Abstract
Objective
To determine the characteristics of curricula for teaching the content of clinical practice guidelines (CPGs) in psychiatric residency and child and adolescent fellowship programs as well as to determine if and how the learning of CPG content is applied in clinical care settings.
Methods
We conducted a national online survey of directors of general psychiatry residency and child and adolescent fellowship programs in the USA. The survey questionnaire included 13 brief questions about the characteristics used to teach CPGs in the programs, as well as two demographic questions about each program and director. Descriptive statistics were reported for each questionnaire item by program classification (i.e., child and adolescent vs. general psychiatry).
Results
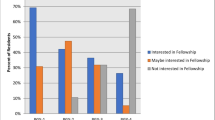
The survey response rate was 49.8 % (146 out of 293). Just 23 % of programs reported having written goals and objectives related to teaching CPGs. The most frequently taught aspect of CPGs was their content (72 % of programs). Didactic sessions were the most frequently employed teaching strategy (79 % of programs). Regarding the application of CPG learning in treatment care settings, just 16 % of programs applied algorithms in care settings, and 15 % performed evaluations to determine consistency between CPG recommendations and care delivery. Only 8 % of programs utilized audit and feedback to residents about their adherence to CPGs. Faculty time constraints and insufficient interest were the leading barriers (39 % and 33 % of programs, respectively) to CPG teaching, although 38 % reported no barriers. However, child and adolescent programs less commonly identified insufficient interest among faculty as a barrier to teaching CPGs compared to general programs (20 % vs. 43 %). Moreover, compared to general programs, child and adolescent fellowship programs taught more aspects of CPGs, used more educational activities to teach the content of specific CPGs, and used more methods to evaluate the teaching of CPGs.
Conclusions
Although the majority of programs provided some teaching of CPGs, the rigorousness of the teaching approaches was limited, especially attempts to evaluate the extent and effectiveness of their use in clinical care. Child and adolescent fellowship programs provided more extensive teaching and evaluation related to CPGs.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The use of clinical practice guidelines (CPGs) has been shown to improve patient outcomes in a variety of medical conditions, including breast cancer [1], uncomplicated urinary tract infection in women [2], and community-acquired pneumonia [3]. In the area of mental health, guideline implementation by clinicians has also shown positive effects on patient outcomes. Patients in opioid substitution treatment clinics showed greater reductions of substance abuse and greater improvement in mental health when consistently treated with guideline recommendations [4]. Guideline-concordant pharmacotherapy for primary care patients with persistent depressive symptoms is associated with greater symptom reduction and recovery rates than usual care [5]. The Texas Medication Algorithm Project showed that consensus, algorithm-based treatment was better than treatment as usual for reducing symptom severity and mental health-related functional status in outpatients with depression [6], improving overall psychiatric symptoms in outpatients with a history of mania [7], and improving cognition and overall symptoms in outpatients with schizophrenia [8].
Despite the knowledge that CPGs can improve patient outcomes, they receive limited use in routine clinical care, including areas such as colorectal cancer screening [9], diagnosing and managing uncomplicated urinary tract infection [10], screening and managing chronic kidney disease [11], and monitoring metabolic side effects of people treated with antipsychotic medication [12].
The uncommon use of CPGs in clinical care may result, at least in part, from shortcomings in guideline education during physician training. A recent survey conducted by Akl et al. on directors of family and internal medicine residency programs found that 5 % of programs provided no teaching of CPGs, 24 % did not teach content of guidelines, and 66 % did not assess resident utilization of guidelines in care delivery [13]. Furthermore, the effectiveness of the method most frequently used to teach CPGs, traditional didactic sessions, may be less than that of evidence-based educational approaches [14].
