICCRTC) in discriminating Indeterminate lesions at low and high risk of malignancy. A systematic review and meta-analysis. Endocrine. https://doi.org/10.1007/s12020-017-1382-6
Straccia P, Santoro A, Rossi ED, Brunelli C, Mosseri C, Musarra T, Pontecorvi A, Lombardi CP, Fadda G (2017) Incidence, malignancy rates of diagnoses and cyto-histological correlations in the new Italian reporting system for thyroid cytology: an institutional experience. Cytopathology. https://doi.org/10.1111/cyt.12455
Ulisse S, Bosco D, Nardi F, Nesca A, D’Armiento E, Guglielmino V, De Vito C, Sorrenti S, Pironi D, Tartaglia F, Arcieri S, Catania A, Monti M, Filippini A, Ascoli V (2017) Thyroid imaging reporting and data system score combined with the new Italian classification for thyroid cytology improves the clinical management of indeterminate nodules. Int J Endocrinol 2017:9692304. https://doi.org/10.1155/2017/9692304
Pu RT, Yang J, Wasserman PG, Bhuiya T, Griffith KA, Michael CW (2006) Does Hurthle cell lesion/neoplasm predict malignancy more than follicular lesion/neoplasm on thyroid fine-needle aspiration? Diagn Cytopathol 34(5):330–334
Acknowledgements
All the authors would like to thank Mrs Tania Del Soldato, professional nurse, for her precious help in collecting data.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that there is no conflict of interest regarding the publication of this paper.
Ethical approval
All procedures performed in our study were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
For this type of study formal consent is not required.
Rights and permissions
About this article
Cite this article
Sparano, C., Parenti, G., Cilotti, A. et al. Clinical impact of the new SIAPEC-IAP classification on the indeterminate category of thyroid nodules. J Endocrinol Invest 42, 1–6 (2019). https://doi.org/10.1007/s40618-018-0871-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40618-018-0871-7