Abstract
Purpose
Men affected by multiple sclerosis often experience neurogenic overactive bladder (OAB), lower urinary tract symptoms and erectile dysfunction (ED). The aim of the study was to investigate modifications of urinary and sexual functions after administration of daily tadalafil (TAD) 5 mg.
Methods
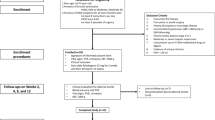
Twenty men were enrolled in a single-blind, 4-week prospective study while 10 men without treatment served as controls. Primary outcomes were changes from baseline of International Prostate Symptom (IPSS), OAB questionnaire (OAB-q-short form) and International Index of Erectile Function (IIEF-5) scores. To evaluate the influence of bladder filling on somatic reflexes, we studied variations of the H-reflex evoked by electrical stimuli applied to the tibial nerve at the popliteal fossa and recorded from the soleus muscle. Also testosterone/estradiol (T/E) ratio was measured before and after treatment.
Results
In TAD group, an improvement in IPSS (p < 0.001), OAB-q (p < 0.001) and IIEF-5 (p < 0.001) scores was found. Also, an increase in Q max (p < 0.01) and T/E ratio (p < 0.01) was found with a concomitant reduction in post-void residual volume (p < 0.001) without any changes in the H-reflex.
Conclusions
The study demonstrates for the first time that daily TAD in patients with multiple sclerosis improves storage symptoms, post-void residual volume, steroid hormone pattern and ED without urodynamic changes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Multiple sclerosis (MS) is most commonly diagnosed among patients aged 20–50 years, with a 2:1 ratio of women versus men [1]. It is primarily characterized by autoimmune demyelination that leads to reduce of neural conduction along axonal pathways through rostral to the lumbosacral level, thus reducing voluntary and supraspinal control of voiding. The lateral corticospinal and reticulospinal cords, in particular, are responsible for innervation of the lower urinary tract. Damage to these pathways can result in detrusor–external sphincter dyssynergia, detrusor overactivity (DO) and detrusor hypocontractility [2]. Indeed the pons or spinal cord demyelination may initially cause an areflexic bladder with complete urinary retention, followed then by a slow development of automatic micturition and neurogenic overactive bladder (OAB) that is mediated by spinal reflex pathways. However, in this case, voiding is commonly inefficient, due to the simultaneous contractions of the bladder and the urethral sphincter (detrusor–sphincter dyssynergia). The incidence of these lower urinary tract symptoms (LUTS) in patients with multiple sclerosis (MS) may be as high as 90 %.
Patients with MS can experience any number of LUTS, including urgency, frequency, incontinence, hesitancy and retention [3, 4]. Even if it is uncommon for LUTS to be the presenting complaint that leads to the diagnosis of MS (fewer than 10 %), the prevalence of LUTS during the disease course is very high, ranging from 60 to 86 % for urgency, from 50 to 83 % for frequency, from 19 to 83 % for incontinence, from 28 to 58 % for hesitancy and from 2 to 20 % for retention [5, 6]. The OAB is a well-recognized, chronic and distressing medical condition characterized by urinary urgency and frequency, with or without incontinence. Symptoms secondary to DO may be responsible for discomfort, shame and loss of self-confidence; in neurogenic patients, who already often present limited autonomy, this urinary distress can determine a complete social withdrawal. The OAB, defined either symptomatically as the OAB syndrome or urodynamically as DO, is a bladder filling disorder. To exert normal bladder control, adequate sensory input to the central nervous system is necessary, and it is well established that changes in sensory mechanisms might give rise to disturbances in bladder function. Therefore, pharmacological control of bladder contraction has focused on how afferent nerve activity is generated peripherally and handled by the CNS. Several factors might contribute to the genesis of OAB, and at least two afferent signaling pathways in the bladder can be identified, the “myogenic” and the “urothelial” pathway [7].
Mechanisms leading to an increased activity in afferent nerves might be interesting targets for drugs aimed at controlling sensory and motor activity of the bladder. It is now widely accepted that antimuscarinic drugs, which are still first-line treatment of OAB/DO, exert effects on afferent signaling important for their clinical efficacy [8]. Recently, tadalafil (TAD) has been approved for the treatment of erectile dysfunction (ED) and LUTS secondary to benign prostate hyperplasia (BPH), but little is known about its mechanism of action.