Several authors have written about the potential advantages of utilizing practice guidelines as a core source of the psychiatric resident curriculum [15–17]. In 2002, Garfield et al. [16] tested the impact of utilizing resident-led, small groups to teach the American Psychiatric Association (APA) Practice Guidelines material, finding improvement in post-study test scores and survey results indicating a generally positive “grading” of the approach by residents (overall rating by residents of a “B”). Our group reported on an experience of implementing the APA guidelines in psychiatric residency training using a traditional lecture presentation format by faculty [18]. The “grading” of our program’s approach [18], as a whole, was similar to that of Garfield et al. [16]. Additional findings were that the CPGs were deemed by residents to be modestly more helpful for teaching pharmacologic than psychosocial interventions and too lengthy for optimal learning in the full guideline form [18]. Osser et al. described a comprehensive psychopharmacology course in which CPGs were a key component, with high ratings of satisfaction for the course overall [17]. In two recent publications [19, 20], Falzer and Garman reported on the use of CPGs as decision aids, along with patient-specific information, in psychiatric residents’ treatment recommendations for case vignettes of various scenarios. For each vignette, residents indicated whether they endorsed the guideline's recommendation. Although decisions were consistent for relatively simple cases, when cases were more ambiguous or proposed treatments risky, resident strategies became complex and relatively inconsistent, suggesting that the incorporation of guideline information into decision-making is influenced by multiple sources of information (e.g., patient preferences) [19, 20].
Enhancing the teaching of CPGs during resident and fellow education may also help programs achieve at least three of the six competency program requirements of the Accreditation Council for Graduate Medical Education (ACGME): [1] practice-based learning and improvement, [2] medical knowledge, and [3] patient care [21, 22]. Learning of guidelines during early stages of career development could also potentially enhance their use by physicians after graduation.
We set out to expand on the survey work of Akl et al. by evaluating two groups of psychiatric programs: general adult residents and child and adolescent fellows. The purpose of this study was to examine the characteristics of curricula for teaching the content of CPGs in general adult psychiatric residency versus child and adolescent fellowship programs throughout the USA. In addition, we sought to further the previous research by identifying if and how CPG content is applied in the teaching of residents and fellows in clinical care settings. A historical comparison to family and internal medicine programs as published by Akl et al. [13] was also provided.
Methods
Participants
Directors of general psychiatry residency (n = 173) and child and adolescent fellowship (n = 120) programs in the USA were invited to participate in a survey study. The survey response rate was 49.8 % (146 out of 293). Directors were identified using the ACGME online website. The institutional review board at the University of Texas Southwestern Medical Center at Dallas approved the study.
Study Design
The survey questionnaire, which was adapted with permission from one used in a prior study [13] of family and internal medicine programs, included fifteen brief, multiple-choice questions about the use of CPGs in each director’s training program. Specifically, the questionnaire included eight questions about the characteristics used to teach CPGs, five additional questions about the characteristics of each residency program, one question about the program director’s gender, and one question about the number of years as program director (the complete questionnaire will be provided upon request).
Participants were contacted by email and invited to participate in the survey in August 2010. The initial email briefly explained the purpose of the online survey and requested their participation in the study. By clicking on a link embedded in the email, participants were directed to the online survey website, SurveyMonkey, which hosted the study survey. Three follow-up emails were sent 2, 4, and 7 weeks after the initial invitation. One week after the last follow-up email was sent, an additional email was sent to all partial responders requesting for their complete response.
Data Analysis
Descriptive statistics were reported for each questionnaire item. For the continuously measured survey items (questions 12 and 15), the sample mean and standard deviation were reported. For the categorical items, one-way to k-way frequency and cross-tabulation tables were reported. Also, 2 × k cross-tabulation (contingency) tables for the frequency of each survey item (stratified) by program classification (child/adolescent fellowship vs. general psychiatry) were reported. Simple logistic regression was also used to examine the relationship between program type (binary indicator: child/adolescent fellowship vs. general psychiatry) and the binary response of each “teaching content of specific CPGs” and “support for use of CPGs,” respectively. The level of significance for all tests was set at α = .05 (two-tailed).
Results
Characteristics of Programs and Program Directors
General psychiatry residency programs were most commonly reported to be university based (65 %) and located in the Northeast (35 %) with an average of about 30 residents (SD = 12.1). Child and adolescent fellowship programs were also most commonly reported to be university based (77 %) and primarily located in the northeast (29 %) and south (29 %) with an average of about 9 residents (SD = 6.8). In the survey of 146 directors of general psychiatry and child and adolescent programs, 85 indicated that less than 25 % of their residents were international medical graduates. Program directors of each specialty averaged about 7 years (SD = 5.9) of directorship; general psychiatry directors were predominately male (63 %), whereas child and adolescent directors were predominantly female (58 %).