Randomized clinical trials have shown significant improvement in urinary symptoms, and the drug is well tolerated [9]. The aim of the present study will be to evaluate modifications of voiding dysfunction after daily TAD administration in men with MS who complain some degree of ED.
Materials and methods
In a 4-week prospective, single-blind controlled study at a single hospital, 30 men with confirmed diagnosis of MS (primary progressive, relapsing-remitting or secondary progressive), bladder symptoms caused by DO (as defined by the International Continence Society) and ED were enrolled into the study. The protocol was approved by the Internal Review Board of the Sapienza University of Rome. After signing an informed consent, twenty men agreed to receive daily TAD 5 mg, whereas ten men refused treatment due to personal (lack of female partner) or other barriers and served as control group.
Inclusion criteria were: MS male subjects referring LUTS of any severity; age >30 and <55; presence of ED of any severity; absence of any concomitant treatment for OAB symptoms. Exclusion criteria: presence of hypogonadism; Q max <4 mL/s at uroflowmetric study; anticoagulant therapy or medication regimen that may interfere with transmission at the neuromuscular junction (e.g., aminoglycosides); any contraindications to the daily use of PDE5 inhibitors (concomitant use of nitrates, NHYA III class or more, cardiac disease) [10]; history for optic neuritis or visual disturbances at any stage of severity. At baseline and after treatment, each patient was administered the International Prostate Symptom Score (IPSS) questionnaire, the OAB questionnaire (OAB-q) short form for measuring the impact of OAB symptoms on health-related quality of life [11] and the validated five-item version of the International Index of Erectile Function (IIEF-5) questionnaire. Then, patients were submitted to the following diagnostic workup: history; general and neurological physical examination; urinalysis and urine culture and uroflowmetry. These latter parameters were measured by the maximum flow rate maintained for 2 s (Q max) with a minimal voided volume of 150 mL (MicroFlow II®) and post-void residual (PVR) volume after micturition (as evaluated by ultrasound) was also investigated. Also baseline and post-treatment plasma assays for total testosterone and 17-beta-estradiol (E2) were evaluated. Total testosterone was measured by electrochemiluminescence (Immulite 2000, Siemens, Milan, Italy; within- and between-assay coefficients of variation were 5.1 and 7.2 %, respectively), and E2 was measured with chemiluminescent enzyme immunoassays (Architet Systems, Abbott Diagnostics, Germany) [12].
Neurophysiologic assessment
Each patient was first submitted to urodynamic evaluation which included flowmetry, cystometry and a pressure-flow study (urodynamic test) with simultaneous concentric needle electromyography of the pelvic floor, as previously published [13].
Stimulation techniques
M wave and H-reflex the right tibial nerve was stimulated at the popliteal fossa with bipolar electrical stimuli and the subjects lying supine. The anode was positioned just above the patella, for selective stimulation of the nerve trunk. Electrical stimuli were delivered at an intensity able to produce a maximal M wave in the soleus muscle. The soleus H-reflex was also collected using a 1-ms rectangular pulse generated by a constant current. To avoid habituation, the stimulator was randomly triggered about once every 20 s. The intensity was set to evoke a maximal H-reflex size. Ten trials were collected for each condition.
Recording techniques
EMG signals were recorded and filtered with a Micromed Myoquick 1400 device (Micromeds p.a., Italy) (bandwidth 20 Hz–1 kHz) and analyzed off-line. For the H-reflex study, the active electrode was placed over the soleus muscle just medial to the tibia, half way from the tibial tubercle to the medial malleolus, and the reference electrode over the Achilles tendon medial and proximal to the medial malleolus. Muscle relaxation was monitored with the aid of an audio–visual feedback. The H-reflex/M wave (H/M) ratio was then calculated to evaluate motor neuron excitability as previously published [15].
Statistical analysis
Clinical and biochemical data were compared before and after treatment. Data are expressed as means ± standard errors (SEM) only when normally distributed and as median [quartiles] when nonparametric. Kolmogorov–Smirnov test has been used to test the parameter distribution. Paired t test and Wilcoxon test (for parametric and nonparametric distributed parameters, respectively) have been used to test the parameter changes during the study. A p value 0.05 was taken as statistically significant. Statistical analysis was performed using the computer statistical package SPSS/22.0 (SPSS, Chicago, IL, USA).
Results
Patient characteristics at baseline are shown in Table 1. TAD determined a significant improvement in mean scores of IPSS (p < 0.001) and OAB-q SF4 (p < 0.001) questionnaires when compared with baseline and controls (Table 2). As expected, an improvement in IIEF-5 (p < 0.001) only in the treated group was found (Table 2). Also, improvements in uroflow parameters as expressed by Q max (p < 0.01) and reduction in PVR volume (p < 0.001) as measured by ultrasound technique were observed in TAD group (Table 2). No variation in prostate volume was found in both groups (as evaluated by US). Interestingly, TAD assumption caused a significant improvement in T/E ratio (p < 0.01). No variation in questionnaires, urodynamic tests, PVR or hormonal modifications was found in the control group (Table 2). In both groups, H-reflex paired, one-way ANOVA showed no significant differences in the H/M ratio between before and after therapy. (H/M ratio 0.54 ± 0.08 vs. 0.57 ± 0.08, respectively). Side effects were those commonly reported with TAD administration (headache and myalgia) and did not determine drug discontinuation (data not shown).
Discussion
To our best knowledge, the present pilot study is the first one aimed to investigate the effects of TAD on urinary and sexual functions in men with MS. In the present series of patients, LUTS may represent the mirror of an established human model of OAB, and this might be the cause of urinary and sexual distress occurrences despite the young age. In addition to improvements in erectile function, we firstly demonstrated that after a short period of daily TAD (4 weeks), a significant improvement in OAB and all domains of IPSS questionnaires were obtained. As previously described by other authors [14], we confirmed a significant improvement in erectile function and sexual satisfaction during treatment. Interestingly, the net improvements in questionnaires were paralleled by an improvement in PVR volume as evaluated by ultrasound, and improvements in testosterone-to-estradiol ratio in plasma mainly due to reduction in estradiol levels. Neurological features, i.e., H/M ratio, were similar before and after TAD administration. Because TAD left the H/M ratio unchanged, we consider unlikely that TAD-induced changes in the bladder DO could be mediated by changes in non-specific spinal neuron excitability. Hence, we cannot exclude that TAD might probably have modulated others specific neuronal pathways.
It is well documented that PDE5i improves male LUTS, independently from the presence of ED. The exact mechanisms by which these beneficial effects are exerted have still not been established, but this has stimulated research activities with respect to the different signaling pathways controlling the function of the lower urinary tract [15]. PDE5 is expressed and has biological activity in all parts of the genitourinary tract, but with respect to its role in LUTS pathophysiology, focus has been on the prostate, bladder and urethra [16, 17]. Although PDE5 inhibition in vitro can relax the smooth muscle of the lower urinary tract, and specifically the outflow region, the symptom score improvements have not been associated with significantly improved urinary flow rates [18]. Caremel et al. evaluated the role of the NO/cGMP signaling pathway on the micturition reflex in a model of bladder hyperactivity associated with C-fiber activation in the rat. They confirmed that compounds inhibiting the NO/cGMP pathway might increase bladder overactivity, whereas compounds activating the NO/cGMP pathway may inhibit it [19]. Similar studies have found that nitric oxide generation of cGMP might be the key step in the NO/cGMP pathway responsible for PDE5 inhibition of bladder overactivity [20, 21]. Several lines of evidence suggest that PDE5 inhibition might affect afferent signaling in vitro and in vivo [22]. PDE5 increases the accumulation of cGMP, which in turn stimulates the increased PKG activity, which might decrease influx through N-type voltage-gated Ca2+ channels in afferent nerve terminals, resulting in decreased neuropeptide release [23]. This would also reduce positive feedback on presynaptic NK1 and NK2 receptors, which might decrease afferent firing [24]. Minagawa et al. [25] found that TAD decreased afferent signaling in Ad and C-fibers in response to both bladder filling and hyperactivity caused by acrolein-induced cystitis with no change in bladder tone. This decrease in afferent signaling seemed to be related to PDE5 inhibitor-mediated increased activity in the NO/cGMP pathway, as the administration of l-arginine inhibited Ad and C-fiber firing, whereas the NOS inhibitor, L-NAME, increased afferent activity [26]. It might be questioned whether a direct effect on afferent nerves is the only mechanism by which PDE5 inhibitors influence afferent signaling. In addition, PKG mediates the synchronization of relaxation muscle through the inhibition of Rho-ROCK system and consequently the maintenance of dephosphorylated state of myosin light chain (MLC).