Characteristics of Curricula for Teaching the Content of CPGs
Table 1 describes the characteristics used to teach CPGs combined and separately for each program. Survey responders indicated that only 23 % of programs had written goals and objectives for teaching CPGs. The two most frequently taught aspects of CPGs were the content of specific CPGs (72 %) and identifying and locating CPGs (69 %). Of responding directors, 13.6 % reported teaching no aspect of CPGs.
The most frequently used educational activity was traditional didactic sessions (79 %), with paper copies being the most reported method to make CPG texts available to residents (54 %). Although 53 % percent of programs provided some form of support for the use of CPGs in clinical care, their use in actual care appeared to be quite limited as an educational tool. The top strategy used to support CPG content to clinical care was providing brief CPG summaries (18 %). Sixteen percent of programs supported the use of CPGs by “applying algorithms” in care; 15 % provided performance evaluations to ascertain if clinical care was consistent with CPG recommendations; and 4 % utilized computerized decision support systems to aid the use of CPGs in clinical care.
The most frequent barrier to teaching the content of CPGs was time constraints on faculty (39 %). Thirty-eight percent of program directors reported having no barriers to teaching CPGs with their residents.
A comparison of psychiatry program types on the teaching of CPGs found that child and adolescent fellowship programs utilized more extensive teaching approaches than general psychiatry programs including: teaching the content of specific CPGs (82 % vs. 64 %, p = 0.02), the use of didactic sessions (88 % vs. 72 %; p = 0.02), making CPG texts available to residents (71 % vs. 53 %; p = 0.03), and the email distribution of CPGs (48 % vs. 21 %; p = 0.0008). Child and adolescent programs also less commonly identified insufficient interest among faculty as a barrier to teaching CPGs (20 % vs. 43 %, p = 0.004).
Discussion
We conducted a national survey of general psychiatry and child and adolescent fellowship directors to determine the characteristics of curricula for teaching the content of Clinical Practice Guidelines (CPGs) in each director’s program and to see if and how the CPG content is applied to residents and fellows in clinical care settings. Although most programs provided some teaching related to CPGs (72 %), the rigor with which they were taught was limited. Only a minority of programs used specific goals and objectives when teaching CPGs. Similarly, the most common form of teaching, use of traditional passive didactic sessions, is considered inferior to more well-supported teaching approaches in medicine [23], questioning the impact that current teaching may have on the learning of CPGs by residents in the USA. Just 8 % of programs utilized audit and feedback, an evidence-based learning approach [23], to teach CPGs.
Perhaps most limiting to the impact of training on the future use of CPGs by psychiatrists in clinical care were findings that 16 % of programs applied algorithms in resident care settings; 15 % performed evaluations to determine consistency between CPG recommendations and care delivery, and only 7 % evaluated resident CPG knowledge through auditing of adherence to use in actual care. These findings appear to indicate that a minority of programs actively use or reference CPGs in care provided by residents. Thus, it is likely that the opportunity to learn skills necessary to use CPGs as a tool in clinical care are currently lacking in most programs. These findings suggest a considerable gap in the evidence-based practice instruction of psychiatric residents compared to that of internal medicine and family practice programs. It seems likely that senior institutional support for such teaching is different between these program types and may result from multiple potential sources. Program leaders may have fewer faculty available to teach evidence-based care approaches in psychiatric programs as identified in this study. Psychiatric program leaders may also themselves have less experience with research and evidence-based practice approaches than their counterparts in internal medicine and family practice, lessoning their ability to best support instruction in these areas.
In comparison to general programs, child and adolescent fellowship programs taught more aspects of CPGs, used more educational activities to teach the content of specific CPGs, and used more methods to evaluate the teaching of CPGs. Support for use in clinical care settings was not different in the program types (general vs. child and adolescent). We did not posit any a priori directional hypothesis about the potential differences between adult psychiatry residency and child and adolescent psychiatry training programs. A partial list of potential explanations for the greater use of CPGs in the teaching of child and adolescent fellowship programs could include, relative to general psychiatry residency programs, more support for evidence-based teaching including CPG use, a more advanced level of training allowing for more extensive education of available resources, and an enhanced “ownership” of association-recommended guidelines compared to more “general” psychiatric residency training programs. Although we did not evaluate the use of CPGs in other psychiatry fellowship subspecialties (geriatric, addiction, etc.), these findings might predict a greater use of CPGs in these areas compared to general psychiatry programs, especially considering the highly-focused content of their learning and potentially greater affiliation with a specialized discipline.
A few key similarities were found between the teaching of CPGs by psychiatry programs in our study and family and internal medicine programs previously reported by Akl et al. [13], including the proportion providing at least some CPG teaching, aspects of CPGs taught, and the use of traditional didactic lecture sessions as the primary teaching approach for CPGs. Family and internal medicine programs, however, were more likely than psychiatry programs (as reported in our study) to make CPGs available through a website of the program or an affiliated hospital, and were less likely to encounter “a lack of interest” among faculty as a barrier to the teaching of CPGs. Of particular importance, family and internal medicine programs were much more likely than psychiatry programs to audit adherence guideline use in patient care (44 % of family/internal medicine programs vs. 7 % of psychiatry programs). This specific difference is concerning and further highlights challenges psychiatry training programs may have in aiding trainees translating CPGs to tools in clinical care. As electronic medical records become universal, computerized decision support systems may provide an opportunity to expand CPG use in clinical care [24] and may create an ideal learning experience for trainees by making the evidence provided by CPGs available to residents in a real-time manner as they make clinical care decisions.
The two most reported barriers to teaching CPGs involve faculty: time constraints and insufficient interest. If institutions could make CPGs more easily accessible (e.g., online access and online tutorials provided directly to residents) and thereby less time-consuming for faculty to teach, perhaps guidelines would be taught more widely. Insufficient interest by faculty might easily be addressed by identifying one or few faculty with interest in the topic area as part of the resident curriculum. Insufficient interest may be a far more challenging issue when attempting to incorporate guideline teaching into routine care at clinical sites where local site faculty are responsible for teaching. Additional measures, including audit and feedback regarding care delivery, which has been shown to improve knowledge in practicing physicians [23] could perhaps be used in the team care of psychiatric residents and faculty, increasing buy-in from faculty.
This study has several strengths. It used an existing survey that allows a comparison to CPG teaching in family and internal medicine programs [13]. In addition, our response rates of 49.8 % and 54 % from general psychiatry and child and adolescent fellowship directors, respectively, neared or surpassed a recommended 50 % response rate for surveys published in medical journals [25]. However, a lack of response from approximately half of directors might lead to a bias in results, particularly if directors who actively use CPGs in their residency and fellowship programs were more likely to respond to our survey. Therefore, it could be implied that our results are not fully representative of all general psychiatric residency and child adolescent fellowship programs throughout the country. Finally, our decision to use an electronic survey instead of a mailed survey may have dissuaded some directors from completing it online.
In conclusion, we found that while guidelines of care are taught in the majority of psychiatry residency programs, the rigorousness of the teaching approaches is lacking, especially attempts to evaluate the extent and effectiveness of their use in clinical care. In contrast, family and internal medicine programs [13] are much more likely to audit resident use of guidelines in actual care delivery, suggesting that guidelines are more commonly used in care delivery of these programs. Our findings indicate that guidelines improve care outcomes, including those with mental disorders [6–8], and thus, suggest that additional efforts should be made in the teaching and clinical care use of CPGs during psychiatric training.