Bladder of both genders expresses high level of PDE5 and a similar distribution of sex steroid receptors and animal studies demonstrate that the activity of the selective and potent PDE5 inhibitor, vardenafil, in potentiating SNP-induced relaxation is almost three times more pronounced in male than in female rat bladder [27] and was associated with an increased T:E2 ratio, thus suggesting that the male bladder could be regarded as a more suitable target for PDE5i than the female counterpart. Interestingly, continuous TAD administration in men with ED determined similar modification in T:E2 ratios, by determining a reduction in plasmatic estradiol levels, thus hypothesizing a possible direct effect of TAD on aromatase expression and activity [28]. In the present study, we confirmed a reduction in plasma estradiol levels with a consequent increase in T:E2 ratio, and this hormonal modification may be one of the potential mechanism(s) implicated in the amelioration of bladder function in the absence of neuro-urodynamic modifications. In fact, estrogen more than androgen receptors are known to up-regulate RhoA/ROCK signaling. Since an altered estrogen/androgen ratio characterizes conditions often associated with LUTS such as aging, obesity and metabolic syndrome, we speculate that a relative reduction in plasma estrogens could be one of potential mechanisms that may reduce bladder overactivity through the up-regulation of RhoA/ROCK pathway.
Limitations
Our study had no matching placebo treatment arm, due to the fact that this was a spontaneous, observational in-office study based on newest approved treatment for neurogenic bladder MS patients in our country.
Due to the gender incidence of the disease (female more than male affected), and to the presence of initial MS symptoms, data were obtained on a small number of patients. For this reason, we cannot state whether ED status could have appreciably influenced TAD treatment response.
Finally, limited neurological investigations were performed; hence, we cannot exclude another neurogenic/reflexogenic pathway involved in the effects described. Despite this, the results appear to be promising when compared with the control group, suggesting that broader studies are necessary to clarify the exact mechanism of action of TAD in MS patients.
Conclusions
OAB is a filling disorder in which abnormal sensations leads to urinary urgency, frequency and incontinence. The afferent signaling pathways that regulate micturition play a central role in the pathogenesis of OAB, and thus represent important targets therapy for patient affected by initial stages of MS. TAD shares a central role such as the possibility of either an inhibition of afferent signaling from the bladder or a bladder neck relaxant myogenic effect and might represent a new therapeutic approach to these patients. This pilot study is the first demonstration that TAD is able to improve both LUTS and ED of any severity in patients with multiple sclerosis and significantly improved their quality of life.
References
Leboeuf L, Cohen B, Gousse AE (2008) Multiple sclerosis. In: Corcos J, Schick E (eds) Textbook of the neurogenic bladder. CRC Press, Boca Raton, pp 294–311
Oppenheimer DR (1978) The cervical cord in multiple sclerosis. Neuropathol Appl Neurobiol 4:151–162
Fernandez O (2002) Mechanisms and current treatments of urogenital dysfunction in multiple sclerosis. J Neurol 249:1–8
Quarto G, Autorino R, Gallo A et al (2007) Quality of life in women with multiple sclerosis and overactive bladder syndrome. Int Urogynecol J Pelvic Floor Dysfunct 18:189–194
Ebers GC, Sadovnick AD, Risch NJ (1995) A genetic basis for familial aggregation in multiple sclerosis. Canadian Collaborative Study Group. Nature 377:150–151
Poser CM (1994) The epidemiology of multiple sclerosis: a general overview. Ann Neurol 36:S180–S193
Kanai A, Andersson KE (2010) Bladder afferent signaling: recent findings. J Urol 183:1288–1295
Andersson KE (2011) Antimuscarinic mechanisms and the overactive detrusor: an update. Eur Urol 59:377–386
Chapple CR, Roehrborn CG, McVary K et al (2015) Effect of tadalafil on male lower urinary tract symptoms: an integrated analysis of storage and voiding international prostate symptom subscores from four randomised controlled trials. Eur Urol 67:114–122