Finally, on the basis of the findings of the current study and those from previous research, we offer the following suggestions regarding a “model curriculum” for the teaching of CPGs. A model curriculum should include communication of the importance of learning CPGs and other evidence-based practices by senior program leaders; make available brief summaries of guidelines to enhance learning of full guideline versions, and provide access to CPGs and their summaries in readily-accessible electronic form. Leading candidates for teaching approaches involve active learning methods (not passive lecture format) such as small-group and team-based learning [26], repeated self-testing (especially retrieval practice) [27], and the use of technology-enhanced simulation training [28]. Finally, we believe that the greatest learning impact will result from successful integration and utilization of CPGs in routine care coupled to the monitoring of charts along with feedback to residents regarding the fit of their care delivery compared with CPG recommendations. Such an approach would require residents to understand current evidence related to their care decisions and think critically about how this evidence is best applied in the care of individualized patients.
Implications for Educators |
• Clinical practice guidelines (CPGs) are currently being taught in the majority of general psychiatry and child and adolescent fellowship programs across the USA. |
• In comparison to general psychiatry programs, child and adolescent fellowship programs provide more extensive teaching and evaluation related to CPGs. |
• Attempts to evaluate the extent and effectiveness of CPG use in clinical care settings are lacking in both programs, a contrast from what family and internal medicine residency programs are currently doing in auditing adherence to guideline use in patient care. |
• CPGs improve clinical care outcomes, and efforts should be made in the teaching and clinical care use of CPGs during psychiatric training. |
Implications for Academic Leaders |
• Although guidelines of care are taught in the majority of general psychiatry and child and adolescent fellowship programs in the USA, the rigorousness of teaching approaches is lacking, especially attempts to evaluate the extent and effectiveness of their use in clinical care. |
• Family and internal medicine programs across the USA are much more likely to audit resident use of guidelines in actual care delivery than psychiatry programs. |
• CPGs improve clinical care outcomes, and efforts should be made in the teaching and clinical care use of CPGs during psychiatric training. |
• A model curriculum for teaching CPGs would involve active learning methods, including communication of the importance of learning CPGs by senior program leaders and making available brief summaries of guidelines in readily-accessible electronic form. |
• Successful integration and utilization of CPGs in routine care coupled with chart monitoring and feedback to residents regarding the fit of their care delivery compared with CPG recommendations should provide the greatest learning impact. |
References
Herbert-Croteau N, Brisson J, Latreille J, et al. Compliance with consensus recommendations for systemic therapy is associated with improved survival of women with node-negative breast cancer. J Clin Oncol. 2004;22:3685–93.
Saint S, Scholes D, Fihn SD, et al. The effectiveness of a clinical practice guideline for the management of presumed uncomplicated urinary tract infection in women. Am J Med. 1999;106:636–41.
Dean NC, Silver MP, Bateman KA, et al. Decreased mortality after implementation of a treatment guideline for community-acquired pneumonia. Am J Med. 2001;110:451–7.
Trafton JA, Humphreys K, Harris AH, Oliva E. Consistent adherence to guidelines improves opioid dependent patients’ first year outcomes. J Behav Health Serv Res. 2007;34(3):260–71.
Katon W, Von Korff M, Lin E, et al. Stepped collaborative care for primary care patients with persistent symptoms of depression: a randomized trial. Arch Gen Psychiatry. 1999;56(12):1109–15.
Trivedi MH, Rush AJ, Crismon ML, et al. Clinical results for patients with major depressive disorder in the Texas Medication Algorithm Project. Arch Gen Psychiatry. 2004;61(7):669–80.
Suppes T, Rush AJ, Dennehy EB, et al. Texas Medication Algorithm Project, phase 3 (TMAP-3): clinical results for patients with a history of mania. J Clin Psychiatry. 2003;64(4):370–82.
Miller AL, Crismon ML, Rush AJ, et al. The Texas medication algorithm project: clinical results for schizophrenia. Schizophr Bull. 2004;30(3):627–47.
Barrison AF, Smith C, Oviedo J, et al. Colorectal cancer screening and familial risk: a survey of internal medicine residents’ knowledge and practice patterns. Am J Gastroenterol. 2003;98(6):1410–6.
Grover ML, Bracamonte JD, Kanodia AK, et al. Assessing adherence to evidence-based guidelines for the diagnosis and management of uncomplicated urinary tract infection. Mayo Clin Proc. 2007;82(2):181–5.
Lenz O, Fornoni A. Chronic kidney disease care delivered by US family medicine and internal medicine trainees: results from an online survey. BMC Med. 2006;4:30.
Mitchell AJ, Delaffon V, Vancampfort D, et al. Guideline concordant monitoring of metabolic risk in people treated with antipsychotic medication: systematic review and meta-analysis of screening practices. Psychol Med. 2012;42(1):125–47. doi:10.1017/S003329171100105X. Epub 2011 Aug 10.
Akl EA, Mustafa R, Wilson MC, et al. Curricula for teaching the content of clinical practice guidelines to family medicine and internal medicine residents in the US: a survey study. Implement Sci. 2009;4:59.
Forsetlund L, Bjørndal A, Rashidian A, et al. Continuing education meetings and workshops: effects on professional practice and healthcare outcomes. Cochrane Database Syst Rev. 2009;2, CD003030.
Yager J, Zarin DA, Pincus HA, et al. Practice guidelines and psychiatric education potential implications. Acad Psychiat. 1997;21:226–33.
Garfield D, Atre-Vaidya N, Sierles F. Teaching the APA Practice Guidelines to psychiatry residents: a novel strategy. Acad Psychiat. 2002;26:70–5.
Osser DN, Patterson RD, Levitt JJ. Guidelines, algorithms, and evidence-based psychopharmacology training for psychiatric residents. Acad Psychiat. 2005;29:180–6.
Byerly MJ, Brenner A (2008, March) Using APA Practice Guidelines in resident didactic education. Poster session presented at the Annual Meeting of the American Association of Directors of Psychiatric Residency Training, New Orleans, LA.
Falzer PR, Garman MD. A conditional model of evidence-based decision making. J Eval Clin Pract. 2009;15(6):1142–51.
Falzer PR, Garman DM. Evidence-based decision-making as a practice-based learning skill: a pilot study. Acad Psychiat. 2012;36(2):104–9.
Accreditation Council for Graduate Medical Education (ACGME) Outcomes Project [http://www.acgme.org/Outcome].
Staton LJ, Kramer SM, Patel S, et al. Peer chart audits: a tool to meet Accreditation Council on Graduate Medical Education (ACGME) competency in practice-based learning and improvement. Implement Sci. 2007;2:24.
Jamtvedt G, Young JM, Kristoffersen DT, et al. Audit and feedback: effects on professional practice and health care outcomes. Cochrane Database of Syst Rev. 2006:CD000259.
Trivedi MH, Kern JK, Grannemann BD, Altshuler KZ, Sunderajan P. A computerized clinical decision support system as a means of implementing depression guidelines. Psychiatr Serv. 2004;55(8):879–85.
Asch DA, Jedrziewski MK, Christakis NA. Response rates to mail surveys published in medical journals. J Clin Epidemiol. 1997;50:1129–36.
Satterlee WG, Eggers RG, Grimes DA. Effective medical education: insights from the Cochrane Library. Obstet Gynecol Surv. 2008;63(5):329–33.
Karpicke JD, Blunt JR. Retrieval practice produces more learning than elaborative studying with concept mapping. Science. 2011;331(6018):772–5.
Cook DA, Hatala R, Brydges R, Zendejas B, Szostek JH, Wang AT, et al. Technology-enhanced simulation for health professions education: a systematic review and meta-analysis. JAMA. 2011;306(9):978–88.
Disclosures
Dr Byerly has the following financial disclosures: Merck - received speaker’s bureau honoraria, travel funds, and advisory panel payments. Novartis - received speaker’s bureau honoraria, travel funds, and advisory panel payments. Otsuka - received advisory panel payments and research grants. The other authors have no disclosures.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bannister, E., Nakonezny, P. & Byerly, M. Curricula for Teaching Clinical Practice Guidelines in US Psychiatry Residency and Child and Adolescent Fellowship Programs: A Survey Study. Acad Psychiatry 38, 198–204 (2014). https://doi.org/10.1007/s40596-014-0057-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40596-014-0057-3