Pofi R, Gianfrilli D, Badagliacca R et al (2016) Everything you ever wanted to know about phosphodiesterase 5 inhibitors and the heart (but never dared ask): How do they work? J Endocrinol Invest 39:131–142
Burks J, Chancellor M, Bates D et al (2013) Development and validation of the actionable bladder symptom screening tool for multiple sclerosis patients. Int J MS Care Winter 15:182–192
Radicioni A, Lenzi A, Spaziani M et al (2013) A multicenter evaluation of immunoassays for follicle-stimulating hormone, luteinizing hormone and testosterone: concordance, imprecision and reference values. J Endocrinol Invest 36:739–744
Conte A, Bettolo CM, Onesti E et al (2009) Cannabinoid-induced effects on the nociceptive system: a neurophysiological study in patients with secondary progressive multiple sclerosis. Eur J Pain 13:472–477
Lombardi G, Macchiarella A, Del Popolo G (2010) Efficacy and safety of tadalafil for erectile dysfunction in patients with multiple sclerosis. J Sex Med 7:2192–2200
Bruzziches R, Francomano D, Gareri P et al (2013) An update on pharmacological treatment of erectile dysfunction with phosphodiesterase type 5 inhibitors. Expert Opin Pharmacother 14:1333–1344
Uckert S, Stief CG (2011) Treatment of erectile dysfunction and lower urinary tract symptoms by phosphodiesterase inhibitors. Handb Exp Pharmacol 204:307–322
Andersson KE, Uckert S, Stief C et al (2007) Phosphodiesterases (PDEs) and PDE inhibitors for treatment of LUTS. Neurourol Urodyn 26:928–933
Yoshimura N, Skei S, de Groat WC (2001) Nitric oxide modulates Ca(2+) channels in dorsal root ganglion neurons innervating rat urinary bladder. J Neurophysiol 86:304–311
Caremel R, Oger-Roussel S, Behr-Roussel D et al (2010) Nitric oxide/cyclic guanosine monophosphate signaling mediates an inhibitory action on sensory pathways of the micturition reflex in the rat. Eur Urol 58:616–625
Persson K, Igawa Y, Mattiasson A et al (1992) Effects of inhibition of the l-arginine/nitric oxide pathway in the rat lower urinary tract in vivo and in vitro. Br J Pharmacol 107:178–184
Sesatomi K, Hiragata S, Miyazato M et al (2008) Nitric oxide-mediated suppression of detrusor overactivity by arginase inhibitor in rats with chronic spinal cord injury. Urology 72:696–700
Artim DE, Kullman FA, Daughtery SL et al (2009) Activation of the nitric oxide-cGMP pathway reduces phasic contractions in neonatal rat bladder strips via protein kinase G. Am J Physiol Renal Physiol 297:F333–F340
Kanai A, Zabbarova I, Oefelein M et al (2012) Mechanisms of action of botulinum neurotoxins, b3-adrenergic receptor agonists, and PDE5 inhibitors in modulating detrusor function in overactive bladders: ICI-RS 2011. Neurourol Urodyn 31:300–308
Sculptoreanu A, Artim DE, de Groat WC (2009) Neurokinins inhibit low threshold inactivating K+ currents in capsaicin responsive DRG neurons. Exp Neurol 219:562–573
Minegawa T, Aizawa N, Igawa Y et al (2012) Inhibitory effects of phosphodiesterase 5 inhibitor, tadalafil, on mechanosensitive bladder afferent nerve activities of the rat and on acrolien-induced hyperactivity of these nerves. BJU Int 110:E259–E266
Aizawa N, Igawa Y, Nishizawa O et al (2011) Effects of nitric oxide on the primary bladder afferent activities of the rat with and without intravesical acrolein treatment. Eur Urol 59:264–271
Vignozzi L, Filippi S, Morelli A et al (2012) Testosterone/estradiol ratio regulates NO-induced bladder relaxation and responsiveness to PDE5 inhibitors. J Sex Med 9:3028–3040
Greco EA, Pili M, Bruzziches R et al (2006) Testosterone:estradiol ratio changes associated with long-term tadalafil administration: a pilot study. J Sex Med 3:716–722
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All the authors have no conflict of interest.
Ethical approval
The research involves human participants.
Informed consent
Each subject signed a detailed informed consent before entering the study.
Additional information
D. Francomano and A. Ilacqua have contributed equally to this article.
Rights and permissions
About this article
Cite this article
Francomano, D., Ilacqua, A., Cortese, A. et al. Effects of daily tadalafil on lower urinary tract symptoms in young men with multiple sclerosis and erectile dysfunction: a pilot study. J Endocrinol Invest 40, 275–279 (2017). https://doi.org/10.1007/s40618-016-0557-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40618-016-0557-y